Abstract
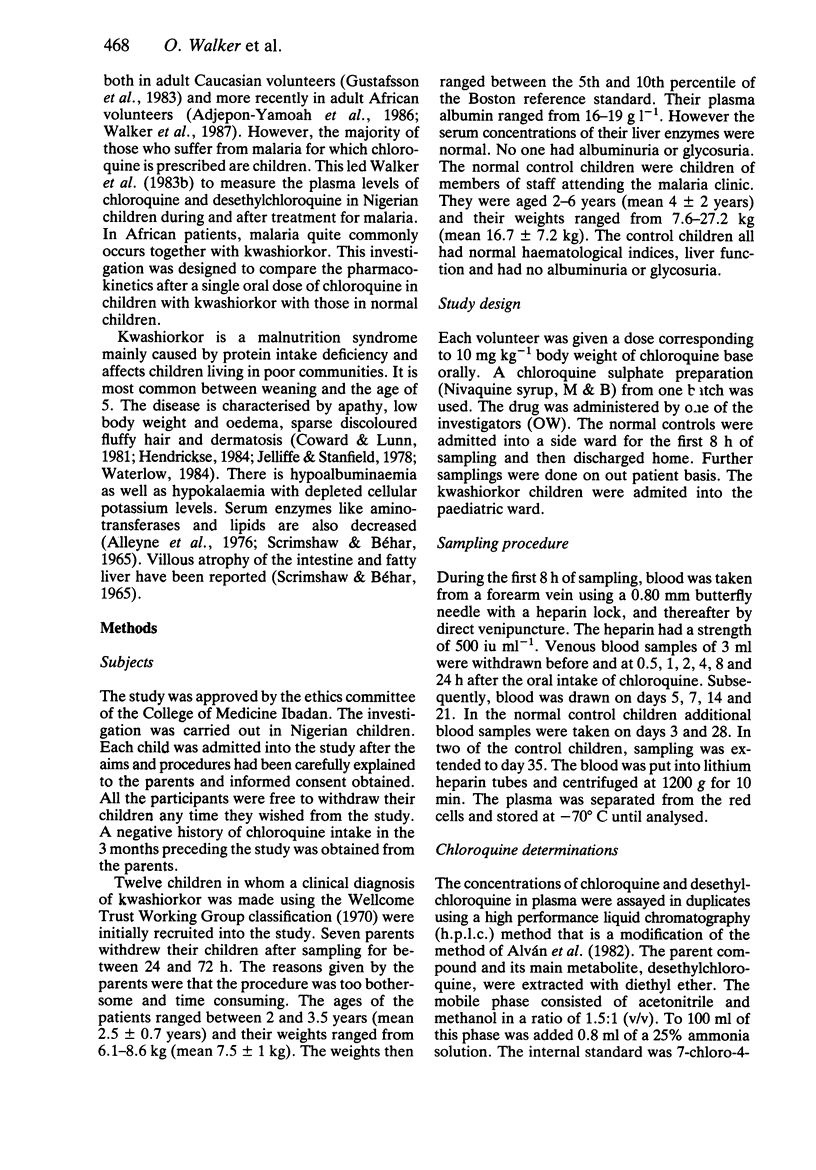
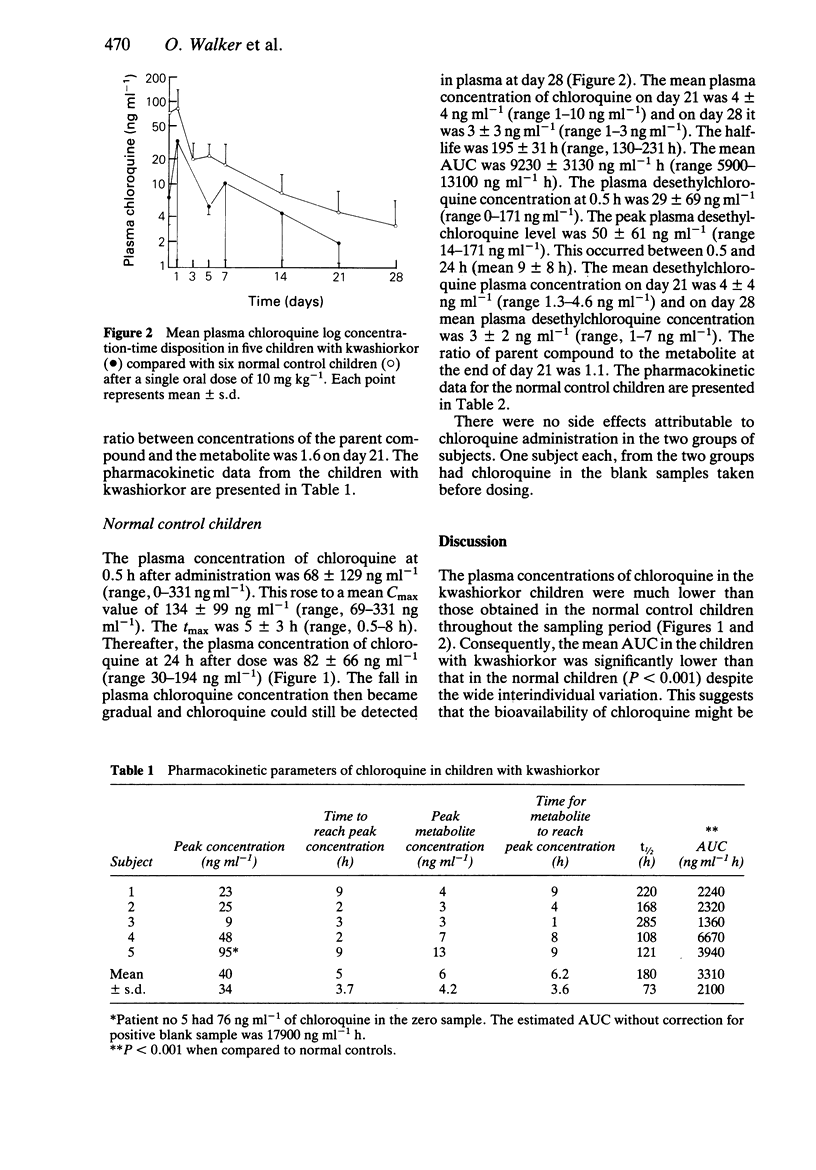
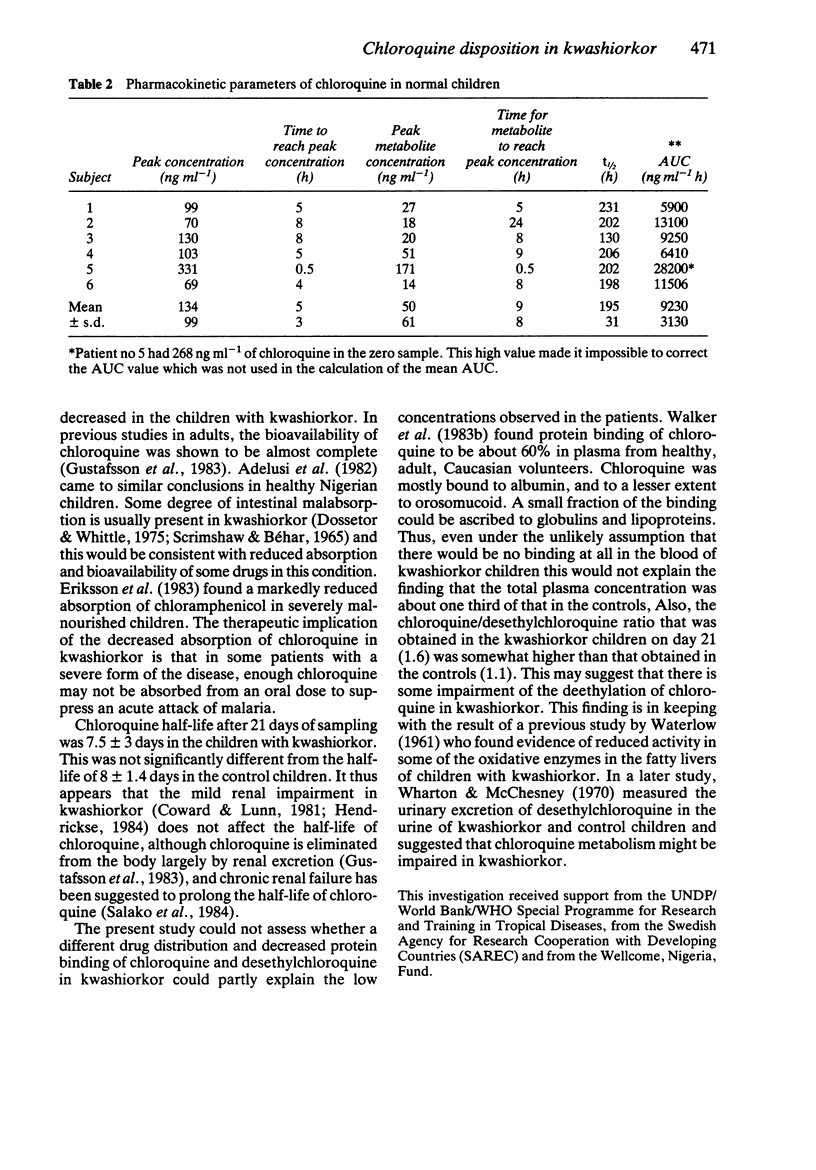
The single dose disposition of chloroquine was studied in five children with kwashiorkor and six normal control children after an oral dose of 10 mg kg-1 of chloroquine base. Plasma concentrations of chloroquine and its main metabolite were assayed by high performance liquid chromatography (h.p.l.c.). Chloroquine was detectable for up to 21 days in all the subjects. Chloroquine was detectable in all the subjects within 30 min after giving the drug except in one subject. Peak levels were reached between 0.5 and 8 h in all the subjects (with no significant difference in the tmax between the two groups of children). Peak plasma chloroquine concentrations in the children with kwashiorkor varied from 9 ng ml-1 to 95 ng ml-1 (mean 40 +/- 34 ng ml-1). Peak chloroquine concentrations in the controls varied between 69 ng ml-1 and 330 ng ml-1 (mean 134 +/- 99 ng ml-1). The mean AUC in the kwashiorkor children was significantly lower than the mean AUC in the control children (P less than 0.001). Peak plasma desethylchloroquine concentrations in the children with kwashiorkor varied between 3 and 13 ng ml-1 (mean 6 +/- 9 ng ml-1) while in the controls the concentrations varied between 14 