Abstract
This article identifies and analyses a framework for “health baskets,” the taxonomy of benefit catalogues for curative services, and the criteria for the in- or exclusion of benefits in nine EU member states (Denmark, England, France, Germany, Hungary, Italy, The Netherlands, Poland and Spain). Focusing on services of curative care, it is found that the explicitness of benefit catalogues varies largely between the countries. In the absence of explicitly defined benefit catalogues, in- and outpatient remuneration schemes have the character of benefit catalogues. The criteria for the in- or exclusion into benefit catalogues are often not transparent and (cost-)effectiveness is applied only for certain sectors. An EU-wide harmonization of benefit baskets does not seem realistic in the short or medium term as the variation in criteria and the taxonomies of benefit catalogues are large but not insurmountable. There may be scope for a European core basket.
Keywords: Health benefit plans, Health services, Health priorities, National health programs, Insurance Benefits
The Kohll/Decker judgments of the European Court of Justice and more recently the Geraets-Smits/Peerbooms cases, have demonstrated that health services can no longer be regarded as operating in isolation from other EU member states [1]. Increasingly there are flows of patients from one member state to another, sometimes due to individual choice, sometimes induced by sickness funds or even by health ministries. Such movements have the potential to stimulate competition between health care systems of the member states. However, the average volume of imported health care services in the EU has been rather small, with approx. €1.99 per person as yet (1998) [2]. One major reason for this low volume of cross country flows is the lack of accurate information as the basis for competitive behavior. Actors in one health care system, for example, sickness funds, do not have sufficient information on benefit catalogues and prices for benefits in other health care systems in order to induce in- or exports of health services. So far research has mainly focused on health services for selected indications or on the comprehensiveness of services, but information on the benefit catalogues, their taxonomy, and inclusion criteria in each country is widely lacking [3, 4, 5, 6, 7].
As one result of the project “Health Benefits and Service Costs in Europe–Health BASKET” funded by the European Commission, this article identifies and analyses the framework for health baskets, the taxonomy of benefit catalogues for curative services, and the criteria for in- or exclusion of benefits in nine EU member states (Denmark, England, France, Germany, Hungary, Italy, The Netherlands, Poland and Spain). It focuses on services of curative care, although an in-depth analysis of all other health sectors is also available as part of the project results (Reports of the EU Health BASKET project on health benefit baskets in each of the nine countries are available at: http://www.ehma.org/projects/healthbasket.asp). One of the main hypotheses of the study is that in the absence of explicit benefit catalogues, inpatient, and outpatient remuneration schemes have the character of (less explicit) benefit catalogues. After introducing the terminology and methodology of the analysis, different regulatory frameworks for the definition of the overall benefit basket in each country are compared and analyzed. Finally the taxonomy and the inclusion criteria of benefit catalogues and their substitutes for curative services are compared and analyzed.
Methodology
In general we differentiate between the terms “benefit basket” (also “benefit package”) and “benefit catalogues.” The benefit basket refers to the totality of services, activities, and goods covered by publicly funded statutory/mandatory insurance schemes (social health insurance, SHI) or by National Health Services (NHS). In contrast, we define benefit catalogues as the document(s) in which the different components of the benefit basket are stated in detail, i.e., which enumerate the services, activities, and goods in a more detailed way, listing single interventions (i.e., specific technologies). Thus a benefit basket may be further defined by one or more benefit catalogues.
Basically, the coverage of a given population for health services can be characterized in three dimensions: “breadth” as the extent of covered population, “depth” as the number and character of covered services, and “height” as the extent to which costs of the defined services are covered by prepaid financial resources as opposed to cost-sharing requirements. Services or goods which are not covered at all (i.e., with a “copayment” of 100%) are not considered to be part of the benefit basket. Figure 1 summarizes the three dimensions of a benefit basket. This article mainly focuses on the coverage of services (depth of benefit coverage) [8].
Fig. 1.
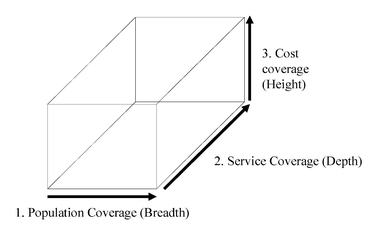
Three dimensions of coverage
An open questionnaire was developed to explore the different benefit baskets and their underlying benefit catalogues of the participating nine countries, and this served as guide in compiling standardized country reports. To scan the different health systems in search for existing benefit catalogues we followed the framework of functional categories of “health care services and goods” proposed by the OECD in its “System of Health Accounts” (Table 1) [9]. As an initial step the researchers in each country were asked to identify the decision-making processes on the benefit basket as a whole in their country. As a second step they were asked to provide a detailed description of the existing benefit catalogues for each functional category, the actors involved in decision making, and the decision criteria.
