Abstract
We identified—by randomly amplified polymorphic DNA (RAPD) analysis at the population level followed by DNA differential display, cloning, and sequencing—three prophage DNA fragments (F5, F7, and F10) in Streptococcus agalactiae that displayed significant sequence similarity to the DNA of S. agalactiae and Streptococcus pyogenes. The F5 sequence aligned with a prophagic gene encoding the large subunit of a terminase, F7 aligned with a phage-associated cell wall hydrolase and a phage-associated lysin, and F10 aligned with a transcriptional regulator (ArpU family) and a phage-associated endonuclease. We first determined the prevalence of F5, F7, and F10 by PCR in a collection of 109 strains isolated in the 1980s and divided into two populations: one with a high risk of causing meningitis (HR group) and the other with a lower risk of causing meningitis (LR group). These fragments were significantly more prevalent in the HR group than in the LR group (P < 0.001). Our findings suggest that lysogeny has increased the ability of some S. agalactiae strains to invade the neonatal brain endothelium. We then determined the prevalence of F5, F7, and F10 by PCR in a collection of 40 strains recently isolated from neonatal meningitis cases for comparison with the cerebrospinal fluid (CSF) strains isolated in the 1980s. The prevalence of the three prophage DNA fragments was similar in these two populations isolated 15 years apart. We suggest that the prophage DNA fragments identified have remained stable in many CSF S. agalactiae strains, possibly due to their importance in virulence or fitness.
Streptococcus agalactiae, a bacterial pathogen frequently carried in the normal fecal and/or vaginal flora, is a leading cause of severe bacterial infections in neonates (33). The characterization of S. agalactiae strains, initially by multilocus enzyme electrophoresis (MLEE) (26, 29) and then by multilocus sequence typing (16) and various other methods (5, 39), has revealed the existence of two strongly differentiated lineages in the species. The first is a homogeneous lineage composed of serotype III strains, and the second is a genetically diverse lineage composed of isolates from all capsular serotypes, including serotype III. The distribution of strains responsible for neonatal meningitis between these two phylogenetic groups is nonrandom (26, 29). The S. agalactiae strains responsible for neonatal meningitis would therefore be expected to have particular genetic attributes accounting for their ability to invade the neonatal brain endothelium.
Phenotypic differences between the S. agalactiae strains causing invasive infections in neonates and those colonizing healthy infants have been identified. These differences concern growth characteristics and the production of enzymes and capsular sialic acid (23, 24, 25, 27). However, no molecular data are currently available to confirm the existence of these differences. Serotype III polysaccharide antigens (8), and surface protein antigens, including Rib, C alpha, C alpha-like, and the immunoglobulin A-binding protein, C beta (17, 25, 43), have also been identified as virulence factors (11). However, no single factor can account for the pathogenicity of S. agalactiae species, suggesting that additional factors are involved in pathogenicity.
Prophages have been shown to play an important role in bacterial virulence and genome diversification in the genus Streptococcus (1, 6). Indeed, sequencing of the genome of Streptococcus pyogenes strains has led to the identification of many virulence factors encoded by phages or phage-like elements, demonstrating the importance of prophage acquisition and loss in the generation of different genotypes with novel combinations of proven and putative virulence factor genes (1, 3, 4, 7). The S. agalactiae strains able to invade the central nervous system (CNS) of neonates are found in widely divergent lineages of S. agalactiae (26, 29), possibly due to various episodes of horizontal transfer, which may have involved phages. Regions resembling prophages, with a mosaic structure including segments highly similar to various bacteriophages, have been identified in sequenced S. agalactiae strains (40, 41).
In this study, we tried to identify new prophage-related DNA elements in S. agalactiae genomes by randomly amplified polymorphic DNA (RAPD) analysis followed by differential display of DNA, as previously described (31). We aimed to identify variable genetic elements located outside the core genome as recently defined by Tettelin et al. (40). We identified, cloned, and sequenced three prophage DNA fragments displaying significant alignments with DNA sequences present in the recently sequenced S. agalactiae and S. pyogenes genomes. We used PCR to evaluate the prevalence of these fragments in 149 strains, including the major genetic subgroups of S. agalactiae. With this approach, we showed that these three fragments were associated with populations of S. agalactiae strains able to invade the CNS of neonates.
MATERIALS AND METHODS
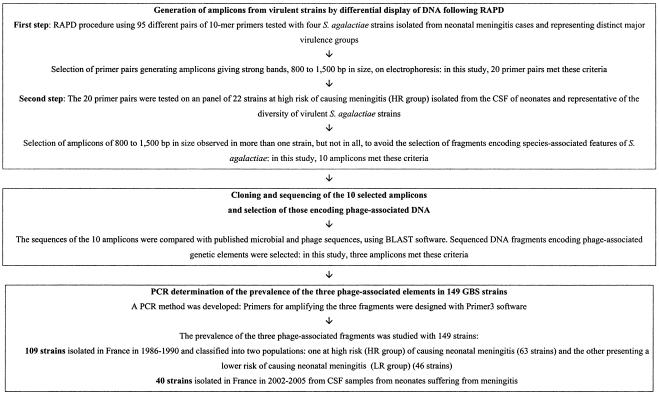
The procedure used is presented in a flowchart (Fig. 1).
FIG. 1.
Flowchart showing the various steps in the procedure used in this study.
Bacterial isolates.
A national collection of 149 S. agalactiae strains was used in this study (Table 1). The first 109 strains were isolated in France 15 to 19 years ago and included 54 strains from cerebrospinal fluid (CSF) samples from neonates suffering from meningitis, and 55 non-CSF strains isolated from asymptomatic women and neonates. Previous characterization, by MLEE, of these 109 strains (29) allowed us to classify them into two populations. The first population consisted of 63 strains, mostly isolated from the CSF (54 strains), belonging to the electrophoretic types (ETs) containing strains isolated from neonatal CSF. The second population of strains consisted of 46 strains isolated from vaginal and gastric samples belonging to ETs that contained no strains from the CSF. The strains belonging to the first population were considered more likely to be able to invade the CSF of neonates than strains of the second population. We therefore named the first population “HR group” (for higher-risk group) and the second “LR group” (for lower-risk group).