and 170 ng ml-1 (mean 50 +/- 61 ng ml-1). There was no significant difference in the half-life of chloroquine between the kwashiorkor children and the normal control children. The possible influence of a different binding and distribution pattern of chloroquine in kwashiorkor could not be assessed in this study.(ABSTRACT TRUNCATED AT 250 WORDS)
Full text
PDF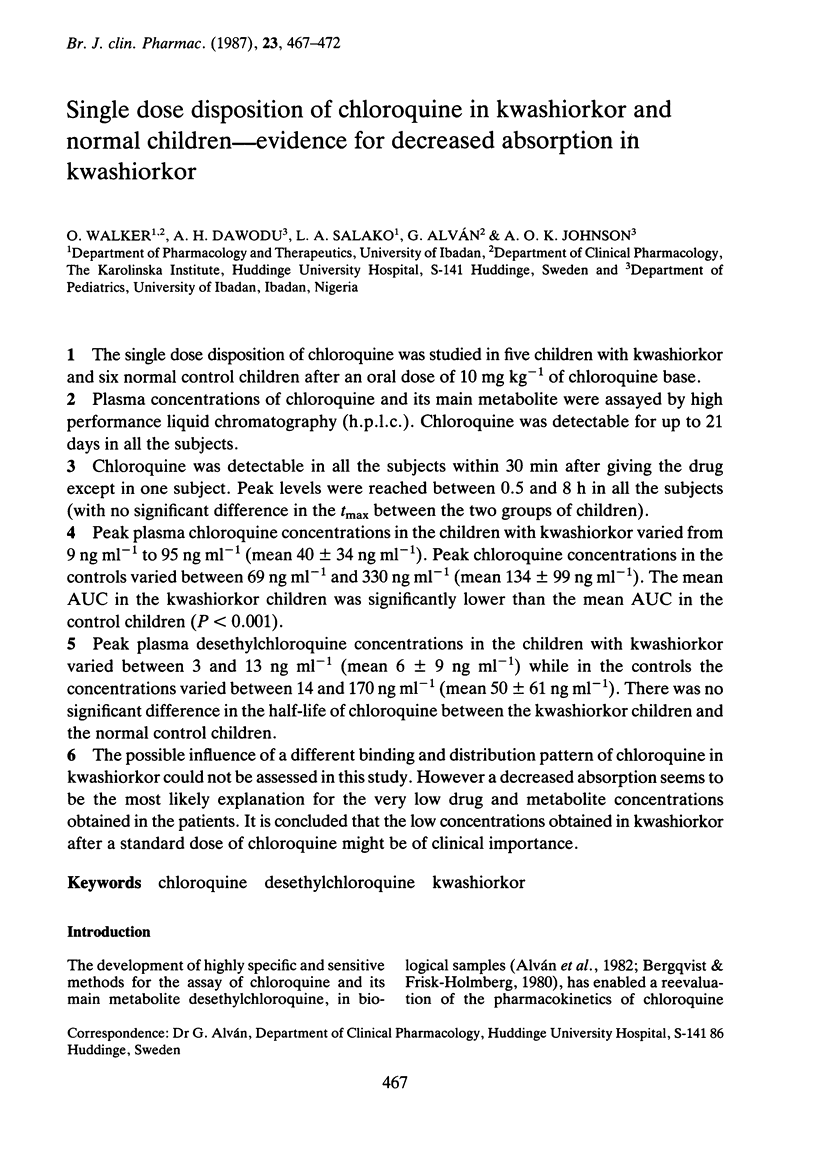
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adelusi S. A., Dawodu A. H., Salako L. A. Kinetics of the uptake and elimination of chloroquine in children with malaria. Br J Clin Pharmacol. 1982 Oct;14(4):483–487. doi: 10.1111/j.1365-2125.1982.tb02016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergqvist Y., Frisk-Holmberg M. Sensitive method for the determination of chloroquine and its metabolite desethyl-chloroquine in human plasma and urine by high-performance liquid chromatography. J Chromatogr. 1980 Nov 14;221(1):119–127. doi: 10.1016/s0378-4347(00)81013-0. [DOI] [PubMed] [Google Scholar]
- Coward W. A., Lunn P. G. The biochemistry and physiology of kwashiorkor and marasmus. Br Med Bull. 1981 Jan;37(1):19–24. doi: 10.1093/oxfordjournals.bmb.a071670. [DOI] [PubMed] [Google Scholar]