Table 1.
Framework of health care functional categories, system of health accounts
| HC.1 Services of curative care |
| HC.1.1 In-patient curative care |
| HC.1.2 Day cases of curative care |
| HC.1.3 Out-patient care |
| HC.1.3.1 Basic medical and diagnostic services (primary health care) |
| HC.1.3.2 Out-patient dental care |
| HC.1.3.3 All other specialized care |
| HC.1.3.9 All other out-patient curative care |
| HC.1.4 Services of curative home care |
| HC.2 Services of rehabilitative care |
| HC.2.1 In-patient rehabilitative care |
| HC.2.2 Day cases of rehabilitative care |
| HC.2.3 Out-patient rehabilitative care |
| HC.2.4 Services of rehabilitative home care |
| HC.3 Services of long-term nursing care |
| HC.3.1 In-patient long-term nursing care |
| HC.3.2 Day cases of long-term nursing care |
| HC.3.3 Long-term nursing care at home |
| HC.4 Ancillary services to health care |
| HC.4.1 Clinical laboratory |
| HC.4.2 Diagnostic imaging |
| HC.4.3 Patient transport and emergency rescue |
| HC.4.9 All other miscellaneous services |
| HC.5 Medical goods dispensed to out-patients |
| HC.5.1 Pharmaceuticals and other medical non-durables |
| HC.5.1.1 Prescription medicines |
| HC.5.1.2 Over-the-counter medicines |
| HC.5.2 Therapeutic appliances and other medical durables |
| HC.5.2.1 Glasses and vision products |
| HC.5.2.2 Orthopedic appliances and other prosthetics |
| HC.5.2.3 Hearing aids |
| HC.5.2.4 Medico-technical devices |
| HC.5.2.9 All other miscellaneous medical durables |
| HC.6 Prevention and public health services |
| HC.6.1 Maternal and child health; family planning and counseling |
| HC.6.2 School health services |
| HC.6.3 Prevention of communicable diseases |
| HC.6.4 Prevention of non-communicable diseases |
| HC.6.5 Occupational health care |
| HC.6.9 All other miscellaneous public health services |
Establishing and shaping health baskets
A generic pattern of establishing and shaping health baskets is found in most of the countries consisting of two levels. At the higher level, legislation passed by the national parliaments (sometimes even rooted in the country’s constitution, e.g., Poland [10]) establishes the general framework by enumerating the areas of health care, often similar to the OECD health care categories, included in the benefit basket. At the lower level, the benefit basket is further shaped by specifying certain procedures provided within each area of health care as part of the benefit catalogues. These catalogues contain recommendations as well as explicit in- or exclusions of services. The extent to and the way in which this shaping actually takes place varies considerably from country to country and within each country from sector to sector of health care. There are several ways used to establish benefit catalogues such as legislations passed by central or regional parliaments, decrees issued by national or regional governments, directives issued by self-governing bodies or by national and/or local authorities, and other documents considered as “quasilaws” (rules without legal character, e.g., clinical guidelines).
In all countries studied a general definition of a benefit basket could be identified at the higher level. Depending on the organization of the system (NHS or SHI), the logic underlying the general definition of the benefit basket differs. In NHS countries the definition of a benefit basket refers to the specification of the duties and obligations of the purchasing organization (regional health authorities), and in SHI countries the issue of the benefit basket is more related to the specification of entitlements of the insured persons. However, it cannot be said that either NHS or SHI countries generally define their benefits more explicitly than the other.
In most NHS countries a coherent legislation contains a list of the areas of care to be provided by the respective NHS, including “regional health services” as part of the benefit basket of regions in decentralized NHS systems, for example, Italy and Spain. Denmark represents an exception from this as the legislation consists of separate acts concerning the categories of hospital, primary and long-term care, and pharmaceuticals [11]. The level of explicitness varies considerably from country to country. The vaguest definition of a benefit basket may be that of the NHS Foundation Act (1946) in England and related posterior documents, where the Secretary of State for Health is legally required to provide services “to such extent as he considers necessary to meet all reasonable requirements” [12]. The responsibility for making available general practitioner, dental, ophthalmic, and pharmaceutical services lay until 2003 with health authorities and since then with Primary Care Trusts. In contrast, the framework of the Italian and Spanish benefit baskets, each of which was established in recently implemented legal documents, is structured in more detail [13, 14]. Common to all four, however, is the differentiation between hospital care and primary care, including specialist outpatient services, as well as preventive or health promotion services.
