Case
A 13-month-old infant is seen routinely in the office of a family physician for immunizations and periodic health examinations. The child's growth is entirely normal but, in taking a developmental history, the physician notes that the child is described as being generally irritable and is reluctant to explore her environment away from her caregiver's side. She was weaned from the breast at 8–9 months of age and went directly to whole cow's milk, as is recommended by the Canadian Paediatric Society. Her current diet consists primarily of jars of fruit and vegetables, with an occasional jar of a meat or poultry meal. She drinks at least 4 8-oz bottles of whole milk daily. On physical examination, the only abnormal finding is slightly pale conjunctiva. The physician suspects a diagnosis of iron deficiency anemia. Blood tests are ordered to confirm the diagnosis.
Iron deficiency anemia is a leading cause of infant morbidity and mortality worldwide.1 Numerous studies have demonstrated that even moderate anemia (hemoglobin < 100 g/L) is associated with depressed mental and motor development in children that may not be reversible.2,3,4 Because of the possible irreversibility of this condition, primary prevention is a more appropriate goal than screening and treatment. In Canada, 4%–5% of non-Aboriginal preschool children suffer from iron deficiency anemia, compared with a prevalence of between 14% and 24% in First Nations and Inuit infants and children.5,6,7 In developing countries, however, the prevalence of anemia reaches and in some countries exceeds 50% in one-year-old children.8 Because of the well-documented sequelae of anemia, there is a continuing need to develop strategies and educate caregivers about the prevention and management of iron deficiency anemia.
Factors that increase the risk of anemia
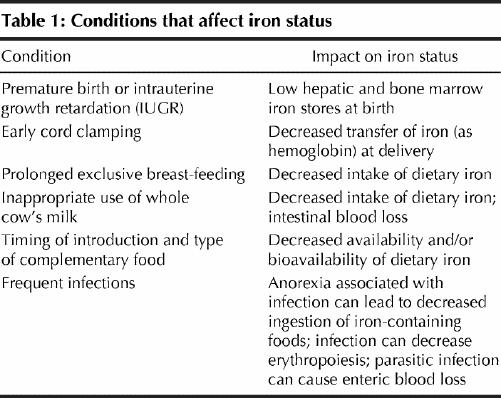
The environmental conditions that are usually found when the prevalence of iron deficiency anemia is high are outlined in Table 1, as is their impact on iron status. Depending on the age and circumstances of the individual child, each condition will affect iron status to varying degrees. The transfer of iron from mother to fetus largely occurs during the last trimester of gestation and is stored mainly in the liver and bone marrow. Thus, the amount of iron present at birth depends on the length of the gestational period and the weight of the baby. Because 5%–7% of infants in Canada (and some 13 million infants internationally) are born either prematurely or with low birth weight, these factors play a large role in increasing predisposition to anemia. Over the first months of life, human milk (which contains 0.2–0.3 mg/L of iron) does not provide enough iron to meet the demands of rapid erythropoiesis, so iron stores are mobilized to meet the iron requirements of the infant.9 Iron stores are generally depleted by 6 months of age, yet from 4 to 12 months after birth the infant's blood volume doubles. Thus, at this age, dietary sources of iron become critical to keep up with this rapid rate of red blood cell synthesis.10
Table 1
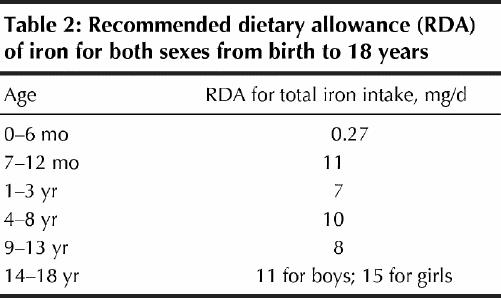
The recommended dietary allowance (RDA) for iron during childhood and adolescence is shown in Table 2.11 To prevent the development of anemia, the Canadian Paediatric Society and the American Academic of Pediatrics recommend exclusive breast-feeding for at least 4 months and the introduction of iron-containing complementary foods and foods containing ascorbic acid, which enhance iron absorption, at the age of 4–6 months.12,13 The choice of complementary foods at this stage will markedly influence iron status. Typical grain-based or rice-based complementary foods are poor sources of iron and may contain phytic acid, which is a potent inhibitor of iron absorption.14 To augment the amount of iron found in these grain-based foods, commercial infant cereals are highly fortified with electrolytically reduced iron. Iron-fortified cereals have been shown to prevent iron deficiency anemia.15,16
Table 2
The adverse effects of anemia
Even moderate anemia (hemoglobin < 100 g/L) has been consistently shown to be associated with depressed mental and motor development in children (Box 1).2,3,4 Although the mechanism whereby iron influences development is not fully understood, older research identified the role of iron in central nervous system neurotransmitter function, and more recent work has shown that brain iron is essential for normal myelinization.17,18,19 Longitudinal studies have indicated that children who were anemic in early childhood continue to have poor cognitive and motor development and depressed school achievement into middle childhood.4 For anemic children less than 2 years of age, there is no good evidence from randomized controlled trials that iron treatment helps their cognitive and motor development.2 For children above 2 years of age, short-term treatment is associated with improvement in cognition but not in school achievement.
