Management of traumatic and surgical wounds has had a chequered history. For example, in 1346 at the Battle of Crécy, France, foot soldiers were issued with cobwebs to staunch haemorrhage caused by trauma. Two centuries later, the eminent surgeon Ambroise Paré (1510-1590) rejected boiling oil as a primary dressing after amputation, preferring a mixture of oil of turpentine, rosewater, and egg.
Figure 1.

Although the 16th century French surgeon Ambroise Paré could successfully dress a wound, he felt that only God could heal it
Classification
Surgical incisions—Surgical incisions cause minimal tissue damage. They are made with precision in an environment where aseptic and antiseptic techniques reduce the risk of infection, with the best of instruments and the facility to control haemostasis. Penetrating trauma may involve minimal damage to skin and connective tissue, though deeper damage to vessels, nerves, and internal organs may occur.
Figure 2.

Pretibial laceration showing treatment with sterile skin closure strips
Lacerations—Lacerations are caused when trauma exceeds intrinsic tissue strength—for example, skin torn by blunt injury over a bony prominence such as the scalp. Tissue damage may not be extensive, and primary suturing (see below) may be possible. Sterile skin closure strips may be appropriate in some circumstances—for example, in pretibial laceration, as suturing causes increased tissue tension, with the swelling of early healing and inflammation leading to more tissue loss.
Table 1.
Types of traumatic and surgical wounds
| Type of wound | Result | Cause |
|---|---|---|
| Incision | Penetrating | Surgical (rarely, trauma) |
| Laceration | Torn tissue | Usually trauma |
| Contusion | Extensive tissue damage | Usually trauma; skin may be intact |
| Abrasion | Superficial epithelial | Usually trauma |
| Combination | Usually severe trauma | Life threatening |
Contusions—Contusions are caused by more extensive tissue trauma after severe blunt or blast trauma. The overlying skin may seem to be intact but later become non-viable. Large haematomas under skin or in muscle may coexist; if they are superficial and fluctuant they can be evacuated with overlying necrosed skin. Ultrasound scanning or magnetic resonance imaging may help to define a haematoma amenable to evacuation. Extensive contusion may lead to infection (antibiotic prophylaxis should be considered in open wounds) and compartment syndromes (fasciotomy will be needed to preserve a limb).
Large open wounds—Such wounds may be left to heal “by secondary intention” (that is, the wound heals from the base upwards, by laying down new tissue) or with delayed skin grafting, depending on the extent of the residual defect. Exploration of a traumatic wound is needed if there is a suspicion of blood vessel or nerve damage, with attention to fractures and debridement of devascularised tissue and removal of foreign material.
Abrasions—Abrasions are superficial epithelial wounds caused by frictional scraping forces. When extensive, they may be associated with fluid loss. Such wounds should be cleansed to minimise the risk of infection, and superficial foreign bodies should be removed (to avoid unsightly “tattooing”).
Management
Surgical wounds are made in optimum conditions with full anaesthetic and operating theatre support; traumatic wounds are not, and they may be associated with much more serious underlying injury. Triage and resuscitation may be needed before definitive wound management is started.
This is the fifth in a series of 12 articles
Wounds usually involve some loss or damage to an epithelial surface (usually skin) but may also include damage to underlying connective tissue, which may occur without epithelial loss
In England, triage and resuscitation should be done following the Advanced Trauma Life Support guidelines of the Royal College of Surgeons of England (www.rcseng.ac.uk)
Arterial bleeding is easy to recognise—pulsatile and bright red—provided it is overt, but if it is hidden from view (for example, the result of a penetrating injury of the aorta) it may lead to profound unexpected haemorrhagic shock. Early exploration and repair or ligation of blood vessels may be required. Venous haemorrhage is flowing and dark red, and can be controlled by adequate direct pressure. Even large veins may spontaneously stop bleeding after this measure. Capillary bleeding oozes and is bright red; it can lead to shock if injury is extensive and it should not be underestimated.
