The first endoscope introduced by Bruening in 1907 was a rigid instrument that allowed inspection of the upper gastrointestinal tract under a general anaesthetic.w1 Forty years later the first flexible fibreoptic instrument allowed procedures to be done under local anaesthetic or light sedation. It took a further 20 years for the technological evolution of the first colonoscope. A major advance occurred in 1999, when capsule endoscopy enabled complete visualisation of the small bowel.w2 A capsule is swallowed and propelled through the gastrointestinal tract by the action of peristalsis. It contains an imaging device, which transmits images of the intestine to sensors on the abdominal wall.
Historically the small bowel was considered technically difficult to examine because of its length (3-5 metres), location, and tortuosity.w3 Previously the small bowel could be partly assessed by a push enteroscope, which is longer (about 2 metres) than a standard gastroscope and therefore allows examination of up to 80-120 cm beyond the ligament of Treitz (anatomically the duodenojejunal flexure), while intraoperative enteroscopy required a general anaesthetic and laparotomy. Barium follow through (small bowel meal) and enteroclysis (double contrast small bowel follow through) allow indirect examination of the small bowel but have a low diagnosis rate.1 w4 w5
Given the limitations of these other tests, there has been a surge in investigations on the practical diagnostic ability and clinical utility of capsule endoscopy.
Summary points
Capsule endoscopy—a novel method of imaging the small bowel—is safe and can be performed on an outpatient basis in both primary and secondary care
It has a higher positive diagnosis rate in the detection of small bowel pathology than conventional small bowel investigations
Capsule endoscopy can be used to investigate patients with obscure gastrointestinal bleeding and negative results on upper and lower gastrointestinal endoscopy
Sources and selection criteria
We performed a comprehensive literature search in Medline, Clinical Evidence, the Cochrane library, and Embase with the keywords capsule endoscopy and enteroscopy. We found 50 prospective and peer review studies, six prospective randomised controlled studies, nine retrospective studies, 34 review articles, 21 case studies, 26 letters, 19 editorials, one pooled analysis, and two sets of guidelines (American and European) on capsule endoscopy.
What is capsule endoscopy?
The PillCam SB capsule endoscope (Given Imaging, Yoqneam, Israel), measures 26 mm × 11 mm and weighs 3.7 g. It contains a complementary metal oxide semiconductor imaging chip video camera, six white light emitting diode illumination sources, two silver oxide batteries, and a radio telemetry transmitterw2 (fig 1). The image field of view is 140° and the magnification 1:8. Once swallowed, the capsule is propelled by intestinal peristalsis and excreted in the faeces. Video images are captured at two frames per second and are transmitted by radio frequency to a sensor array in a belt placed around the patient's abdomen. The patient wears this digital data recorder for the duration of the battery life (eight hours). The recorded images are then downloaded to a workstation. The software produces a video of these images, which can be reviewed at any time thereafter. The current cost of a single use capsule is £300 ($522; €439).
Fig 1.

A capsule endoscope
Capsule endoscopy v conventional investigations
Capsule endoscopy has been shown to have a superior positive diagnosis rate (range from 45-76%) for the recognition of small bowel pathology compared with other methods, including push enteroscopy, barium contrast studies, computed tomographic enteroclysis, and magnetic resonance imaging (collective positive diagnosis rate is 21 positive diagnosis rate 1-52%1-11 w6) (table). As a result of these observations, in 2001 capsule endoscopy obtained approval from the Food and Drug Administration in the United States. It is also being used in community gastroenterology practice (primary care) within the US.w7 Patients may soon be able to opt for capsule endoscopy as their first line investigation instead of conventional endoscopy, though this is not currently an option in the NHS.
Table 1.
