Abstract
From 1979 to 1985 2435 patients having had transient ischaemic attacks (TIAs) or minor ischaemic strokes, were enrolled in the UK TIA trial and were randomised to receive either aspirin 300 mg, daily or aspirin 1200 mg or placebo. Analysis of reported upper gastrointestinal bleeding events (defined as haematemesis or melaena, or both) showed a risk of bleeding in a dose dependent manner, odds ratios (95% CI) for 300 mg of aspirin = 3.3 (1.2 to 9.0) and for 1200 mg = 6.4 (2.5 to 16.5) and, as would be expected, an increased risk of hospitalisation because of bleeding also in a dose dependent manner, odds ratio = 3.6 (0.7 to 17.2) for 300 mg and 8.7 (2.0 to 37.6) for 1200 mg. Further analysis suggested greater risks of bleeding from duodenal ulcers than gastric ulcers and that bleeding is more likely early in the course of treatment with aspirin used as secondary prevention. There was also an increased risk of lower gastrointestinal bleeding, defined as fresh blood per rectum for both doses of aspirin, odds ratio 1.8 (0.5 to 6.1) for 300 mg of aspirin, and 1.5 (0.4 to 5.3) for 1200 mg of aspirin.
Full text
PDF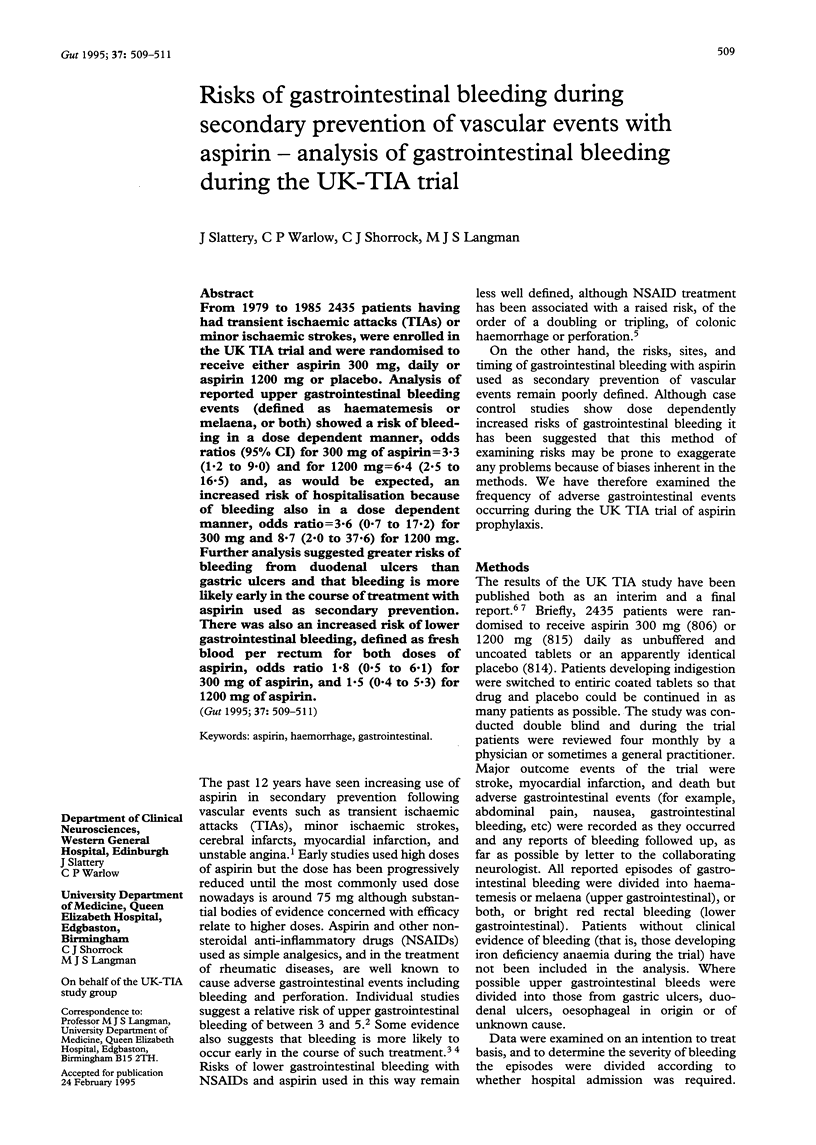

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Graham D. Y., Smith J. L., Spjut H. J., Torres E. Gastric adaptation. Studies in humans during continuous aspirin administration. Gastroenterology. 1988 Aug;95(2):327–333. [PubMed] [Google Scholar]
- Griffin M. R., Piper J. M., Daugherty J. R., Snowden M., Ray W. A. Nonsteroidal anti-inflammatory drug use and increased risk for peptic ulcer disease in elderly persons. Ann Intern Med. 1991 Feb 15;114(4):257–263. doi: 10.7326/0003-4819-114-4-257. [DOI] [PubMed] [Google Scholar]
- Langman M. J. Epidemiologic evidence on the association between peptic ulceration and antiinflammatory drug use. Gastroenterology. 1989 Feb;96(2 Pt 2 Suppl):640–646. doi: 10.1016/s0016-5085(89)80060-5. [DOI] [PubMed] [Google Scholar]
- Langman M. J., Morgan L., Worrall A. Use of anti-inflammatory drugs by patients admitted with small or large bowel perforations and haemorrhage. Br Med J (Clin Res Ed) 1985 Feb 2;290(6465):347–349. doi: 10.1136/bmj.290.6465.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langman M. J., Weil J., Wainwright P., Lawson D. H., Rawlins M. D., Logan R. F., Murphy M., Vessey M. P., Colin-Jones D. G. Risks of bleeding peptic ulcer associated with individual non-steroidal anti-inflammatory drugs. Lancet. 1994 Apr 30;343(8905):1075–1078. doi: 10.1016/s0140-6736(94)90185-6. [DOI] [PubMed] [Google Scholar]
- Risk of myocardial infarction and death during treatment with low dose aspirin and intravenous heparin in men with unstable coronary artery disease. The RISC Group. Lancet. 1990 Oct 6;336(8719):827–830. [PubMed] [Google Scholar]
- Shorrock C. J., Prescott R. J., Rees W. D. The effects of indomethacin on gastroduodenal morphology and mucosal pH gradient in the healthy human stomach. Gastroenterology. 1990 Aug;99(2):334–339. doi: 10.1016/0016-5085(90)91013-v. [DOI] [PubMed] [Google Scholar]
- Weil J., Colin-Jones D., Langman M., Lawson D., Logan R., Murphy M., Rawlins M., Vessey M., Wainwright P. Prophylactic aspirin and risk of peptic ulcer bleeding. BMJ. 1995 Apr 1;310(6983):827–830. doi: 10.1136/bmj.310.6983.827. [DOI] [PMC free article] [PubMed] [Google Scholar]