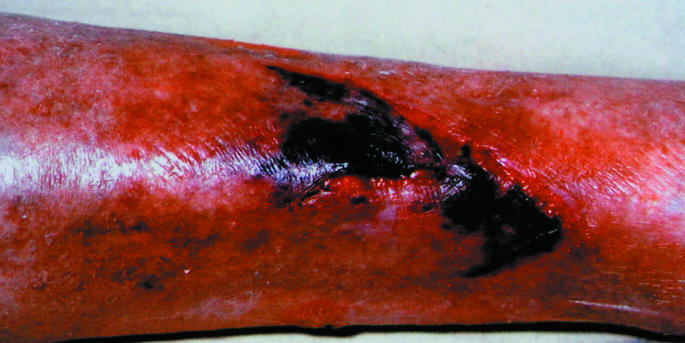
Figure 3.
Streptococcal cellulitis complicating a leg wound (wound not shown)
The risk of infection in traumatic wounds is reduced by adequate wound cleansing and debridement with removal of any non-viable tissue and foreign material. If severe contamination is present, broad spectrum antibiotic prophylaxis is indicated and should be extended as specific therapy as recommended for surgical wounds that are classed as “dirty” or when there are early signs of infection. Traumatic wounds need tetanus prophylaxis (parenteral benzylpenicillin and tetanus toxoid, depending on immune status). Strong evidence supports the use of antibiotic prophylaxis and treatment for surgical wounds that are classed as “clean contaminated” or “contaminated.” The value of antibiotic prophylaxis in “clean” wounds is controversial but is widely accepted in prosthetic surgery (such as hip and knee replacement and synthetic vascular bypass surgery).
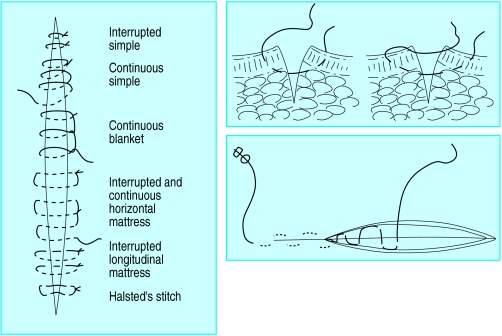
Figure 4.
Left: Suture techniques in skin. Top right: Simple and mattress closure. Bottom right: Subcuticular closure
Wounds from explosions and gunshot
When the source of the wound is high velocity (for example, an explosion or gunshot), it causes more damage because of the dissipation of kinetic energy ( , where m is the mass of the bullet or shrapnel and v its velocity). In addition to gross skeletal injury, soft tissues (such as muscles of the thigh) develop cavitation ahead of the bullet track. These tissues are rendered ischaemic and there may be a large exit wound. Behind the missile there is a sucking action that deposits clothing or dirt in the wound. Together with ischaemia, this contamination provides an ideal culture medium for anaerobic organisms (such as Clostridium perfringens, which can lead to gas gangrene).
, where m is the mass of the bullet or shrapnel and v its velocity). In addition to gross skeletal injury, soft tissues (such as muscles of the thigh) develop cavitation ahead of the bullet track. These tissues are rendered ischaemic and there may be a large exit wound. Behind the missile there is a sucking action that deposits clothing or dirt in the wound. Together with ischaemia, this contamination provides an ideal culture medium for anaerobic organisms (such as Clostridium perfringens, which can lead to gas gangrene).
Table 2.
Categories of surgical wounds
| Category | Example | Recommendation for antibiotics |
|---|---|---|
| Clean | Hernia, varicose veins, breast | None |
| Prosthetic surgery: vascular, orthopaedic implants | Prophylaxis | |
| Clean contaminated | Elective cholecystectomy | Prophylaxis |
| Contaminated | Elective colorectal operations | Prophylaxis |
| Dirty | Drainage of abscess | Treatment if spillage |
| Faecal peritonitis | Treatment |
These wounds need extensive debridement down to viable tissue and should be left open until healthy granulation tissue has formed; repeated debridement may be necessary. Even after extensive debridement, infection may develop, requiring antibiotic treatment. Where there is doubt or an obvious crush injury, fasciotomy can prevent systemic complications, including infection. After debridement, delayed primary or secondary suturing may be done, with or without reconstructive surgery (see eighth article in this series). Alternatively, if the combination of wound contraction and epithelialisation will leave an acceptable cosmetic appearance, a wound may be left to heal by secondary intention. Human and animal bites are traditionally managed in this way, but primary closure can be done after wound debridement and excision of non-viable tissue.
Table 3.