Box 1.
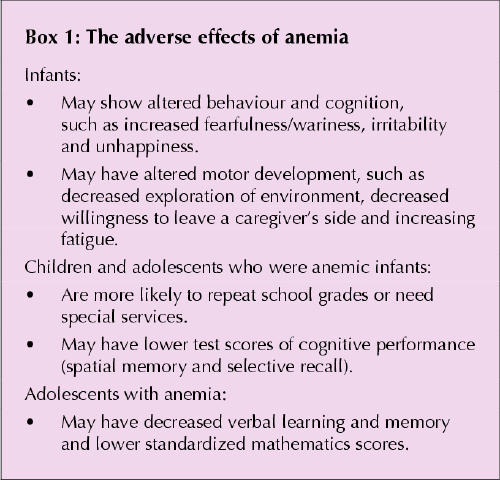
The study of cognitive function and iron status has been expanded to older children and adolescents. In a randomized controlled trial, adolescent girls with depleted iron stores who received iron supplements improved their scores on a test of memory and verbal learning compared with the placebo-treated group.20 Another large study in preadolescents and adolescents described an association between iron status and standardized mathematics scores.21 Those with iron deficiency anemia or iron deficiency without anemia were 2.3 and 2.4 times more likely to have low mathematics scores than those with no iron deficiency. The authors of this report suggested that screening for iron deficiency may be warranted for all children and adolescents.
Interventions to prevent anemia
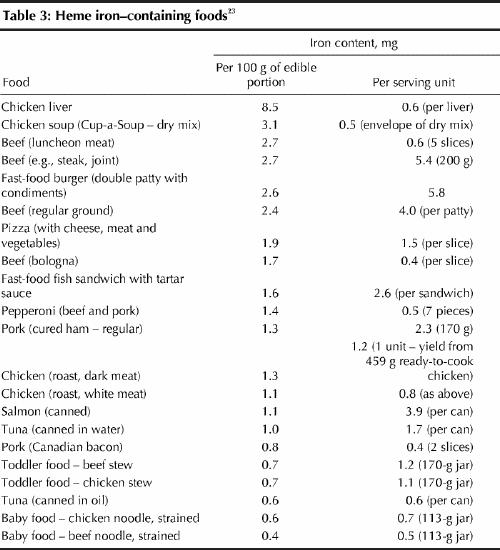
There are 3 interventions that if implemented successfully are likely to prevent anemia. These include dietary diversification to foods with more bioavailable iron; fortification of foods targeted to full-term infants and children; and supplementation of the individual. Dietary diversification involves promotion of a diet with a wider variety of naturally iron-containing foods, especially red meat, poultry and fish (Table 3). These foods have a high content of highly bioavailable heme iron and thus are most appropriate for infants and children above 6 months of age. Despite their widespread availability, even among Aboriginal children, they are not widely used (possibly because of the perceived unacceptable taste and smell of commercial products) or are diluted before use (e.g., meat is rich in iron but meat broth is not). Recent Canadian survey data indicated that 57% of female teenagers do not consume the minimum number of servings from the “meat and alternatives” food group.22 An increasing number of adolescents are following vegetarian diets and thus restrict their intake of heme iron sources.