The level of explicitness is not only heterogeneous across different countries, but also within the same country. For instance, in Spain some areas of health care may be further shaped by mentioning specific services or in some cases even specific procedures or technologies being in- or excluded from the benefit basket. Thus the definition of the benefit basket within NHS countries does not always follow a systematic approach of going into further detail. It rather addresses shortcomings perceived by decision makers of each health care system, not necessarily being based on evidence. Concerning the origin of more detailed benefit catalogues some similarities are observed across countries with similar organization of the health care system or with similar organizational demands (i.e., the need to reimburse providers in free practice). In the two countries with regionalized NHS, Italy and Spain, the motivation for defining a detailed benefit catalogue is to be seen in the autonomous status of regions. The national benefit basket can be regarded as a minimum basket of health services that must be provided by the regional health authorities. Therefore the regions in both countries are free to offer additional services not included in the national benefit basket.
Health baskets in SHI countries stem from two different roots. On the one hand, SHI countries formulate the basket as an entitlement for persons insured under the respective statutory health insurance schemes. The main reason for this lies in the fact that SHI schemes have evolved from fragmented voluntary/statutory health insurance schemes not covering the whole population and only covering certain services, for example, sickness benefits. Statutory health insurance in Germany as well as in The Netherlands does still not cover the whole population [15, 16]. Therefore in SHI countries the health basket is also used to indicate the boundaries between those insured under the statutory health insurance and those insured under other schemes. The second root are fee catalogues which were originally more prevalent in SHI than in NHS countries due to the frequently used fee-for-service reimbursement system, at least in ambulatory specialist care.
Another common characteristic of decision making on health baskets in most SHI countries is the role of the self-governing institutions. Within a general framework stipulated by laws, self-governing institutions (e.g., sickness funds, physician associations) specify the rules to explicit benefit catalogues or remuneration schemes with the character of benefit catalogues, limiting the scope of service provision.
As observed in NHS countries, the level of explicitness also varies considerably among SHI countries. Poland has by far the most explicit benefit basket, which is even rooted in the constitution. Different legal acts define benefit catalogues specifying detailed procedures or even technologies being provided. At the other extreme, Germany probably has the vaguest legal definition of the benefit basket among the SHI countries, with the Social Code Book as a general framework. For instance, inpatient services in Germany are limited to only a certain extent by the diagnosis-related group (DRG) reimbursement system because they can be provided unless they are explicitly excluded by directives [17]. There is a trend in all SHI countries towards more explicit benefit baskets. In The Netherlands a system of diagnosis-procedure combinations has been introduced in 2005 defining procedures provided in inpatient care and by specialists in outpatient care [18]. In France a similar list is currently being prepared, while Germany and Hungary recently updated their outpatient remuneration schemes specifying certain procedures that are reimbursed by the statutory health insurance [17, 19].
Definition of benefit catalogues for curative services
Benefit catalogues for inpatient care
As in other sectors of the health care system, the provided inpatient services can either be listed as procedures being part of an explicit benefit catalogue or indirectly determined by grouping systems that serve remuneration purposes, for example, DRGs. France, Poland, and Spain have defined explicit benefit catalogues, grouped according to medical specialties, for inpatient services listing detailed procedures serving as positive lists [10, 14, 20]. While there are clear decision criteria for the inclusion of benefits in the benefit catalogue in France and Spain, no transparent criteria are applied in Poland. In all other countries DRG and other grouping systems serve as a tool for estimating resource consumption supporting budget assignations or providing the basis for remuneration. In general, they classify a single episode of care according to main diagnoses, comorbidities and main surgical interventions into one of a limited number of groups. Thus each classified episode is assumed to require more or less homogeneous resource consumption, independently of whether exactly the same items (e.g., drugs, diagnostics) are used. As, finally, monetary values are attached to the different groups, the use of drugs, diagnostics etc. is confined to the given monetary scope of each group.
In our study four countries have introduced DRG systems: Italy [13], Germany [17], Hungary [19], and Denmark [11]. England and The Netherlands have DRG-like grouping systems called, respectively, health care resource groups and Diagnose Behandeling Combinaties. The main features of the DRG and other grouping systems are very similar (Table 2) [12, 18]. In each country the groups have been developed from data collected on resource consumption, clustering in homogeneous resource consumption groups. The observed variability in the number of classified groups in each system may be explained by the different criteria used to classify them (Table 2). Another possible explanation is the creation of additional groups in certain countries to increase the scope for the use of new innovative technologies (devices, procedures, and even drugs theoretically) which are considered to be worth the promotion (i.e., because of higher efficacy). This has been the case in Italy, where the regional health authority of Lombardy added three new DRGs to its system in order to specifically consider the use of drug-eluting stents and to encourage its utilisation [13].
