Abstract
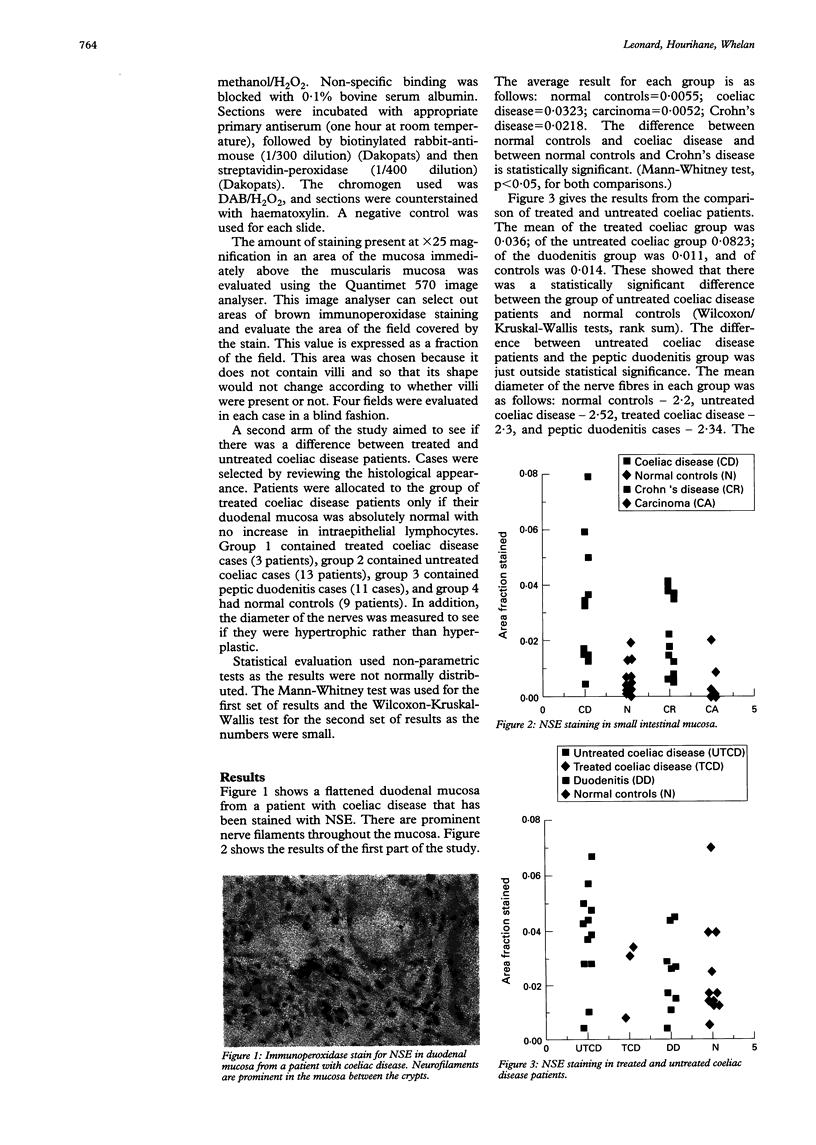
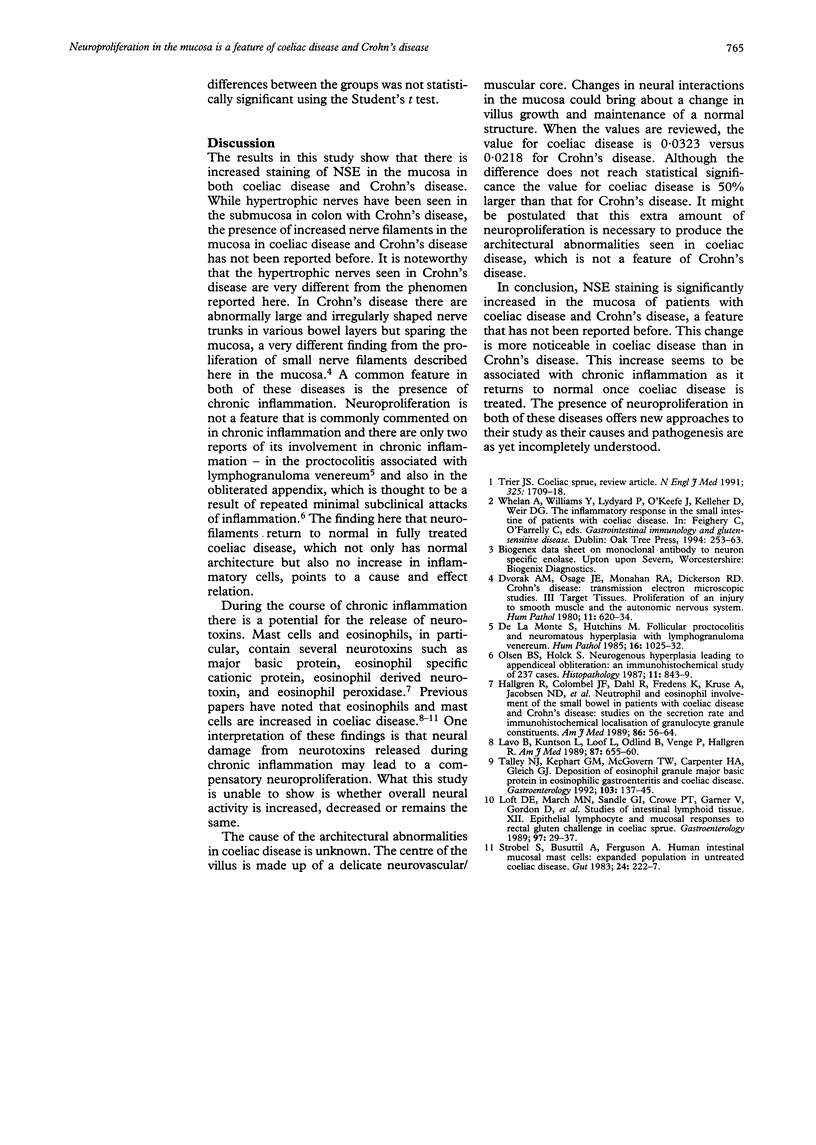
The pathogenesis of villous damage in coeliac disease is unknown. Change to the delicate neuromuscular core may be significant and this study stained various categories of coeliac disease and controls with neuron-specific enolase (NSE) to examine neurofilaments in the mucosa. The amount of NSE staining was evaluated using computer image analysis. The first part of the study compared coeliac disease with Crohn's disease, carcinoma, and biopsy specimens from normal subjects. There was increased NSE staining in both the coeliac disease and Crohn's disease cases but not in carcinomas or normal controls. This difference was statistically significant. The average value for the coeliac disease patients was 50% higher than that of Crohn's disease patients. The second part of the study compared treated coeliac disease with untreated coeliac disease. Treated coeliac disease cases had normal amounts of NSE staining, which were the same as normal controls. These findings suggest that neuroproliferation is a feature of coeliac disease and Crohn's disease. Both share a common feature--namely chronic inflammation--which has been occasionally associated with neuroproliferation. The fact that neuroproliferation resolves with treatment is further evidence for its association with chronic inflammation. The extra neuroproliferation seen in coeliac disease compared with Crohn's disease may contribute to the architectural abnormalities seen in coeliac disease.