TABLE 1.
Characteristics of the 149 group B streptococcus strains studied
| Date of isolation (yr) | Groupa | No. of strains | Period (yr) | No. of strains isolated from:
|
No. of strains of serotype:
|
No. of strains from MLEE division:
|
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| CSF | Vaginal samples | Gastric samples | III | Others | I | II | NDb | ||||
| 1986-1990 | HR | 63 | 1986-1990 | 54 | 9 | 44 | 19 | 29 | 34 | ||
| 1986-1990 | LR | 46 | 1986-1990 | 25 | 21 | 9 | 37 | 9 | 37 | ||
| 2002-2005 | 40 | 2002-2005 | 40 | 32 | 8 | 40 | |||||
The HR group of strains comprises the strains isolated from CSF samples from neonates suffering from meningitis and strains isolated from vaginal samples belonging to all of the ETs containing strains isolated from neonatal CSF. The strains of the LR group were isolated from vaginal and gastric samples and belonged to ETs that did not contain strains from CSF. The HR group strains are considered more likely to invade the CSF of neonates than LR group strains.
ND, not defined.
We also compared the CSF strains isolated in the 1980s with 40 additional S. agalactiae strains isolated in France in 2002 to 2005 from the CSF samples of neonates suffering from meningitis.
Differential display of DNA following RAPD.
RAPD involves the molecular epidemiological characterization of strains to detect genetic specificities within subgroups of bacteria (31, 42). We used a multistep approach: (i) generation of amplicons from virulent strains by multiple random amplification and (ii) cloning and sequencing of the selected amplicons (Fig. 1).
Generation of amplicons.
Random amplification was carried out by an RAPD procedure (9), using 95 different pairs of 10-mer primers selected from five oligonucleotide 10-mer kits—OPN, OPAM, OPO, OPI, and OPR (Operon Technologies, Inc., Alameda, California)—on the basis of having a G+C content of 40 to 77% and no palindromic sequences. We retained 20 primer pairs that generated amplicons giving strong bands of 800 and 1.500 bp in size on electrophoresis. We aimed (i) to sequence these amplicons for the identification of coding sequences related to putative phage elements and (ii) to amplify these sequences by PCR from our collection of strains. The Raoult ladder (Qbiogene, France) was used as a molecular size standard. The 20 primer pairs were tested on an initial panel of 22 HR group strains isolated from the CSF of neonates and selected on the basis of MLEE data (26) as representative of the diversity of virulent S. agalactiae strains.
Cloning and sequencing of the selected amplicons.
Tettelin et al. (40) recently showed that genes associated with mobile and extrachromosomal elements are abundant in the S. agalactiae genome but only poorly represented within the core genome of S. agalactiae species. We therefore aimed to select amplicons of 800 to 1,500 bp in size observed in more than one strain, but not in all, to avoid the selection of fragments encoding species-associated features of S. agalactiae and to take into account the variable part of the genome that may contain virulence-related genes. Ten fragments meeting these criteria were selected, extracted, and purified from the agarose plugs, using the GFXTM PCR DNA gel band purification kit (Amersham Biosciences, Orsay France). Each DNA fragment was inserted into pCR 2.1 (TA cloning kit; Invitrogen, Cergy Pontoise, France). The PCR product ligated into pCR 2.1 was used to transform Escherichia coli TOP10 (Invitrogen). The bacteria were lysed, and plasmid DNA was purified from the lysate with the Wizard plus SV Minipreps DNA purification system (Promega, Charbonnières, France). We then carried out PCR with M13R and T7 promoter primers to amplify insert sequences. PCR was carried out in a final volume of 50 μl containing PCR buffer (10 mM Tris-HCl, 50 mM KCl, 1.5 mM MgCl2, pH 8.3), 0.2 mM concentrations of each deoxynucleoside triphosphate (Amersham Biosciences), 0.2 μM concentrations of each primer (Eurogentec, Angers, France), and 0.5 U Taq polymerase (Perkin Elmer, Saint Quentin en Yvelines, France). The cycling conditions were as follows: initial denaturation at 94°C for 4 min, followed by 25 cycles at 94°C for 1 min, 52°C for 1 min, and 72°C for 1 min (additional 10 min at 72°C for the last extension). The products were separated by electrophoresis in a 1.6% agarose gel in TBE buffer (8.9 mM Tris, 8.9 mM boric acid, 0.25 mM EDTA, pH 8.0). PCR products were purified on Microcon concentrators (Amicon, Epernon, France). Nucleotide sequences were determined by cycle sequencing, based on the chain termination method of Sanger and using the ABI Prism 3100-Avant genetic analyzer (Applied Biosystem, Cergy Pontoise, France) and the BigDye Terminator, version 3.0, chemistry premix kit. The sequences were compared with published microbial and phage sequences, using BLAST software (http://www.ncbi.nlm.nih.gov/BLAST/).
PCR determination of the prevalence of phage-associated elements in 149 S. agalactiae strains.
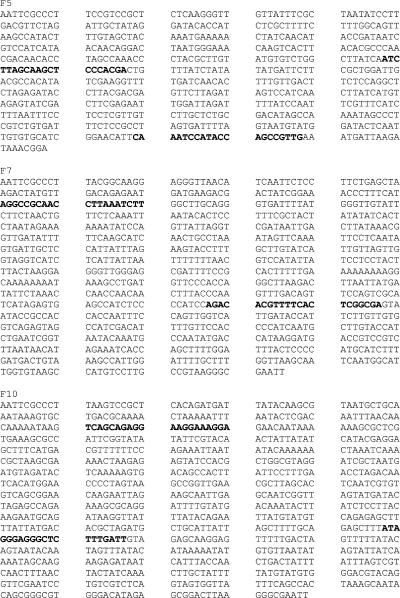
Three of the 10 sequenced DNA fragments were selected, as they encoded phage-associated genetic elements. A PCR method was developed for assessing the prevalence of three phage-associated fragments in our collection of 149 strains. Primers for amplifying the three fragments were designed with primer3 software (http://frodo.wi.mit.edu/cgi-bin/primer3/primer3_www.cgi), and validated by checking that they amplified the fragments in the S. agalactiae strains found to contain these fragments in the initial step of differential display (Fig. 2). PCR was carried out in a final volume of 20 μl containing PCR buffer, 0.2 mM concentrations of each deoxynucleoside triphosphate, 0.5 μM concentrations of each primer, 1 U Taq polymerase, and 25 ng of template DNA. The cycling conditions were as follows: initial denaturation at 94°C for 4 min, followed by 25 cycles of 94°C for 30 s, 45°C for 30 s, and 72°C for 1 min (additional 7 min at 72°C for the final extension). The products were separated by electrophoresis in a 1.6% agarose gel in TBE buffer.