Table 2.
Inpatient benefit catalogues or substitutes
| Country | Name of taxonomy, year of introduction | Applied geographical area | Taxonomy (and grouping criteria) | Actors involved in decision making | Criteria for in-/ exclusion of benefits |
|---|---|---|---|---|---|
| Denmark | DRG system (Nordic-DRG); 1998 | National | 25 MDC (anatomical, etiological, other) with 589 DRG, special category for chemotherapy and radiotherapy. Grouping criteria: main diagnosis, procedures, sex, age, cause of discharge | Legislation at the national level (law, general framework) | Need, budget |
| Ministry for the Interior and Health (approval) | |||||
| National Board of Health (DRG catalogue) | |||||
| County level (budgeting, hospital plan) | |||||
| Clinicians (priority setting in hospital) | |||||
| France | Common Classification of Medical Procedures (CCAM); 2005 | National | CCAM lists reimbursable and excluded medical procedures thus being a positive and negative list; Grouping criteria: anatomic classification, medical specialties | National level (law, general framework) | Effectiveness, safety |
| Ministry of Health (approval) | |||||
| National Union of Health Insurance Funds (in- and exclusion of services) | |||||
| High Health Authority (advisory body on in- and exclusion of services) | |||||
| Germany | G-DRG system (based on AR-DRG 4.1); stepwise 2003–2009 | National | 25 MDC (anatomical/ etiological/ other) with 876 DRG, 71 extra remunerations for special services (in 2005). Grouping criteria: main diagnosis, procedures, age, comorbidity, cause of discharge | Legislation at the national level (law, general framework) | Services can be provided as long as they are not explicitly excluded. Adequate, expedient and cost-effective |
| Ministry of Health (approval) | |||||
| Federal Joint Committee (exclusion of benefits) | |||||
| Institute for Hospital Reimbursement with assistance of the Committee of on Hospital | |||||
| Payment (DRG catalogue) | |||||
| Clinicians (priority setting in hospital) | |||||
| Hungary | DRG system (US-DRG); 1993 | National | 26 MDC (anatomical, etiological, other) with 786 DRG. Grouping criteria: main diagnosis, procedures, age, comorbidity | Legislation at the national level (law, general framework, budgeting) | Costs, effectiveness |
| Ministry of Welfare, Health division (DRG catalogue) | |||||
| National Health Insurance Fund | |||||
| Administration, especially (prepares decisions) | |||||
| Clinicians (priority setting in hospitals) | |||||
| Italy | DRG system (HCFA no. 10); 1995 | National reference list with regional differences | 23 MDC (anatomical, etiological, other) with 489 to 506 DRG, exceptional DRGs (e.g. liver and bone marrow transplantation). Grouping criteria: main diagnosis, procedures, age, comorbidity, cause of discharge | Legislation at the national level (law, general framework) | Effectiveness, costs |
| Central level (national DRG catalogue) | |||||
| Regional level (redefines DRG catalogue, sets tariffs) | |||||
| Clinicians (priority setting in hospitals) | |||||
| The Netherlands | Diagnose Behandeling Combinaties (DBC) (DRG-like system); Jan. 2005 | National | 111,527 procedures regarding diagnosis and therapy (DBCs) are combined to 641 product groups. DBCs are on three different lists determining the status for tariff negotiations or excluding DBCs from the benefit package. Grouping criteria: medical specialty, product group | Legislation at the national level (law, general framework) | Costs, effectiveness, |
| Ministry of Health (decrees) | |||||
| DBC Maintenance Organization (DBC system) | |||||
| Clinicians (priority setting in hospitals) | |||||
| Poland | Governmental decrees and catalogue of benefits | National | Catalogue lists all services covered under social health insurance scheme; services are linked to the respective regulation/law. Grouping criteria: area of care (e.g., hospital care), medical specialty | Legislation at the national level (law, general framework) | / |
| Ministry of Health (regulations decrees) | |||||
| National Health Fund (catalogue) | |||||
| Spain | Royal Decree 63/1995 / Law 16/2003 on cohesion and qualtiy of the National Health System | National with regional differences | Services are listed explicitly in decree. In some cases services are restricted to specific patient groups. Grouping criteria: area of care, medical specialty | Legislation at the national level (law, general framework) | Safety, efficacy, efficiency |
| Federal Government (decree) | |||||
| Inter-territorial Council and Council of the State (inclusion of new benefits) | |||||
| Clinicians (provision of services relating to entitlements defined by decree) | |||||
| England | Health care resource group (DRG-like system); stepwise 2004–2009 | National | In April 2004 there were only 48 HRGs in use. Grouping criteria: diagnosis, complexity, procedure | Legislation at the national level (law, general framework) | Costs, budget |
| Ministry of Health (catalogue) | |||||
| Primary Care Trusts (negotiate with providers on quantity and tariffs) |
The fact that specific procedures and technologies drive the development of DRG systems confirms our hypothesis that they serve as some kind of benefit catalogues. Technologies specifically mentioned in certain groups may not be used if less resource consuming alternatives are available. In this way a less specific DRG system may act as a hidden negative list of technologies which de facto are not available for beneficiaries of publicly financed care since the monetary value assigned to certain groups does not cover the actual resource consumption associated with its use. Furthermore, in most applied grouping systems certain groups (e.g., in DRG systems so-called surgical DRGs) are even defined by specific procedures or specific technologies, such as drug-eluting stents. These groups can therefore be considered as a kind of explicitly defined benefits, similar to a positive list. Thus it can be assumed that grouping systems are applied as substitutes for benefit catalogues, containing incentives to limit the provision of benefits for those services not being explicitly mentioned.