Full text
PDF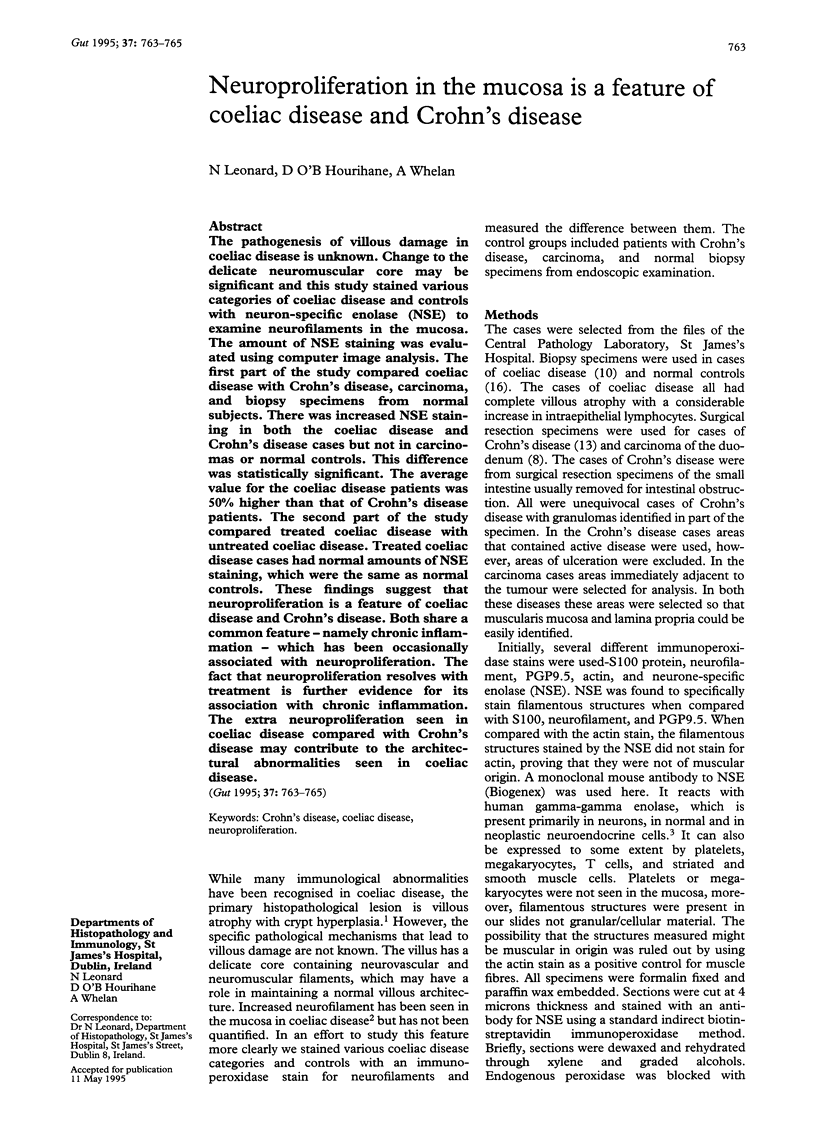
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Dvorak A. M., Osage J. E., Monahan R. A., Dickersin G. R. Crohn's disease: transmission electron microscopic studies. III. Target tissues. Proliferation of and injury to smooth muscle and the autonomic nervous system. Hum Pathol. 1980 Nov;11(6):620–634. doi: 10.1016/s0046-8177(80)80073-6. [DOI] [PubMed] [Google Scholar]
- Hällgren R., Colombel J. F., Dahl R., Fredens K., Kruse A., Jacobsen N. O., Venge P., Rambaud J. C. Neutrophil and eosinophil involvement of the small bowel in patients with celiac disease and Crohn's disease: studies on the secretion rate and immunohistochemical localization of granulocyte granule constituents. Am J Med. 1989 Jan;86(1):56–64. doi: 10.1016/0002-9343(89)90230-1. [DOI] [PubMed] [Google Scholar]
- Lavö B., Knutson L., Löf L., Odlind B., Venge P., Hällgren R. Challenge with gliadin induces eosinophil and mast cell activation in the jejunum of patients with celiac disease. Am J Med. 1989 Dec;87(6):655–660. doi: 10.1016/s0002-9343(89)80399-7. [DOI] [PubMed] [Google Scholar]
