Abstract
FOLLOWING THE LAUNCH OF A PUBLICLY FUNDED influenza immunization program for all residents of Ontario over the age of 6 months, we evaluated 203 parents of children who presented to our emergency department between January and March of the following year (2001). Overall, 54 (27%) of the children had been vaccinated. Parents of non-immunized children were more likely to believe that immunization resulted in a flu-like illness (42% v. 17%; p = 0.001), caused side effects that were more severe than having influenza (36% v. 17%; p = 0.010) and weakened the immune system (52% v. 24%; p < 0.001). Parents of both immunized and non-immunized children incorrectly identified gastrointestinal symptoms as symptoms of influenza. The primary reason for deciding against immunization was the belief that their child was not at risk. After adjustment, children with a chronic disease were more likely than those without a chronic disease to be immunized (adjusted odds ratio [OR] 4.7, 95% confidence interval [CI] 1.8–12.6). Children of parents who discussed immunization with a physician were more likely to be immunized than those who had not discussed immunization with a physician (OR 6.8, 95% CI 2.4–19.2).
More than 20%–30% of children are infected annually with influenza.1,2 The Canadian National Advisory Committee on Immunization currently recommends annual immunization of all people 6 months of age or older who are at increased risk of influenza- related complications.3 Vaccination of healthy children is effective and decreases the spread of the disease in schools and the community.1,2,4,5,6,7,8,9
During the 2000/01 influenza season, the Ontario Ministry of Health and Long-Term Care sponsored a universal program of publicly funded influenza immunization for all people in Ontario over the age of 6 months. We felt this was an opportunity to explore factors that influence parents in the decision to immunize their children against influenza.
Between January and March 2001, a convenience sample of parents of Ontario children presenting to the emergency department (ED) of the Children's Hospital of Eastern Ontario were surveyed. After written consent was obtained, a piloted standardized survey was administered by study personnel. Open and closed questions in French or English identified demographic characteristics, parental knowledge of influenza illness and immunization, and factors influencing decisions on immunization. The parents of a parallel subset of all children 6 months of age and older presenting to the ED were surveyed for immunization status alone. Univariate comparisons were conducted using χ2 analysis, Fisher's exact test and risk ratio with a level of significance of α = 0.05. A logistic regression model was constructed that included all 7 factors that were thought might influence the influenza immunization decision. No variable-selection techniques were employed.
A total of 203 (97%) of 208 parents agreed to participate in the study. Overall, 54 (27%) of 203 children had received the influenza immunization in the 2000/01 influenza season. In the parallel subset of 8679 children, 1813 (21%) were also immunized (p = 0.06).
There were no differences between immunized children and nonimmunized children in terms of age (p = 0.16), sex (p = 0.75), daycare attendance (p = 1.00), parental education level (mother p = 0.49; father p = 1.00) or final ED diagnosis (p = 0.66). Children who had received an influenza immunization in the past (relative risk [RR] 2.7, 95% confidence interval [CI] 1.8–4.2) and children with immunized family members (RR 7.5, 95% CI 3.7–15.1) were more likely to be immunized. Knowledge of influenza illness was similar among parents of immunized and nonimmunized children. Of the parents, 119 (58%) incorrectly identified vomiting and diarrhea as symptoms of influenza illness. Parents of nonimmunized children were more likely than those of immunized children to believe that influenza-like illness was a side effect of the immunization (42% v. 17%; p = 0.001), that side effects of the influenza immunization are worse than the illness itself (36% v. 17%; p = 0.010) and that influenza immunization could weaken the immune system (52% v. 24%; p < 0.001).
The 2 most common reasons for immunization were the belief that immunization prevents influenza (54% [29/54]) and that a physician had recommended it (39% [21/54]). The most common reason against immunization was the belief that their child was not at risk (38% [56/149]).
Of all parents, 57% (166/202) had discussed influenza immunization with a physician, and of these only 57% (64/112) received a recommendation for immunization. When immunization was not recommended, 96% (46/48) of children did not receive immunization. Of the parents who had not discussed immunization with a physician, 87% (75/86) of these children did not receive immunization.
Results of the logistic regression analysis of factors potentially associated with the decision to immunize are presented in Fig. 1. Having a chronic disease (OR = 4.7, 95% CI 1.8–12.6) and discussing immunization with a physician (OR = 6.8, 95% CI 2.4–19.2) both significantly influenced parental decisions to have their child immunized.
