Abstract
Influenza A viruses cause pandemics at sporadic intervals. Pandemic viruses can potentially be introduced into the human population through in toto transfer of an avian influenza virus or through reassortment between avian and human strains. Pigs are believed to play a central role in the creation of pandemic viruses through reassortment because of their susceptibility to infection with both avian and human influenza viruses. However, we recently found that a human-lineage H3N2 influenza virus was highly restricted in its ability to infect pigs after intranasal inoculation. We hypothesized that this restricted infectivity phenotype was controlled by the hemagglutinin (HA) and neuraminidase (NA). To test this, we infected pigs with reverse genetics-created HA plus NA reassortant viruses. Specifically, introduction of the HA and NA genes of a contemporary H3N2 swine virus into the genetic background of the wholly human virus resulted in a significant increase in virus shedding and pathogenicity. These data indicate that the HA/NA can play important roles in controlling human influenza virus infectivity in pigs. The results further support the premise that a barrier exists to human influenza virus infection in pigs, which may limit the role of pigs in pandemic virus creation through reassortment of human and avian influenza viruses.
Influenza pandemics remain a very serious threat to public health. Pandemics are caused by viruses that have a hemagglutinin (HA) to which the majority of the human population has no immunity. Such a novel HA can be introduced into the human population either through the direct transmission of an avian influenza virus to humans or through reassortment between human and avian virus strains. However, since avian influenza viruses do not replicate efficiently in humans (2, 41, 42), host range restrictions must be overcome before an avian virus can be introduced into the human population. Although the molecular basis for influenza virus host range restriction is not fully understood, it is known that host specificity is determined in part by the binding preference of the HA protein to cellular sialic acids (14, 15, 42). While avian influenza viruses preferentially bind to receptors terminating in sialic acid (SA) linked α2,3 to galactose (N-acetylneuraminic α2,3Gal [NeuAcα2,3Gal] or N-glycolylneuraminic α2,3Gal) (6, 16, 32, 35), human viruses prefer α2,6-linked receptors (NeuAcα2,6Gal) (6, 7, 9, 32). Correspondingly, NeuAcα2,6Gal is the predominant sialic acid expressed on epithelial cells in the human trachea, whereas SAα2,3Gal is the major form found on duck intestinal cells (6, 7, 15-17, 32). These patterns are not absolute, as Matrosovich and colleagues have shown that NeuAcα2,3Gal can be expressed in a subset of cells cultured from human respiratory tissues (25). Swine respiratory epithelial cells, however, express substantial quantities of both SAα2,3Gal and SAα2,6Gal (15), which likely explains why pigs are uniquely susceptible to infection with avian and human influenza viruses (20). Pigs may, therefore, serve as a “mixing vessel” for reassortment between these viruses and as the source of pandemic viruses (4, 14, 32, 34, 41).
Despite the fact that infection of pigs with human viruses may be a critical factor in the development of pandemic viruses, little research has been directed toward determining whether any barrier exists to efficient human-to-pig transmission of influenza viruses. The existence of such a barrier is suggested by the fact that, although human-lineage influenza viruses have been isolated from pigs (1, 4, 12, 18), sustained circulation of human viruses in pig populations appears to be a relatively rare event (8, 12, 14). As such, it has been suggested that, as with maintenance of avian viruses in pigs, efficient transmission of human viruses among pigs requires mutational adaptation to the new host (4, 23). This hypothesis is supported by our recent finding that a wholly human-lineage H3N2 influenza A virus (A/Sw/ONT/00130/97 [Sw/ONT]) was highly restricted in its ability to infect pigs after intranasal infection compared to a contemporary triple reassortant (HA, neuraminidase [NA], and PB1 polymerase genes of human-lineage virus; matrix, nonstructural, and nucleoprotein [NP] genes of classical swine-lineage virus; and PA and PB2 polymerases of avian-lineage virus) H3N2 swine isolate (A/Sw/MN/593/99 [Sw/MN]) (21). Furthermore, the triple reassortant H3N2 viruses have spread efficiently throughout the pig population in the United States (18, 40, 43), while the wholly human Sw/ONT virus, although initially able to cross the species barrier to infect a single baby piglet, did not spread to other pigs (18).