FIG. 2.
DNA sequences of fragments F5, F7, and F10 and selection of primer sequences for PCR. Primer sequences are shown in boldface type.
RESULTS
Differential display of DNA following RAPD.
RAPD amplification carried out with 20 pairs of primers generated 10 amplicons (F1 to F10), selected on the basis of size and representation in strains representative of the diversity of virulent S. agalactiae strains. These 10 amplicons were cloned and sequenced. All but one (F2) displayed significant sequence alignment with DNA sequences found in the published complete genome sequences of S. agalactiae and/or S. pyogenes in international genomic databases (Tables 2 and 3). The sequences of six fragments (F1, F3, F4, F6, F8, and F10) aligned with DNA sequences found in the published genome sequence of S. agalactiae (14, 40, 41). The sequences of four fragments (F5, F7, F9, and F10) displayed significant alignment with DNA sequences found in published S. pyogenes genome sequences (2, 4, 13, 15, 28, 32, 36, 37). On account of our objectives, we studied in more detail the three DNA fragments (F5, F7, and F10) that displayed significant alignment with prophagic DNA sequences (Fig. 2). These three prophagic DNA fragments displayed significant alignment with known phage-associated DNA sequences from S. pyogenes genomes, and one (F10) also displayed significant alignment with the prophage SA1 DNA sequence in the S. agalactiae 2603V/R genome and the prophage LambdaSa03 in the S. agalactiae A909 genome (Table 3). The significant alignments of the three DNA fragment sequences with the S. pyogenes and S. agalactiae genomes are shown in Fig. 3.
TABLE 2.
Alignments of 10 DNA fragments identified by differential display of DNA with published S. agalactiae genome sequences
| Fragment designation | Genome identity | Sequence including fragment | Protein encoded |
|---|---|---|---|
| F1 | NEM316 and 2603V/R | rpoC gene | ARN polymerase β-subunit |
| F3 | NEM316 | gbs1135 | Putative protein |
| 2603V/R | SAG1287 | Putative protein sharing homology with a transposon protein (Tn5252, Orf26) | |
| F4 | NEM316 | ccpA gene | Catabolite control protein A |
| 2603V/R | SAG0707 | RegM gene transcriptional regulator | |
| F5a | |||
| F6 | NEM316 | gbs0299 | Putative protein |
| gbs0300 | |||
| 2603V/R | SAG0311 | Conserved putative protein | |
| F7a | |||
| F8 | NEM316 | gbs0504 | Putative protein |
| gbs0505 | Putative protein | ||
| 2603V/R | SAG0457 | Conserved putative protein | |
| SAG0458 | Protein TIGR00048 | ||
| F9b | |||
| F10a |
Results are shown in Table 3.
Results were similar to those obtained with F7.
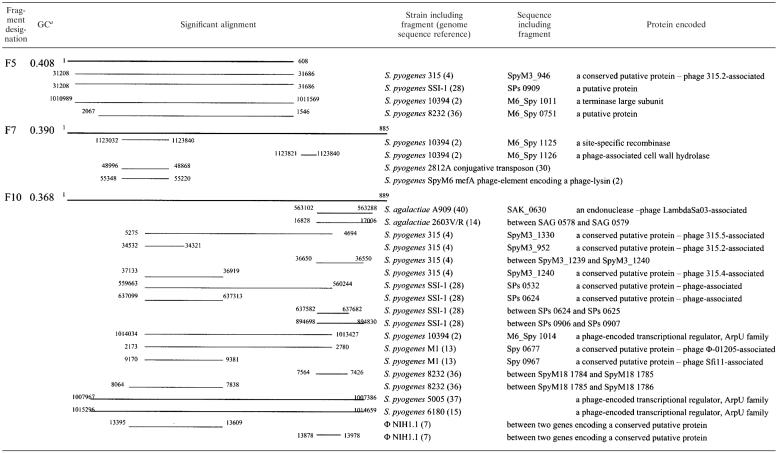
TABLE 3.
Significant alignments of three prophage DNA fragments with published S. pyogenes and S. agalactiae genome sequences
GC, % G+C.
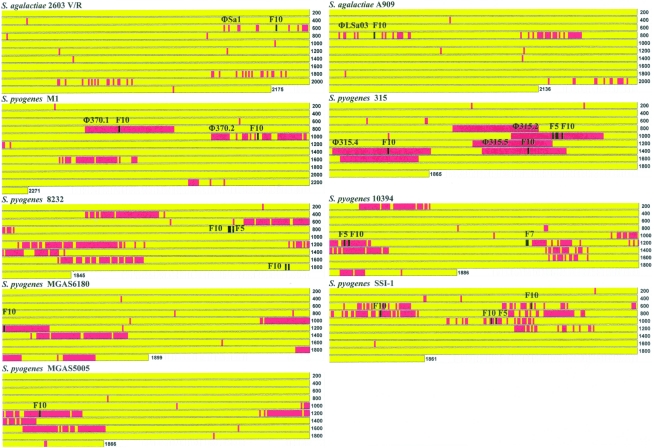
FIG. 3.
Localization of the significant alignments of F5, F7, and F10 within nine sequenced genomes. Loci harboring prophagic genes are shown in red blocks. Loci harboring significant alignments of F5, F7, and F10 are shown in black blocks.
Fragment F5.