Benefit catalogues for outpatient care
In the outpatient sector benefit catalogues are, again, often replaced by grouping systems serving remuneration purposes. Although they generally seem to be more explicit than the inpatient catalogues, the explicitness varies even more than in the inpatient sector (Table 3). These different degrees of explicitness are due mainly to the applied remuneration schemes in each country. If physicians receive fixed budgets or capitations, the benefit “catalogue” (i.e., the procedures that they can offer) is indirectly restricted by the amount of money allocated to them. Therefore in these countries the benefit package for outpatient care is regulated rather implicitly through decrees issued by national or regional health authorities describing the obligation of physicians to provide those benefits that are considered necessary. Examples of these kind of implicit benefit catalogues are the “Health Insurance Treatment and Services Decree” for care provided by general practitioners in The Netherlands and the “General Medical Services Contract” in England. These decrees do not mention specific procedures, although in the case of The Netherlands, the general practitioners’ association, the Landelijke Huisartsen Vereniging, defined a basic general practitioner benefit package in the 1980s [21].
Table 3.
Outpatient benefit catalogues or substitutes
| Country | Name of taxonomy | Applied geographical area | Taxonomy (and grouping criteria) | Actors involved in decision making | Criteria for in-/exclusion of benefits | Benefits, procedures explicitly excluded |
|---|---|---|---|---|---|---|
| Denmark | Health Care Reimbursement Scheme Fee Schedule | National | Services are grouped according to medical specialty and for GPs additionally in basic, supplementary, laboratory and miscellaneous services. Each service has an item number. It is referred to the respective legislation decree specifying the benefit, certain goods, procedures or in rare cases indications | National level (law, general framework) | Need | Alternative care |
| Ministry for the Interior and Health (approval) | ||||||
| Counties (budgeting, health plan) | ||||||
| Health care Reimbursement Negotiating Committee and health professional associations (negotiate catalogue) | ||||||
| France | Common Classification of Medical Procedures (CCAM) | National | Lists all medical procedures reimbursable and excluded. Grouping criteria: anatomic classification, medical specialties | National level (law, general framework) | Effectiveness, safety | Spa treatments; cosmetic surgery |
| Ministry of Health (approval) | ||||||
| National Union of Health Insurance Funds (in- and exclusion of services) | ||||||
| High Health Authority (advisory body on in- and exclusion of services) | ||||||
| Germany | SHI-EBM, SHI-BEMA, SHI-BEL-II | National | Services are grouped according to the medical specialty allowed to provide the service. Each service is assigned a numeric code in accordance with the subjection of the catalogue | National level (law, general framework) | Diagnostic and therapeutic expedience, medical necessity and cost-effectiveness | Orthopedic services after the age of 18 years |
| Federal Joint Committee (approval of new benefits) | ||||||
| Valuation Committee (negotiates EBM) | ||||||
| Dental Valuation Committee (negotiates BEMA, BEL-II) | ||||||
| Hungary | Governmental decrees and reimbursement catalogues | National | Similar services are listed in groups. Governmental decrees relate to different areas of care (e.g., dental care, specialist services). Items in reimbursement catalogues are listed with the respective ICPM code and a point value | Legislation at the national level (law, general framework, budgeting) | Costs, effectiveness | – |
| Ministry of Welfare (decrees, approval) | ||||||
| National Health Insurance Fund | ||||||
| Administration, especially (prepares decisions) | ||||||
| Payment Codes Updating Committee (reimbursement catalogues) | ||||||
| Italy | National contract for primary care; decree on specialist outpatient services | National benefit package, regions include additional services | Contract for primary care describes obligations of GP. Individual services are not further itemized. Decree on specialist outpatient services lists services in three sections: available, availability restricted to specific indications, excluded | Government at national level (sets decree, negotiates contract) | Effectiveness, costs | Nonconventional treatments (e.g., acupuncture, phytotherapy); vaccination for traveling purposes |
