Abstract
Background
Little is known about the determinants of parental response when children appear to have a respiratory tract infection (RTI). Our objective was to identify what factors predict that parents will seek medical consultation.
Methods
In a prospective cohort study we consecutively recruited 400 children aged 2 months to 12 years from the urban, largely middle-class, primary-care practices of 7 pediatricians in Toronto. Baseline demographic data were collected and the children followed by telephone inquiry until an RTI developed or 6 months elapsed. Data about any medical consultation for the RTI were collected. The parents completed a questionnaire on clinical features and parental interpretations and concerns. Potential predictors of consultation were organized into 4 domains: family factors, principal complaints, functional burden of illness (determined with a validated measure, the Canadian Acute Respiratory Illness and Flu Scale [CARIFS]) and parental interpretation of the illness. Key variables for each domain were derived by endorsement, correlation and combination, and univariate association with the outcome (medical consultation). A model was created to identify independent predictors of consultation.
Results
Of the 383 children (96%) for whom the study was completed, 275 (72%) had symptoms of an RTI within 6 months after recruitment. Medical consultation was sought for 140 (56%) of the 251 for whom further data were available. The questionnaire data and follow up were complete for 197 (78%) of the 251. Children with earaches compared to children without were more likely to be taken to a physician (odds ratio [OR] 10.2; 95% confidence interval [CI] 2.8–37.4), as were children with high fever (temperature > 40°C) compared to children with no fever or fever ≤ 40°C (OR 3.2; 95% CI 1.2–8.6). Parents who rated their children as having a complaint that was severe or persisting for more than 24 hours were more likely to see a physician than parents who rated their children as having no complaints (OR 8.5; 95% CI 2.3–32.0). Parental concern that the illness had an unusual course, with prolonged duration or deterioration (OR 5.7; 95% CI 1.3–24.8), that the child had a specific illness (OR 2.9; 95% CI 1.1–7.7) or that specific treatment was needed (OR 5.0; 95% CI 1.1–23.1), compared to children with no illnesses or need for treatment, also predicted consultation with a physician. Parents' postsecondary education (OR 4.0; 95% CI 1.1–14.6), compared to parents with less than postsecondary education, was the only parental factor that independently predicted taking a child to see a physician. Child's age 48 months or less was the only child factor that independently predicted physician consultation (0–6 months, OR 9.2, 95% CI 1.4–58.1; 7–12 months, OR 17.3, 95% CI 2.0–147.2; 13–24 months, OR 9.2, 95% CI 1.3–63.6; 25–48 months, OR 5.2, 95% CI 0.8–34.4). Neither family demographics nor functional burden of illness predicted consultation.
Interpretation
Generally, parents choose reasonable criteria for seeking physician advice. However, their perceptions and interpretations may be based in part on limited understanding of some factors. Further research is necessary to determine how these findings can be used to improve anticipatory guidance to parents and better address parental concerns.
Most respiratory tract infections (RTIs) in children are minor and self-limiting.1 However, their financial impact and burden on health care resources are immense. In the United States the annual cost of ambulatory treatment of RTIs totals billions of dollars.2 RTIs are common worldwide. A European multicentre study found that French and Italian children averaged 4.26 episodes of upper RTIs per year.3 Wang and colleagues4 reported 140 892 physician visits for RTIs in a single year in a cohort of 61 165 Canadian children less than 5 years of age.
Symptoms associated with innocuous upper RTI may herald much more serious disease, such as pneumonia, sepsis or meningitis. Parents, understandably, are concerned about excluding these potentially life-threatening diagnoses. Furthermore, they may seek medical advice to ensure that all reasonable measures to comfort their sick children have been taken.
Why do parents respond the way they do? We hypothesized that for families with an established medical “home” (a medical practice that they regularly attend and that is available for consultation about acute sickness) a broad variety of factors influence parental decision-making. These factors would include the presence of specific symptoms (e.g., sore throat, earache and wheezing), the overall functional severity of the illness, parental interpretation of the disease process and certain family demographic factors (e.g., patient age, number of children and single-parent home). Proving this hypothesis might permit physicians to better anticipate the information needs of parents and might help identify factors whose modification could reduce the likelihood of unnecessary visits. The purpose of this study was to identify factors that predict that parents will seek medical consultation for symptoms of an RTI in their children.