- Dossetor J. F., Whittle H. C. Protein-losing enteropathy and malabsorption in acute measles enteritis. Br Med J. 1975 Jun 14;2(5971):592–593. doi: 10.1136/bmj.2.5971.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eriksson M., Paalzow L., Bolme P., Mariam T. W. Chloramphenicol pharmacokinetics in Ethiopian children of differing nutritional status. Eur J Clin Pharmacol. 1983;24(6):819–823. doi: 10.1007/BF00607094. [DOI] [PubMed] [Google Scholar]
- Hendrickse R. G. The influence of aflatoxins on child health in the tropics with particular reference to kwashiorkor. Trans R Soc Trop Med Hyg. 1984;78(4):427–435. doi: 10.1016/0035-9203(84)90052-x. [DOI] [PubMed] [Google Scholar]
- SCRIMSHAW N. S., BEHAR M. MALNUTRITION IN UNDERDEVELOPED COUNTRIES. N Engl J Med. 1965 Jan 21;272:137–CONCL. doi: 10.1056/NEJM196501212720306. [DOI] [PubMed] [Google Scholar]
- Salako L. A., Walker O., Iyun A. O. Pharmacokinetics of chloroquine in renal insufficiency. Afr J Med Med Sci. 1984 Sep-Dec;13(3-4):177–182. [PubMed] [Google Scholar]
- Sandor P., Naranjo C. A., Khouw V., Sellers E. M. Variations in drug free fraction during alcohol withdrawal. Br J Clin Pharmacol. 1983 Apr;15(4):481–486. doi: 10.1111/j.1365-2125.1983.tb01533.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WATERLOW J. C. Oxidative phosphorylation in the livers of normal and malnourished human infants. Proc R Soc Lond B Biol Sci. 1961 Oct 17;155:96–114. doi: 10.1098/rspb.1961.0059. [DOI] [PubMed] [Google Scholar]