Studies comparing diagnostic yield of capsule endoscopy with push enteroscopy and radiology for small bowel disease
| Study country | No of patients | P value* | Comparator and diagnostic yield | Yield of capsule endoscopy |
|---|---|---|---|---|
| Italy1 |
20 |
<0.05 |
Barium follow through 20% (5% for OGB) |
45% (31% for OGB) |
| Germany2 |
32 |
<0.0001 |
PE 28% |
66% |
| United Kingdom3 |
50 |
<0.05 |
PE 32% |
66% |
| France4 |
58 |
0.04 |
PE 38% |
69% |
| Germany5 |
33 |
PE 21% |
76% |
|
| Belgium6 |
21 |
PE 52% |
61% |
|
| Spain7 |
42 |
0.05 |
PE 19% |
74% |
| United States8 |
20 |
0.06 |
PE 30% |
55% |
| Germany9 |
22 |
0.12 |
CT enterolysis 36% |
59% |
| United States10 |
52 |
<0.001 |
SB follow through 3% |
55% |
| 0.02 |
Contrast CT 21 |
63% |
||
| United States11 | 20 | PE 25% | 70% |
PE=push enteroscopy; OGB=obscure gastrointestinal bleeding; SB=small bowel; CT=computed tomography.
For comparison of positive diagnosis rate between capsule endoscopy and the comparator—that is, push enteroscopy, CT enteroclysis, etc.
Indications for capsule endoscopy
The clinical use of capsule endoscopy is rapidly expanding, and there is now evidence for specific indications. Obscure gastrointestinal bleeding, defined as recurrent gastrointestinal bleeding in the absence of a cause found using standard endoscopic and radiological methods, is the most common. Initial investigations for obscure gastrointestinal bleeding are upper and lower gastrointestinal endoscopy (gastroscopy and colonoscopy). For patients in whom results are normal, the subsequent prevalence of small bowel pathology identified with capsule endoscopy ranges from 45% to 76%.2,3,5,8 w8-w11 Commonly detected abnormalities include angiodysplasia, tumours, varices, and ulcers.12 Recognition of these lesions can lead to therapeutic intervention (adrenaline injection, diathermy, laser therapy, or surgery) and resolution of bleeding (fig 2).4 In some patients, however, the source of bleeding is found in the upper gastrointestinal tract proximal to the small bowel.1 w4 w10 w11 In such cases a careful second look endoscopy is advisable before capsule endoscopy. In patients with negative results on capsule endoscopy and persistent obscure gastrointestinal bleeding, a second capsule endoscopy should be considered as small studies have shown an additional yield of 35-75%.w12 w13 Figure 3 shows a proposed algorithm for the management of patients with obscure gastrointestinal bleeding.
Fig 2.
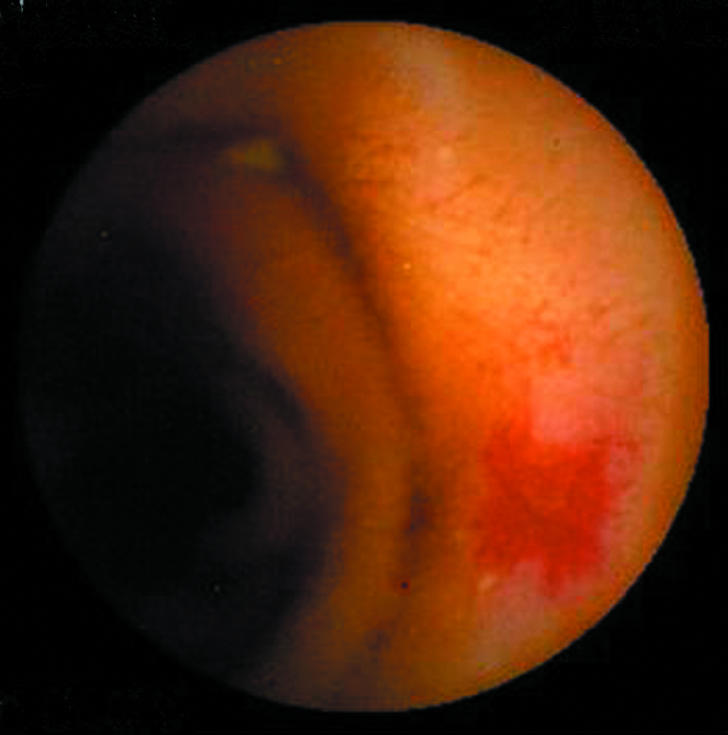
Bleeding in the small bowel secondary to angioectasia
Fig 3.