Taken together, these findings suggest that the lack of spread of Sw/ONT in the swine population may have been due to inefficient infection of pigs with this wholly human virus. Given the importance of the HA protein in limiting avian-to-human influenza virus transmission, we sought to address whether the HA also controls the infectivity and pathogenicity of the human-lineage Sw/ONT virus in pigs. However, the receptor-binding properties of the viral HA and the receptor-destroying activity of the viral NA must be balanced, both for efficient release of virus from infected cells (11, 13, 19, 28, 39) and likely also during initial infection (26). Thus, to avoid changing virus growth characteristics in pigs simply as a result of an imbalance between HA and NA functions, we generated HA/NA double reassortants between Sw/ONT and Sw/MN by reverse genetics (rg). We then inoculated pigs intranasally with the HA/NA reassortant viruses and rg-created parental control viruses and determined each virus' infectivity, replication kinetics, and ability to induce pathological lesions.
MATERIALS AND METHODS
Cells.
Madin-Darby canine kidney (MDCK) cells were maintained in Eagle's minimal essential medium (GIBCO/BRL) supplemented with 10% fetal bovine serum (GIBCO/BRL), penicillin-streptomycin (GIBCO/BRL), and amphotericin B (Fungizone; GIBCO/BRL). 293T human embryonic kidney cells were grown in Dulbecco's modified Eagle's medium (GIBCO/BRL) supplemented with 10% fetal bovine serum and antimicrobials. All cells were maintained at 37°C in a 5% CO2 atmosphere.
Plasmid construction and generation of reverse genetics viruses.
To generate infectious influenza viruses of defined genotype, we used a previously described RNA polymerase I rg system (29). Four specific viruses were created: the two parental viruses (rgSw/ONT and rgSw/MN) that derived all eight negative-sense RNA segments from Sw/ONT (H3N2) or Sw/MN (H3N2), respectively (field isolates were generously provided by S. Carman, University of Guelph, Ontario, Canada [Sw/ONT] and G. Anderson, ImmTech Biologics, LLC, Bucyrus, KS [Sw/MN]), and two reassortant viruses containing the HA plus NA gene segments of Sw/ONT with the remaining gene segments derived from Sw/MN (rgSw/MN+ONT HA/NA) and vice versa, the HA plus NA gene segments of Sw/MN with the remaining gene segments derived from Sw/ONT (rgSw/ONT+MN HA/NA). The virus stocks were analyzed by direct cycle sequencing to ensure that the rg-created viruses contained the desired constellation of genes and to rule out the introduction of spurious mutations. All rg-created viruses grew to high titers in MDCK cells (data not shown).
Animals.
Forty-five domestic pigs were purchased from a commercial herd and shown to be serologically negative for prior exposure to porcine reproductive and respiratory syndrome virus, Mycoplasma hyopneumoniae, and H1 and H3 influenza viruses. The pigs were 6 weeks old at the start of the experiment and were maintained in accordance with guidelines of the USDA and the University of Wisconsin Research Animal Resources Center.
Experimental design.
The pigs were randomly assigned to 9 cohorts of 5 pigs each and acclimated to biosafety level 2 isolation housing for 1 week. On day 0 of the experiment, prior to inoculation, a short physical examination was performed to assess the general condition of the animals. At this time, and daily throughout the experiment, each pig's attitude, as well as clinical signs of respiratory disease (sneezing and coughing), were quantified on a scale of 0 to 3, with 0 indicating a clinically normal animal and 3 indicating a severely abnormal condition. Each pig's food intake was scored as 0, indicating that the animal was eating, or 1, indicating that the animal was not eating. Following the physical exams on day 0, the pigs were sedated by intramuscular injection of 4 mg/kg of body weight of xylazine (Phoenix Pharmaceutical) and 4 mg/kg of tiletamine plus zolazepam (Telazol; Fort Dodge) and weighed, and preinoculation nasal swab (Dacron polyester; Hardwood Products Company, Guilford, Maine) samples for virus isolation and blood samples for serology were collected. The pigs were then inoculated by intranasal instillation with rgSw/MN, rgSw/ONT, rgSw/MN+ONT HA/NA, or rgSw/ONT+MN HA/NA, at 2 × 103 or 2 × 106 50% tissue culture infective doses (TCID50; titers determined in MDCK cells). Five pigs were inoculated with each dose of virus, and the 5 pigs in the ninth cohort were mock inoculated to serve as uninfected controls. At daily intervals after inoculation, the animals were assessed clinically and nasal swab samples were obtained from each pig. The swabs were placed in 1 ml of viral transport medium containing phosphate-buffered saline, 0.5% bovine serum albumin, and the antimicrobials penicillin G, streptomycin, nystatin, and gentamicin and stored at −80°C for subsequent analysis. Blood samples for serology were collected from each animal onday 7.
