Abstract
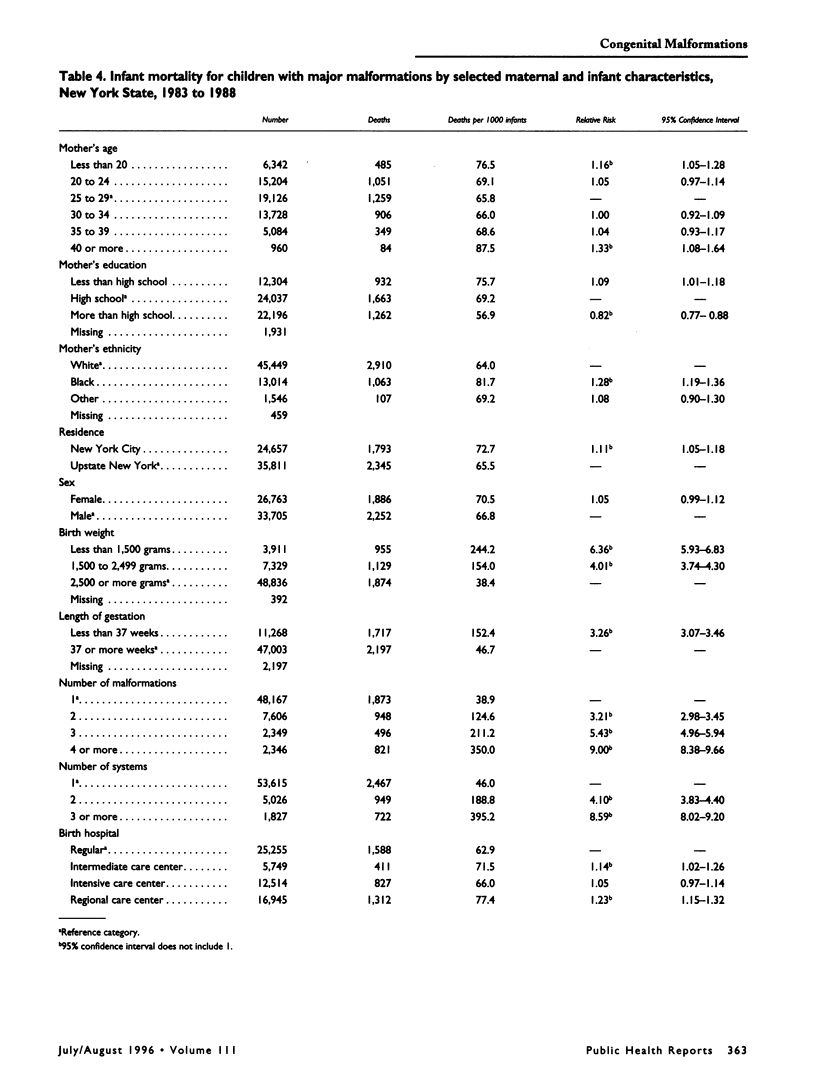
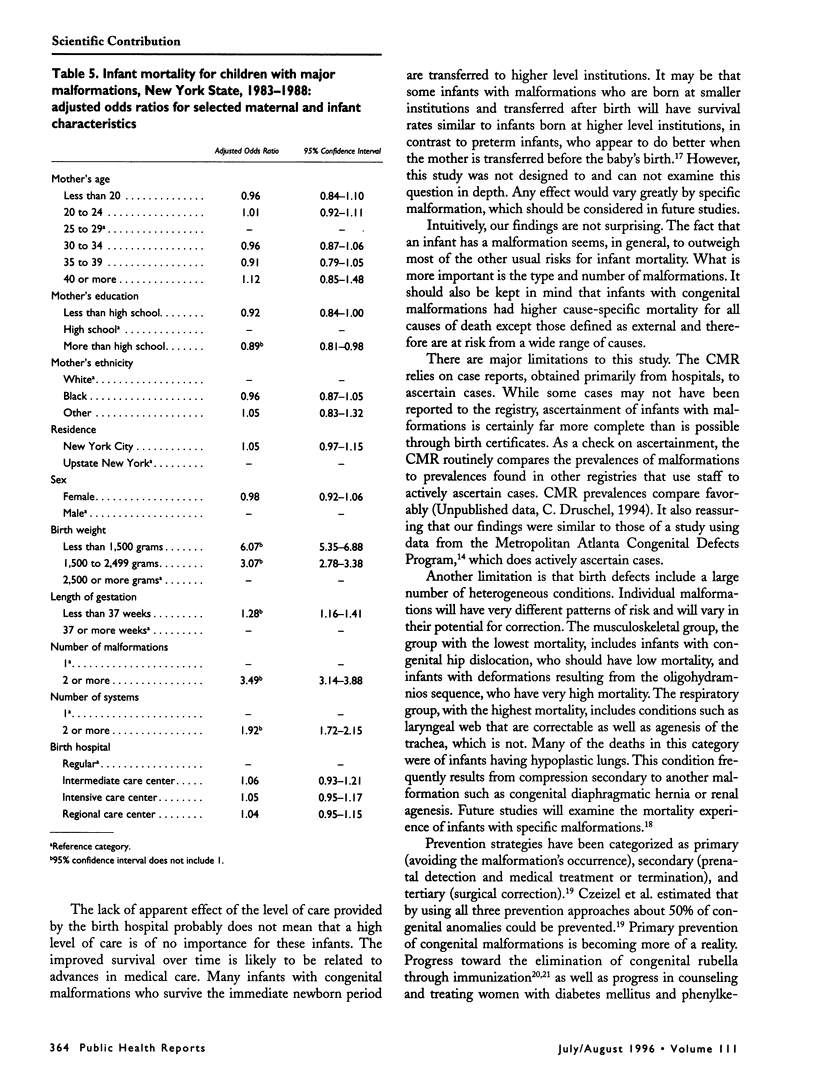
OBJECTIVE. The authors examined first-year mortality and risk factors for mortality among infants with major congenital malformations. METHODS. Infants with major congenital malformations born from 1983 to 1988 were identified from a statewide population-based congenital malformations registry. Variables analyzed included year of birth, birth weight, gestational age, infant sex, number of malformations, number of organ systems involved, level of care of the birth hospital, maternal age, maternal education, and maternal ethnicity. RESULTS. Infants with major malformations had a risk of death 6.3 times higher than the general population of live births. The risk declined from 6.5 in 1983 to 5.9 in 1988. Birth weight and number of malformations were the strongest risk factors. The likelihood of survival was similar for white and black infants. CONCLUSIONS. Being born with a malformation outweighs most of the other risks for infant mortality. Children with congenital malformations had higher cause-specific mortality for all causes except injury.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berry R. J., Buehler J. W., Strauss L. T., Hogue C. J., Smith J. C. Birth weight-specific infant mortality due to congenital anomalies, 1960 and 1980. Public Health Rep. 1987 Mar-Apr;102(2):171–181. [PMC free article] [PubMed] [Google Scholar]
- Cochi S. L., Edmonds L. E., Dyer K., Greaves W. L., Marks J. S., Rovira E. Z., Preblud S. R., Orenstein W. A. Congenital rubella syndrome in the United States, 1970-1985. On the verge of elimination. Am J Epidemiol. 1989 Feb;129(2):349–361. doi: 10.1093/oxfordjournals.aje.a115138. [DOI] [PubMed] [Google Scholar]
- Czeizel A. E., Intôdy Z., Modell B. What proportion of congenital abnormalities can be prevented? BMJ. 1993 Feb 20;306(6876):499–503. doi: 10.1136/bmj.306.6876.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeizel A. E. Prevention of congenital abnormalities by periconceptional multivitamin supplementation. BMJ. 1993 Jun 19;306(6893):1645–1648. doi: 10.1136/bmj.306.6893.1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Druschel C. M. A descriptive study of prune belly in New York State, 1983 to 1989. Arch Pediatr Adolesc Med. 1995 Jan;149(1):70–76. doi: 10.1001/archpedi.1995.02170130072017. [DOI] [PubMed] [Google Scholar]