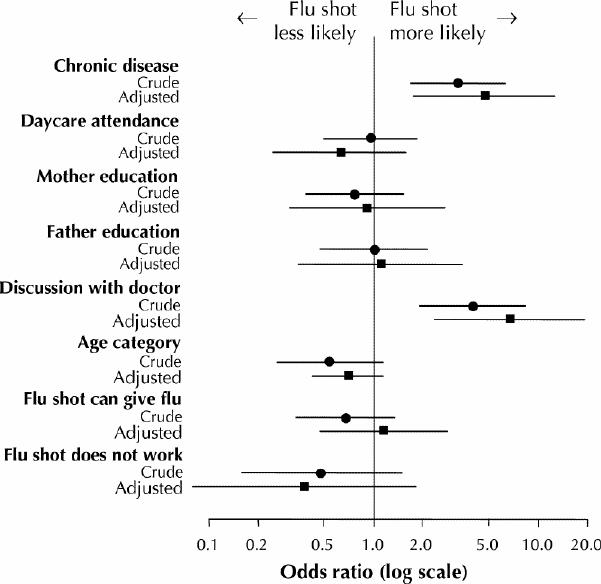
Fig. 1: Crude and adjusted odds ratios for factors potentially influencing parents' decisions regarding influenza immunization of their.
The main limitation of this study is that the survey was administered to parents of children visiting the ED of a tertiary care pediatric hospital and may not represent parents of children in the general population who do not seek care at similar institutions. It is, however, the only dedicated ED for children in the region, and more than 50% of visits are for non-urgent care.
In our survey, about 25% of eligible children were vaccinated. This is comparable to provincial data for the 2000/01 influenza season, which showed an estimated immunization coverage of 20.4% for the 0- to 4-year age group and 30.2% for the 5- to 18-year age group (Ontario Ministry of Health and Long-Term Care: personal communication, June 2002). Our rates are also in keeping with data from other populations10,11,12,13,14 and other optional vaccines.15,16
Our results suggest that parents have gaps in knowledge concerning influenza illness and immunization. Many parents believed that influenza manifests as gastrointestinal symptoms. This belief may cause parents to think that diarrhea or vomiting temporally associated with a vaccination is a sign of vaccine failure. As well, 40% of the parents of nonimmunized children felt that their children were not at risk of disease. In fact, children are often the “epicentre” of influenza outbreaks and can become very ill. These 2 issues should be emphasized in education campaigns.
In our study, logistic regression analysis revealed that children whose parents discussed influenza immunization with a physician were 7 times more likely than those whose parents did not discuss immunization to be vaccinated. This underscores the pivotal role of the physician in the promotion of immunization.10,11,15 Why immunization was not recommended in 43% of cases is not known; the only contraindications to vaccination for children 6 months of age or older are previous anaphylaxis to the vaccine and allergy to eggs or other vaccine components.17
Although the costs and benefits of universal influenza immunization remain widely debated, public health and primary care physicians may find our findings useful in planning future influenza immunization campaigns.18,19,20
Acknowledgments
We thank Dr. Estee Marczinski and our emergency department volunteers for help with data collection; David Moher and Nick Barrowman from the Thomas C. Chalmers Centre for Systematic Reviews for their guidance and helpful suggestions; Ann Walker and the Child and Youth Clinical Trials Network for assistance with the survey tool, data entry and analysis.
Footnotes
This article has been peer reviewed.
Contributors: Drs. Grant, Le Saux, Plint, Ellis and Tam and Ms. Correll conceived and designed the study. Drs. Grant, Le Saux, Plint and Ms. Correll collected and assembled the data. Drs. Grant and Le Saux and Ms. Gaboury analyzed and interpreted the data. Ms. Gaboury provided statistical expertise. Dr. Grant drafted the article. All authors provided critical revision for important intellectual content and approved the final version of the manuscript.
This research was supported by a grant from the Children's Hospital of Eastern Ontario Research Institute.
Competing interests: None declared.