Wounds to consider for open management
| • Severe contamination (during laparotomy for faecal peritonitis) |
| • Old laceration (> 12-24 hours; depends on amount of contusion) |
| • Shock (of any cause but usually haemorrhagic) |
| • Devitalisation (local poor tissue perfusion) |
| • Foreign body (either external or known dead tissue) |
| • Kinetic energy (in wounds caused by explosions; implies presence of dead tissue and foreign material) |
Methods of wound closure
For primary closure, the technique of closure, the suture material, and the type of needle or appliance all need to be considered.
Various suturing techniques exist. Skin may be closed with simple or mattress sutures using interrupted or continuous techniques. Knots should not be tied tightly, to allow swelling as a result of inflammation and to prevent necrosis at the skin edge. Mattress sutures ensure optimal eversion at the skin edge and appose deeper tissue, reducing the risk of formation of haematoma or seroma. The subcuticular suture is the most widely favoured technique for closing surgical skin wounds and has good cosmetic results. Arterial anastomoses and arteriotomies are closed to ensure eversion, but gut anastomosis conventionally has an inverted suture line.
A tourniquet is rarely needed in traumatic bleeding—control by direct pressure prevents irreversible ischaemia and nerve damage
Bomb blast and gunshot injuries should not be sutured—primarily because of the high risk of infection
The ideal suture material for a particular wound remains controversial. Sutures that are absorbable (for example, polyglactin or polydioxanone) clearly do not require removal. Catgut should no longer be used as it causes an excessive tissue reaction, which may predispose to infection. Such reactions are less likely to occur with the use of synthetic polymers. Non-absorbable sutures (for example, natural silk or synthetic polymers such as nylon or polypropylene) need removal. The monofilament polymers cause minimal tissue reaction and are least likely to lead to secondary (exogenous) infection. Silk can cause an intense tissue reaction, with an increased risk of excessive scarring and of formation of a suture abscess; silk is therefore no longer recommended.
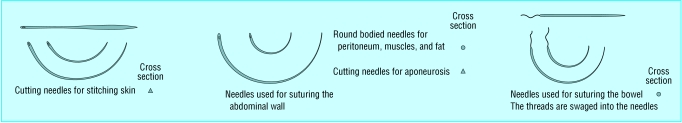
Figure 5.
Types of needles used for different surgical procedures. Straight needles and all hand needles are no longer recommended as they have an added risk of causing needle stick injury and the passage of viruses through body fluids. Instrument mounted needles or, when appropriate (as in closure of abdominal fascia), blunted needles should be used
Metal clips and staples are alternatives to conventional suturing. Despite their need for removal, they are associated with good cosmetic results and low infection rates. Disposable applicators are expensive but allow rapid closure of long wounds after prolonged surgical procedures. Some stapling devices are sophisticated and allow safer surgery—for example, for very low coloanal anastomosis.
Figure 6.


Left: Final appearance of subcuticular closure with polypropylene closure. Right: Final appearance of subcuticular closure with polyglactin closure
Adhesive strips are useful for closing superficial wounds. In emergency departments a child's forehead laceration can be closed without anaesthetic or tears. They allow for wound swelling and are associated with low infection rates. Adhesive polyurethane film dressings have a similar effect with sutured wounds and provide a barrier to infection. The methacrylate superglues are widely used for skin closure, particularly with scalp wounds (though surrounding hair should be trimmed first). Fibrin glues are relatively expensive but allow rapid closure.
Figure 7.

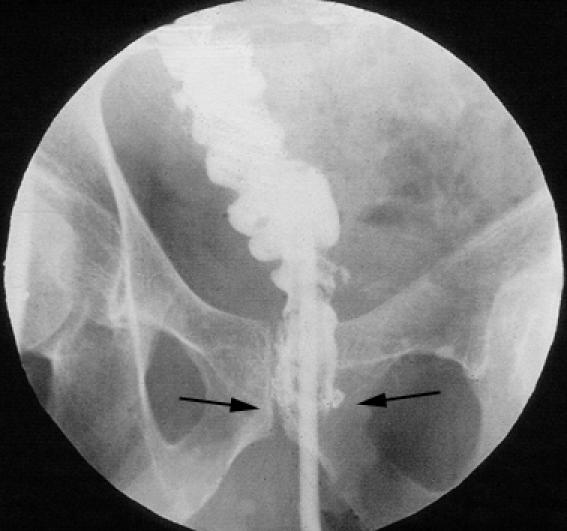
Left: Incision of neck closed with skin clips. Right: X ray showing stapled low anterior resection: the gastrografin enema shows no leakage from the anastomosis
Modern suture materials are presented in sterile, single use packets. Sutures are bonded on to hollow needles. Dispensing with the eye of the needle results in a “shoulderless” needle, permitting easier passage through, and less disruption of, tissues.