Evaluation for pathological lesions.
On day 7, the animals were euthanized by exsanguination following anesthesia by intramuscular injection of 4 mg/kg xylazine and 4 mg/kg tiletamine plus zolazepam. The lungs were removed for postmortem analysis. Macroscopic pulmonary lesions were graded according to the percentage of each lung lobe exhibiting gross pathological evidence of tissue consolidation. The value for each individual lobe was adjusted by a factor that accounted for the contribution of each individual lung lobe to the total lung mass (as determined by examining the lungs of 10 age-matched, uninfected, normal pigs). The adjusted values for each lobe were then added to obtain the overall percentage of lung tissue consolidation for each pig.
Evaluation of virus shedding.
The amounts of virus shed in nasal secretions were determined as previously described (21). Briefly, 10-fold serial dilutions of the viral transport medium containing the nasal swabs were inoculated (in duplicate) onto MDCK cells and incubated for 72 h. The presence of virus replication in each well was confirmed by immunocytochemical staining using a mouse anti-NP monoclonal antibody (68D2; kindly provided by M. McGregor and Y. Kawaoka, University of Wisconsin—Madison). Each staining procedure included an isotype-matched, negative-control antibody and mock-infected negative-control cells. The virus titer of each specimen, expressed as the TCID50 perml of transport medium, was calculated using the method of Reed and Muench(31).
Hemagglutination inhibition assay.
The levels of hemagglutination-inhibiting (HI) antibodies in serum samples were determined as described previously (21, 30). Briefly, sera were incubated overnight with receptor-destroying enzyme (Denka Seiken Co., Tokyo, Japan). After inactivation of the receptor-destroying enzyme, twofold serial dilutions of sera were mixed with 4 HA units of rgSw/MN or rgSw/ONT. Inhibition of hemagglutination was tested by adding 0.5% (vol/vol) washed turkey red blood cells, and the HI antibody titers were defined as the reciprocal of the highest dilution causing complete inhibition of agglutination.
Statistical analysis.
Values are expressed as means ± standard errors of the means (SEMs). Data between treatment groups were analyzed by t test or one-way analysis of variance. When F was significant (P ≤ 0.05), further differences between means were determined by Tukey's omega procedure. Means were considered statistically significantly different at P values of ≤0.05.
RESULTS AND DISCUSSION
Only mild changes in the clinical appearances of the animals were observed in this study. Lack of serious disease is, however, not unusual when pigs are infected intranasally with influenza virus in a clean isolation environment (21, 22). Overall, animals inoculated with rgSw/ONT developed only mild pulmonary lesions. In contrast, pigs infected with rgSw/MN exhibited a moderate to severe level of pulmonary pathology, and there was a dose-dependent effect (Table 1). The severity of lung pathology seen in pigs infected with the rg-created parental viruses closely mirrored the extent of pulmonary pathology observed in our previous study using field isolates of Sw/ONT and Sw/MN (21). The exchange of the HA plus NA genes between the two parental viruses resulted in a reversal of their phenotypes (Table 1). While replacing the HA and NA genes of Sw/MN virus with the Sw/ONT envelope glycoprotein genes (Sw/MN+ONT HA/NA) led to only a partial attenuation of pathogenicity (as assessed by the degree of lung tissue consolidation in comparison to the rgSw/MN parental virus), a marked and significant increase in pathogenicity was observed for rgSw/ONT virus expressing the Sw/MN HA and NA genes (Sw/ONT+MN HA/NA) compared to rgSw/ONT.
TABLE 1.