Proposed role of capsule endoscopy in obscure gastrointestinal bleeding
Indications for capsule endoscopy
Obscure gastrointestinal bleeding (overt/occult)
Suspected small bowel Crohn's disease
Assessment of coeliac disease
Screening and surveillance for polyps in familial polyposis syndromes
Assessment of Crohn's disease and gastrointestinal bleeding in children
Diagnosis of Barrett's oesophagus
Small bowel Crohn's can be an elusive diagnosis, with the mean time from onset of symptoms to diagnosis ranging from one to seven years.w14 w15 Patients with suspected Crohn's disease can present with diarrhoea, abdominal pain, weight loss, or raised inflammatory markers. Results of standard endoscopic or radiological investigations may be equivocal or normal. In such patients, capsule endoscopy can establish the diagnosis in 40-70% of patients by identifying ulcers, erosions, erythema, and mucosal oedema13 w16-w20 and is more sensitive than small bowel follow through and computed tomographic enteroclysis.13 w20-w24 It will also allow assessment of the extent of disease, and these findings can then potentially be confirmed by ileocolonoscopic biopsies.
Capsule endoscopy has two reported roles in coeliac disease. Firstly, it can be used to identify complications related to coeliac disease in refractory disease (for example, small bowel lymphoma or ulcerative jejunitis).w25 w26 The ability of capsule endoscopy to visualise the entire small bowel allows assessment of the extent of disease and detection of early complications.14 More recently, some patients are opting for capsule endoscopy with a photograph of small bowel villous atrophy (virtual histology) in conjunction with a positive result for anti-endomysial antibody. Preliminary data indicate that the recognition of coeliac disease with capsule endoscopy is comparable with macroscopic endoscopic appearances. The ability to diagnose coeliac disease with capsule endoscopy may be specific but not sensitive.w27 Some patients, however, may prefer this test to a more invasive gastroscopy and small bowel biopsy.
Several small studies have reported the use of capsule endoscopy in the surveillance of polyposis syndromes (n = 20-40).w28-w30 Capsule endoscopy is more accurate in the detection of polyps than small bowel follow through and is more likely than magnetic resonance imaging to detect smaller polyps (< 5 mm).15 Larger follow-up studies are needed to assess whether the use of capsule endoscopy changes the management of these patients. It has also been used in the investigation of functional gastrointestinal disorders, but with less impressive results. An initial small study (n = 20) of capsule endoscopy in the assessment of chronic abdominal pain has shown a low positive diagnosis rate.16
Capsule endoscopy is being evaluated in children for similar clinical indications.17 The diagnosis of Crohn's disease not confirmed by standard means has been reported with a similar positive diagnosis rate to that it adults (50-58%).17 w31 One of the potential benefits for using capsule endoscopy in children may be the avoidance of gastroscopy and a general anaesthetic.
Use has now extended beyond the confines of the small bowel. The desire for adults to avoid gastroscopy has also led the manufacturers of capsule endoscopy to produce novel prototypes. The PillCam ESO (Given Imaging, Yoqneam, Israel) has been shown to be accurate, safe, and well tolerated for the detection of oesophageal pathology.18 The conventional PillCam capsule has also been used in the assessment of Barrett's oesophagus by attaching a string to allow controlled movement up and down the oesophagus.w32 This technique provides multiple endoscopic images and transforms a physiological process into a procedure that is operator dependent.
Limitations and complications
Capsule endoscopy is contraindicated in patients with known gastrointestinal obstruction and swallowing disorders. The potentially most serious adverse event after capsule endoscopy is intestinal obstruction due to a pre-existing stricture; this may occur in 0.75% of patients (J Barkin, et al, Annual Scientific Meeting, American College of Gastroenterology, Washington, 2002). Risk factors for retention of the capsule include prolonged use of non-steroidal anti-inflammatory drugs, injury from abdominal radiation, and extensive small bowel Crohn's. The capsule may be retained even in the presence of a previously normal barium small bowel radiograph.12 An alternative safety measure is the Given M2A patency capsule. This is similar in size and shape to the conventional capsule but has a lactose body and contains about 100 mg of barium sulphate. It is excreted intact unless it is impacted in stenosed bowel, in which case it will disintegrate within 40 hours through contact with intestinal fluids.w33
Despite its valuable diagnostic potential, capsule endoscopy can only detect and record small bowel pathology. Currently the device is unable to take biopsies or perform any therapeutic procedures. Interpretation and reading of capsule endoscopy images can be time consuming, especially to the inexperienced. One potentially cost effective strategy is the use of nurse endoscopists for the reporting of images.19 In addition, general practitioners with a specialist interest in endoscopy may wish to provide a capsule endoscopy service in primary care.