- Eskes T. K., Mooij P. N., Steegers-Theunissen R. P., Lips J. P., Pasker-de Jong P. C. Prepregnancy care and prevention of birth defects. J Perinat Med. 1992;20(4):253–265. doi: 10.1515/jpme.1992.20.4.253. [DOI] [PubMed] [Google Scholar]
- Hexter A. C., Harris J. A., Roeper P., Croen L. A., Krueger P., Gant D. Evaluation of the hospital discharge diagnoses index and the birth certificate as sources of information on birth defects. Public Health Rep. 1990 May-Jun;105(3):296–307. [PMC free article] [PubMed] [Google Scholar]
- Hogue C. J., Buehler J. W., Strauss L. T., Smith J. C. Overview of the National Infant Mortality Surveillance (NIMS) project--design, methods, results. Public Health Rep. 1987 Mar-Apr;102(2):126–138. [PMC free article] [PubMed] [Google Scholar]
- Hook E. B., Cross P. K., Regal R. R. The frequency of 47,+21,47,+18, and 47,+13 at the uppermost extremes of maternal ages: results on 56,094 fetuses studied prenatally and comparisons with data on livebirths. Hum Genet. 1984;68(3):211–220. doi: 10.1007/BF00418391. [DOI] [PubMed] [Google Scholar]
- Hujoel P. P., Bollen A. M., Mueller B. A. First-year mortality among infants with facial clefts. Cleft Palate Craniofac J. 1992 Sep;29(5):451–455. doi: 10.1597/1545-1569_1992_029_0451_fymaiw_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- Jason J. M., Jarvis W. R. Infectious diseases: preventable causes of infant mortality. Pediatrics. 1987 Sep;80(3):335–341. [PubMed] [Google Scholar]
- Kalter H., Warkany J. Medical progress. Congenital malformations: etiologic factors and their role in prevention (first of two parts). N Engl J Med. 1983 Feb 24;308(8):424–431. doi: 10.1056/NEJM198302243080804. [DOI] [PubMed] [Google Scholar]
- Koch R., Levy H. L., Matalon R., Rouse B., Hanley W., Azen C. The North American Collaborative Study of Maternal Phenylketonuria. Status report 1993. Am J Dis Child. 1993 Nov;147(11):1224–1230. doi: 10.1001/archpedi.1993.02160350098015. [DOI] [PubMed] [Google Scholar]
