Abstract
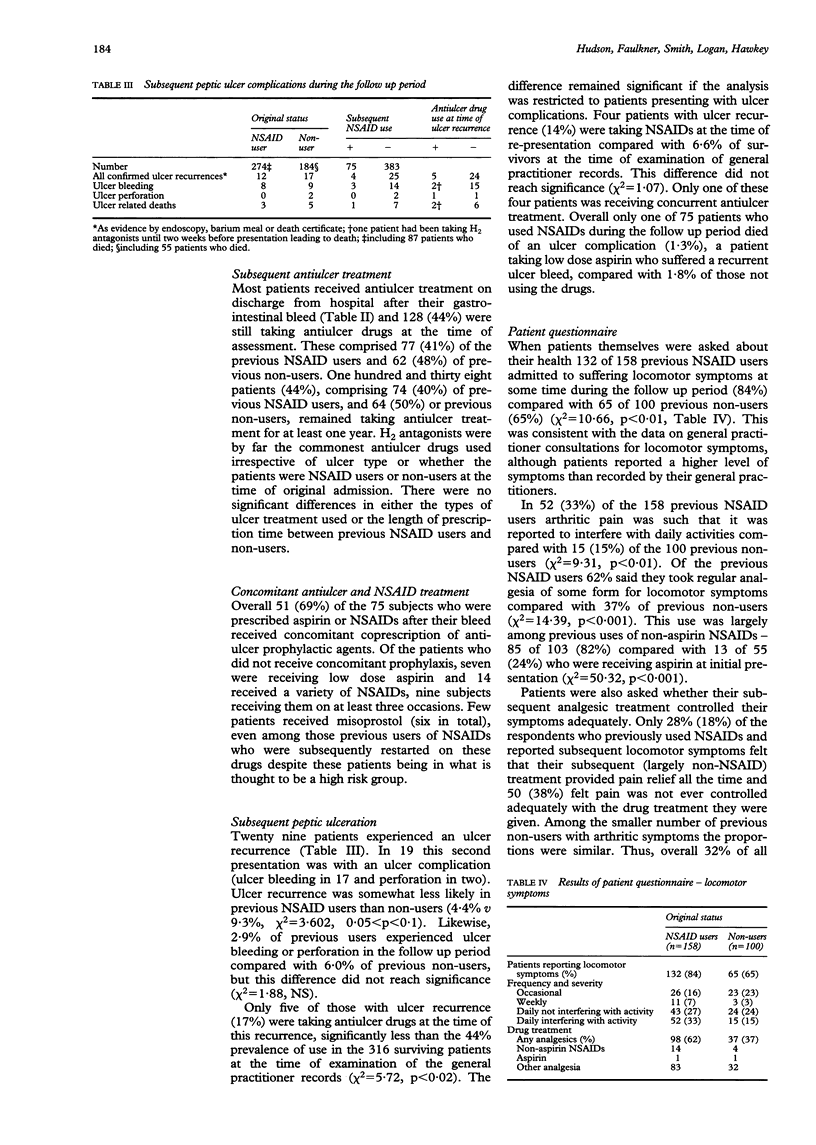
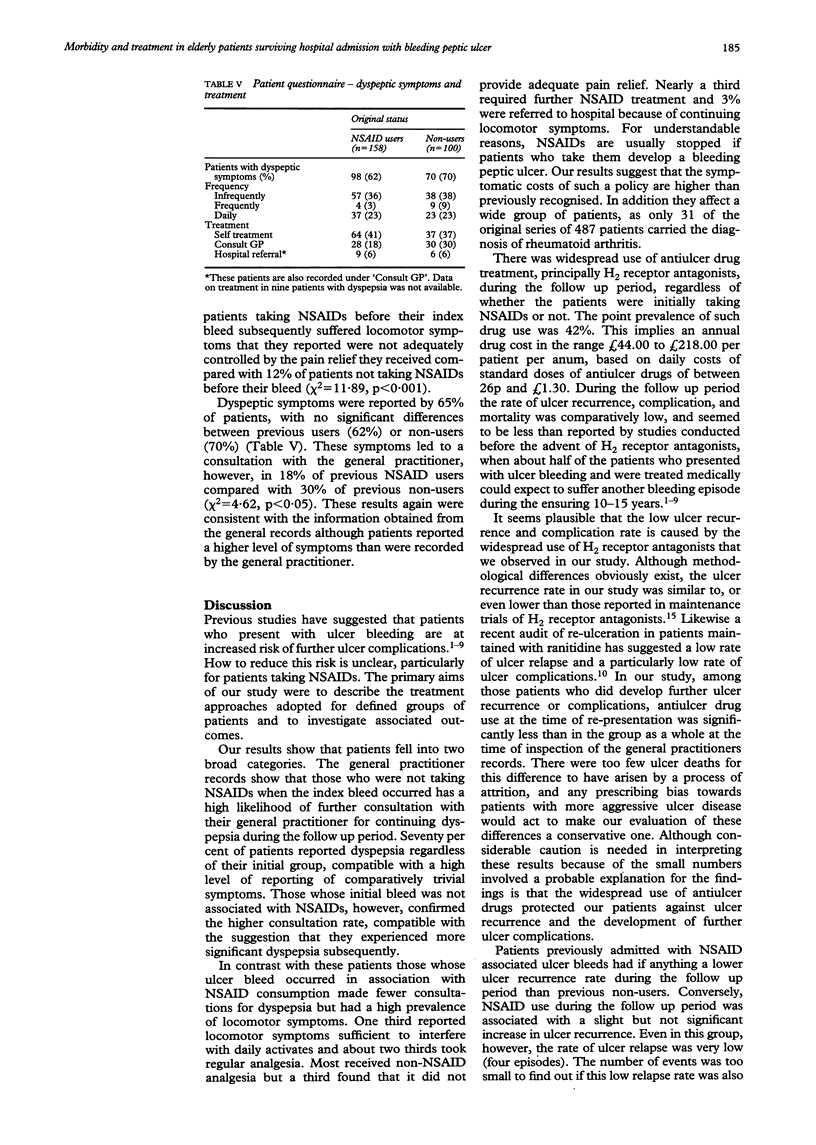
Bleeding peptic ulcer in the elderly is associated with use of non-steroidal, anti-inflammatory drugs (NSAIDs) and aspirin, presenting a therapeutic dilemma for the treatment of survivors. To determine the longterm morbidity of patients surviving bleeding peptic ulcer and their treatment, with particular reference to NSAID use, this study followed up 487 patients aged over 60 years, who survived an episode of bleeding peptic ulcer in Nottingham during 1986 to 1991. Information was gathered by evaluation of general practitioner and hospital records, scrutiny of death certificates, and postal questionnaire to surviving patients. Of 487 patients surviving a bleeding peptic ulcer, 345 were alive at the follow up, a mean 34.2 months after discharge. Of these 201 (58%) had taken NSAIDs before their ulcer bleed (104 non-aspirin NSAIDs, 77 aspirin, 20 both). Compared with non-users, the patients using NSAIDs at the time of presentation were significantly more likely subsequently to consult their general practitioner with locomotor symptoms (56% v 35%, p < 0.001) and receive further NSAIDs (34% v 13%, p < 0.001), but significantly less likely to consult their general practitioner for dyspepsia (31% v 54%, p < 0.001). Antiulcer drug use was widespread in both groups, with an overall point prevalence of 44%. Seventy five patients received NSAIDs during the follow up period (69% with coprescription of antiulcer drugs, usually H2 antagonists). Recurrent peptic ulcer, ulcer complications, and ulcer related deaths were uncommon. Antiulcer drug use was lower in those with ulcer recurrence compared with the point prevalence in those without (17% v 44%, p < 0.05). Patient questionnaire responses confirmed a high level of locomotor symptoms especially in patients previously admitted with NSAID associated ulcer bleeding. In conclusion, in patients surviving peptic ulcer bleeding, recurrent ulcer complications and death seem to be lower than reported by