Multiple sclerosis is the most common disabling neurological disease in young adults. Recent advances in understanding the underlying mechanisms and the development of new therapies have increased hope for doctors and their patients. New therapies are available and many other agents are undergoing clinical trials. New information does reveal some disturbing aspects of the disease however. Evidence from several sources suggests that the disease is present long before the first symptom. The disease is also more widespread and continuous than previously thought, with changes in grey as well as white matter and changes in normal appearing white matter. Multiple sclerosis has long been regarded as a demyelinating disease, but evidence now suggests widespread damage to axons that may be more closely correlated with progression of disability. Better understanding of the underlying mechanisms of the disease is allowing more focused development of new therapies.
Sources and selection criteria
This review is based on the conclusions of recent randomised clinical trials, the 15 Cochrane reviews of multiple sclerosis therapy, and guidelines of the American Academy of Neurology.
Diagnosis
Since the early 1980s the Poser criteria was used to classify multiple sclerosis. This relied on evidence of at least two relapses typical of multiple sclerosis and evidence of involvement of white matter in more than one site in the central nervous system, the concept of “lesions scattered in time and space.” A new system of classification, the McDonald criteria (see bmj.com), incorporates clinical and laboratory elements, allowing an earlier confirmation of the diagnosis and thus enabling earlier decisions about starting disease modifying therapies.1,2 Multiple sclerosis is a clinical diagnosis on the basis of two episodes involving two or more areas of the central nervous system over time, but the McDonald criteria incorporate magnetic resonance imaging to demonstrate multiple areas of involvement and also involvement over time with the appearance of new enhancing lesions.
Types of multiple sclerosis
About 85% of patients with multiple sclerosis present with the relapsing-remitting form, comprising episodic relapses and remissions that may be partial or complete. A first attack is categorised as clinically isolated syndrome. After many years most of these patients will enter a phase of progression with or without attacks, called secondary progressive multiple sclerosis. About 15% of patients present without relapses but show a slowly progressive pattern called primary progressive multiple sclerosis. A few of them may later relapse, called progressive-relapsing multiple sclerosis. Fifteen per cent of patients with relapsing-remitting multiple sclerosis have a mild course with minimal disability after 15 years, called benign multiple sclerosis.3 Classification of multiple sclerosis is important as all the disease modifying drugs have shown benefit only in the relapsing-remitting type and no benefit in the primary progressive form.
Summary points
Multiple sclerosis was thought to be an intermittent disease with inflammatory breakdown of myelin in patches in the white matter
It is now evident that the disease is more continuous, with diffuse changes in the white and grey matter, breakdown of myelin, and damage to axons
The McDonald criteria allow earlier confirmation of the diagnosis of multiple sclerosis and earlier decisions on therapy
Disease modifying drugs moderately reduce the number and severity of attacks, the number of new lesions on magnetic resonance imaging, and progression
Early therapy in relapsing-remitting multiple sclerosis has better outcomes
Therapy late in the disease when no relapses are occurring has doubtful benefit
Recently trials have been carried out in patients with a first relapse accompanied by evidence on magnetic resonance imaging characteristic of multiple sclerosis (clinically isolated syndrome) to see if outcomes would be better if therapy was started when symptoms first arose and the patient had not had a second relapse.4 The term clinically isolated syndrome was used to describe a first demyelinating event after trials in 2000-3 that started treatment with disease modifying drugs after a single attack. Although the trials showed fewer patients experiencing a second attack while receiving therapy, it is uncertain how many would have converted to “clinically definite multiple sclerosis,” with a second attack in the long term—although most convert in the first five years, and especially in the first two years, after an initial attack.
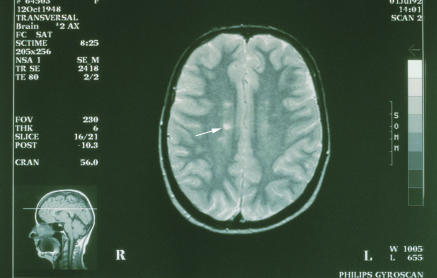
Figure 1.