- Loft D. E., Marsh M. N., Sandle G. I., Crowe P. T., Garner V., Gordon D., Baker R. Studies of intestinal lymphoid tissue. XII. Epithelial lymphocyte and mucosal responses to rectal gluten challenge in celiac sprue. Gastroenterology. 1989 Jul;97(1):29–37. doi: 10.1016/0016-5085(89)91411-x. [DOI] [PubMed] [Google Scholar]
- Olsen B. S., Holck S. Neurogenous hyperplasia leading to appendiceal obliteration: an immunohistochemical study of 237 cases. Histopathology. 1987 Aug;11(8):843–849. doi: 10.1111/j.1365-2559.1987.tb01887.x. [DOI] [PubMed] [Google Scholar]
- Strobel S., Busuttil A., Ferguson A. Human intestinal mucosal mast cells: expanded population in untreated coeliac disease. Gut. 1983 Mar;24(3):222–227. doi: 10.1136/gut.24.3.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talley N. J., Kephart G. M., McGovern T. W., Carpenter H. A., Gleich G. J. Deposition of eosinophil granule major basic protein in eosinophilic gastroenteritis and celiac disease. Gastroenterology. 1992 Jul;103(1):137–145. doi: 10.1016/0016-5085(92)91106-e. [DOI] [PubMed] [Google Scholar]
- Trier J. S. Celiac sprue. N Engl J Med. 1991 Dec 12;325(24):1709–1719. doi: 10.1056/NEJM199112123252406. [DOI] [PubMed] [Google Scholar]
- de la Monte S. M., Hutchins G. M. Follicular proctocolitis and neuromatous hyperplasia with lymphogranuloma venereum. Hum Pathol. 1985 Oct;16(10):1025–1032. doi: 10.1016/s0046-8177(85)80280-x. [DOI] [PubMed] [Google Scholar]