Abstract
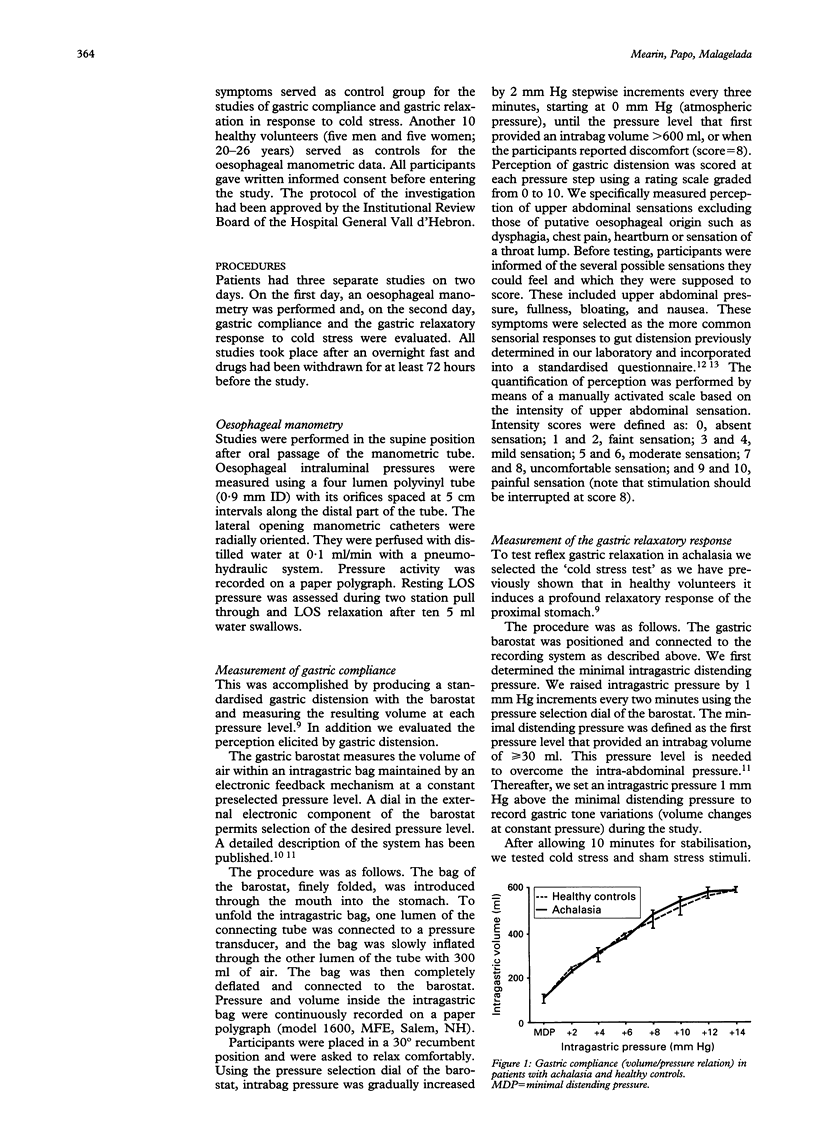
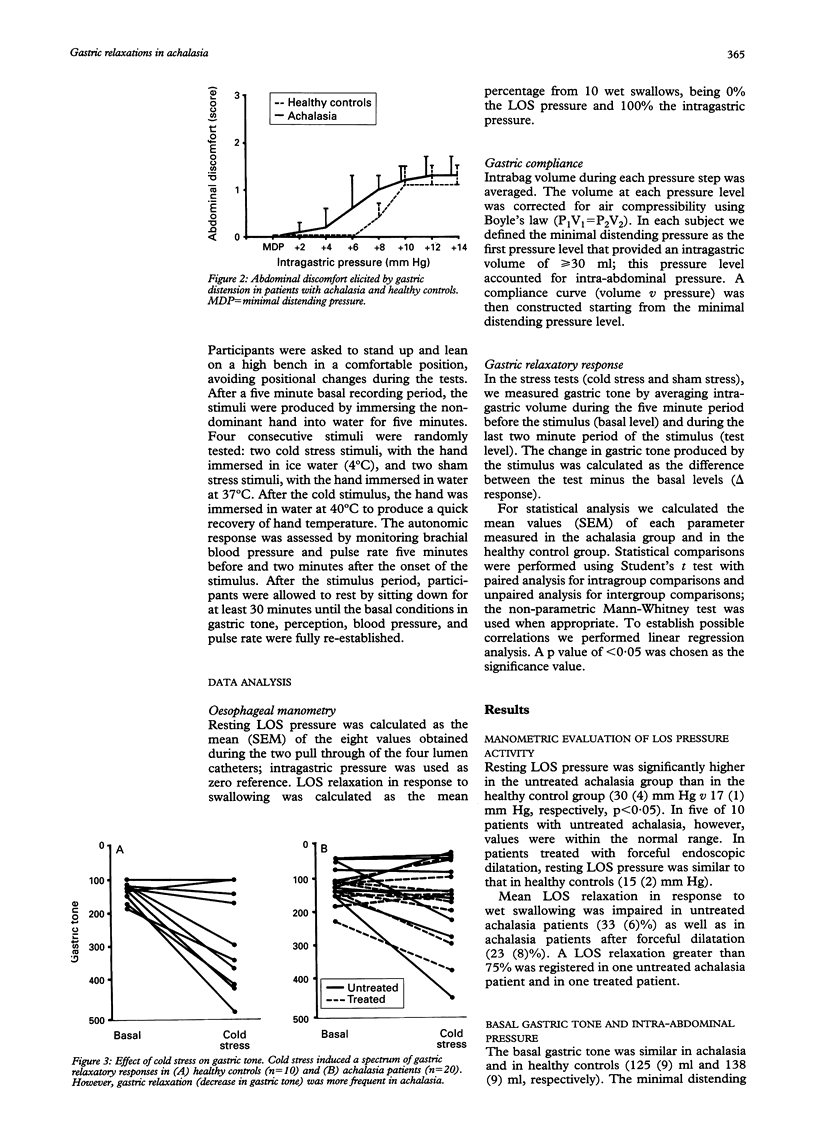
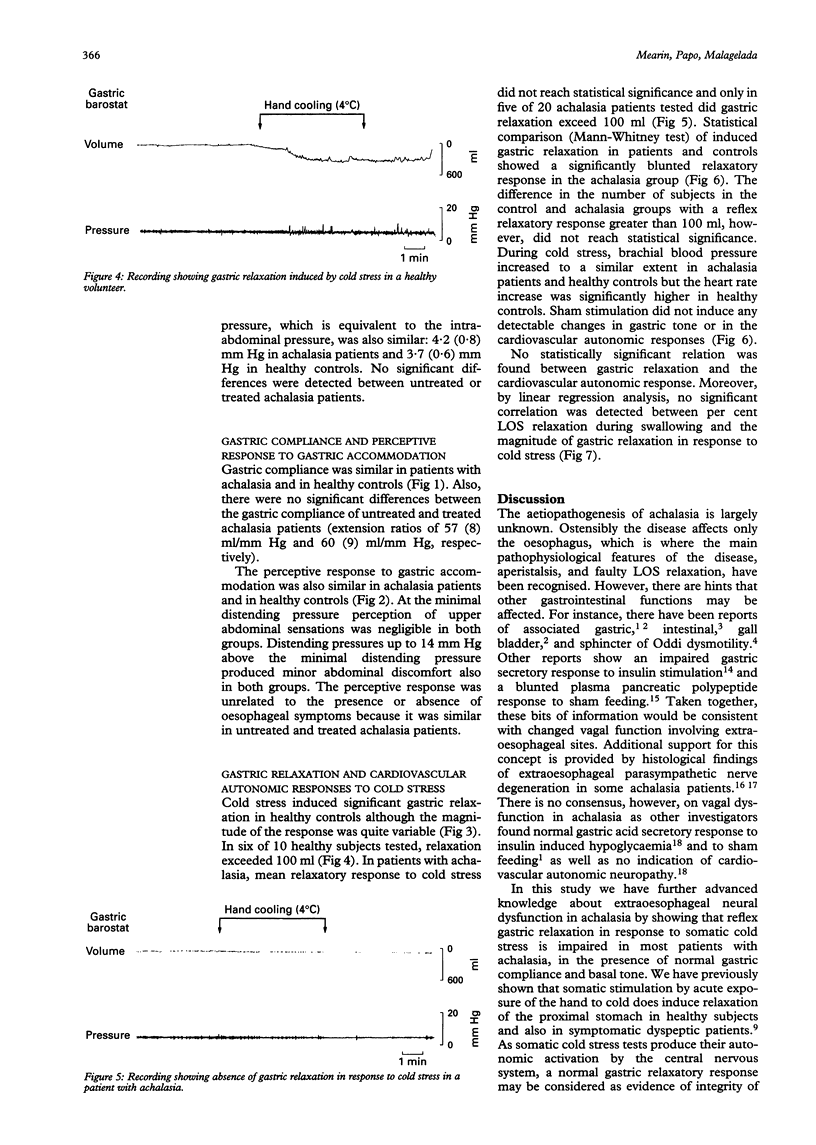
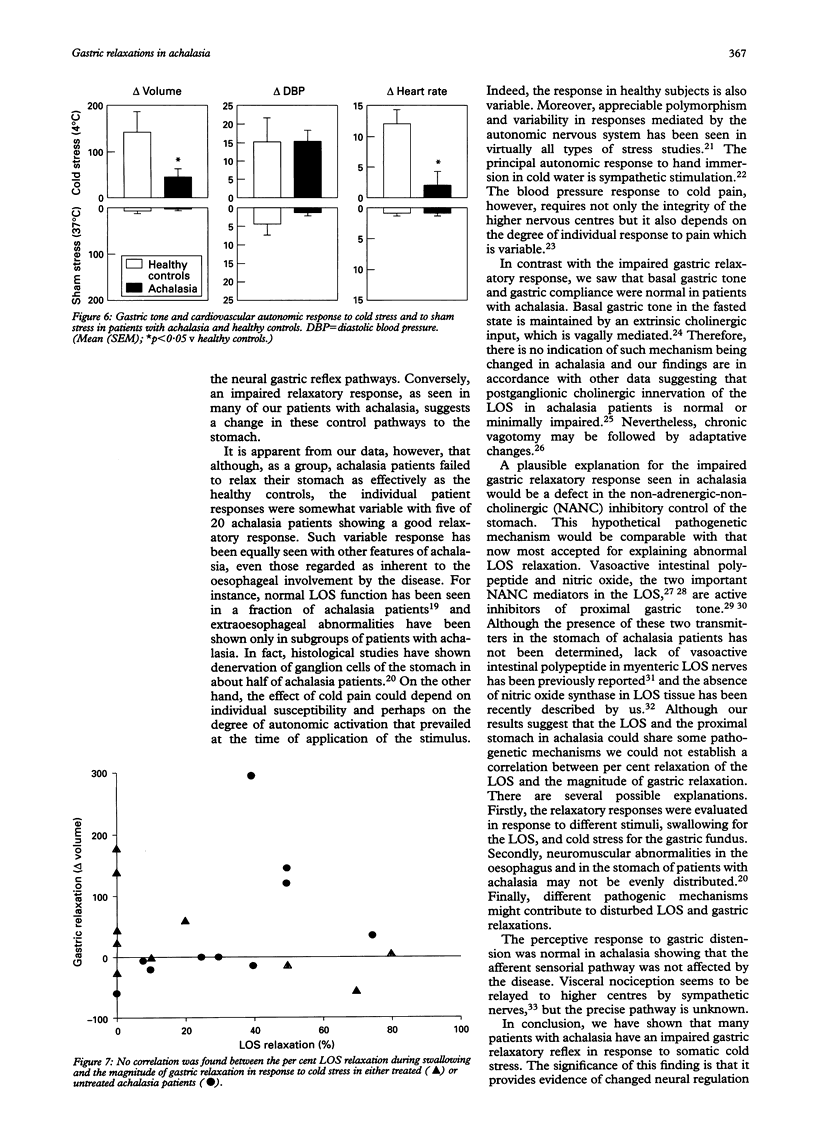
Achalasia is considered a primary motility disorder confined to the oesophagus. The lower oesophageal sphincter (LOS) in achalasia is frequently hypertonic and manifests absent or incomplete relaxation in response to deglution. On the other hand, the LOS and the proximal stomach act physiologically as a functional unit whereby relaxation of the LOS during deglution is associated with receptive relaxation of the proximal stomach. Thus, this study investigated the hypothesis that impaired LOS relaxation in patients with achalasia might be associated with impaired relaxation of the proximal stomach. The study consisted of 20 patients with achalasia and 10 healthy controls. Gastric tone variations were quantified using an electronic barostat. Firstly, the study established the basal gastric tone (intragastric volume at the minimal distending pressure+1 mm Hg) and gastric compliance (volume/pressure relation) during isobaric distension (increasing stepwise the intragastric pressure from 0 to 20 mm Hg up to 600 ml). Secondly, the gastric tone response to cold stress (hand immersion into ice water for five minutes) or to control stimuli (water at 37 degrees) was determined. Basal gastric tone mean (SEM) was similar in achalasia and in healthy controls (125 (9) ml v 138 (9) ml, respectively). Compliance was linear and similar in both groups, which also showed similar gastric extension ratios (58 (7) ml/mm Hg v 57 (6) ml/mm Hg). Cold