| Representatives of GPs (negotiate contract) | ||||||
| Ministry of Health (transfers contract into law) | ||||||
| Government at regional level (negotiates additional contracts) | ||||||
| The Netherlands | Health Insurance (Treatment and Services) Decree; Diagnose Behandeling Combinaties (DBC; DRG-like system); Jan. 2005 | National | GP services are regulated in generic terms only by decree, DBC catalogue (111,527 DBCs) combine information on diagnosis and treatment for medical specialists. DBCs are on three different lists determining the status for tariff negotiations or excluding DBCs from the benefit package. Grouping criteria: medical specialty, product group | Legislation at the national level (law, general framework) | Costs, effectiveness | – |
| Ministry of Health (decrees) | ||||||
| DBC-Maintenance Organization (DBC-System) | ||||||
| Physicians (priority setting) | ||||||
| Poland | Governmental decrees and catalogue of benefits | National | Catalogue lists all services covered under social health insurance scheme. Services are linked to the respective regulation/law. Grouping criteria: area of care, medical specialty | Legislation at the national level (law, general framework) | – | Vaccination; acupuncture, unless part of chronic pain management |
| Ministry of Health (regulations) | ||||||
| National Health Fund (catalogue) | ||||||
| Spain | Royal Decree 63/1995 | National with regional differences | Services are listed explicitly in decree. In some cases, services are restricted to specific patient groups. Decree lists services in 5 areas of care (e.g., primary care, specialized care, pharmaceutical care) which are further subdivided. | Legislation at the national level (law, general framework) | Safety, efficacy, efficiency | Cosmetic surgery (transplantation of hair and nails); sex change |
| Federal Government (decree) | ||||||
| Inter-territorial Council and Council of the State (inclusion of new benefits) | ||||||
| Clinicians (provision of services relating to entitlements defined by decree) | ||||||
| England | National Service Framework | National | Health Resource Groups are linked to procedures. Currently only 48 HRGs are in use. Guidelines recommend services to be used on certain indications | Legislator at national level (law, general framework) | Need, effectiveness | Cosmetic dental treatments |
| General Medical Services Contract | National, with possible variation at PCT-level | NHS Confederation and General Practitioners Committee (negotiate contract) | Need, costs | |||
| Clinical Guidelines | National | Primary Care Trusts (PCT) (negotiate additional contracts) | Need, costs, effectiveness | |||
| NICE (clinical guidelines) |
In contrast, the countries remunerating providers on the basis of fee-for-service schemes need detailed lists of procedures or at least of service complexes (aggregated multiple procedures) to be able to negotiate on price and/or volumes. These lists can therefore be interpreted as substitutes for benefit catalogues, as physicians are usually reimbursed only for those items listed. The explicitness of these lists differs largely. Some countries issue detailed lists of all procedures to be performed by physicians (e.g. the “Common Classification of Medical Procedures” in France [20]) while other countries list service complexes making physicians responsible for the priority setting within such a service complex (e.g., SHI-EBM or SHI-BEMA in Germany [17] and the Health Care Reimbursement Scheme Fee Schedule in Denmark [11]).
Interestingly, taxonomy and structure are very similar in all countries. For example, in Denmark, France, Germany, Hungary, and The Netherlands services are grouped according to medical specialty. Certain outpatient benefits are also linked to indications or special patient groups in Poland and Spain [10, 14]. The high degree of explicitness regarding the definition of the benefit package is also underlined by the diverse lists of excluded services, common in all countries. Exclusion practices vary from issuing negative lists (e.g., Spain, Poland) and directives of self-governmental institutions with the character of negative lists (e.g., Germany) to excluded services within the framework of the national law (e.g., England). However, most countries exclude similar benefits such as cosmetic surgery (if not closely linked to certain treatments), vaccination for nonstandard diseases (e.g., for traveling purposes), and certain nonconventional treatments (e.g., acupuncture). Benefits of dental care are either restricted to specific treatment methods or age groups (e.g., Germany).
