Abstract
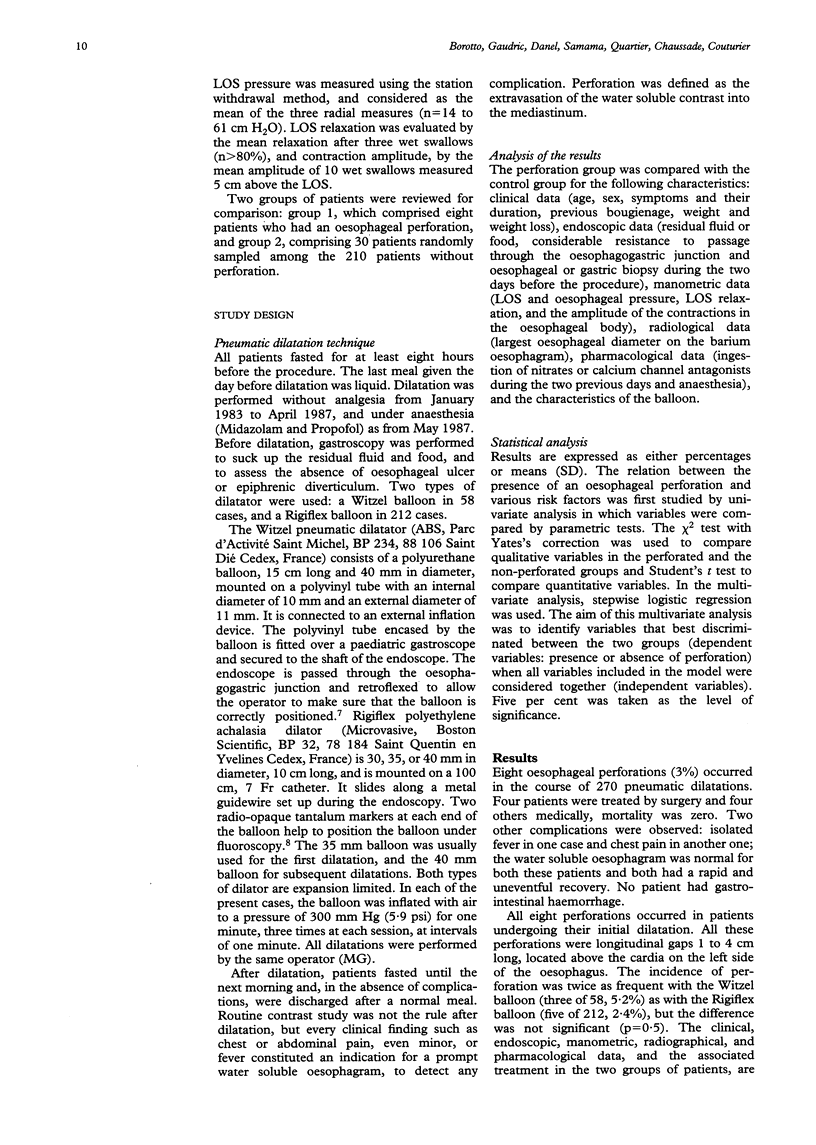
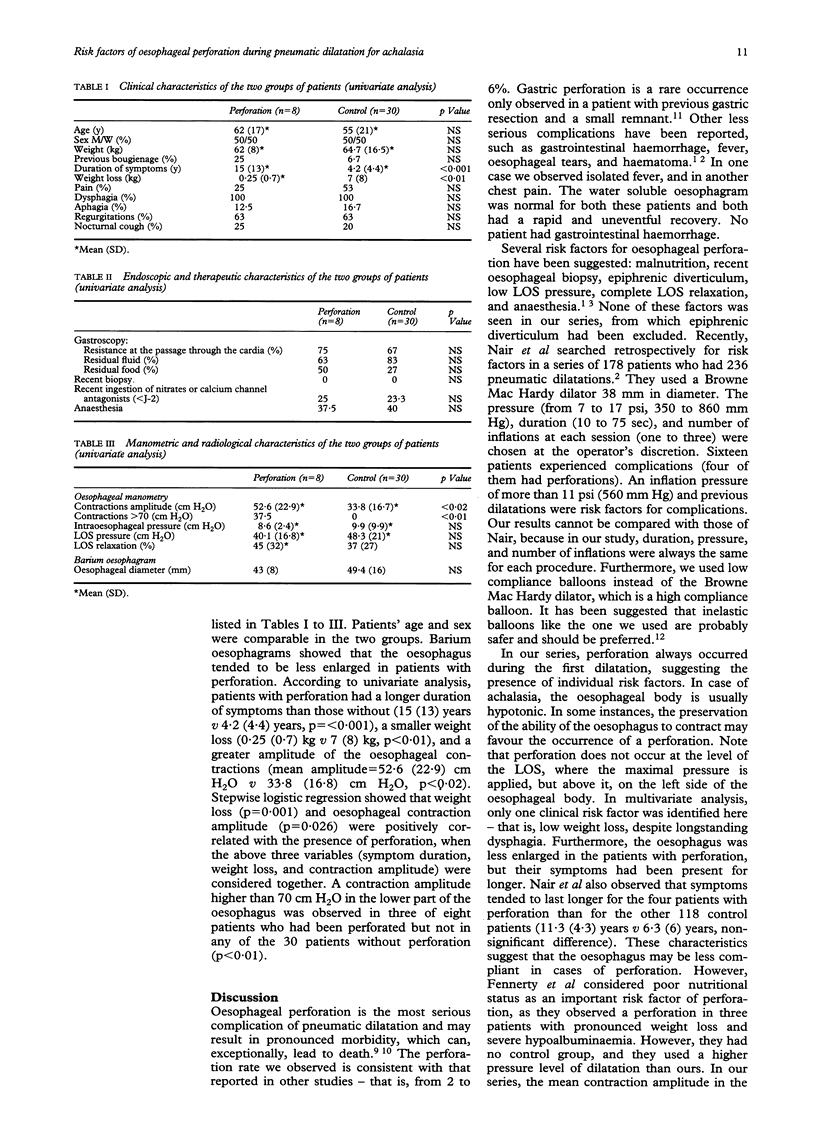
BACKGROUND/AIMS: Pneumatic dilatation of the oesophagus is a well established treatment for achalasia. Oesophageal perforation is the most serious complication that occurs in 2% to 6% of cases. The aim of this retrospective survey was to identify predictive risk factors for perforation in a consecutive series of 218 patients with achalasia. METHODS: Between 1983 and 1993, 270 pneumatic dilatations were performed in 218 patients. A Witzel dilator was used in 58 cases and a Rigiflex dilator in 212. Eight oesophageal perforations occurred (3%). The clinical, radiological, endoscopic, manometric, and technical data for the eight perforated patients were compared with those of 30 patients randomly sampled among those without perforation. RESULTS: All perforations occurred during the first dilatation. Perforations were fewer during dilatations with the Rigiflex dilator than with the Witzel dilator (2.4% v 5.2%). Perforations were all located above the cardia, on the left side of the oesophagus. In a multivariate analysis, a small weight loss and a high amplitude of oesophageal contractions in the group of patients with perforations were predictive of complications (respectively, p = 0.001 and p = 0.026). A contraction amplitude higher than 70 cm H2O in the lower part of the oesophagus was observed in three of eight patients with perforations but was not seen in any of the 30 patients without perforation (p < 0.01). CONCLUSIONS: This identification of risk factors should facilitate the choice between pneumatic dilatation or a surgical approach.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Castell D. O. Achalasia and diffuse esophageal spasm. Arch Intern Med. 1976 May;136(5):571–579. [PubMed] [Google Scholar]
- DERBES V. J., MITCHELL R. E., Jr Rupture of the esophagus. Surgery. 1956 Apr;39(4):688–709. [PubMed] [Google Scholar]
- Fennerty M. B. Esophageal perforation during pneumatic dilatation for achalasia: a possible association with malnutrition. Dysphagia. 1990;5(4):227–228. doi: 10.1007/BF02412692. [DOI] [PubMed] [Google Scholar]
- Henderson J. A., Péloquin A. J. Boerhaave revisited: spontaneous esophageal perforation as a diagnostic masquerader. Am J Med. 1989 May;86(5):559–567. doi: 10.1016/0002-9343(89)90385-9. [DOI] [PubMed] [Google Scholar]