Capsule endoscopy v double balloon enteroscopy
Double balloon enteroscopy (push and pull enteroscopy) is a relatively new technique that allows total enteroscopy by intubation of the small intestine through the oral (extended gastroscopy) or anal (extended ileocolonoscopy) route. Deeper examination of the small intestine is possible with the help of sequential inflation and deflation of the two anchoring balloons at the distal end of the enteroscope (allowing the enteroscope to proceed through a marching effect). Using this novel technique loops are also more easily resolved, which is a distinct advantage over push enteroscopy (the current method most commonly used for endoscopic examination of the small bowel). The procedure can be done under conscious sedation, and the average time for examination for each route is 75 minutes.20 The yield positive diagnosis rate is comparable with that of capsule endoscopy, but early data suggest that it may be superior in its therapeutic yield and ability to perform endoscopic interventions.20 Larger prospective studies are needed to clarify the roles and make cost effective comparisons between double balloon enteroscopy, push enteroscopy, and capsule endoscopy.
Additional educational resources
Rey JF, et al. European Society of Gastrointestinal Endoscopy guidelines for video capsule endoscopy. Endoscopy 2004;36: 656-8.
O'Loughlin C, Barkin JS. Wireless capsule endoscopy: summary. Gastrointest Endosc Clin N Am 2004;14: 229-37.
Websites for patients
Conclusion
Capsule endoscopy is a procedure that can be performed on an outpatient basis in both primary and secondary care. It has revolutionised the investigation of small bowel disease because it is more sensitive at identifying mucosal lesions than previous small bowel investigations. Capsule endoscopy has now become the investigation of choice in those patients with obscure gastrointestinal bleeding and normal results on gastroscopy and colonoscopy.
Despite this important technological advance, there are still unresolved clinical issues that require further investigation: how do we manage diffuse small bowel vascular abnormalities or obtain histology from observed inflammatory and mass lesions? Real time viewing is now possible (H Ogata et al, American Society of Gastrointestinal Endoscopy, Chicago, 2005), and we anticipate the development of a device whose movement back and forth within the gut can be controlled. The possibility of targeting lesions within the small bowel for real time thermal coagulation or biopsy no longer seems like science fiction.
Supplementary Material
 A full list of references to identified studies is on bmj.com.
A full list of references to identified studies is on bmj.com.
Contributor: RS wrote the initial draft, and all three authors were involved in subsequent revisions and the final draft. DSS is guarantor.
Funding: None.
Competing interests: MEMcA attended the third international conference for capsule endoscopy in Miami 2004 courtesy of Given Imaging. DSS and MEMcA are both small bowel section committee members of the British Society of Gastroenterology and are currently engaged in drafting the capsule endoscopy and enteroscopy guidelines.
Ethical approval: Not required.
References
- 1.Costamagna G, Shah SK, Riccioni ME, Foschia F, Mutignani M, Perri V, et al. A prospective trial comparing small bowel radiographs and video capsule endoscopy for suspected small bowel disease. Gastroenterology 2002;123: 999-1005. [DOI] [PubMed] [Google Scholar]
- 2.Ell C, Remke S, May A, Helou L, Henrich R, Mayer G. The first prospective controlled trial comparing wireless capsule endoscopy with push enteroscopy in chronic gastrointestinal bleeding. Endoscopy 2002;34: 685-9. [DOI] [PubMed] [Google Scholar]