Magnetic resonance imaging scan of brain of patient with multiple sclerosis. White lesions in white matter (arrow) caused by destruction of myelin sheaths
Credit: COMO-UNIQUE/CUSTOM MEDICAL STOCK/SPL
New understanding of the mechanisms in multiple sclerosis
Since the mid-1800s multiple sclerosis was considered an episodic disorder characterised by the development of discrete lesions or plaques with breakdown of myelin in the white matter of the central nervous system but relative preservation of the axons.5 Evidence now suggests widespread involvement, even in normal appearing white matter, and extensive involvement of grey matter and damage to axons. Damage to axons may be the more important aspect of multiple sclerosis and the basis of the disease's eventual and mostly irreversible progression. The focus has been on understanding mechanisms of attack and breakdown in the disease, but attention will also be given to the processes of neuroprotection, repair, and recovery in the search for new treatments.
Additional educational resources
Polman CH, Thompson AJ, Murray TJ, Noseworthy J, Bolling AC. Multiple sclerosis: the guide to treatment and management. 5th ed. New York: Demos, 2001 (6th ed, 2006)—a regularly updated review, sponsored by the Multiple Sclerosis International Federation
Compston A (ed) McAlpine's Multiple Sclerosis. London: Churchill Livingstone, 4th ed, 2005—classic textbook of multiple sclerosis
Cochrane Collaboration (www.cochrane.org)—numerous Cochrane reviews are available on treatments, symptomatic therapies, rehabilitation, and outcome measures in multiple sclerosis; many more are in preparation
Information for patients
National multiple sclerosis societies (UK: www.mssociety.org.uk; USA: www.nmss.org; Canada: www.mssociety.ca; Australia: www.msaustralia.org.au; and Ireland: www.ms-society.ie)—information on all aspects of multiple sclerosis, including specific symptoms of the disease, treatments, current research, and trials
Kalb RC. Multiple sclerosis: the questions you have, the answers you need. 3rd ed. New York: Demos, 2004—specifically written for patients
Holland NJ, Murray TJ, Reingold SC. Multiple sclerosis: a guide for the newly diagnosed. 2nd ed. New York: Demos, 2002 (3rd ed, 2006)—specifically aimed at people who have just developed multiple sclerosis and are usually doing well but want introductory information about the disease
Treatment
Treatment is of acute attacks, prevention of relapses and progression, management of symptoms, and rehabilitation. In recent years advances have been made in all four areas.
Acute attacks
Unless an attack is mild, such as minor sensory symptoms, the treatment is intravenous methylprednisolone 1000 mg daily for three days. Protocols vary, but this is the most widely used. Clinicians differ on whether to taper off treatment with oral prednisone for two weeks, but this probably does not improve results and increases side effects. Patients are usually not admitted to hospital for this therapy unless severe problems justify other approaches. Large doses of oral steroids may achieve comparable results, but further studies are required.6 Trials that have shown a modest effect on the speed of recovery from an acute attack have not shown any change in eventual deficit or disability.
Relapses and progression
Since the mid-1990s new drugs have been shown by large randomised clinical trials to reduce the number and severity of relapses, reduce the number of new lesions appearing on magnetic resonance imaging, and probably reduce long term progression of multiple sclerosis.7 The disease modifying drugs include injections of interferon beta-1b (Betaseron subcutaneous; Schering, Berlin); interferon beta-1a (Avonex intramuscular; Biogen, Cambridge, MA; Rebif subcutaneous; Serono, Geneva), and glatiramer acetate (Copaxone subcutaneous; Teva; Petach Tikva, Israel). About one in four patients receiving interferon beta-1b or subcutaneous interferon beta-1a and one in 20 receiving intramuscular interferon beta-1a will develop neutralising antibodies against the drug and within two years treatment will be less efficacious.8,9 If antibodies are not detected after two years then no further tests are needed. If antibodies are present the author's approach is to switch patients to glatiramer acetate.
More recently some countries have approved the use of mitoxantrone (Novantrone intravenous infusion; Serono USA, Rockland, MA) for patients with progressive relapsing-remitting and secondary progressive multiple sclerosis whose symptoms are worsening despite treatment with disease modifying drugs.10-13 Although mitoxantrone may interrupt or slow the progression of disease in a substantial number of patients in the short term, the long term results are unclear.14 Cardiac complications can occur in 2% of patients, with uncertain long term effects and, rarely, leukaemia induced by therapy.14 Few other options are available for patients whose disease is progressing despite treatment with disease modifying drugs.