Response of pigs to intranasal infection with rgSw/ONT, rgSw/MN, rgSw/ONT+MN HA/NA, or rgSw/MN+ONT HA/NA
| Dose (TCID50) and virus | % Lung tissue consolidationa | HI antibody titer in seruma |
|---|---|---|
| None (controls) | 0.106 ± 0.0649 | 0 |
| 2 × 103 | ||
| rgSw/ONT | 0.53 ± 0.4744d | 4 ± 4c |
| rgSw/ONT+MN HA/NA | 12.65 ± 3.7452b,d | 36 ± 31.2 |
| rgSw/MN | 7.51 ± 3.37 | 92 ± 17.44b,c,d |
| rgSw/MN+ONT HA/NA | 5.194 ± 1.7332b | 0d |
| 2 × 106 | ||
| rgSw/ONT | 1.348 ± 1.0948c,d | 0c,d |
| rgSw/ONT+MN HA/NA | 16.614 ± 2.7937b,d | 324 ± 85.9b,d |
| rgSw/MN | 22.7 ± 5.4425b,c | 480 ± 101.2b,c,d |
| rgSw/MN+ONT HA/NA | 7.48 ± 5.1117 | 96 ± 29.9b,d |
Data are means ± SEM, n = 5 animals per treatment group.
P ≤ 0.05 versus controls.
P ≤ 0.05 between parental viruses at the given dose.
P ≤ 0.05 for parental virus versus HA/NA reassortant viruses.
Prior to inoculation, all pigs were seronegative to swine influenza virus. All rgSw/MN-infected animals had virus-specific antibodies present in their sera by day 7 (Table 1), as is typical of infection of pigs with swine-adapted viruses (21, 22). Conversely, with the exception of one animal challenged at 2 × 103 TCID50 that produced a weak antibody response (1:20), none of the pigs inoculated with rgSw/ONT developed detectable antibody titers by day 7. Inoculation of pigs with rgSw/MN+ONT HA/NA resulted in significantly decreased antibody responses to infection compared to the parental rgSw/MN virus. In contrast, pigs inoculated with rgSw/ONT+MN HA/NA produced a considerably stronger antibody response than animals inoculated with the parental rgSw/ONT; the titers were significantly different among pigs at the higher challenge dose.
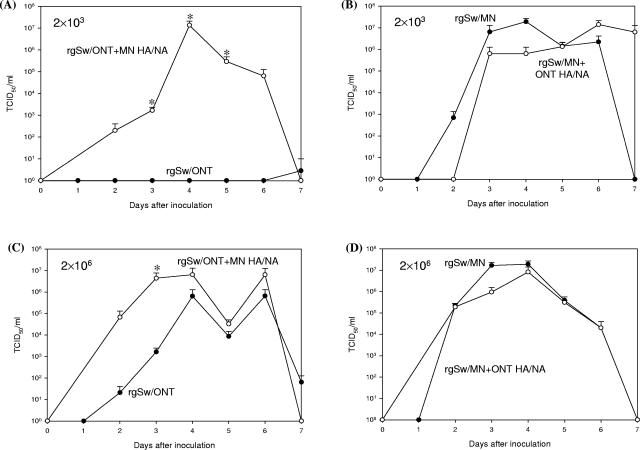
The kinetics and absolute levels of virus shedding were remarkably different between the two rg-created parental viruses (Fig. 1). On average, pigs inoculated with rgSw/MN shed detectable levels of virus for 4.9 days over the course of the experiment. Conversely, the mean duration of virus shedding among animals infected with rgSw/ONT was only 1.8 days. Furthermore, the nasal virus titers were generally higher for pigs infected with rgSw/MN than for pigs receiving rgSw/ONT. Overall, the nasal virus shedding patterns observed for the rg-created parental viruses closely resembled those previously described for the field isolates of Sw/ONT and Sw/MN (21). The introduction the HA and NA genes of Sw/MN into the Sw/ONT genetic backbone substantially increased the duration and level of nasal virus shedding compared to the Sw/ONT parental virus (Fig. 1). For instance, the mean duration of virus shedding in animals inoculated with rgSw/ONT+MN HA/NA increased to 3.5 days. In addition, nasal virus titers on days 3, 4, and 5 in pigs infected with 2 × 103 TCID50 of the rgSw/ONT+MN HA/NA virus and on day 3 in pigs infected with 2× 106 TCID50 of the virus were significantly higher than those for pigs infected with the parental rgSw/ONT virus.