studies that preceded the advent of antiulcer drugs. It is suggested that this low incidence may be a consequence of their use. Granted the low level of recurrent ulceration and the high level of locomotor symptoms in patients studied, current treatment may unduly emphasise the importance of stopping NSAIDs in this group of patients.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ARIAS I. M., ZAMCHECK N., THROWER W. B. Recurrence of hemorrhage from medically treated gastric ulcers; four-to eight-year follow-up of forty-seven patients. AMA Arch Intern Med. 1958 Feb;101(2):369–376. doi: 10.1001/archinte.1958.00260140201030. [DOI] [PubMed] [Google Scholar]
- BOLES R. S., Jr, CASSIDY W. J., JORDAN S. M. Medical versus surgical management for the complication of hemorrhage in duodenal ulcer. Gastroenterology. 1957 Jan;32(1):52-7; discussion, 57-9. [PubMed] [Google Scholar]
- Borland J. L., Sr, Hancock W. R., Borland J. L., Jr Recurrent upper gastrointestinal hemorrhage in peptic ulcer. Gastroenterology. 1967 Apr;52(4):631–637. [PubMed] [Google Scholar]
- Bradley J. D., Brandt K. D., Katz B. P., Kalasinski L. A., Ryan S. I. Comparison of an antiinflammatory dose of ibuprofen, an analgesic dose of ibuprofen, and acetaminophen in the treatment of patients with osteoarthritis of the knee. N Engl J Med. 1991 Jul 11;325(2):87–91. doi: 10.1056/NEJM199107113250203. [DOI] [PubMed] [Google Scholar]
- Doyle D. V., Dieppe P. A., Scott J., Huskisson E. C. An articular index for the assessment of osteoarthritis. Ann Rheum Dis. 1981 Feb;40(1):75–78. doi: 10.1136/ard.40.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabriel S. E., Jaakkimainen L., Bombardier C. Risk for serious gastrointestinal complications related to use of nonsteroidal anti-inflammatory drugs. A meta-analysis. Ann Intern Med. 1991 Nov 15;115(10):787–796. doi: 10.7326/0003-4819-115-10-787. [DOI] [PubMed] [Google Scholar]