stress induced a gastric relaxatory response that, as a group, was significantly lower in achalasia than in healthy controls (volume: 43 (20) ml v 141 (42) ml; p < 0.05). The responses in each group were not uniform, five of the 20 patients with achalasia showed definite (volume > 100 ml) relaxatory responses whereas four of the 10 healthy controls did not. In conclusion, reflex gastric relaxation is impaired in most patients with achalasia showing that the proximal stomach, and not exclusively the oesophagus, may be effected by the disease.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aggestrup S., Uddman R., Sundler F., Fahrenkrug J., Håkanson R., Sørensen H. R., Hambraeus G. Lack of vasoactive intestinal polypeptide nerves in esophageal achalasia. Gastroenterology. 1983 May;84(5 Pt 1):924–927. [PubMed] [Google Scholar]
- Annese V., Caruso N., Accadia L., Gabbrielli A., Modoni S., Frusciante V., Federici T. Gallbladder function and gastric liquid emptying in achalasia. Dig Dis Sci. 1991 Aug;36(8):1116–1120. doi: 10.1007/BF01297456. [DOI] [PubMed] [Google Scholar]
- Atkinson M., Ogilvie A. L., Robertson C. S., Smart H. L. Vagal function in achalasia of the cardia. Q J Med. 1987 Apr;63(240):297–303. [PubMed] [Google Scholar]
- Azpiroz F., Malagelada J. R. Gastric tone measured by an electronic barostat in health and postsurgical gastroparesis. Gastroenterology. 1987 Apr;92(4):934–943. doi: 10.1016/0016-5085(87)90967-x. [DOI] [PubMed] [Google Scholar]