Figure 8.

Polyurethane film dressing over a wound after subcuticular closure
Table 4.
Time to removal of non-absorbable sutures
| Site of sutures | No of days |
|---|---|
| Scalp and face | 3-4 |
| Upper limb | 7 |
| Lower limb | 7-10 |
| Trunk | 10-14 |
Suture removal depends on the wound site. The role of dressings to cover sutured wounds remains controversial. Polyurethane dressings allow inspection and provide a bacterial barrier. Island dressings allow absorbance of wound exudate and lessen the risk of leakage.
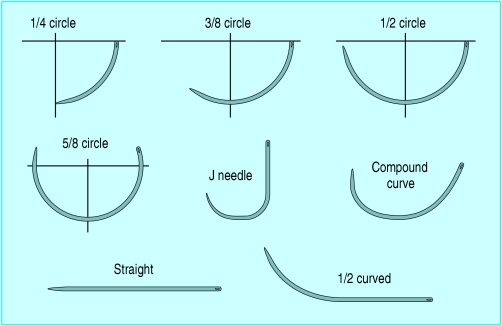
Figure 9.
Shapes of needle used in surgical and traumatic wound closure
Hidradenitis suppurativa and pilonidal sinus wounds
Hidradenitis, an infection of apocrine sweat glands, affects armpits and groins; pilonidal sinus, a tissue infection caused by ingrowing hair, mainly affects the natal cleft.
Figure 10.

Excision wound in hidradenitis suppurativa
Failed, repeated drainage of the abscesses requires complete excision. The defect usually heals by secondary intention. Initially, excision wounds are usually dressed with polymeric foam. Once the wound has reduced in size, a topical antimicrobial dressing (such as those that contain iodine or silver) may be used. However, grafts or flaps are also used, either as the primary treatment or for non-healing wounds. These wounds often become infected and require prolonged treatment to cover Gram positive and anaerobic organisms.
The picture of Ambroise Paré is published with permission from TopFoto.
The ABC of wound healing is edited by Joseph E Grey (joseph.grey@cardiffandvale.wales.nhs.uk), consultant physician, University Hospital of Wales, Cardiff and Vale NHS Trust, Cardiff, and honorary consultant in wound healing at the Wound Healing Research Unit, Cardiff University, and by Keith G Harding, director of the Wound Healing Research Unit, Cardiff University, and professor of rehabilitation medicine (wound healing) at Cardiff and Vale NHS Trust. The series will be published as a book in summer 2006.
Competing interests: DJL has received an educational grant for his research group from Merck Sharp and Dohme and had expenses and a fee paid by Ethicon for attending an advisory panel and for the making of an educational film. For series editors' competing interests, see the first article in this series.
Further reading and resources
- • Téot L, Banwell PE, Ziegler UE, eds. Surgery in wounds. Berlin: Springer, 2004.
- • Leaper DJ, Harding KG, eds. Wounds. Biology and management. Oxford: Oxford Medical Publications, 1998.
- • Bales S, Harding K, Leaper DJ. An introduction to wounds. London: Emap Healthcare, 2000.
- • Leaper DJ, Harding KG, Phillips CJ. Management of wounds. In: Johnson C, Taylor I, eds. Recent advances in surgery. 25th ed. London: Royal Society of Medicine, 2002.
- • Leaper DJ, Low L. Surgical access: incisions and the management of wounds. In: Kirk RM, Ribbons WJ, eds. Clinical surgery in general. 4th ed. Edinburgh: Churchill Livingstone, 2004.
- • Leaper DJ. Basic surgical skills and anastomoses. In: Russell RCG, Williams NS, Bulstrode CJK, eds. Bailey and Love's short practice of surgery. 24th ed. London: Arnold, 2004.