FIG. 1.
Group means + SEMs of the nasal virus shedding from the day of inoculation (day 0) to day 7 after inoculation. (A) Pigs infected with 2 × 103 TCID50 of rgSw/ONT (•) or rgSw/ONT+MN HA/NA (○); (B) pigs infected with 2 × 103 TCID50 of rgSw/MN (•) or rgSw/MN+ONT HA/NA (○); (C) pigs infected with 2 × 106 TCID50 of rgSw/ONT (•) or rgSw/ONT+MN HA/NA (○); (D) pigs infected with 2 × 106 TCID50 of rgSw/MN (•) or rgSw/MN+ONT HA/NA (○). Control animals did not shed virus at any point during the experiment and are not represented in the graphs. *, P ≤ 0.05 between viruses.
Although the HA and NA of Sw/MN are both of human influenza virus origin, previous work has shown that many of the early triple reassortant H3N2 viruses (including Sw/MN) contain 12 amino acid differences in their HA protein that are unique to the swine triple reassortant viruses and are not present in the most closely related human H3 virus HAs (including Sw/ONT) (18, 43). The sites of these amino acid differences include residues previously implicated in species specificity (3, 5, 10), receptor binding (18, 42, 43), and/or glycosylation (18). Given the fact that viruses with the triple reassortant genotype have spread throughout the U.S. swine population while Sw/ONT has not, these differences are of interest as potential swine adaptation mutations. For instance, amino acid differences at residues 135, 138, and/or 190 may impact the sialic binding preferences of Sw/ONT and Sw/MN. Additionally, the loss of a putative glycosylation site at amino acid residue 246 may contribute to an increased resistance of Sw/MN to porcine surfactant protein D (pSP-D)-mediated inhibition. Van Eijk and colleagues (38) demonstrated that H1-subtype viruses containing several glycosylation sites on HA1 were highly susceptible to inhibition by pSP-D, whereas viruses with a lower number of high-mannose oligosaccharides were markedly more resistant to pSP-D-mediated inhibition. However, it remains to be determined if a similar mechanism applies to H3-subtype viruses.
Interestingly, replacing the HA and NA genes of Sw/MN with those of Sw/ONT resulted in a milder negative impact on virus replication and pathogenicity than the positive impact seen with the reciprocal exchange (Table 1 and Fig. 1). These findings suggest that, although the HA and NA are clearly of substantial influence, they may not be the sole factors controlling influenza virus infectivity in pigs. Previous findings have indicated that genes encoding the “internal” viral proteins also contribute to influenza virus host range in other contexts. Apart from the PB1 gene, which is of human influenza virus origin, the remaining internal genes of Sw/MN are of the classical swine virus lineage (NP, matrix, and nonstructural genes) or avian influenza virus lineage (PA and PB2 genes). In this regard, it is noteworthy that NP was previously found to be a determinant of influenza virus species specificity (33, 36). Furthermore, the polymerase complex (particularly PB2) of avian viruses was found to support replication of the viral genome more effectively at temperatures between 37 and 40°C (24), whereas human viruses were found to grow more efficiently at 33°C (37). Although there is a temperature gradient along mammalian airways (27), the normal body temperature of pigs is higher (38.7 to 39.7°C) than that of humans (36.5 to 37.4°C). Thus, it is conceivable that Sw/MN′s PA and PB2 genes convey a replication advantage for rgSw/MN+ONT HA/NA at the prevailing temperatures in the porcine respiratory tract.
In summary, our findings indicate that HA and NA play important roles in limiting the ability of a wholly human-lineage virus (Sw/ONT) to efficiently infect pigs, although we cannot discount the fact that another viral protein (or constellations of proteins) may further modulate this infectivity in concert with the impact of HA and NA. We have also demonstrated recently, using a human and swine primary respiratory epithelial cell in vitro culture system, that a wide range of H1 and H3 human influenza viruses share the same restricted infectivity phenotype in swine cells as the wholly human Sw/ONT virus (G. A. Landolt, A. I. Karasin, R. A. Brockman-Schneider, J. E. Gern, K. Tewari, M. Suresh, A. S. Gambaryan, K. Shinya, Y. Kawaoka, and C. W. Olsen, unpublished data). Taken together, our results support the hypothesis that a barrier exists to human influenza virus infection in pigs and swine cells, and such a barrier may limit the role of pigs in pandemic virus creation through reassortment of human and avian influenza viruses.