- Li D. K., Daling J. R., Mueller B. A., Hickok D. E., Fantel A. G., Weiss N. S. Periconceptional multivitamin use in relation to the risk of congenital urinary tract anomalies. Epidemiology. 1995 May;6(3):212–218. doi: 10.1097/00001648-199505000-00004. [DOI] [PubMed] [Google Scholar]
- Lindegren M. L., Fehrs L. J., Hadler S. C., Hinman A. R. Update: rubella and congenital rubella syndrome, 1980-1990. Epidemiol Rev. 1991;13:341–348. doi: 10.1093/oxfordjournals.epirev.a036077. [DOI] [PubMed] [Google Scholar]
- Mills J. L., Knopp R. H., Simpson J. L., Jovanovic-Peterson L., Metzger B. E., Holmes L. B., Aarons J. H., Brown Z., Reed G. F., Bieber F. R. Lack of relation of increased malformation rates in infants of diabetic mothers to glycemic control during organogenesis. N Engl J Med. 1988 Mar 17;318(11):671–676. doi: 10.1056/NEJM198803173181104. [DOI] [PubMed] [Google Scholar]
- Naylor A., Eaton A. P., Aplin E. R., Eska B. Birth certificate revision and reporting of congenital malformations. Am J Public Health. 1974 Aug;64(8):786–791. doi: 10.2105/ajph.64.8.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper J. M., Mitchel E. F., Jr, Snowden M., Hall C., Adams M., Taylor P. Validation of 1989 Tennessee birth certificates using maternal and newborn hospital records. Am J Epidemiol. 1993 Apr 1;137(7):758–768. doi: 10.1093/oxfordjournals.aje.a116736. [DOI] [PubMed] [Google Scholar]
- Shaw G. M., Lammer E. J., Wasserman C. R., O'Malley C. D., Tolarova M. M. Risks of orofacial clefts in children born to women using multivitamins containing folic acid periconceptionally. Lancet. 1995 Aug 12;346(8972):393–396. doi: 10.1016/s0140-6736(95)92778-6. [DOI] [PubMed] [Google Scholar]
- Tolarova M., Harris J. Reduced recurrence of orofacial clefts after periconceptional supplementation with high-dose folic acid and multivitamins. Teratology. 1995 Feb;51(2):71–78. doi: 10.1002/tera.1420510205. [DOI] [PubMed] [Google Scholar]
- Welch K. J., Kraney G. P. Abdominal musculature deficiency syndrome prune belly. J Urol. 1974 May;111(5):693–700. doi: 10.1016/s0022-5347(17)60049-1. [DOI] [PubMed] [Google Scholar]
- Woodhouse C. R., Ransley P. G., Innes-Williams D. Prune belly syndrome--report of 47 cases. Arch Dis Child. 1982 Nov;57(11):856–859. doi: 10.1136/adc.57.11.856. [DOI] [PMC free article] [PubMed] [Google Scholar]