Four sequences, originating from four of the five completely sequenced S. pyogenes genomes, displayed significant alignment with the 609-bp sequence of fragment F5 (more than 80% identity). In S. pyogenes strain 315, the sequence that aligned with F5 was present in the SpyM3_946 gene, which is thought to have been inserted into the φ315.2 genome and encodes a putative phage protein. In S. pyogenes SSI-1 and S. pyogenes 10394, sequences displaying significant alignments with F5 were also found inserted into prophage DNA elements in the genome. Furthermore, in S. pyogenes 10394, the sequence that aligned with F5 was found within the M6_Spy1011 gene, encoding a protein identified as the large subunit of a terminase. In these three cases, F5 was found in the neighborhood of F10. Only in S. pyogenes 8232 did the sequence aligning with F5 not seem to encode a putative protein or to be associated with a phage.
Fragment F7.
A significant alignment with three sequences previously identified in S. pyogenes genomes was observed over 138 of the 885 bp of the F7 fragment. These fragments were a fragment from S. pyogenes 10394, a fragment from the S. pyogenes 2812A transposon, and a fragment from the S. pyogenes SpyM6 mef(A) phage element. Thus, in two of these three cases, the observed alignments with F7 identified prophage-associated genes. In S. pyogenes 10394, the sequence aligning with F7 was found in a prophage, more specifically in the M6_Spy1125 gene encoding a site-specific recombinase, and in the M6_Spy1126 gene encoding a phage-associated cell wall hydrolase. In the S. pyogenes SpyM6 mef(A) phage element, the sequence aligning with F7 was found in a gene encoding a phage-associated lysin.
Fragment 10.
Nineteen sequences, originating from the genomes of seven different S. pyogenes strains, S. agalactiae 2603V/R, S. agalactiae A909, and the prophage NH1.1, displayed significant alignment with various parts of the 889-bp sequence of the F10 fragment. These significant alignments concerned genes encoding phage-associated proteins, with the exception of the two alignments in the MGAS 8232 strain (Fig. 3). Six of these 19 significant alignments, covering 502 to 608 bp, concerned the same part of the F10 fragment. The F10 fragment displayed significant alignment with the genome of S. agalactiae strain A909 and S. pyogenes strains 315, SSI-1, 10394, M1, 5005, and 6180 (Table 3). It was found in the SAK_0630 gene of the S. agalactiae strain A909 encoding a prophage LambdaSa03 endonuclease, in the SpyM3_1330 gene of the φ315.5 genome of S. pyogenes 315, and in a gene encoding a transcriptional regulator from the ArpU family (autolysin regulatory proteins) in S. pyogenes 10394, 5005, and 6180 (20). In all cases, the sequences aligning with the various parts of the F10 fragment were located in the middle of the prophagic region, regardless of the phage concerned. Similarly, the sequence originating from the completed genome sequence of S. agalactiae strain 2603V/R and displaying significant alignment with the F10 fragment over 178 bp was also located in the middle part of prophage SA1, between the SAG 0578 and SAG 0579 genes (Fig. 3).
Determination by PCR of the prevalence of the prophage DNA fragments in HR and LR groups of strains.
PCR was carried out for the 109 strains (Fig. 2) previously studied by MLEE and comprising the HR (63 strains) and LR (56 strains) groups. We determined the prevalence of the F5, F7, and F10 fragments in each group (Table 4) and found that F10 was the most frequent (50/109, 46%), with F5 and F7 found in about one-fifth of the strains tested (21/109, 19% and 23/109, 21%, respectively). HR group strains (high risk of meningitis) contained at least one fragment in 67% of cases (42/63) versus only 37% (17/46) of cases for LR group (low risk of meningitis) (P = 0.002). The significance of the difference in prevalence between HR and LR groups was higher if we considered the accumulation of prophage DNA fragments (at least two fragments) (Table 4).
TABLE 4.
Prevalence of the three DNA fragments in the HR and LR groups of S. agalactiae strains and according to MLEE data and serotype
| Strain groupa | No. of strains | No. of strains (%) with positive detection ofb:
|
|||||
|---|---|---|---|---|---|---|---|
| F5 | F7 | F10 | At least:
|
||||
| 1 fragment | 2 fragments | 3 fragments | |||||
| All strains | |||||||
| HR | 63 | 17 (27) | 19 (30) | 38 (60) | 42 (67) | 28 (44) | 3 (5) |
| LR | 46 | 4 (9) | 4 (9) | 12 (26) | 17 (37) | 3 (6) | |
| Total | 109 | 21 (19) | 23 (21) | 50 (48) | 59 (54) | 31 (28) | 3 (3) |
| MLEE division I | |||||||
| HR | 29 | 9 (31) | 2 (7) | 12 (41) | 14 (48) | 9 (31) | |
| LR | 9 | 1 (11) | 1 (11) | 2 (22) | 4 (44) | ||
| Total | 38 | 10 (26) | 3 (8) | 14 (37) | 18 (47) | 9 (24) | |
| MLEE division II | |||||||
| HR | 34 | 8 (23) | 17 (50) | 26 (76) | 28 (80) | 19 (56) | 3 (9) |
| LR | 37 | 3 (8) | 3 (8) | 10 (27) | 13 (36) | 3 (8) | |
| Total | 71 | 11 (15) | 20 (28) | 36 (51) | 28 (58) | 22 (31) | 3 (4) |
| Serotype III | |||||||
| HR | 45 | 12 (27) | 15 (33) | 26 (58) | 28 (62) | 22 (49) | 3 (7) |
| LR | 11 | 1 (9) | 2 (18) | 2 (18) | 5 (45) | ||
| Total | 56 | 13 (23) | 17 (30) | 28 (50) | 33 (59) | 22 (39) | 3 (5) |
| Other serotypes | |||||||
| HR | 18 | 5 (28) | 4 (22) | 12 (67) | 14 (78) | 6 (33) | 1 (6) |
| LR | 35 | 3 (8) | 2 (6) | 10 (28) | 12 (34) | 3 (8) | |
| Total | 53 | 8 (15) | 6 (11) | 22 (41) | 26 (49) | 9 (17) | 1 (2) |
HR group strains are more likely invade the CSF of neonates than LR group strains.