Acknowledgments
This work was supported by funding to C.W.O. from the USDA National Research Initiative Competitive Grants Program (2001-35204-10184) and the NIH NIAID (1 RO1 AI060646).
We thank Gabriele Neumann and Yoshihiro Kawaoka for technical assistance and Julie Mahaney, Chris Haase, Jerry Brokish, and Claudia Hirsch for assistance during the animal experiments.
REFERENCES
- 1.Bean, W. J., M. Schell, J. Katz, Y. Kawaoka, C. Naeve, O. Gorman, and R. G. Webster. 1992. Evolution of the H3 influenza virus hemagglutinin from human and nonhuman hosts. J. Virol. 66:1129-1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beare, A. S., and R. G. Webster. 1991. Replication of avian influenza viruses in humans. Arch. Virol. 119:37-42. [DOI] [PubMed] [Google Scholar]
- 3.Bikour, M. H., E. H. Frost, S. Deslandes, B. Talbot, J. M. Weber, and Y. Elazhary. 1995. Recent H3N2 swine influenza virus with haemagglutinin and nucleoprotein genes similar to 1975 human strains. J. Gen. Virol. 76:697-703. [DOI] [PubMed] [Google Scholar]
- 4.Brown, I. H. 2000. The epidemiology and evolution of influenza viruses in pigs. Vet. Microbiol. 74:29-46. [DOI] [PubMed] [Google Scholar]
- 5.Castrucci, M. R., I. Donatelli, L. Sidoli, G. Barigazzi, Y. Kawaoka, and R. G. Webster. 1993. Genetic reassortment between avian and human influenza A viruses in Italian pigs. Virology 193:503-506. [DOI] [PubMed] [Google Scholar]
- 6.Connor, R. J., Y. Kawaoka, R. G. Webster, and J. C. Paulson. 1994. Receptor specificity in human, avian, and equine H2 and H3 influenza virus isolates. Virology 205:17-23. [DOI] [PubMed] [Google Scholar]
- 7.Couceiro, J. N., J. C. Paulson, and L. G. Baum. 1993. Influenza virus strains selectively recognize sialyloligosaccharides on human respiratory epithelium; the role of the host cell in selection of hemagglutinin receptor specificity. Virus Res. 29:155-165. [DOI] [PubMed] [Google Scholar]
- 8.Easterday, B. C. 1980. Animals in the influenza world. Philos. Trans. R. Soc. Lond. B 288:433-437. [DOI] [PubMed] [Google Scholar]
- 9.Gambaryan, A. S., A. B. Tuzikov, V. E. Piskarev, S. S. Yamnikova, D. K. Lvov, J. S. Robertson, N. V. Bovin, and M. N. Matrosovich. 1997. Specification of receptor-binding phenotypes of influenza virus isolates from different hosts using synthetic sialylglycopolymers: non-egg-adapted human H1 and H3 influenza A and influenza B viruses share a common high binding affinity for 6′-sialyl (N-acetyllactosamine). Virology 232:345-350. [DOI] [PubMed] [Google Scholar]
- 10.Gregory, V., W. Lim, K. Cameron, M. Bennett, S. Marozin, A. Klimov, H. Hall, N. Cox, A. Hay, and Y. P. Lin. 2001. Infection of a child in Hong Kong by an influenza A H3N2 virus closely related to viruses circulating in European pigs. J. Gen. Virol. 82:1397-1406. [DOI] [PubMed] [Google Scholar]
- 11.Hatta, M., P. Halfmann, K. Wells, and Y. Kawaoka. 2002. Human influenza A viral genes responsible for the restriction of its replication in duck intestine. Virology 295:250-255. [DOI] [PubMed] [Google Scholar]
- 12.Hinshaw, V. S., W. J. Bean, Jr., R. G. Webster, and B. C. Easterday. 1978. The prevalence of influenza viruses in swine and the antigenic and genetic relatedness of influenza viruses from man and swine. Virology 84:51-62. [DOI] [PubMed] [Google Scholar]
- 13.Hughes, M. T., M. Matrosovich, M. E. Rodgers, M. McGregor, and Y. Kawaoka. 2000. Influenza A viruses lacking sialidase activity can undergo multiple cycles of replication in cell culture, eggs, or mice. J. Virol. 74:5206-5212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ito, T. 2000. Interspecies transmission and receptor recognition of influenza A viruses. Microbiol. Immunol. 44:423-430. [DOI] [PubMed] [Google Scholar]