Most clinical trials of therapy in multiple sclerosis have been supported and driven by industry, but trials are problematic as the waxing and waning course of the disease requires large numbers of patients studied over a long period. Unfortunately most of the trial questions have been about relapses and changes detected by magnetic resonance imaging when the important issue is prevention of long term disability. Answers are still not clear as to how much if any long term disability is prevented by current disease modifying drugs.
Symptomatic management
Multiple sclerosis can produce an array of symptoms, many of which are manageable.15 Bladder frequency and urgency will often respond to oxybutynin. Pain and spasms from spastic limbs usually respond to baclofen. Emotional lability with pathological laughing or crying can be managed with a tricyclic antidepressant. Amantadine reduces fatigue in half the patients. More difficult to manage are pain, sexual dysfunction, weakness, dysesthesia and other sensory symptoms, tremor, ataxia, and cognitive change, but even these may respond to various therapeutic approaches. It is important to recognise that half of patients with multiple sclerosis will become depressed and that therapy and counselling may be necessary.15
Alternative therapies
Although most complementary and alternative medicines have not been subjected to randomised clinical trials, three out of four patients with multiple sclerosis use one or more complementary and alternative medicines and visit alternative practitioners more than they do their doctors.16 Although funding for research into complementary and alternative medicine is available it is not utilised fully because the trials are difficult to design and interest has been low.17
Ongoing research
Research now looks at neuroprotection, repair, and recovery mechanisms in the brain as well as the process of central nervous system damage. The new treatments have shown promise in the short term but the important questions are all long term, so long term outcomes are essential in evaluating the cost effectiveness of current and future therapies. The genetic predisposition, geographical distribution, and potential trigger mechanism for the disease are all areas of current research.
Prognosis
The prognosis in multiple sclerosis is often given as an average of the outcomes of all forms of multiple sclerosis taken together. It is more relevant to individual patients to know what the expected outcome might be for their type of multiple sclerosis. The clinical course of multiple sclerosis is being assessed in large clinics with decades of follow-up of their patients, and also by the Sylvia Lawry Center, which has accumulated the outcomes of the placebo groups in the many large clinical trials of multiple sclerosis therapies.
One limiting factor in determining the potential improvement in outcome with new therapies is the lack of a direct biomarker for disease outcome. Three domains are assessed to determine outcome in trials: number of relapses, neurological status according to the expanded disability status scale, and evidence of changes on magnetic resonance imaging. In clinical practice assessing the number and severity of relapses and changes in neurological status are the only practical measures as findings on magnetic resonance imaging are not well correlated with outcome, especially if a standardised approach is not used. Thus magnetic resonance imaging is not a useful way to follow how patients are doing, a common misconception.18 Response to therapy is more likely during the relapsing phase of multiple sclerosis but unlikely when patients have entered a progressive phase of the disease.
Clinical tips
Early is late in multiple sclerosis—when patients develop the first symptoms the disease has been present for a long time and they may have evidence of old lesions on magnetic resonance imaging and some atrophy of the brain. Decisions on therapy should be made as soon as possible
Patients receiving interferon may develop antibodies to the drug and treatment is less efficacious
Repeating conventional magnetic resonance imaging is not a useful way to assess a patient's progress
Over 120 randomised clinical trials are underway in multiple sclerosis, using 30 agents or combinations of agents (including nine oral agents), so the outlook for better therapies in the future is bright. Advances in the understanding of underlying mechanisms in multiple sclerosis is allowing a more focused approach to the development of new therapies for patients with the disease.
Supplementary Material
 McDonald criteria are on bmj.com
McDonald criteria are on bmj.com
TJM is former director of the Dalhousie MS Research Unit.
Competing interests: TJM is chairman of the Health Services Committee of the MS Society of Canada. He is involved in clinical trials with Aventis, BiogenIdec, Serono, Teva Neurosciences, Berlex, Bayer, Health Canada, and the MS Society of Canada. He is on advisory boards for Teva Neurosciences, BiogenIdec, Bayer, and Serono Canada.