Prevalences of the three fragments within the HR and LR groups of strains were compared by chi-square test, with significant differences indicated in boldface type. P values are as follows: for the group of all strains, F5, 0.017; F7, 0.007; F10, <0.001; 1 fragment, 0.002; 2 fragments, <0.001; 3 fragments, 0.107; for MLEE division I, F5, 0.233; F7, 0.567; F10, 0.264; 1 fragment, 0.573; 2 fragments, 0.061; for MLEE division II, F5, 0.073; F7, 0.001; F10, 0.001; 1 fragment, 0.001; 2 fragments, 0.001; 3 fragments, 0.104; for serotype III, F5, 0.206; F7, 0.277; F10, 0.018; 1 fragment, 0.249; 2 fragments, 0.002; 3 fragments, 0.512; for other serogroups, F5, 0.077; F7, 0.093; F10, 0.008; 1 fragment, 0.003; 2 fragments, 0.032; 3 fragments, 0.339.
PCR determination of the prevalence of the prophage DNA fragments according to MLEE divisions.
When the strains of each MLEE division were examined separately, only strains from the heterogeneous MLEE division II showed a significant difference in prevalence between HR and LR groups. Indeed, 80% of the HR group strains (28/34) had at least one of the three prophagic fragments versus only 36% (13/37) of the LR group strains (P < 0.001). However, the F5 fragment, considered alone, was found to be associated with strains from MLEE division I, especially HR group (9/29, 31%) strains, more frequently than with strains belonging to LR group (1/9, 11%) and MLEE division II (11/71, 15%). This resulted in a nonsignificant difference in prevalence between HR and LR groups from MLEE division I, with 9 of the 29 HR group strains (31%) having at least two fragments versus none of the LR group strains (P = 0.061).
PCR determination of the prevalence of the prophage DNA fragments according to serotype.
S. agalactiae serotype III strains are considered to present a high risk for meningitis (26). We therefore studied the strains of the HR and LR groups belonging to serotype III separately from those of other serotypes. In the serotype III population, the HR group strains showed a higher prevalence of prophage DNA fragments than LR group strains (Table 4). The difference was significant for F10, with 58% of the HR group strains (26/45) having this fragment versus only 18% (2/11) of the LR group strains (P = 0.018). Similarly, in the population of strains of other serotypes, the HR group strains showed a higher prevalence of prophage DNA fragments than LR group strains. The difference was significant for F10, which was present in 67% of the HR group strains (12/18) versus only 28% (10/35) of the LR group strains (P = 0.008).
Determination by PCR of the prevalence of the prophage DNA fragments in meningitis strains isolated in 2002 to 2005.
We tested 40 CSF strains isolated between 2002 and 2005: 7 tested positive for F5 (17%), 14 tested positive for F7 (35%), and 23 tested positive for for F10 (57%). For the CSF strains isolated in the 1986 to 1990 period, the prevalence was 27% for F5, 30% for F7, and 60% for F10. There was therefore no significant difference in the prevalence of these three prophagic DNA fragments between the CSF strains isolated in these two periods separated by about 15 years.
DISCUSSION
A recent analysis of eight genomes of S. agalactiae strains showed that genes associated with mobile and extrachromosomal elements are abundant, supporting the hypothesis that most specific traits depend on lateral gene transfer events (40). The authors suggested that “serotype or core-genome based methods fail to take into account the variable genome in which many of the virulence-related genes might reside” (40). We therefore need to develop strategies taking into account this variable part of the bacterial genome and populations of strains, if we are to identify virulence-related DNA elements (40). Using a strategy based on differential display of DNA following RAPD, we identified three DNA elements (F5, F7, and F10) that displayed significant alignment with previously identified prophage sequences from S. agalactiae and S. pyogenes. F5 significantly aligned with a prophage gene encoding the large subunit of a terminase, F7 aligned with sequences encoding a phage-associated cell wall hydrolase and a phage-associated lysin, and F10 aligned with sequences encoding a transcriptional regulator and an endonuclease. These three fragments were significantly more frequent in strains from ETs that contained strains from the CSF of neonates and recently isolated CSF strains than in strains from ETs that did not contain S. agalactiae strains from the CSF (P < 0.001). This difference was particularly marked if we considered the accumulation of prophage DNA fragments (at least two fragments) (Table 4).
MLEE has been successfully used in studies of population genetics (34). MLEE data for S. agalactiae species were first reported by Musser et al. (26). Quentin et al. and Rolland et al. (29, 30) confirmed these findings by correlating them with data obtained in more recent studies. Indeed, the high-virulence clone identified by MLEE (ET-1 of Musser et al. [26] and MLEE division I of Quentin et al. [29]) corresponds to clone III-3 defined on the basis of restriction digestion patterns for genomic DNA (38), ST-17 identified by multilocus sequence typing (26), and GIII defined by pulsed-field gel electrophoresis (5). Based on these strong correlations, we believe that the populations of strains used in this study, defined on the basis of MLEE data, accurately represented a population of strains associated with a high risk of causing meningitis (HR group) and a population of strains associated with a lower risk of causing meningitis (LR group), each of which were distributed in both MLEE divisions.
The association found between the presence of prophage DNA fragments F5, F7, and F10 and groups of S. agalactiae strains able to invade the CNS of neonates suggests that genetic events contemporary to lysogeny may have increased the ability of strains to invade the brain endothelium. As recently pointed out by Brussow et al. (6), temperate phages affect the fitness of bacteria as anchor points for genomic rearrangements, via gene disruption, by protecting against lytic infection, by lysis of competing strains through prophage induction, and via the introduction of new fitness factors. The prophage DNA fragments described here displayed significant alignments with S. agalactiae and S. pyogenes prophage genes encoding proteins with important functions. In S. pyogenes, horizontal transfer events have led to the emergence of increasingly pathogenic strains, mostly by the transfer of genes encoding virulence factors (1, 13). In S. agalactiae, the presence of F5, F7, and F10 may indicate the possible unidentified contemporary horizontal transfer of virulence genes. Indeed, sequencing of the genome of S. agalactiae 2603V/R predicted the production of 1333 proteins, including 623 of unknown function and 219 that did not match any entry in databases (41). A recent analysis of the genomic sequence of S. agalactiae strains representing the major disease-causing serotypes of S. agalactiae showed that about one-third of the shared genes encoded putative proteins and proteins of unknown function (40). However, S. agalactiae strains have to survive in several ecological environments (vagina, cervix, amniotic fluid, and blood) and cross a large variety of anatomical barriers (pulmonary filter and brain endothelium) before invading the CNS of neonates. No major virulence factor in S. agalactiae has clearly been identified as related to neonatal meningitis. The mechanisms by which lysogeny has increased S. agalactiae virulence are therefore probably more complex than the transfer of a single virulence gene. Lysogenic S. agalactiae strains may have several fitness factors favoring metabolic activity and growth, as demonstrated for lysogenic strains of E. coli in the 1970s (10, 12, 19). This would account for the S. agalactiae strains causing invasive infections in neonates having growth characteristics, enzyme production, and capsular sialic acid production levels different from those of strains colonizing healthy infants that did not cause invasive disease (23, 24, 26, 27). In addition, the correlation between the identification of “virulent clones” by MLEE—a tool that explores metabolic enzymes playing a major role in bacterial life—and the presence of the prophage DNA fragments identified, also provides evidence that the pathogenicity of some S. agalactiae genogroups should be seen more in terms of “fitness factor” mediation than in terms of pathogenicity island acquisition.