Methods
Study design
This was a prospective cohort study conducted between April 1998 and March 1999. The Research Ethics Board of The Hospital for Sick Children, Toronto, Ont., approved the investigation.
We recruited 400 children consecutively from the urban, largely middle-class, primary-care practices of 7 pediatricians in Toronto at the time of a routine, scheduled health-maintenance visit. Inclusion criteria were age between 2 months and 12 years, absence of serious underlying disease and regarding the participating pediatric practice as the medical home. Exclusion criteria included lack of telephone at the patient's residence, inability of the child's primary caregiver to communicate effectively in English, residence outside the Greater Toronto area and participation of a sibling in the study.
At the time of recruitment, having first obtained informed parental consent, a research nurse collected baseline demographic data: parental age, education, occupation, workload, perceived stress and affective state, as well as composition of the family unit, type of residence and available support systems. Specific child variables recorded included birth order, general level of health, presence of chronic disease, recent hospitalizations or emergency department visits and perceived temperament.
All participating families received a scheduled telephone call from the research nurse every 2 weeks until symptoms of an RTI occurred or 6 months had elapsed. When symptoms suggestive of an RTI were reported, the nurse determined whether medical consultation had been sought. From the subgroup that had sought medical consultation she collected data on how the advice was obtained: by telephone alone, by visiting the primary-care pediatrician or by visiting an emergency department or a walk-in clinic, for example.
On the 7th day after symptoms had appeared the parents were given a questionnaire and asked to report their child's principal complaint (the major symptom) and assess the apparent functional severity of the illness with a validated measure, the Canadian Acute Respiratory Illness and Flu Scale (CARIFS).5 Data on parental interpretations and concerns about specific symptoms, appearance or a particular illness (e.g., meningitis or pneumonia) were also gathered. The questionnaire included an unstructured section that asked the parents to describe their greatest concerns.
The research nurse assisted in questionnaire completion by providing clarification to the parents. To avoid underreporting of symptoms, she used the elicitation approach,6 asking about the presence of a symptom with a simple Yes/No question oriented to the parent's perception of the problem and not by clinician-defined criteria. The number of complaints identified by the parents was not restricted. The parents were then asked to quantify severity with qualifying terms that define a patient-centred threshold distinguishing clinically bothersome symptoms:6 they were asked whether they considered the complaint severe (causing distress and reduced function), persistent (continuously present for more than 24 hours) and/or associated with specific features (e.g., sore throat with difficulty eating or drinking and/or tender neck glands). The items for these questions were generated from clinical experience and literature review according to accepted techniques.7
Two important variables required the coding of responses to open-ended questions. Parental concern about an “abnormal course of illness” consisted of responses of concern that the illness was unusually severe or long-lasting or that the child's condition was deteriorating. Parental concern about an “illness needing specific treatment” consisted of responses in which the parent interpreted that the illness involved otitis media, streptococcal pharyngitis, pneumonia or sepsis. One variable was derived from the combination of a number of variables: if the parent indicated a severe problem with any principal complaint involving sore throat, respiratory symptoms or the child's level of interaction (e.g., sore throat with difficulty swallowing, painful swollen neck glands, stridor at rest or persistent noisy breathing, lack of interest in play, lack of walking or inconsolable state) the sign or symptom was graded as severe or persistent.
Data analysis
From the variables assessed, 4 predictor domains were identified: family factors, principal complaints, functional burden of illness and parental interpretation. We described the relationship between the 4 domains and seeking medical consultation with relative risks and used Fisher's exact test to determine the significance of this univariate association.
We then created a multiple logistic regression model with “seeking medical consultation” (Yes/No) as the outcome and variables from the 4 domains as predictors. To exclude variables that contributed little or redundant information, we used a specific strategy.8 First, we excluded questions for which the response was uniform (all parents responded “No” or “Not applicable”), there was a poor response rate or the variable on its own didn't have even minimal signs of association with seeking medical consultation. Next, we examined questions whose responses highly correlated with other responses (correlation coefficient > 0.5) and chose a representative or combined question. Of the 17 candidate variables thus selected for model building, 2 — child's age and presence of a high fever — were forcibly retained in the model because of their known importance in interpreting illness. The remainder were selected through backwards elimination of candidate variables that failed to contribute to the model (α = 0.10). We examined the correlation matrix, interaction terms and variable coefficients with their standard errors to ensure that the final model was free from significant collinearity, zero-cell problems and interaction. The Hosmer–Lemeshow test was used to assess model fit.8 The statistical procedure used for this analysis in SAS was PROC LOGISTIC (SAS Institute, Cary, NC).