- Walker O., Birkett D. J., Alván G., Gustafsson L. L., Sjöqvist F. Characterization of chloroquine plasma protein binding in man. Br J Clin Pharmacol. 1983 Mar;15(3):375–377. doi: 10.1111/j.1365-2125.1983.tb01513.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker O., Dawodu A. H., Adeyokunnu A. A., Salako L. A., Alvan G. Plasma chloroquine and desethylchloroquine concentrations in children during and after chloroquine treatment for malaria. Br J Clin Pharmacol. 1983 Dec;16(6):701–705. doi: 10.1111/j.1365-2125.1983.tb02244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker O., Salako L. A., Alván G., Ericsson O., Sjöqvist F. The disposition of chloroquine in healthy Nigerians after single intravenous and oral doses. Br J Clin Pharmacol. 1987 Mar;23(3):295–301. doi: 10.1111/j.1365-2125.1987.tb03048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waterlow J. C. Kwashiorkor revisited: the pathogenesis of oedema in kwashiorkor and its significance. Trans R Soc Trop Med Hyg. 1984;78(4):436–441. doi: 10.1016/0035-9203(84)90053-1. [DOI] [PubMed] [Google Scholar]
- Wharton B. A., McChesney E. W. Chloroquine metabolism in kwashiorkor. J Trop Pediatr (1967) 1970 Sep;16(3):130–132. doi: 10.1093/tropej/16.3.130. [DOI] [PubMed] [Google Scholar]