The association we found between the DNA prophage fragments F5, F7, and F10 and groups of S. agalactiae strains able to invade the CNS of neonates was stronger for strains from MLEE division II (80% for group HR and 58% for all strains) than for strains from MLEE division I (48% for group HR and 47% for all strains). Only F5 was more frequent in strains from MLEE division I associated with a high risk of meningitis (Table 2) (26, 29). Horizontal transfer via phages is a major mechanism of diversification in bacterial species. It also activates the SOS system, promoting genome-wide mutations in the host and in housekeeping genes, particularly in stressful environmental conditions (18, 21, 22, 35, 44). The two major phylogenetic populations comprising the species S. agalactiae, as represented by MLEE divisions I and II, are markedly distant and different in terms of genetic diversity. A higher level of allelic variation is observed in strains from MLEE division II (26, 29). The high prevalence of multiple prophage DNA fragments in strains from the more heterogeneous MLEE division II may indicate the greater exposure of strains of this phylogenetic group than of MLEE division I strains to environmental and ecological pressures.
The association we found between the DNA prophage fragments F5, F7, and F10 and groups of S. agalactiae strains able to invade the CNS of neonates did not depend on strain serotypes. This provides further evidence that serotyping is not an appropriate technique for the identification of virulent lineages of strains, consistent with the recent conclusions of Tettelin et al. (40).
The prevalence of the three prophage DNA fragments (F5, F7, and F10) significantly associated with S. agalactiae strains able to invade the CNS of neonates was similar in two populations of CSF strains isolated 15 years apart. This suggests that the identified prophage DNA fragments, which may be involved in the virulence of some groups of S. agalactiae strains, have remained stable over time. These prophage DNA fragments may therefore be one of the few rearrangements that have remained stable during the evolution of S. agalactiae (40), possibly due to their importance for virulence or fitness.
In conclusion, our data suggest that lysogeny has played a role in the genetic diversification of S. agalactiae and in the emergence of strains able to invade the CNS of neonates. The molecular characterization of S. agalactiae prophages and studies of the impact of these prophage DNA elements on the pathogenicity of strains tested in animal and/or cellular models should increase our understanding of the impact of lysogeny on the virulence of S. agalactiae strains.
REFERENCES
- 1.Banks, D. J., S. B. Beres, and J. M. Musser. 2002. The fundamental contribution of phages to GAS evolution, genome diversification and strain emergence. Trends Microbiol. 10:515-521. [DOI] [PubMed] [Google Scholar]
- 2.Banks, D. J., S. F. Porcella, K. D. Barbian, S. B. Beres, L. E. Philips, J. M. Voyich, F. R. DeLeo, J. M. Martin, G. A. Somerville, and J. M. Musser. 2004. Progress toward characterization of the group A Streptococcus metagenome: complete genome sequence of a macrolide-resistant serotype M6 strain. J. Infect. Dis. 190:727-738. [DOI] [PubMed] [Google Scholar]
- 3.Banks, D. J., S. F. Porcella, K. D. Barbian, J. M. Martin, and J. M. Musser. 2003. Structure and distribution of an unusual chimeric genetic element encoding macrolide resistance in phylogenetically diverse clones of group A Streptococcus. J. Infect. Dis. 188:1898-1908. [DOI] [PubMed] [Google Scholar]
- 4.Beres, S. B., G. L. Sylva, D. E. Sturdevant, C. N. Granville, M. Liu, S. M. Ricklefs, A. R. Whitney, L. D. Parkins, N. P. Hoe, G. J. Adams, D. E. Low, F. R. DeLeo, A. McGeer, and J. M. Musser. 2004. Genome-wide molecular dissection of serotype M3 group A Streptococcus strains causing two epidemics of invasive infections. Proc. Natl. Acad. Sci. USA 101:11833-11838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bidet, P., N. Brahimi, C. Chalas, Y. Aujard, and E. Bingen. 2003. Molecular characterization of serotype III group B-Streptococcus isolates causing neonatal meningitis. J. Infect. Dis. 188:1132-1137. [DOI] [PubMed] [Google Scholar]
- 6.Brussow, H., C. Canchaya, and W. D. Hardt. 2004. Phages and the evolution of bacterial pathogens: from genomic rearrangements to lysogenic conversion. Microbiol. Mol. Biol. Rev. 68:560-602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Canchaya, C., F. Desiere, W. M. McShan, J. J. Ferretti, J. Parkhill, and H. Brussow. 2002. Genome analysis of an inducible prophage and prophage remnants integrated in the Streptococcus pyogenes strain SF370. Virology 302:245-258. [DOI] [PubMed] [Google Scholar]
- 8.Chaffin, D. O., S. B. Beres, H. H. Yim, and C. E. Rubens. 2000. The serotype of type Ia and III group B streptococci is determined by the polymerase gene within the polycistronic capsule operon. J. Bacteriol. 182:4466-4477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chatellier, S., C. Ramanantsoa, P. Harriau, K. Rolland, A. Rosenau, and R. Quentin. 1997. Characterization of Streptococcus agalactiae strains by randomly amplified polymorphic DNA analysis. J. Clin. Microbiol. 35:2573-2579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chibani-Chennoufi, S., A. Bruttin, M. L. Dillmann, and H. Brussow. 2004. Phage-host interaction: an ecological perspective. J. Bacteriol. 186:3677-3686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Doran, K. S., and V. Nizet. 2004. Molecular pathogenesis of neonatal group B streptococcal infection: no longer in its infancy. Mol. Microbiol. 54:23-31. [DOI] [PubMed] [Google Scholar]