Table 3
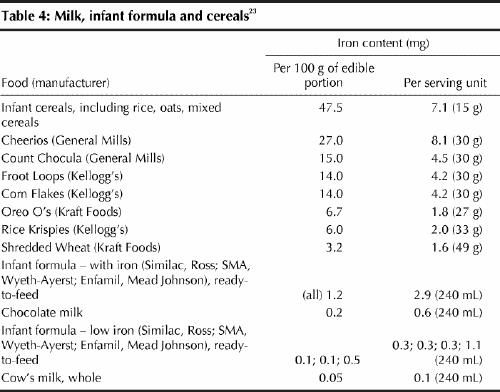
Two types of fortification strategies have been implemented successfully in Canada. These are the fortification of staple foods, such as flour, and the fortification of specific foods, such as infant formula, infant cereals and most breakfast cereals (Table 4). Fortification of staple foods is likely to increase iron intake for those who eat the most (i.e., adult males). However, infants and children who have a limited capacity to eat large quantities of food are not likely to benefit significantly from this strategy. Targeted fortification (e.g., the fortification of foods typically eaten by infants and children), however, provides an excellent source of iron to those who need it the most. Infant cereals, for example, typically contain 7.1 mg of iron per 15-g serving, and breakfast cereals for children contain over 4 mg of iron per 30-g serving.23 A single 30-g serving of these “ready-to-eat” cereals provides 60% of the RDA for children aged between 1 and 3 years, 45% of the RDA for children aged 4–8 years and 75% for boys and girls aged 9–13 years. For adolescents, especially those who are restricting their total food intake or who are vegetarians, the use of iron-fortified breakfast cereals that typically contain 4–8 mg/serving is an excellent way to prevent anemia.23 In fact, ready-to-eat cereals are among the top contributors to iron, folate, vitamin A and C, and zinc intakes.24
Table 4
The third approach is through supplementation of individuals or communities at risk. This approach would be implemented for the treatment of individuals with anemia or in situations where at-risk communities of infants and young children do not have ready access to targeted iron-fortified foods (e.g., geographically isolated Aboriginal communities).25 When a soluble form of iron (such as ferrous sulfate or fumarate) is ingested in the proper dose, this intervention is efficacious. However, adherence to long-term ingestion of oral iron drops is often poor because of the unpleasant metallic taste of drops; drops can stain a baby's teeth unless wiped off immediately after use; and if the dose is high, the infant may complain of abdominal discomfort. In recently completed studies in anemic infants, it has been demonstrated that the impact of iron drops on anemia is equally effective if the drops are provided once daily versus the traditional 3 times daily, without additional “side effects.” Daily dosing may improve compliance with this intervention.26
The case revisited
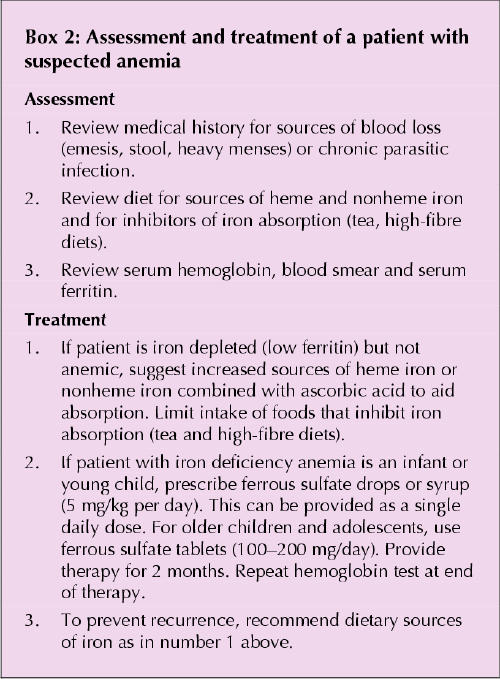
Blood work, which included a complete blood count and measurement of serum ferritin and transferrin receptor levels, revealed a hypochromic microcytic anemia (hemoglobin 92 g/L) and a ferritin level that was less than 12 μg/L. Serum transferrin receptor, a relatively new measure of the availability of iron to the erythrocyte, was elevated at 12 mg/L, which is consistent with iron deficiency anemia. Because ferritin is an acute phase reactant, it may be falsely elevated in the presence of infection or inflammation. Serum transferrin receptor, however, is insensitive to inflammation and can be used to distinguish iron deficient anemia from the anemia of chronic disease.27 A 2-month treatment course with daily ferrous sulfate drops was initiated. A repeat blood sample 10 days later that revealed an increase in hemoglobin of 5 g/L and a brisk reticulocyte response confirmed the diagnosis of iron deficiency anemia and was evidence of an appropriate hematologic response. Concurrent dietary counselling is important to maintain the child's nonanemic status when treatment is completed (Box 2). A list of recommended foods that contain a lot of highly available heme iron (Table 3) and nonheme iron (Table 4) was provided to the child's caregiver.