Results
Outcomes
The study was completed for 383 (96%) of the 400 children recruited. Symptoms of an RTI developed within 6 months after recruitment in 275 (72%) of the 383 children. These 275 children were significantly younger than the children in whom RTI symptoms did not develop (mean ages 2.77 and 4.46 years) according to the t-test (p < 0.0001).
Further data were available for 251 (91%) of the symptomatic children. Medical consultation (Fig. 1) was sought for 140 (56%) of the 251. Although 35% of the 251 children were reported by the parents to have a “high fever”, only 17% had a temperature of more than 40°C. Earache was reported as a principal complaint for 17% of the 251 children and rhinorrhea for 91%.
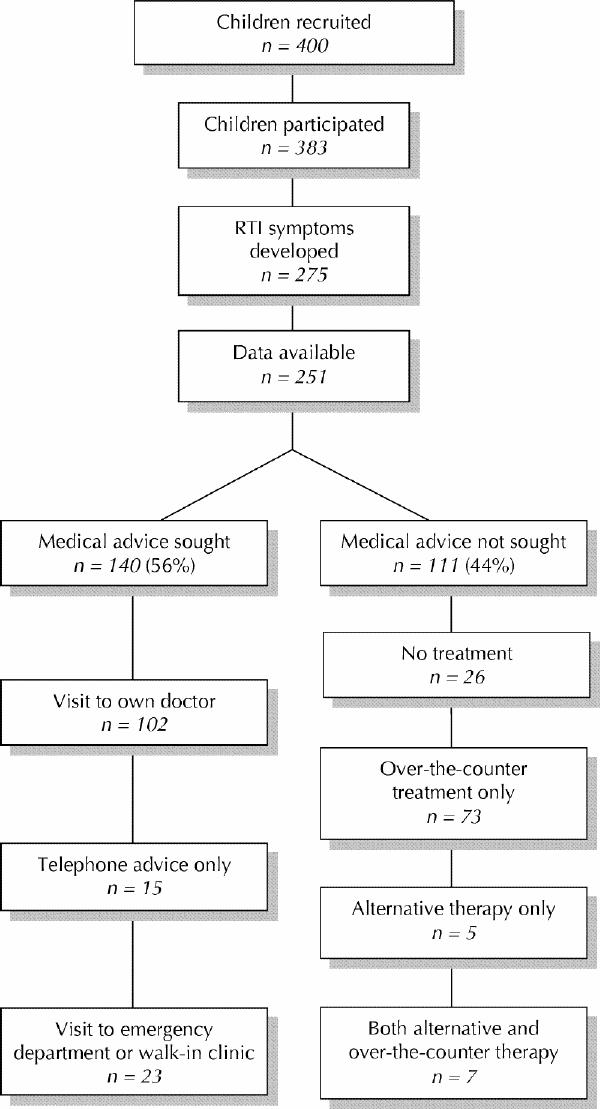
Fig. 1: Outcomes in study of children for symptoms of respiratory tract infection (RTI). “Alternative therapy” includes use of herbal remedies and vitamin C.
Unadjusted predictors
The questionnaire data and follow up were complete for 197 (78%) of the 251 symptomatic children with further data. Univariate analysis of the relationship between the 4 predictor domains and seeking medical consultation (Fig. 2) suggested that factors from all 4 domains (family factors, principal complaints, functional burden of illness and parental interpretation) might predict seeking medical consultation when considered without adjustment for other factors.

Fig. 2: Unadjusted predictors of seeking medical consultation for an RTI.
Independent predictors
The final results of the multiple logistic regression analyses are shown in Fig. 3. The model was stable and had good explanatory ability. Examination of the correlation matrix, interaction terms and coefficient standard errors did not reveal problems with significant collinearity or interaction. Reconsideration of excluded variables and other model-building techniques did not suggest that any alternative models should be considered.