- 12.Edlin, G., L. Lin, and R. Kudrna. 1975. Lambda lysogens of E. coli reproduce more rapidly than non-lysogens. Nature 255:735-737. [DOI] [PubMed] [Google Scholar]
- 13.Ferretti, J. J., W. M. McShan, D. Ajdic, D. J. Savic, G. Savic, K. Lyon, C. Primeaux, S. Sezate, A. N. Suvorov, S. Kenton, H. S. Lai, S. P. Lin, Y. Qian, H. G. Jia, F. Z. Najar, Q. Ren, H. Zhu, L. Song, J. White, X. Yuan, S. W. Clifton, B. A. Roe, and R. McLaughlin. 2001. Complete genome sequence of an M1 strain of Streptococcus pyogenes. Proc. Natl. Acad. Sci. USA 98:4658-4663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glaser, P., C. Rusniok, C. Buchrieser, F. Chevalier, L. Frangeul, T. Msadek, M. Zouine, E. Couve, L. Lalioui, C. Poyart, P. Trieu-Cuot, and F. Kunst. 2002. Genome sequence of Streptococcus agalactiae, a pathogen causing invasive neonatal disease. Mol. Microbiol. 45:1499-1513. [DOI] [PubMed] [Google Scholar]
- 15.Green, N. M., S. Zhang, S. F. Porcella, M. J. Nagiec, K. D. Barbian, S. B. Beres, R. B. LeFebvre, and J. M. Musser. 2005. Genome sequence of a serotype M28 strain of group a streptococcus: potential new insights into puerperal sepsis and bacterial disease specificity. J. Infect. Dis. 192:760-770. [DOI] [PubMed] [Google Scholar]
- 16.Jones, N., J. F. Bohnsack, S. Takahashi, K. A. Oliver, M. S. Chan, F. Kunst, P. Glaser, C. Rusniok, D. W. Crook, R. M. Harding, N. Bisharat, and B. G. Spratt. 2003. Multilocus sequence typing system for group B Streptococcus. J. Clin. Microbiol. 41:2530-2536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lachenauer, C. S., R. Creti, J. L. Michel, and L. C. Madoff. 2000. Mosaicism in the alpha-like protein genes of group B streptococci. Proc. Natl. Acad. Sci. USA 97:9630-9635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lane, D., J. Cavaille, and M. Chandler. 1994. Induction of the SOS response by IS1 transposase. J. Mol. Biol. 242:339-350. [DOI] [PubMed] [Google Scholar]
- 19.Lin, L., R. Bitner, and G. Edlin. 1977. Increased reproductive fitness of Escherichia coli lambda lysogens. J. Virol. 21:554-559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mar Lleo, M., R. Fontana, and M. Solioz. 1995. Identification of a gene (arpU) controlling Muramidase-2 export in Enterococcus hirae. J. Bacteriol. 177:5912-5917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martiel, J. L., and M. Blot. 2002. Transposable elements and fitness of bacteria. Theor. Popul. Biol. 61:509-518. [DOI] [PubMed] [Google Scholar]
- 22.Matic, I., F. Taddei, and M. Radman. 2004. Survival versus maintenance of genetic stability: a conflict of priorities during stress. Res. Microbiol. 155:337-341. [DOI] [PubMed] [Google Scholar]
- 23.Mattingly, S. J., J. J. Maurer, E. K. Eskew, and F. Cox. 1990. Identification of a high-virulence clone of serotype III Streptococcus agalactiae by growth characteristics at 40 degrees C. J. Clin. Microbiol. 28:1676-1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maurer, J. J., and S. J. Mattingly. 1988. In vitro method to differentiate isolates of type III Streptococcus agalactiae from symptomatic and asymptomatic patients. J. Clin. Microbiol. 26:686-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mawn, J. A., A. J. Simpson, and S. R. Heard. 1993. Detection of the C protein gene among group B streptococci using PCR. J. Clin. Pathol. 46:633-636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Musser, J. M., S. J. Mattingly, R. Quentin, A. Goudeau, and R. K. Selander. 1989. Identification of a high-virulence clone of type III Streptococcus agalactiae (group B Streptococcus) causing invasive neonatal disease. Proc. Natl. Acad. Sci. USA 86:4731-4735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nagano, Y., N. Nagano, S. Takahashi, A. Suzuki, and Y. Okuwaki. 1989. Sialic acid levels and lag time of growth in chemically defined medium containing 200 mM phosphate among strains of various serotypes of Streptococcus agalactiae. J. Clin. Microbiol. 27:2148-2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nakagawa, I., K. Kurokawa, A. Yamashita, M. Nakata, Y. Tomiyasu, N. Okahashi, S. Kawabata, K. Yamazaki, T. Shiba, T. Yasunaga, H. Hayashi, M. Hattori, and S. Hamada. 2003. Genome sequence of an M3 strain of Streptococcus pyogenes reveals a large-scale genomic rearrangement in invasive strains and new insights into phage evolution. Genome Res. 13:1042-1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Quentin, R., H. Huet, F. S. Wang, P. Geslin, A. Goudeau, and R. K. Selander. 1995. Characterization of Streptococcus agalactiae strains by multilocus enzyme genotype and serotype: identification of multiple virulent clone families that cause invasive neonatal disease. J. Clin. Microbiol. 33:2576-2581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rolland, K., C. Marois, V. Siquier, B. Cattier, and R. Quentin. 1999. Genetic features of Streptococcus agalactiae strains causing severe neonatal infections, as revealed by pulsed-field gel electrophoresis and hylB gene analysis. J. Clin. Microbiol. 37:1892-1898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rolland, K., L. Mereghetti, S. Watt, S. Chatellier, and R. Quentin. 2002. tRNA gene clusters at the 3′ end of rRNA operons are specific to virulent subgroups of Streptococcus agalactiae strains, as demonstrated by molecular differential analysis at the population level. Microbiology 148:1493-1499. [DOI] [PubMed] [Google Scholar]