Discussion
The analysis of benefits defined in the countries under study reveals that there is a clear trend towards a more explicit definition of benefit baskets and their benefit catalogues. Those countries which recently introduced new health care legislations, such as Italy, Poland, and Spain, have more explicitly defined benefit catalogues. Other countries with older health care legislations, for example, the UK’s English-NHS Foundation Act (1946) and Germany’s Social Code Book (1988) have rather implicitly defined benefit catalogues, but increasingly work with negative lists, based on evidence provided by independent institutions such as the Englisch NICE and the German Institute for Quality and Efficiency (IQWiG) [12, 17]. Apart from negative lists remuneration schemes, for example, DRGs and procedures catalogues used for grouping are more and more used as benefit catalogues. These developments indicate that all included countries move towards a more explicit definition of benefit catalogues. Explicitly defined benefit catalogues, however, require clear and transparent decision criteria for the in- or exclusion of benefits.
Most countries officially state that (cost)-effectiveness is an important decision criteria. However, further inquiries often demonstrate that there is no rational process of reviewing the available evidence on specific procedures or technologies [22]. In reality the decision-making process is rather guided by lobbying activities of certain actors in the system. Especially those countries with very explicit benefit baskets, e.g. Poland, often lack transparency of decision criteria [10]. In contrast to this, countries with rather implicitly defined benefit baskets, such as England and Germany, define very transparent criteria for benefit exclusion, although lists with excluded services are minor compared to explicitly oriented countries. In addition, criteria such as cost-effectiveness and even effectiveness are often restricted to one or few sectors of the health care system, for example, pharmaceuticals or medical devices, and are not generalizable to all products or services [23]. In general the transparency of decision criteria must be improved in all countries in order to achieve accountability for all actors of the health care systems as well as consumers.
This contribution, as well as the overall EU Health BASKET project, provides useful information for health care providers and industrial companies willing to invest in EU countries but do not have the necessary information on benefit baskets and their underlying decision-making processes. However, to improve the environment for investments and to provide confidence for foreign investors, public documents should be regularly prepared by each country giving a transparent overview of the health baskets and the decision-making criteria.
The information provided will be beneficial especially to decision makers at all levels of health policy enabling them to compare different approaches of benefit definitions in order to develop their own position. The need for benchmarking will grow in line with the further development of cross boarder flows and the establishment of coherent benchmark criteria as part of the “Open Method of Coordination” initiated by EU policy makers [24, 25]. However, the project results also demonstrate that a harmonization of health baskets of EU countries, which in the view of certain decision makers could be the final stage after identifying best practice in benchmarking, is not realistic in the short or medium term since the definitions of benefit baskets vary substantially. Additionally, as shown in the cases of Italy and Spain, especially in NHS countries there is rather a trend towards more decentralization of decision making on benefits, delegating to regions the autonomy to offer certain benefits in addition to nationally defined health baskets [26, 27]. On the other hand, this could also mean that in future a minimum basket of health benefits may be defined by all countries on the national level, which could be harmonized on the EU level at a certain stage due to systems’ competition as a result of increased cross-border flows. Beyond this minimum basket, there could be regional variations reflecting differences in wealth and of preferences.
Acknowledgements
The results presented here are based on the project “Health Benefits and Service Costs in Europe–HealthBASKET” which is funded by the European Commission within the Sixth Framework Research Programme (grant no. SP21-CT-2004-501588). The authors thank all project partners in the nine European countries who contributed to this analysis with their comprehensive reports. We are also indebted to the European Health Management Association (EHMA) responsible for the coordination of the project.