Correspondence to: Dr. Vincent J. Grant, Division of Emergency Medicine, Department of Pediatrics, Children's Hospital of Eastern Ontario, 401 Smyth Rd., Ottawa ON K1H 8L1; fax 613 738-4852; grant_v@cheo.on.ca
References
- 1.Neuzil KM, Zhu Y, Griffin MR, Edwards KM, Thompson JM, Tollefson SJ, Wright PF. Burden of interpandemic influenza in children younger than 5 years: a 25 year prospective study. J Infect Dis 2002;185:147-52. [DOI] [PubMed]
- 2.Glezen WP, Taber LH, Frank AL, Gruber WC, Piedra PA. Influenza virus infections in infants. Pediatr Infect Dis J 1997;16:1065-8. [DOI] [PubMed]
- 3.National Advisory Committee on Immunization. Statement on influenza vaccination for the 2001-2002 season. Can Commun Dis Rep 2001;27(ACS-4):1-24. [PubMed]
- 4.Gruber WC. Children as a target for immunization. In: Nicholson KG, Webster RG, Hay AJ, editors. Textbook of influenza. London: Blackwell Science; 1998. p. 435-44.
- 5.Piedra PA, Glezen WP. Influenza in children: epidemiology, immunity, and vaccines. Semin Pediatr Infect Dis 1991;2:140-6.
- 6.White T, Lavoie S, Nettleman MD. Potential cost savings attributable to influenza vaccination of school-aged children. Pediatrics 1999;103:e73. [DOI] [PubMed]
- 7.Izurieta HS, Thompson WW, Kramarz P, Shay DK, Davis RL, DeStefano F, et al. Influenza and the rates of hospitalization for respiratory disease among infants and young children. N Engl J Med 2000;342:232-9. [DOI] [PubMed]
- 8.Neuzil KM, Mellen BG, Wright PF, Mitchel EF, Griffin MR. The effect of influenza on hospitalizations, outpatients visits and course of antibiotics in children. N Engl J Med 2000;342:225-31. [DOI] [PubMed]
- 9.Hurwitz ES, Haber M, Chang A, Shope T, Teo S, Ginsberg M, et al. Effectiveness of influenza vaccination of day care children in reducing influenza- related morbidity among household contacts. JAMA 2000;284:1677-82. [DOI] [PubMed]
- 10.Findlay PF, Gibbons YM, Primrose WR, Ellis G, Downie G. Influenza and pneumococcal vaccination: patient perceptions. Postgrad Med J 2000;76:215-7. [DOI] [PMC free article] [PubMed]
- 11.Nichol KL, Hauge M. Influenza vaccination of healthcare workers. Infect Control Hosp Epidemiol 1997;18:189-94. [DOI] [PubMed]
- 12.Krieger JW, Castorina JS, Walls ML, Weaver MR, Ciske S. Increasing influenza and pneumococcal immunization rates: a randomized controlled study of a senior center-based intervention. Am J Prev Med 2000;18:123-31. [DOI] [PubMed]
- 13.Ipp M, Macarthur C, Winders P, Gold R. Influenza vaccination of high-risk children: a survey of three physician groups. Can J Public Health 1998;89:415-8. [DOI] [PMC free article] [PubMed]
- 14.Walls C. Reasons that healthcare workers decline influenza vaccination in a New Zealand hospital environment. Infect Control Hosp Epidemiol 2000;21: 249-50. [DOI] [PubMed]
- 15.Freeman VA, Freed GL. Parental knowledge, attitudes, and demand regarding a vaccine to prevent varicella. Am J Prev Med 1999;17:153-5. [DOI] [PubMed]
- 16.Impicciatore P, Bosetti C, Schiavio S, Pandolfini C, Bonati M. Mothers as active partners in the prevention of childhood diseases: maternal factors related to immunization status of preschool children in Italy. Prev Med 2000;31:49-55. [DOI] [PubMed]
- 17.National Advisory Committee on Immunization. Influenza vaccine. In: Canadian Immunization Guide. 5th ed. Ottawa: Health Canada; 1998. Cat no H49-8 /1998E. p. 103-10.
- 18.Schabas RE. Mass influenza vaccination in Ontario: A sensible move. CMAJ 2001; 164(1):36-7. [PMC free article] [PubMed]
- 19.Demicheli V. Mass influenza vaccination in Ontario: Is it worthwhile? CMAJ 2001; 164(1):38-9. [PMC free article] [PubMed]
- 20.Iwane MK, Schwartz B. Pediatric influenza immunization: should healthy children be vaccinated? Pediatr Ann 2001;30(6):354-7. [DOI] [PubMed]