- MACKLER S. A. Spontaneous rupture of the esophagus; an experimental and clinical study. Surg Gynecol Obstet. 1952 Sep;95(3):345–356. [PubMed] [Google Scholar]
- Miller R. E., Tiszenkel H. I. Esophageal perforation due to pneumatic dilation for achalasia. Surg Gynecol Obstet. 1988 May;166(5):458–460. [PubMed] [Google Scholar]
- Nair L. A., Reynolds J. C., Parkman H. P., Ouyang A., Strom B. L., Rosato E. F., Cohen S. Complications during pneumatic dilation for achalasia or diffuse esophageal spasm. Analysis of risk factors, early clinical characteristics, and outcome. Dig Dis Sci. 1993 Oct;38(10):1893–1904. doi: 10.1007/BF01296115. [DOI] [PubMed] [Google Scholar]
- Pasricha P. J., Ravich W. J., Hendrix T. R., Sostre S., Jones B., Kalloo A. N. Intrasphincteric botulinum toxin for the treatment of achalasia. N Engl J Med. 1995 Mar 23;332(12):774–778. doi: 10.1056/NEJM199503233321203. [DOI] [PubMed] [Google Scholar]
- Rabinovici R., Katz E., Goldin E., Kluger Y., Ayalon A. The danger of high compliance balloons for esophageal dilatation in achalasia. Endoscopy. 1990 Mar;22(2):63–64. doi: 10.1055/s-2007-1012793. [DOI] [PubMed] [Google Scholar]
- Reynolds J. C., Parkman H. P. Achalasia. Gastroenterol Clin North Am. 1989 Jun;18(2):223–255. [PubMed] [Google Scholar]
- Tidman M. K., John H. T. Spontaneous rupture of the oesophagus. Br J Surg. 1967 Apr;54(4):286–292. doi: 10.1002/bjs.1800540409. [DOI] [PubMed] [Google Scholar]
- Tulman A. B., Boyce H. W., Jr Complications of esophageal dilation and guidelines for their prevention. Gastrointest Endosc. 1981 Nov;27(4):229–234. doi: 10.1016/s0016-5107(81)73230-9. [DOI] [PubMed] [Google Scholar]
- Vantrappen G., Hellemans J. Treatment of achalasia and related motor disorders. Gastroenterology. 1980 Jul;79(1):144–154. [PubMed] [Google Scholar]
- Winans C. S. Manometric asymmetry of the lower-esophageal high-pressure zone. Am J Dig Dis. 1977 Apr;22(4):348–354. doi: 10.1007/BF01072193. [DOI] [PubMed] [Google Scholar]
- Witzel L. Treatment of achalasia with a pneumatic dilator attached to a gastroscope. Endoscopy. 1981 Jul;13(4):176–177. doi: 10.1055/s-2007-1021677. [DOI] [PubMed] [Google Scholar]


