Abstract
Purpose
To investigate the set up and operation of a Managed Clinical Network for cardiac services and assess its impact on patient care.
Methods
This single case study used process evaluation with observational before and after comparison of indicators of quality of care and costs. The study was conducted in Dumfries and Galloway, Scotland and used a three-level framework.
Process evaluation of the network set-up and operation through a documentary review of minutes; guidelines and protocols; transcripts of fourteen semi-structured interviews with health service personnel including senior managers, general practitioners, nurses, cardiologists and members of the public.
Outcome evaluation of the impact of the network through interrupted time series analysis of clinical data of 202 patients aged less than 76 years admitted to hospital with a confirmed myocardial infarction one-year pre and one-year post, the establishment of the network. The main outcome measures were differences between indicators of quality of care targeted by network protocols.
Economic evaluation of the transaction costs of the set-up and operation of the network and the resource costs of the clinical care of the 202 myocardial infarction patients from the time of hospital admission to 6 months post discharge through interrupted time series analysis. The outcome measure was different in National Health Service resource use.
Results
Despite early difficulties, the network was successful in bringing together clinicians, patients and managers to redesign services, exhibiting most features of good network management. The role of the energetic lead clinician was crucial, but the network took time to develop and ‘bed down’. Its primary “modus operand” was the development of a myocardial infarction pathway and associated protocols. Of sixteen clinical care indicators, two improved significantly following the launch of the network and nine showed improvements, which were not statistically significant. There was no difference in resource use.
Discussion and conclusions
The Managed Clinical Network made a difference to ways of working, particularly in breaching traditional boundaries and involving the public, and made modest changes in patient care. However, it required a two-year “set-up” period. Managed clinical networks are complex initiatives with an increasing profile in health care policy. This study suggests that they require energetic leadership and improvements are likely to be slow and incremental.
Keywords: clinical networks, disease management, integrated healthcare networks, managed care
Introduction
Initiatives to improve the quality of care through reorganisation of services have a long history. In the United Kingdom, the most recent innovation is the use of network-based organisations to encourage more widespread integration of services and improvement in quality of care [1]. While professional staff in the National Health Service (NHS) have historically worked in informal professional networks, national policy was steered toward more formal networks following the Calman Hine report (1995) on cancer services and the Acute Services Review for Scotland (1998) [2–3]. The concept of networks is well established in other sectors, particularly in the USA, and it is suggested that they will become the main form of health service organisation in the next twenty years [1, 4–6].
Goodwin et al., in their comprehensive review of networks, suggest that clinical networks allow for continuous working relationships between individual clinicians and their organisations, improving the care for patients required across a range of institutions [1]. Advocates of clinical networks suggest that they can: make more efficient use of staff; reduce professional boundaries; allow good practice to be shared; put patients at the centre of care; and improve access to care [7]. However, there is as yet, little understanding of the impact of networks on patient care or much evidence on the most appropriate ways to organise and manage networks in health care [1, 8].
Scotland has the second highest mortality rate from coronary heart disease (CHD) in Western Europe and improving the care for patients with CHD is a national priority. [3, 9–10]. The Scottish NHS’ Acute Services Review highlighted the need for improvement across Scotland in thrombolysis, secondary prevention of CHD and cardiac rehabilitation. It identified a lack of co-ordination of services and staff; ambiguity of roles, advice and treatment; and uncertainty about the best use of resources. Managed clinical networks were recommended as a way to improve these matters by promoting high quality care and integrated service delivery throughout the NHS in Scotland [3]. They were defined as:
“linked groups of health professionals and organisations from primary, secondary and tertiary care, working in a co-ordinated manner, unconstrained by existing professional and Health Board boundaries, to ensure equitable provision of high quality, clinically effective services” [11].
Two types of networks were proposed. The first are national, comprising professionals working at tertiary specialist level. The second are local networks, based in each NHS Board area, and include general practices, Local Health Care Co-operatives (groups of local general practices) and District General Hospitals [9, 12]. NHS Quality Improvement Scotland (the organisation that oversees improving the quality of care and treatment delivered by NHS Scotland) is responsible for endorsing, supporting and monitoring the progress of Managed Clinical Networks [13].
This paper concerns the first local network in Scotland. It was established for cardiac services in Dumfries and Galloway, a predominantly rural area in South West Scotland. It covers a population of 145,800 using thirty-six general practices organised in four Local Health Care Co-operatives, with one District General Hospital [14]. The MCN began as a pilot phase in May 2000 and was formally launched in July 2001. Its broad aims were to provide patients with improved quality of care through better co-ordination between services, the provision of consistent advice and better care and prevention [15].