- Gough K. R., Korman M. G., Bardhan K. D., Lee F. I., Crowe J. P., Reed P. I., Smith R. N. Ranitidine and cimetidine in prevention of duodenal ulcer relapse. A double-blind, randomised, multicentre, comparative trial. Lancet. 1984 Sep 22;2(8404):659–662. doi: 10.1016/s0140-6736(84)91224-8. [DOI] [PubMed] [Google Scholar]
- Graham D. Y., Hepps K. S., Ramirez F. C., Lew G. M., Saeed Z. A. Treatment of Helicobacter pylori reduces the rate of rebleeding in peptic ulcer disease. Scand J Gastroenterol. 1993 Nov;28(11):939–942. doi: 10.3109/00365529309098288. [DOI] [PubMed] [Google Scholar]
- Hallenbeck G. A. Elective surgery for treatment of hemorrhage from duodenal ulcer. Gastroenterology. 1970 Nov;59(5):784–789. [PubMed] [Google Scholar]
- Harvey R. F., Langman M. J. The late results of medical and surgical treatment for bleeding duodenal ulcer. Q J Med. 1970 Oct;39(156):539–547. [PubMed] [Google Scholar]
- Hawkey C. J. Non-steroidal anti-inflammatory drugs and peptic ulcers. BMJ. 1990 Feb 3;300(6720):278–284. doi: 10.1136/bmj.300.6720.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson C., Bàràny F. A retrospective study on the outcome of massive bleeding from peptic ulceration. Scand J Gastroenterol. 1973;8(2):113–118. [PubMed] [Google Scholar]
- Jones A. C., Berman P., Doherty M. Non-steroidal anti-inflammatory drug usage and requirement in elderly acute hospital admissions. Br J Rheumatol. 1992 Jan;31(1):45–48. doi: 10.1093/rheumatology/31.1.45. [DOI] [PubMed] [Google Scholar]
- MacLeod I. A., Mills P. R. Factors identifying the probability of further haemorrhage after acute upper gastrointestinal haemorrhage. Br J Surg. 1982 May;69(5):256–258. doi: 10.1002/bjs.1800690509. [DOI] [PubMed] [Google Scholar]
- Serebro H. A., Mendeloff A. I. Late results of medical and surgical treatment of bleeding peptic ulcer. Lancet. 1966 Sep 3;2(7462):505–508. doi: 10.1016/s0140-6736(66)92874-1. [DOI] [PubMed] [Google Scholar]
- Wyllie J. H., Clark C. G., Alexander-Williams J., Bell P. R., Kennedy T. L., Kirk R. M., MacKay C. Effect of cimetidine on surgery for duodenal ulcer. Lancet. 1981 Jun 13;1(8233):1307–1308. doi: 10.1016/s0140-6736(81)92472-7. [DOI] [PubMed] [Google Scholar]