Box 2.
Summary
Iron deficiency anemia in childhood and adolescence is associated with serious adverse outcomes that may not be reversible. Infants born prematurely, infants who are exclusively breast-fed for a prolonged period and adolescent girls who are menstruating and restricting their food intake are particularly at risk. It can be prevented through the use of iron-containing or iron-fortified foods such as meat and fortified breakfast cereals. If anemia is detected, it should be treated with appropriate doses of bioavailable iron, such as ferrous sulfate or fumarate.
Articles in this series .
Hoffer LJ. Clinical nutrition: 1. Protein–energy malnutrition in the inpatient. CMAJ 2001;165(10):1345-9.
Atkinson SA, Ward WE. Clinical nutrition: 2. The role of nutrition in the prevention and treatment of adult osteoporosis. CMAJ 2001;165(11):1511-4.
Young SN. Clinical nutrition: 3. The fuzzy boundary between nutrition and psychopharmacology. CMAJ 2002;166(2):205-9.
Holub BJ. Clinical nutrition: 4. Omega-3 fatty acids in cardiovascular care. CMAJ 2002;166(5):608-15.
Birmingham CL, Jones PJ. Clinical nutrition: 5. How much should Canadians eat? CMAJ 2002;166(6):767-70.
Jeejeebhoy KN. Clinical nutrition: 6. Management of nutritional problems of patients with Crohn's disease. CMAJ 2002;166(7):913-8.
Jones PJ. Clinical nutrition: 7. Functional foods — more than just nutrition. CMAJ 2002;166(12):1555-63.
Footnotes
This series is supported, in part, by an unrestricted educational grant from the Danone Institute of Canada.
This article has been peer reviewed.
Acknowledgements: Dr. Zlotkin's research program on the prevention and treatment of iron and micronutrient deficiencies in infants and children was supported by grants from the US Agency for International Development's OMNI Research Program through the Human Nutrition Institute of the International Life Sciences Institute Research Foundation, from the Canadian Institutes of Health Research and from the H.J. Heinz Company Foundation to the Hospital for Sick Children Foundation, Toronto, Ont.
Competing interests: Dr. Zlotkin is an occasional consultant to General Mills Canada, Gerber Products Company and Mead Johnson Nutritionals.
Correspondence to: Dr. Stanley Zlotkin, Department of Pediatrics, The Hospital for Sick Children, 555 University Ave., Toronto ON M5G 1X8; fax 416 813-4972; szlotkin@sickkids.ca
References
- 1.World Health Organization. Malnutrition: the global picture. Geneva: The Organization; 2000.
- 2.Grantham-McGregor S, Ani C. A review of studies on the effect of iron deficiency on cognitive development in children. J Nutr 2001;131:649S-668S. [DOI] [PubMed]
- 3.Pollitt E. Iron deficiency and cognitive function. Ann Rev Nutr 1993;13:521-37. [DOI] [PubMed]
- 4.Lozoff B, Jimenez MD, Hagen J, Mollen E, Wolf AW. Poorer behavioral and developmental outcome more than 10 years after treatment for iron deficiency in infancy. Pediatrics 2000;105:E51. [DOI] [PubMed]
- 5.Zlotkin SH, Ste-Marie M, Kopelman H, Jones A, Adam J. The prevalence of iron depletion and iron-deficiency anaemia in a randomly selected group of infants from four Canadian cities. Nutr Res 1996:729-33.
- 6.Willows N, Dewailly E, Grey-Donald K. Anemia and iron status in inuit infants from Northern Quebec. Can J Public Health 2000:91;407-10. [DOI] [PMC free article] [PubMed]
- 7.Willows N, Morel J, Grey-Donald K. Prevalence of anemia among James Bay Cree infants of Northern Quebec. CMAJ 2000:162(3);323-6. [PMC free article] [PubMed]
- 8.Yip R. The challenge of improving iron nutrition: limitations and potentials of major intervention approaches. Eur J Clin Nutr 1997;51:516-24. [PubMed]
- 9.Dallman PR. Changing iron needs from birth through adolescence. In: Fomon SJ, Zlotkin SH, editors. Nutritional anemias. Nestle Nutrition Workshop Series. New York: Vevey/Raven Press; 1992. p. 29-38.