- Azpiroz F., Malagelada J. R. Importance of vagal input in maintaining gastric tone in the dog. J Physiol. 1987 Mar;384:511–524. doi: 10.1113/jphysiol.1987.sp016467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azpiroz F., Malagelada J. R. Isobaric intestinal distension in humans: sensorial relay and reflex gastric relaxation. Am J Physiol. 1990 Feb;258(2 Pt 1):G202–G207. doi: 10.1152/ajpgi.1990.258.2.G202. [DOI] [PubMed] [Google Scholar]
- Azpiroz F., Malagelada J. R. Perception and reflex relaxation of the stomach in response to gut distention. Gastroenterology. 1990 May;98(5 Pt 1):1193–1198. doi: 10.1016/0016-5085(90)90333-v. [DOI] [PubMed] [Google Scholar]
- Azpiroz F., Malagelada J. R. Physiological variations in canine gastric tone measured by an electronic barostat. Am J Physiol. 1985 Feb;248(2 Pt 1):G229–G237. doi: 10.1152/ajpgi.1985.248.2.G229. [DOI] [PubMed] [Google Scholar]
- CASSELLA R. R., ELLIS F. H., Jr, BROWN A. L., Jr FINE-STRUCTURE CHANGES IN ACHALASIA OF THE ESOPHAGUS. I. VAGUS NERVES. Am J Pathol. 1965 Feb;46:279–288. [PMC free article] [PubMed] [Google Scholar]
- Cervero F., Tattersall J. E. Somatic and visceral sensory integration in the thoracic spinal cord. Prog Brain Res. 1986;67:189–205. doi: 10.1016/s0079-6123(08)62763-6. [DOI] [PubMed] [Google Scholar]
- Csendes A., Smok G., Braghetto I., González P., Henríquez A., Csendes P., Pizurno D. Histological studies of Auerbach's plexuses of the oesophagus, stomach, jejunum, and colon in patients with achalasia of the oesophagus: correlation with gastric acid secretion, presence of parietal cells and gastric emptying of solids. Gut. 1992 Feb;33(2):150–154. doi: 10.1136/gut.33.2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desai K. M., Sessa W. C., Vane J. R. Involvement of nitric oxide in the reflex relaxation of the stomach to accommodate food or fluid. Nature. 1991 Jun 6;351(6326):477–479. doi: 10.1038/351477a0. [DOI] [PubMed] [Google Scholar]