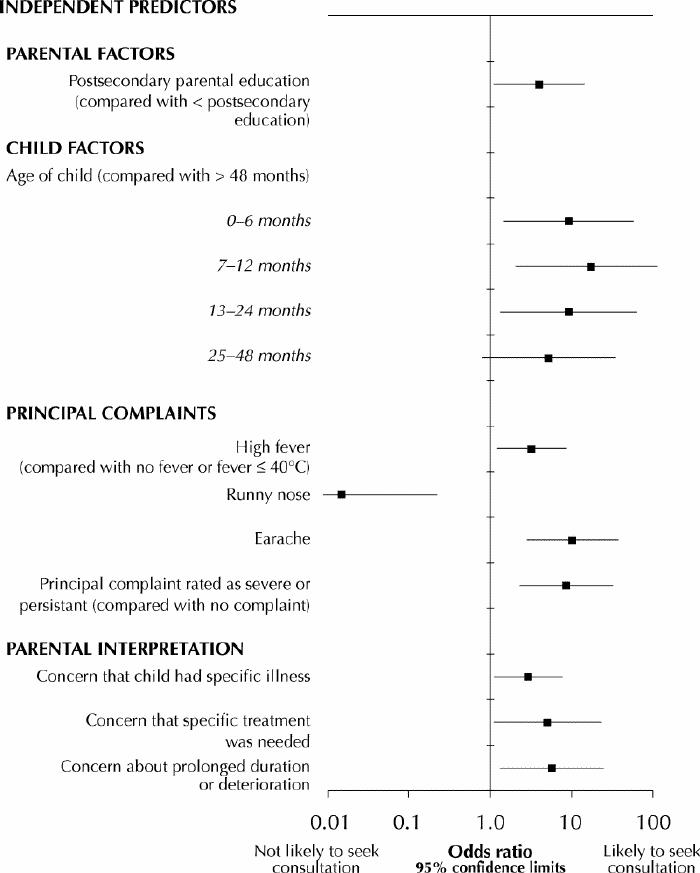
Fig. 3: Independent predictors of seeking medical consultation for an RTI. Adjusted for other factors with multiple logistic regression with R2 = 0.4715 and goodness of fit as demonstrated by no significant departure of model predictions from observed data (Hosmer–Lemeshow test p = 0.20).
The most important independent factors predicting seeking medical consultation came from 2 domains: principal complaints and parental interpretation. Seeking medical consultation was associated with a complaint of earache (odds ratio [OR] 10.2; 95% confidence interval [CI] 2.8–37.4) or high fever (temperature > 40°C) (OR 3.2; 95% CI 1.2–8.6) or a complaint rated as severe or persisting for more than 24 hours (OR 8.5; 95% CI 2.3–32.0). Parental concern that the illness had an unusual course, with prolonged duration or deterioration (OR 5.7; 95% CI 1.3–24.8), that the child had a specific illness (OR 2.9; 95% CI 1.1–7.7) or that a specific treatment was needed (OR 5.0; 95% CI 1.1–23.1) also predicted medical consultation. Postsecondary education (OR 4.0; 95% CI 1.1–14.6) was the only parental factor that independently predicted medical consultation. Child's age 48 months or less was the only child factor that independently predicted medical consultation (0–6 months, OR 9.2, 95% CI 1.4–58.1; 7–12 months, OR 17.3, 95% CI 2.0–147.2; 13–24 months, OR 9.2, 95% CI 1.3–63.6; 25–48 months, OR 5.2, 95% CI 0.8–34.4).
Interpretation
When their children appear to have an RTI, parents in a population of families with a medical home seek medical consultation for specific reasons related to the principal complaint, their perception of the severity of the symptoms and signs, and their interpretation of these observations. They are more likely to take infants and toddlers than older children to the doctor, independent of the presenting complaint.
In the United States, children under 1 year of age are more than twice as likely as those 5-14 years of age to be taken to a physician for consultation about respiratory conditions.1 When the presenting problem is simply a cough, cold or runny nose, infants under 1 year of age averaged 6.78 times as many physician visits as did children 5–14 years.1 In our study, we were somewhat surprised that low patient age alone (i.e., in the univariate analysis) was not a very strong predictor of medical consultation. However, when adjusted for complaint severity and overall burden of illness, age became a very significant predictor; that is, parents tended to seek advice for much milder signs and symptoms in children less than 1 year of age.