- 10.Saarinen UM. Need for iron supplementation in infants on prolonged breastfeeding. J Pediatr 1978;93:177-80. [DOI] [PubMed]
- 11.Food and Nutrition Board, Institute of Medicine. Dietary reference intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium and zinc. Washington: National Academy Press; 2001. [PubMed]
- 12.American Academy of Pediatrics, Committee on Nutrition. Iron supplementation for infants. Pediatrics 1976;58:765-8. [PubMed]
- 13.Statement of the Joint Working Group: Canadian Paediatric Society, Dietitians of Canada and Health Canada. Nutrition for healthy term infants. Ottawa: Ministry of Public Works and Government Services; 1998. Highlights available: www.hc-sc.gc.ca/hppb/childhood-youth/cyfh/homepage/nutrition/index.html (accessed 2002 Nov 18).
- 14.Gibson RS. Ferguson EL, Lehrfeld J. Complementary foods for infant feeding in developing countries: their nutrient adequacy and improvement. Eur J Clin Nutr 1998;52:764-70. [DOI] [PubMed]
- 15.Walter T, Dallman PR, Pizarro F, Velozo L, Pena G, Bartholmey SJ, et al. Effectiveness of iron-fortified infant cereal in prevention of iron deficiency anemia. Pediatrics 1993:91;976-82. [PubMed]
- 16.Zlotkin SH, Beaton GH, Tanaka P, Anderson GH, Menon IA, Yeung DL. Double blind trial of iron fortification of infant cereals: effect on growth and haematologic status. Pediatr Res 1993:33:113A.
- 17.Youdin MBH. Neuropharmacological and neurobiochemical aspects of iron deficiency. In: Dobbing J, editor. Brain, behaviour and iron in the infant diet. London: Springer-Verlag; 1990. p. 83-106.
- 18.Roncagliolo M, Garrido M, Walter T, Peirano P, Lozoff B. Evidence of altered central nervous system development in infants with iron deficiency anemia at 6 mo: delayed maturation of auditory brainstem responses. Am J Clin Nutr 1998;68:683-90. [DOI] [PubMed]
- 19.Angulo-Kinzler RM, Peirano P, Lin E, Garrido M, Lozoff B. Spontaneous motor activity in human infants with iron deficiency anemia. Early Hum Dev 2002;66:67-79. [DOI] [PubMed]
- 20.Bruner AB, Joffe A, Duggan AK, Casella JF, Brandt J. Randomized study of cognitive effects of iron supplementation in non-anaemic iron-deficient adolescent girls. Lancet 1996;348:992-6. [DOI] [PubMed]
- 21.Halterman JS, Kaczorowski JM, Aligne A, Auinger P, Szilagyi P. Iron deficiency and cognitive achievement among school-aged children and adolescents in the United States. Pediatrics 2001;107:1381-6. [DOI] [PubMed]
- 22.Jacobs Starkey L, Johnson-Down L, Gray-Donald K. Food habits of Canadians: comparison of intakes in adults and adolescents to Canada's Food Guide to Healthy Eating. Can J Dietetic Practice Res 2001;62:61-7. [PubMed]
- 23.United States Department of Agriculture (USDA) nutrient database for standard reference: release 14. Beltsville (MD): Nutrient Data Laboratory, Human Nutrition Research Center of the Agricultural Research Service (ARS); 2001. Available: www.nal.usda.gov/fnic/foodcomp/Data/SR14/sr14.html (accessed 2002 Nov 18).
- 24.Subar AF, Krebs-Smith SM, Cook A, Kahle LL. Dietary sources of nutrients among US children, 1989–91. Pedaitr 1998;102:913-23. [DOI] [PubMed]
- 25.Andres NC. Disorders of iron metabolism. N Engl J Med 1999;341:1986-95. [DOI] [PubMed]
- 26.Zlotkin SH, Arthur P, Antwi KY, Yeung G. Randomized controlled trial of single versus three-times daily ferrous sulfate drops for treatment of anemia. Pediatrics 2001;108:613-6. [DOI] [PubMed]
- 27.Skikne B, Flowers CH, Cook JD. Serum transferrin receptor: a quantitative measure of tissue iron deficiency. Blood 1990;75:1870-6. [PubMed]