- 15.Ito, T., J. N. Couceiro, S. Kelm, L. G. Baum, S. Krauss, M. R. Castrucci, I. Donatelli, H. Kida, J. C. Paulson, R. G. Webster, and Y. Kawaoka. 1998. Molecular basis for the generation in pigs of influenza A viruses with pandemic potential. J. Virol. 72:7367-7373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ito, T., and Y. Kawaoka. 2000. Host-range barrier of influenza A viruses. Vet. Microbiol. 74:71-75. [DOI] [PubMed] [Google Scholar]
- 17.Ito, T., Y. Suzuki, T. Suzuki, A. Takada, T. Horimoto, K. Wells, H. Kida, K. Otsuki, M. Kiso, H. Ishida, and Y. Kawaoka. 2000. Recognition of N-glycolylneuraminic acid linked to galactose by the α2,3 linkage is associated with intestinal replication of influenza A virus in ducks. J. Virol. 74:9300-9305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karasin, A. I., M. M. Schutten, L. A. Cooper, C. B. Smith, K. Subbarao, G. A. Anderson, S. Carman, and C. W. Olsen. 2000. Genetic characterization of H3N2 influenza viruses isolated from pigs in North America, 1977-1999: evidence for wholly human and reassortant virus genotypes. Virus Res. 68:71-85. [DOI] [PubMed] [Google Scholar]
- 19.Kaverin, N. V., A. S. Gambaryan, N. V. Bovin, I. A. Rudneva, A. A. Shilov, O. M. Khodova, N. L. Varich, B. V. Sinitsin, N. V. Makarova, and E. A. Kropotkina. 1998. Postreassortment changes in influenza A virus hemagglutinin restoring HA-NA functional match. Virology 244:315-321. [DOI] [PubMed] [Google Scholar]
- 20.Kida, H., T. Ito, J. Yasuda, Y. Shimizu, C. Itakura, K. F. Shortridge, Y. Kawaoka, and R. G. Webster. 1994. Potential for transmission of avian influenza viruses to pigs. J. Gen. Virol. 75:2183-2188. [DOI] [PubMed] [Google Scholar]
- 21.Landolt, G. A., A. I. Karasin, L. Phillips, and C. W. Olsen. 2003. Comparison of the pathogenesis of two genetically different H3N2 influenza A viruses in pigs. J. Clin. Microbiol. 41:1936-1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Larsen, D. L., A. Karasin, F. Zuckermann, and C. W. Olsen. 2000. Systemic and mucosal immune responses to H1N1 influenza virus infection in pigs. Vet. Microbiol. 74:117-131. [DOI] [PubMed] [Google Scholar]
- 23.Lipatov, A. S., E. A. Govorkova, R. J. Webby, H. Ozaki, M. Peiris, Y. Guan, L. Poon, and R. G. Webster. 2004. Influenza: emergence and control. J. Virol. 78:8951-8959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Massin, P., S. van der Werf, and N. Naffakh. 2001. Residue 627 of PB2 is a determinant of cold sensitivity in RNA replication of avian influenza viruses. J. Virol. 75:5398-5404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Matrosovich, M. N., T. Y. Matrosovich, T. Gray, N. A. Roberts, and H. D. Klenk. 2004. Human and avian influenza viruses target different cell types in cultures of human airway epithelium. Proc. Natl. Acad. Sci. USA 101:4620-4624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Matrosovich, M. N., T. Y. Matrosovich, T. Gray, N. A. Roberts, and H. D. Klenk. 2004. Neuraminidase is important for the initiation of influenza virus infection in human airway epithelium. J. Virol. 78:12665-12667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McFadden, E. R., Jr., B. M. Pichurko, H. F. Bowman, E. Ingenito, S. Burns, N. Dowling, and J. Solway. 1985. Thermal mapping of the airways in humans. J. Appl. Physiol. 58:564-570. [DOI] [PubMed] [Google Scholar]
- 28.Mitnaul, L. J., M. N. Matrosovich, M. R. Castrucci, A. B. Tuzikov, N. V. Bovin, D. Kobasa, and Y. Kawaoka. 2000. Balanced hemagglutinin and neuraminidase activities are critical for efficient replication of influenza A virus. J. Virol. 74:6015-6020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Neumann, G., T. Watanabe, H. Ito, S. Watanabe, H. Goto, P. Gao, M. Hughes, D. R. Perez, R. Donis, E. Hoffmann, G. Hobom, and Y. Kawaoka. 1999. Generation of influenza A viruses entirely from cloned cDNAs. Proc. Natl. Acad. Sci. USA 96:9345-9350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Palmer, D. F., W. R. Dowdle, M. T. Coleman, and G. C. Schild. 1975. Advanced laboratory techniques for influenza diagnosis. United States Department of Health, Washington, D.C.