This paper reports a two-year evaluation of this first local MCN. It combines process and outcome data to answer three interrelated questions:
How was the network set up, how did it operate and what did it do?
What was the impact of the network on quality of patient care?
What were the resource implications of the network?
Finally, it considers these data in relation to current evidence on clinical network development and their future in the UK NHS.
Design and methods
Due to the constraints of funding and time, the evaluation was designed as a single case study; the methods of data collection and analysis were designed to answer the three research questions as follows:
Set up, operation and activities of the network
All minutes of meetings, electronic and paper publications, guidelines and protocols were reviewed. Contemporaneous field notes of meetings were also written. Interviews were carried out with two patients who had been involved in the network, and a random sample of health service personnel which included three consultants, two nurses, one medical director, one nursing director, three general practitioners and two managers. The interviews followed a proforma which covered interviewees’ perceptions of the MCN, its aims, how it was working, together with local barriers and facilitating factors. With permission, interviews were tape-recorded and transcribed. Analysis of documents, field notes and interview transcripts was undertaken concurrently by KH and analytical themes confirmed by RT and SW reading a sample of transcripts. A timeline of structures and activities was constructed from documentary analysis and field notes. Interview transcripts then provided an understanding of how these structures and activities were perceived and identified potential barriers and facilitating factors.
Impact of the network on quality of care
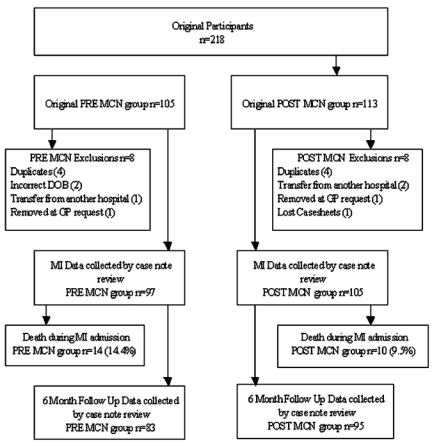
To investigate whether those aspects of quality targeted by the network's quality protocols were achieved, databases from the local District General Hospital were used to identify all patients admitted with a suspected myocardial infarction (MI) between 1st July 2000 and 30th June 2002. The inclusion criteria reduced the original sample of 245 to 218 (Appendix A) [16]. Of the 218 patients in the original cohort there were 16 exclusions (Appendix B). All of the remaining 202 patients consented to inclusion in the study. The variables chosen for study were those identified as important for high quality care by the Scottish Clinical Standards Board and the English and Welsh National Service Framework [17]. Data were abstracted from hospital and general practice held case sheets by KH for the period which covered the time of MI and for a follow-up period of 6 months post MI. Using SPSS for Windows release 10.0.7, linear regression techniques were used to investigate the segmented interrupted time series to determine the difference between clinical indicators of quality of care before and after the MCN launch, after adjusting for time trends and patient characteristics [18]. Independent variables considered in the multiple regression models are listed in Box 1. A test for the change in slope was carried out by fitting a time X pre-post interaction term (MCN Interaction Term). Statistical significance was set at p=0.05.
Box 1. Independent variables used in clinical and economic analysis.
Pre/Post MCN
Month of MI
MCN Interaction Term (MI Month (1–24)(Pre/Post MCN (0 or 1))
Gender
Age at MI (years)
Practice Type:Urban or Rural (as defined by >30 minutes transfer time to local hospital)
Carstairs social deprivation category score (based on measures of income and overcrowding) [19]
Co-morbidity (Previous history of any of the following:
MI (Myocardial Infarction or ‘Heart Attack’)
Angina (Chest pain on exertion relieved by rest)
Bypass surgery (Operation which takes blood around a blocked coronary artery)
Angioplasty (Operation to unblock a coronary artery)
Cerebrovascular disease
Peripheral vascular disease
Chronic obstructive airways disease
Arthritis
Hypertension (defined as >160/90 or already on treatment)
Diabetes (previous history or new diagnosis)
Current smoker
Overweight (defined as Body Mass Index >25 kg/m2)
Economic implications of the network
The transaction costs of the network were calculated to include initial project set-up grants and estimates of the value of time for those attending MCN meetings, abstracted from meeting minutes. The resource implications were investigated by examining all resources used by the 202 patients who had an MI in the study period, with data collected retrospectively alongside the clinical data. The resource costs per patient incorporated all NHS costs from the time of hospital admission to 6 months post-discharge and included both costs in primary care (general practice visits and prescribing) and secondary care (hospital stays and outpatient visits). The average cost per patient before and after the MCN was introduced was compared using regression analysis to control for time trends and patient characteristics. Statistical significance was set at p=0.05.