- Dooley C. P., Taylor I. L., Valenzuela J. E. Impaired acid secretion and pancreatic polypeptide release in some patients with achalasia. Gastroenterology. 1983 Apr;84(4):809–813. [PubMed] [Google Scholar]
- Eckardt V. F., Krause J., Bolle D. Gastrointestinal transit and gastric acid secretion in patients with achalasia. Dig Dis Sci. 1989 May;34(5):665–671. doi: 10.1007/BF01540335. [DOI] [PubMed] [Google Scholar]
- Goyal R. K., Rattan S., Said S. I. VIP as a possible neurotransmitter of non-cholinergic non-adrenergic inhibitory neurones. Nature. 1980 Nov 27;288(5789):378–380. doi: 10.1038/288378a0. [DOI] [PubMed] [Google Scholar]
- Hagenmüller F., Classen M. Motility of Oddi's sphincter in Parkinson's disease, progressive systemic sclerosis, and achalasia. Endoscopy. 1988 Aug;20 (Suppl 1):189–192. doi: 10.1055/s-2007-1018174. [DOI] [PubMed] [Google Scholar]
- Holloway R. H., Dodds W. J., Helm J. F., Hogan W. J., Dent J., Arndorfer R. C. Integrity of cholinergic innervation to the lower esophageal sphincter in achalasia. Gastroenterology. 1986 Apr;90(4):924–929. doi: 10.1016/0016-5085(86)90869-3. [DOI] [PubMed] [Google Scholar]
- Katz P. O., Richter J. E., Cowan R., Castell D. O. Apparent complete lower esophageal sphincter relaxation in achalasia. Gastroenterology. 1986 Apr;90(4):978–983. doi: 10.1016/0016-5085(86)90876-0. [DOI] [PubMed] [Google Scholar]