References
- 1.McDonald WI, Compston A, Edan G, Goodkin D, Hartung HP, Lublin FD, et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the international panel on the diagnosis of multiple sclerosis. Ann Neurol 2001;50: 121-7. [DOI] [PubMed] [Google Scholar]
- 2.Fangerau T, Schimrigk S, Haupts M, Kaeder M, Ahle G, Brune N, et al. Diagnosis of multiple sclerosis: comparison of the Poser criteria and the new McDonald criteria. Acta Neurol Scand 2004;109: 385-9. [DOI] [PubMed] [Google Scholar]
- 3.Pittock SJ, McClelland RL, Mayr WT, Jorgensen NW, Weinshenker BG, Noseworthy J, et al. Clinical implications of benign multiple sclerosis: a 20-year population-based follow-up study. Ann Neurol 2004;56: 303-6. [DOI] [PubMed] [Google Scholar]
- 4.Jacobs LD, Beck RW, Simon JH, Murray TJ, et al. Intramuscular interferon beta 1a therapy initiated during a first demyelinating event in multiple sclerosis. Champs study group. N Engl J Med 2000;343: 898-904. [DOI] [PubMed] [Google Scholar]
- 5.Murray TJ. Multiple sclerosis: the history of a disease. New York: Demos, 2005.
- 6.Morrow SA, Stoian CA, Dmitrovic J, Chan SC, Metz LM. The bioavailability of IV methylprednisolone and oral prednisone in multiple sclerosis. Neurology 2004;63: 1079-80. [DOI] [PubMed] [Google Scholar]
- 7.Goodin DS, Frohman EM, Garmany GP Jr, Halper J, Likosky WH, Lublin FD, et al. Disease modifying therapies in multiple sclerosis: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and the MS council for clinical practice guidelines. Neurology 2002;58; 169-78. [DOI] [PubMed] [Google Scholar]
- 8.Giovannoni G, Goodman A. Neutralizing anti-IFN-beta antibodies: how much more evidence do we need to use them in practice? Neurology 2005;65: 6-8. [DOI] [PubMed] [Google Scholar]
- 9.Kappos L, Clanet M, Sandberg-Wollheim M, Radue EW, Hartung HP, Hohlfeld R, et al. Neutralizing antibodies and efficacy of interferon beta1a: a 4-year controlled study. Neurology 2005;65: 40-7. [DOI] [PubMed] [Google Scholar]
- 10.Hartung HP, Gonsette R, König N, Kwiecinski H, Guseo A, Morrissey SP, et al. Mitoxantrone in progressive multiple sclerosis: a placebo-controlled, double-blind randomized, multicenter trial. Lancet 2002;360: 2018-25. [DOI] [PubMed] [Google Scholar]
- 11.Goodin DS, Arnason BG, Coyle PK, Frohman EM, Paty DW. The use of mitoxantrone (Novantrone) for the treatment of multiple sclerosis: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 2003;61: 1332-8. [DOI] [PubMed] [Google Scholar]
- 12.In: Cohen BA, Jeffery DR, eds. Identification of suboptimal responders to immune modulating agents and the role of mitoxantrone in worsening multiple sclerosis. Supplement to Neurology 2004;(suppl 6)63(12). [Nine articles.]
- 13.Novantrone prescribing information [package insert]. Serono. Available at www.novantrone.com.
- 14.Shapiro RT. Managing the symptoms of multiple sclerosis. 4th ed. New York: Demos, 2003.
- 15.Feinstein A. The neuropsychiatry of multiple sclerosis. Can J Psychiatry 2004;49: 157-63. [DOI] [PubMed] [Google Scholar]
- 16.Bowling AC. Alternative medicine and multiple sclerosis. New York: Demos, 2001.
- 17.Murray TJ. Complementary and alternative medicine for MS. Int MS J 2005;13: 3. [PubMed] [Google Scholar]
- 18.Frohman EM, Goodin DS, Calabrese PA, Corboy JR, Coyle PK, Filippi M, et al. The utility of MRI in suspected MS: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 2003;61: 602-11. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.