- 31.Reed, L. J., and H. Muench. 1938. A simple method of estimating fifty per cent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 32.Rogers, G. N., and B. L. D'Souza. 1989. Receptor binding properties of human and animal H1 influenza virus isolates. Virology 173:317-322. [DOI] [PubMed] [Google Scholar]
- 33.Scholtissek, C., H. Burger, O. Kistner, and K. F. Shortridge. 1985. The nucleoprotein as a possible major factor in determining host specificity of influenza H3N2 viruses. Virology 147:287-294. [DOI] [PubMed] [Google Scholar]
- 34.Scholtissek, C., and E. Naylor. 1988. Fish farming and influenza pandemics. Nature 331:215. [DOI] [PubMed] [Google Scholar]
- 35.Skehel, J. J., and D. C. Wiley. 2000. Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annu. Rev. Biochem. 69:531-569. [DOI] [PubMed] [Google Scholar]
- 36.Snyder, M. H., A. J. Buckler-White, W. T. London, E. L. Tierney, and B. R. Murphy. 1987. The avian influenza virus nucleoprotein gene and a specific constellation of avian and human virus polymerase genes each specify attenuation of avian-human influenza A/Pintail/79 reassortant viruses for monkeys. J. Virol. 61:2857-2863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stern, H., and K. C. Tippett. 1963. Primary isolation of influenza viruses at 33 degrees C. Lancet i:1301-1302. [DOI] [PubMed] [Google Scholar]
- 38.van Eijk, M., M. R. White, J. J. Batenburg, A. B. Vaandrager, L. M. van Golde, H. P. Haagsman, and K. L. Hartshorn. 2004. Interactions of influenza A virus with sialic acids present on porcine surfactant protein D. Am. J. Respir. Cell Mol. Biol. 30:871-879. [DOI] [PubMed] [Google Scholar]
- 39.Wagner, R., T. Wolff, A. Herwig, S. Pleschka, and H. D. Klenk. 2000. Interdependence of hemagglutinin glycosylation and neuraminidase as regulators of influenza virus growth: a study by reverse genetics. J. Virol. 74:6316-6323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Webby, R. J., S. L. Swenson, S. L. Krauss, P. J. Gerrish, S. M. Goyal, and R. G. Webster. 2000. Evolution of swine H3N2 influenza viruses in the United States. J. Virol. 74:8243-8251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Webster, R. G., W. J. Bean, O. T. Gorman, T. M. Chambers, and Y. Kawaoka. 1992. Evolution and ecology of influenza A viruses. Microbiol. Rev. 56:152-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wright, P. F., and R. G. Webster. 2001. Orthomyxoviruses, p. 1533-1580. InD. M. Knipe, P. M. Howley, D. E. Griffen, R. A. Lamb, M. A. Martin, B. Roizman, and S. E. Straus (ed.), Fields virology, 4th ed. Lippincott Williams and Wilkins, Philadelphia, Pa.
- 43.Zhou, N. N., D. A. Senne, J. S. Landgraf, S. L. Swenson, G. Erickson, K. Rossow, L. Liu, K. Yoon, S. Krauss, and R. G. Webster. 1999. Genetic reassortment of avian, swine, and human influenza A viruses in American pigs. J. Virol. 73:8851-8856. [DOI] [PMC free article] [PubMed] [Google Scholar]