In terms of background and personal situation the parents in our study responded similarly when their children took ill. Somewhat surprisingly, parental age, health, perceived affect, sense of support, employment situation and current marital status did not affect response, nor did the child's birth order, general level of health and underlying temperament. Postsecondary parental education, however, moderately increased the likelihood of medical consultation.
The perceived functional burden of illness did not predict medical consultation. This is probably because most children with RTIs, particularly colds, don't appear to raise specific concerns, even when the RTI is severe enough to affect the child's functioning. Furthermore, general appearance seldom identifies children suffering from serious disease. For example, Teach and associates9 reported that the median Yale Observation Score for children aged 3 to 36 months of age with bacteremia was the same as the median for those without bacteremia. Infants with occult bacteremia are just as likely as children without bacteremia to display a social smile.10
Certain specific presenting complaints predicted medical consultation. High fever (temperature > 40°C) was an independent predictor. Many parents fear and misunderstand fever. In 1985 Kramer, Naimark and Leduc11 reported that nearly 50% of parents considered temperatures less than 38.0°C to constitute a fever, and 43% felt that temperatures less than 40°C could be dangerous. In 1999 Van Stuijvenberg and coworkers12 reported that 45% of parents in their survey were afraid of fever.
Although high fever and earache were the only principal complaints that were independent predictors of medical consultation, sore throat, cough, irritability and respiratory difficulties such as stridor, wheeze and tachypnea predicted medical consultation if they were perceived as being severe or persistent. These observations were consistent in both the structured and the open-ended questions, and they make clinical sense.
How parents synthesized their observations into an interpretation of the disease process was also important in determining their response. Parents sought medical consultation if they had a major concern that the course of the disease was unusually long or severe or that the child's condition was deteriorating, or if they thought the clinical presentation suggested a diagnosis that would typically necessitate medical treatment such as antibiotic therapy. Parents were also more likely to seek medical consultation if they had a specific bacterial infection in mind. Unfortunately, parents may harbour inappropriate perceptions about the need for treatment and the effectiveness of antibiotics in treating simple viral infections.13,14
There were a number of significant limitations to this study. Prevalidated measures were limited or nonexistent. To thoroughly obtain insight on parental perceptions, we developed questionnaires that contained a large number of variables. Furthermore, the sample population was not entirely representative. The families were generally better educated, more affluent and more intact than those in the general population; however, one of our major findings was the limited importance of family demographics compared with observations and perceptions in parental decision-making. The fact that all the children in this study had a medical home may explain why a relatively small percentage were assessed at an emergency department or a walk-in clinic.15
What implications do these results have for the formulation of strategies that ensure the appropriateness of medical visits? Some predictors of medical consultation, such as patient age, are not amenable to modification. On the other hand, educating parents to distinguish between important sentinel symptoms and unimportant signs and symptoms might diminish the frequency of inappropriate consultation. Casey and colleagues16 have demonstrated that educating parents about fever management reduces the frequency of both physician contact and medication error. The possibility of further reductions through parental education about the natural history of RTIs, transient ear pain and other factors needs exploration. However, there remains an inherent inefficiency in parents' distinguishing serious RTIs from trivial ones that health care providers must continue to acknowledge.
Overall, parents appear to be influenced mainly by a reasonable set of factors in deciding when to seek physician advice. However, their perceptions and interpretations may be based in part on limited understanding of some factors, such as fever and illnesses requiring treatment. Further work is necessary to determine how these findings can be used to improve anticipatory guidance and better address parental concern about specific symptoms. It will also be important to examine these factors in other populations, including those without an established medical home.
β See related article page 43
Acknowledgments
We thank Mary Antonopoulos for her dedicated administrative support.
Footnotes
This article has been peer reviewed.
Contributors: Norman Saunders was the principal investigator; with Paul Dick he designed the study and prepared the manuscript, as well as helping to acquire funding and to collect and analyze the data. He, Olwen Tennis, Sheila Jacobson and Marvin Gans recruited the patients. Olwen Tennis was responsible for data collection and contributed to data analysis. Sheila Jacobson and Marvin Gans contributed to study design and data collection. Paul Dick was responsible for funding acquisition and data analysis. All the authors contributed to the manuscript's writing.