Results
Network set-up, operation and activities
Instigation and infrastructure
The Dumfries and Galloway MCN was the first local network in Scotland. Initial impetus for the project had come from a general practitioner involved in local management who took on the network's clinical leadership. It began as a one-year pilot project in May 2000 with a grant of £50,000 from the Scottish Executive Health Department to fund three part-time posts: a lead clinician, a network manager and an administrator. The lead clinician was appointed in July 2000 for 2 sessions per week with the key responsibility of clinical leadership of the MCN in addition to promotion of evidence-based practice, liaison with existing local health care and public involvement groups, and leadership in the development and reconfiguration of cardiac services in the region. The network manager and administrator were appointed in October 2000 with supportive roles of the work of the lead clinician and administration of the developing network.
The MCN infrastructure proved fragile; when the manager left after 10 months, and was not replaced, its progress was solely dependent on the lead clinician. He was very much ‘in control’ in the early stages of network development as he single-handedly created the vision for the MCN, designed it and set its work patterns in the early stages. This was recognised in interviews, with one interviewee saying that “[the MCN is down to] the personal drive of one man” [A3aB]. However, there were both positive and negative views about this, illustrated in Box 2.
Box 2. Examples of interviewees' perceptions of the managed clinical network.
Network Set-up and Operation
– Clinical leadership
“I think it is useful for an area to have a clinical champion”[A1aG]
“It has developed in the way it has because it has been very much led by an individual who has the drive to actually move the agenda forward. I think one of the problems with that perhaps is that the general population has been rather left behind or engulfed in the wake of the process rather than making a difference.”[A3aG]
– Early scepticism and lack of support
“I suppose it is an attempt to co-ordinate the delivery of cardiac care across conventional barriers. My fear is that it will simply rearrange a number of deckchairs. My hope is that it will eliminate a number of frustrations that exist in the current system which lead to poorer quality of care. “ [B2aC]
“The other thing is that how committed are the highest level of the organisations to these Networks? A Network can have its own work plan, its own direction of travel and I'm sure can achieve quite a lot on its own, but how valuable to it is commitment from the very top? And how much difference could that make to its success or failure? “ [B5bN]
Network Activities
– Collaboration
“It is trying to involve patients in the work that hospitals do and bring medical people and patients closer together.”[E1b]
“The fact that the MCN meets on a regular basis to actually go over some of the issues and it takes patients views very strongly and its committees do involve patient groups, that is not something that is usually done in other clinical areas”[A2aG]
– Communication
“There has not been the same emphasis in the past on sharing information between primary and secondary care, and also between different parts of primary care as to how well we are delivering our services and how universally we are targeting patients with heart problems.“ [A4aG]
“Through the network protocols and leaflets we know what is happening and when and how everything works”[E1a]
– Quality
“The aim is to get a common pathway of treatment so that we standardise things to promote quality care for all patients.”[A1aG]
“It is an attempt to co-ordinate the delivery of cardiac care across conventional barriers.”[C1bC]
– Equity
“It is about equity of access for all customers.”[B1aC]
“It is definitely in the patients best interest to have seamless care and viewing the whole journey wherever you are, and for the Network to take ownership of that. Managers, folk who manage the health service don't get down to that level of improvement, that's clinician and patient led. The MCN facilitates that”[B5bN]
The desirability of independence from existing institutional and professional structures was built into the notion of MCNs from the beginning [9]. Financial and clinical responsibilities remained separate and no binding contracts between organisations were written to support the work of the MCN. There was resistance from some managers to the MCN in its early days, in particular to its role in setting and operationalising strategy. It was felt to be in an “uncomfortable position” straddling three NHS organisations [B2bN]. Certainly, some interviewees were uncertain that the MCN had support from some elements of senior management, see Box 2. Whilst this did not lead to a breakdown of the MCN, it was felt to have slowed down its progress. Some interviewees expressed concerns over difficulties with “presenting a unanimous front” [A3aG] which they felt “had made the process more complicated than it needed to be” [C1b].
In addition, the MCN also faced initial scepticism from some clinicians, who partly felt that it was capitalising on previous advances in cardiac care in the region, illustrated in Box 2. Certainly, there were a number of projects dedicated to improvements in care such as a Cardiac Rehabilitation Programme, started as early as 1990, and a Cardiac Services Group started in 1999. There were also more discrete projects such as a Cardiology Redesign Project, completed in 2000, nurse-administered thrombolysis in the Acute Trust and a Triage Monitoring Project, started at the same time as the MCN in July 2001.