References
- 1.Busse R, Wismar M, Berman P (2002) The European Union and health services—the impact of the single European market on member states. IOS: Amsterdam
- 2.Palm W, Nickless J, Lewalle H, Coheur A (2000) Implications of recent jurispuridence on the co-ordination of health care protection systems. General report produced for the Directorate-General for Employment and Social Affairs of the European Commission. Association Internationale de la Mutualité: Brussels
- 3.Johnson S, Kuhlmann R, and the EPCAT Group (2000) The European Service Mapping Schedule (ESMS): development of an instrument for the description and classification of mental health services. Acta Psychiatr Scand 102:14–23 [PubMed]
- 4.Kupsch S, Kern A, Klas C, Kressin B, Vienonen M, Beske F (2000) Health service provision on a microcosmic level—an international comparison; results of a WHO/IGSF survey in 15 European countries. Institute for Health Systems Research: Kiel
- 5.OECD (2002) Measuring up: improving health system performance in OECD countries. Proceedings of the Ottawa Conference. OECD: Paris
- 6.Polikowski M, Santos-Eggimann B (2002) How comprehensive are the basic packages of health services? An international comparison of six health insurance systems. J Health Serv Res Policy 7:133–142 [DOI] [PubMed]
- 7.Henke K-D, Schreyögg J (2004) Towards sustainable health care systems—strategies in health insurance schemes in France, Germany, Japan and The Netherlands. International Social Security Association: Geneva
- 8.Busse R, Schreyögg J, Guericke CA (2005) Challenges of health financing in high income countries. In Schieber G (ed) Health financing revisited. World Bank: Washington (in press)
- 9.OECD (2000) A system of health accounts, version 1.0. OECD: Paris
- 10.Kozierkiewicz A, Trabka W, Romaszewski A, Krzysztof G, Gilewski D (2005) Definition of the “Health Basket” in Poland. Eur J Health Econ (s10198-005-320-3) [DOI] [PMC free article] [PubMed]
- 11.Bilde L, Ankjaer-Jensen A, Danneskiold-Samsoe B (2005) The “Health Benefit Basket” in Denmarks: a description of entitlements, actors and decision-making processes in the curative health sector. Eur J Health Econ (s10198-005-313-2) [DOI] [PMC free article] [PubMed]
- 12.Mason A (2005) Does the United Kingdom’s NHS have a “Health Benefit Basket”? Eur J Health Econ (s10198-005-314-1) [DOI] [PMC free article] [PubMed]
- 13.Torbica A, Fattore G (2005) The “Essential Levels of Care” in Italy: when being explicit serves the devolution of powers. Eur J Health Econ (s10198-005-318-y) [DOI] [PMC free article] [PubMed]
- 14.Planas-Miret I, Tur-Prats A, Puig-Junoy J (2005) Spanish health benefits for services of curative care. Eur J Health Econ (s10198-005-321-2) [DOI] [PMC free article] [PubMed]
- 15.Busse R, Riesberg A (2005) Health care systems in transition: Germany. WHO Regional Office for Europe on behalf of the European Observatory on Health Systems and Policies: Copenhagen
- 16.Den Exter A, Hermany H, Dosljak M, Busse R, van Ginneken E, Schreyögg J (2004) Health care systems in transition: The Netherlands. WHO Regional Office for Europe on behalf of the European Observatory on Health Systems and Policies: Copenhagen
- 17.Busse R, Stargardt T, Schreyögg J (2005) Determining the “Health Benefits Basket” of the Statutory Health Insurance scheme in Germany: methodologies and criteria. Eur J Health Econ (s10198-005-316-z) [DOI] [PMC free article] [PubMed]
- 18.Stolk EA, Rutten FFH (2005) The “Health Benefit Basket” in the Netherlands. Eur J Health Econ (s10198-005-319-0) [DOI] [PMC free article] [PubMed]
- 19.Gaal P (2005) Benefits and entitlements in the Hungarian health care system. Eur J Health Econ (s10198-005-317-y) [DOI] [PMC free article] [PubMed]
- 20.Bellanger MM, Cherilova V, Paris V (2005) The “Health Benefit Basket” in France. Eur J Health Econ (s10198-005-315-0) [DOI] [PMC free article] [PubMed]
- 21.Groenewegen P, Greß S (2004) Der Hausarzt in den Niederlanden—Auslaufmodell oder Reformperspektive in der GKV. Jahrb Krit Med 38:73–91
- 22.Busse R, Orvain J, Velasco M, Perleth M, Drummond M, Gürtner F, Jorgensen T, Jovell A, Malone J, Rüther A, Wild C (2002) Best practice in undertaking and reporting HTA. Int J Technol Assess Health Care 18:361–422 [DOI] [PubMed]
- 23.Gibis B, Koch P, Bultman J (2004) Shifting criteria for benefit decisions. In: Saltman RB, Busse R, Figueras J (eds) Social health insurance systems in western Europe. Open University Press: Maidenhead, pp 189–206
- 24.Henke K-D (2002) Soft co-ordination versus hard rules in European economic policy—does co-ordination lead to a new direction for a common European economic policy? Diskussionspapiere zu Staat und Wirtschaft 34/2002. Europäisches Zentrum für Staatswissenschaften und Staatspraxis: Berlin
- 25.Wismar M Busse R (2002) Scenarios on the future of healthcare in Europe. In: Busse R, Wismar M, Berman P (eds) The European Union and health services—the impact of the single European market on member states. IOS: Amsterdam, pp 261–272
- 26.Hurly J, Birch S, Eyles J (1995) Geographically decentralized planning and management in health care: some informational issues and their implications for efficiency. Soc Sci Med 41:3–11 [DOI] [PubMed]
- 27.World Bank (2001) Decentralization and governance: does decentralization improve public service delivery? No. 55. World Bank: Washington