- Lefkowitz R. J. Clinical physiology of adrenergic receptor regulation. Am J Physiol. 1982 Jul;243(1):E43–E47. doi: 10.1152/ajpendo.1982.243.1.E43. [DOI] [PubMed] [Google Scholar]
- Lovallo W. The cold pressor test and autonomic function: a review and integration. Psychophysiology. 1975 May;12(3):268–282. doi: 10.1111/j.1469-8986.1975.tb01289.x. [DOI] [PubMed] [Google Scholar]
- Mearin F., Cucala M., Azpiroz F., Malagelada J. R. The origin of symptoms on the brain-gut axis in functional dyspepsia. Gastroenterology. 1991 Oct;101(4):999–1006. doi: 10.1016/0016-5085(91)90726-2. [DOI] [PubMed] [Google Scholar]
- Mearin F., Mourelle M., Guarner F., Salas A., Riveros-Moreno V., Moncada S., Malagelada J. R. Patients with achalasia lack nitric oxide synthase in the gastro-oesophageal junction. Eur J Clin Invest. 1993 Nov;23(11):724–728. doi: 10.1111/j.1365-2362.1993.tb01292.x. [DOI] [PubMed] [Google Scholar]
- Tøttrup A., Svane D., Forman A. Nitric oxide mediating NANC inhibition in opossum lower esophageal sphincter. Am J Physiol. 1991 Mar;260(3 Pt 1):G385–G389. doi: 10.1152/ajpgi.1991.260.3.G385. [DOI] [PubMed] [Google Scholar]
- Vantrappen G., Hellemans J. Treatment of achalasia and related motor disorders. Gastroenterology. 1980 Jul;79(1):144–154. [PubMed] [Google Scholar]
- WOLFF H. H. The mechanism and significance of the cold pressor response. Q J Med. 1951 Jul;20(79):261–273. [PubMed] [Google Scholar]
- de la Fuente A., Garcia-Calvo M., Ramon y Cajal, Cuesta P. G. Alteraciones ultraestructurales del nervio vago en la acalasia del esófago. Rev Esp Enferm Apar Dig. 1977 Nov 15;51(6):659–666. [PubMed] [Google Scholar]