- 32.Santagati, M., F. Iannelli, C. Cascone, F. Campanile, M. R. Oggioni, S. Stefani, and G. Pozzi. 2003. The novel conjugative transposon tn1207.3 carries the macrolide efflux gene mef(A) in Streptococcus pyogenes. Microb. Drug Resist. 9:243-247. [DOI] [PubMed] [Google Scholar]
- 33.Schuchat, A. 1998. Epidemiology of group B streptococcal disease in the United States: shifting paradigms. Clin. Microbiol. Rev. 11:497-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Selander, R. K., J. M. Musser, D. A. Caugant, M. N. Gilmour, and T. S. Whittam. 1987. Population genetics of pathogenic bacteria. Microb. Pathog. 3:1-7. [DOI] [PubMed] [Google Scholar]
- 35.Shapiro, J. A. 1992. Natural genetic engineering in evolution. Genetica 86:99-111. [DOI] [PubMed] [Google Scholar]
- 36.Smoot, J. C., K. D. Barbian, J. J. Van Gompel, L. M. Smoot, M. S. Chaussee, G. L. Sylva, D. E. Sturdevant, S. M. Ricklefs, S. F. Porcella, L. D. Parkins, S. B. Beres, D. S. Campbell, T. M. Smith, Q. Zhang, V. Kapur, J. A. Daly, L. G. Veasy, and J. M. Musser. 2002. Genome sequence and comparative microarray analysis of serotype M18 group A Streptococcus strains associated with acute rheumatic fever outbreaks. Proc. Natl. Acad. Sci. USA 99:4668-4673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sumby, P., S. F. Porcella, A. G. Madrigal, K. D. Barbian, K. Virtaneva, S. M. Ricklefs, D. E. Sturdevant, M. R. Graham, J. Vuopio-Varkila, N. P. Hoe, and J. M. Musser. 2005. Evolutionary origin and emergence of a highly successful clone of serotype M1 group a Streptococcus involved multiple horizontal gene transfer events. J. Infect. Dis. 192:771-782. [DOI] [PubMed] [Google Scholar]
- 38.Takahashi, S., E. E. Adderson, Y. Nagano, N. Nagano, M. R. Briesacher, and J. F. Bohnsack. 1998. Identification of a highly encapsulated, genetically related group of invasive type III group B streptococci. J. Infect. Dis. 177:1116-1119. [DOI] [PubMed] [Google Scholar]
- 39.Takahashi, S., S. Detrick, A. A. Whiting, A. J. Blaschke-Bonkowksy, Y. Aoyagi, E. E. Adderson, and J. F. Bohnsack. 2002. Correlation of phylogenetic lineages of group B streptococci, identified by analysis of restriction-digestion patterns of genomic DNA, with infB alleles and mobile genetic elements. J. Infect. Dis. 186:1034-1038. [DOI] [PubMed] [Google Scholar]
- 40.Tettelin, H., V. Masignani, M. J. Cieslewicz, C. Donati, D. Medini, N. L. Ward, S. V. Angiuoli, J. Crabtree, A. L. Jones, A. S. Durkin, R. T. Deboy, T. M. Davidsen, M. Mora, M. Scarselli, I. Margarit, J. D. Peterson, C. R. Hauser, J. P. Sundaram, W. C. Nelson, R. Madupu, L. M. Brinkac, R. J. Dodson, M. J. Rosovitz, S. A. Sullivan, S. C. Daugherty, D. H. Haft, J. Selengut, M. L. Gwinn, L. Zhou, N. Zafar, H. Khouri, D. Radune, G. Dimitrov, K. Watkins, K. J. O'Connor, S. Smith, T. R. Utterback, O. White, C. E. Rubens, G. Grandi, L. C. Madoff, D. L. Kasper, J. L. Telford, M. R. Wessels, R. Rappuoli, and C. M. Fraser. 2005. Genome analysis of multiple pathogenic isolates of Streptococcus agalactiae: implications for the microbial “pan-genome.” Proc. Natl. Acad. Sci. USA 102:13950-13955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tettelin, H., V. Masignani, M. J. Cieslewicz, J. A. Eisen, S. Peterson, M. R. Wessels, I. T. Paulsen, K. E. Nelson, I. Margarit, T. D. Read, L. C. Madoff, A. M. Wolf, M. J. Beanan, L. M. Brinkac, S. C. Daugherty, R. T. DeBoy, A. S. Durkin, J. F. Kolonay, R. Madupu, M. R. Lewis, D. Radune, N. B. Fedorova, D. Scanlan, H. Khouri, S. Mulligan, H. A. Carty, R. T. Cline, S. E. Van Aken, J. Gill, M. Scarselli, M. Mora, E. T. Iacobini, C. Brettoni, G. Galli, M. Mariani, F. Vegni, D. Maione, D. Rinaudo, R. Rappuoli, J. L. Telford, D. L. Kasper, G. Grandi, and C. M. Fraser. 2002. Complete genome sequence and comparative genomic analysis of an emerging human pathogen, serotype V Streptococcus agalactiae. Proc. Natl. Acad. Sci. USA 99:12391-12396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.van Leeuwen, W., H. Verbrugh, J. van der Velden, N. van Leeuwen, M. Heck, and A. van Belkum. 1999. Validation of binary typing for Staphylococcus aureus strains. J. Clin. Microbiol. 37:664-674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wastfelt, M., M. Stalhammar-Carlemalm, A. M. Delisse, T. Cabezon, and G. Lindahl. 1996. Identification of a family of streptococcal surface proteins with extremely repetitive structure. J. Biol. Chem. 271:18892-18897. [DOI] [PubMed] [Google Scholar]
- 44.Zhong, S., A. Khodursky, D. E. Dykhuizen, and A. M. Dean. 2004. Evolutionary genomics of ecological specialization. Proc. Natl. Acad. Sci. USA 101:11719-11724. [DOI] [PMC free article] [PubMed] [Google Scholar]