- 3.Mylonaki M, Fritscher-Ravens A, Swain P. Wireless capsule endoscopy: a comparison with push enteroscopy in patients with gastroscopy and colonoscopy negative gastrointestinal bleeding. Gut 2003;52: 1122-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saurin JC, Delvaux M, Vahedi K, Gaudin JL, Villarejo J, Florent C, et al. Clinical impact of capsule endoscopy compared to push enteroscopy: 1-year follow-up study. Endoscopy 2005;37: 318-23. [DOI] [PubMed] [Google Scholar]
- 5.Hartmann D, Schilling D, Bolz G, Hahne M, Jakobs R, Siegel E, et al. Capsule endoscopy versus push enteroscopy in patients with occult gastrointestinal bleeding. Z Gastroenterol 2003;41: 377-82. [DOI] [PubMed] [Google Scholar]
- 6.Van Gossum A, Hittelet A, Schmit A, Francois E, Deviere J. A prospective comparative study of push and wireless-capsule enteroscopy in patients with obscure digestive bleeding. Acta Gastroenterol Belg 2003;66: 199-205. [PubMed] [Google Scholar]
- 7.Mata A, Bordas JM, Feu F, Gines A, Pellise M, Fernandez-Esparrach G, et al. Wireless capsule endoscopy in patients with obscure gastrointestinal bleeding: a comparative study with push enteroscopy. Aliment Pharmacol Ther 2004;20: 189-94. [DOI] [PubMed] [Google Scholar]
- 8.Lewis BS, Swain P. Capsule endoscopy in the evaluation of patients with suspected small intestinal bleeding: results of a pilot study. Gastrointest Endosc 2002;56: 349-53. [DOI] [PubMed] [Google Scholar]
- 9.Voderholzer WA, Ortner M, Rogalla P, Beinholzl J, Lochs H. Diagnostic yield of wireless capsule enteroscopy in comparison with computed tomography enteroclysis. Endoscopy 2003;35: 1009-14. [DOI] [PubMed] [Google Scholar]
- 10.Hara AK, Leighton JA, Sharma VK, Fleischer DE. Small bowel: preliminary comparison of capsule endoscopy with barium study and CT. Radiology 2004;230: 260-5. [DOI] [PubMed] [Google Scholar]
- 11.Adler DG, Knipschield M, Gostout C. A prospective comparison of capsule endoscopy and push enteroscopy in patients with GI bleeding of obscure origin. Gastrointest Endosc 2004;59: 492-8. [DOI] [PubMed] [Google Scholar]
- 12.Pennazio M, Santucci R, Rondonotti E, Abbiati C, Beccari G, Rossini FP, et al. Outcome of patients with obscure gastrointestinal bleeding after capsule endoscopy: report of 100 consecutive cases. Gastroenterology 2004;126: 643-53. [DOI] [PubMed] [Google Scholar]
- 13.Fireman Z, Mahajna E, Broide E, Shapiro M, Fich L, Sternberg A, et al. Diagnosing small bowel Crohn's disease with wireless capsule endoscopy. Gut 2003;52: 390-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cellier C, Green PH, Collin P, Murray J. ICCE consensus for celiac disease. Endoscopy 2005;37: 1055-9. [DOI] [PubMed] [Google Scholar]
- 15.Caspari R, von Falkenhausen M, Krautmacher C, Schild H, Heller J, Sauerbruch T. Comparison of capsule endoscopy and magnetic resonance imaging for the detection of polyps of the small intestine in patients with familial adenomatous polyposis or with Peutz-Jeghers' syndrome. Endoscopy 2004;36: 1054-9. [DOI] [PubMed] [Google Scholar]
- 16.Bardan E, Nadler M, Chowers Y, Fidder H, Bar-Meir S. Capsule endoscopy for the evaluation of patients with chronic abdominal pain. Endoscopy 2003;35: 688-9. [DOI] [PubMed] [Google Scholar]
- 17.Guilhon de Araujo Sant'Anna AM, Dubois J, Miron MC, Seidman EG. Wireless capsule endoscopy for obscure small-bowel disorders: final results of the first pediatric controlled trial. Clin Gastroenterol Hepatol 2005;3: 264-70. [DOI] [PubMed] [Google Scholar]
- 18.Eliakim R, Yassin K, Shlomi I, Suissa A, Eisen GM. A novel diagnostic tool for detecting oesophageal pathology: the PillCam oesophageal video capsule. Aliment Pharmacol Ther 2004;20: 1083-9. [DOI] [PubMed] [Google Scholar]
- 19.Levinthal GN, Burke CA, Santisi JM. The accuracy of an endoscopy nurse in interpreting capsule endoscopy. Am J Gastroenterol 2003;98: 2669-71. [DOI] [PubMed] [Google Scholar]
- 20.May A, Nachbar L, Ell C. Double-balloon enteroscopy (push-and-pull enteroscopy) of the small bowel: feasibility and diagnostic and therapeutic yield in patients with suspected small bowel disease. Gastrointest Endosc 2005;62: 62-70. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