This study was made possible by a generous grant from the Sir Jules Thorn Charitable Trust, London, England. The Paediatric Outcomes Research Team is funded by The Hospital for Sick Children Foundation, Toronto. Paul Dick receives financial support from the Ontario Ministry of Health and Long Term Care through a Career Scientist Award (#05239). The results and conclusions are those of the authors; no official endorsement by the ministry is intended or should be inferred.
Competing interests: None declared.
Correspondence to: Dr. Norman R. Saunders, Division of Pediatric Medicine, The Hospital for Sick Children, 555 University Ave., Toronto ON M5G 1X8; fax 416 489-1510; norman.saunders@utoronto.ca
References
- 1.Freid VM, Makuc DM, Rooks RN. Ambulatory health care visits by children: principal diagnosis and place of visit. National Center for Health Statistics. Vital Health Stat 13 1998;137:1-23. [PubMed]
- 2.Dixon RE. Economic costs of respiratory tract infections in the United States. Am J Med 1985;78:45-51. [DOI] [PubMed]
- 3.Rhinitis Survey Group. Van Cauwenberge P, Berdeaux G, Morineau A, Smadja C, Allaire JM. Use of diagnostic clusters to assess the economic consequences of rhinopharyngitis in children in Italy and France during the winter. Clin Ther 1999;21:404-21. [DOI] [PubMed]
- 4.Wang EEL, Einarson TR, Kellner JD, Conly JM. Antibiotic prescribing for Canadian preschool children: evidence of overprescribing for viral respiratory infections. Clin Infect Dis 1999;29:155-60. [DOI] [PubMed]
- 5.Jacobs B, Young NL, Dick PT, Ipp MM, Dutkowski R, Davies HD, et al. Canadian Acute Respiratory Illness and Flu Scale (CARIFS). Development of a valid measure for childhood respiratory infections. J Clin Epidemiol 2000; 53: 793-9. [DOI] [PubMed]
- 6.Kroenke K. Studying symptoms: sampling and measurement issues. Ann Intern Med 2001;134:844. [DOI] [PubMed]
- 7.Feinstein AR. Clinimetrics. New Haven, Conn: Yale University Press; 1987. p. 51-2.
- 8.Hosmer DW, Lemeshow SL. Applied logistic regression. 2nd ed. New York: John Wiley & Sons; 2000. p. 92-141.
- 9.Teach SJ, Fleisher GR, Occult Bacteremia Study Group. Efficacy of an observation scale in detecting bacteremia in febrile children three to thirty-six months of age, treated as outpatients. J Pediatr 1995;126:877-81. [DOI] [PubMed]
- 10.Bass JW, Wittler RR, Weisse ME. Social smile and occult bacteremia. Pediatr Infect Dis J 1996;15:541. [DOI] [PubMed]
- 11.Kramer MS, Naimark L, Leduc DG. Parental fever phobia and its correlates. Pediatrics 1985;75:1110-3. [PubMed]
- 12.Van Stuijvenberg M, deVos S, Tijang GC, Steyerberg EW, Derksen Lubsen G, Moll HA. Parents' fear regarding fever and febrile seizures. Acta Paediatr 1999;88:618-22. [DOI] [PubMed]
- 13.Collett CA, Pappas DE, Evans BA, Hayden GF. Parental knowledge about common respiratory infections and antibiotic therapy in children. South Med J 1999;92:971-6. [DOI] [PubMed]
- 14.McKee MD, Mills L, Mainous AG III. Antibiotic use for the treatment of upper respiratory tract infections in a diverse community. J Fam Pract 1999;48:993-6. [PubMed]
- 15.St Peter RF, Newacheck PW, Halfon N. Access to care for poor children. Separate and unequal? JAMA 1992;267:2760-4. [PubMed]
- 16.Casey R, McMahon F, McCormick MC, Pasquariello PS Jr, Zavod W, King FH Jr. Fever therapy: an educational intervention for parents. Pediatrics 1984;73:600-5. [PubMed]