Towards the latter part of the evaluative period, the regional organisation of the NHS in Dumfries and Galloway changed. The existing NHS Trusts merged, and NHS Dumfries and Galloway became a vertically integrated provider organisation with one Board responsible for planning and delivering health care in the area. A cardiac services group was set up by the new Unified Board, on which the MCN lead clinician was given a strategic role. This group also had a remit to act as a management board for the MCN so that, by the end of the study, the extent of the MCN's incorporation into the routine NHS structure was substantially greater.
Network activities
While the broad aim, or mission, of the network was published in an article in the British Medical Journal [15] and generic MCN activities were suggested in an Executive Letter from the Scottish Executive Health Department (which act as instructions for regional and local health organisations) [11], the network did not identify specific, clear, operational goals to achieve its broad aims from the outset. This was reflected in some interviewee comments, such as one when asked whether they knew what the MCN was doing: ‘Not really, it's a bit like “the Matrix”’ (a film about alternative realities widely viewed at the time)” [C1bC]. However, although not articulated publicly, analysis of documentation and interviews suggests that the work of the MCN throughout the evaluative period was underpinned by four inter-linked principles: collaboration; communication; quality and equity.
From an early stage efforts were focused on collaboration through bringing together representatives from all sectors involved in cardiac care, including patients and carers from local self-help groups, into its operational groups. These were five overlapping working groups: public involvement; service mapping and care pathways; protocols, guidelines and standards; information management and technology; finance and administration; which used the tools of health service redesign in their work (including service mapping, developing quality assurance systems, incorporating the concept of the “typical patient journey”) [20]. As illustrated in Box 2, this new, collaborative approach was well received by most clinicians and patients.
There was an early emphasis on communication, which remained a feature throughout the study period. Although relatively good communications existed between primary and secondary care, as illustrated by a comment from one patient “Here the cardiologists know a lot of the GPs by their first name, I don't know that other regions would be able to boast that” [A3bG], the network set up a new approach to empower the public in planning regional cardiology services with clinicians and managers. Communication skills training was organised for patients and carers to encourage active participation in working group meetings. The aim was to facilitate effective public involvement in these groups, and was approved by both patients and professionals, as suggested by interview data, illustrated in Box 2.
The working group activities were disseminated through regular newsletters, which included another new concept, “a patient story” (a patient-recalled clinical experience), and a specially created website [21]. Again, these new approaches were favourably received as one GP commented “I found the newsletter is very helpful. It is something I can get through very quickly in my paper bundle” [A1aG].
The activities of the working groups resulted in a quality assurance programme, which supported increasing patient and carer involvement in service redesign through the voluntary sector and local self-help groups. It also detailed public information, clinical governance structures, equipment levels and staff training. The concept of “a typical patient journey” was used in the design of a care pathway for chest pain and acute myocardial infarction. Patients and their carers were involved in the drawing-up of thirteen associated protocols with professionals, which were detailed for each stage of the care pathway, set explicit quality targets, were accredited by NHS QIS and widely disseminated through meetings, electronic and paper publication. There was also an emphasis on the development of information technology systems to support the delivery of care across boundaries and piloting of a patient-held cardiac record.
In keeping with the “incremental approach to service improvement” [B5bN], the process of mapping regional cardiac services revealed substantial inequalities between rural parts of the region with elsewhere, particularly in equity of access to cardiac rehabilitation and thrombolysis [22]. Subsequently a pre-hospital thrombolysis training programme for ambulance staff and all ‘rural’ general practitioners was developed and all GPs signed up to a regional pre-hospital thrombolysis protocol. Further to a successful opportunistic funding bid for two heart failure nurses, the network's focus shifted to heart failure. A heart failure strategy was designed and the MCN began to develop a regional heart failure service with initial work focusing on inequity in access to heart failure nurse management.
Impact of the MCN on quality of patient care
As indicated, a major feature of MCN activity was the drawing up of an “MI pathway” with thirteen detailed protocols of related care. These protocols provided sixteen clinical indices of quality of care.
The MCN was launched on 1 July 2001, 97 MIs occurred in the 12-month observation period preceding this date and 105 MIs in the twelve-month period which followed it. The average age of patients was 63 years at time of infarct and males outnumbered females by 2:1. Over a quarter (28%) had at least one recorded co-morbidity. The majority came from urban practices (61%) and, using Carstairs deprivation score, over a third belonged to deprivation categories 4 and 5 (most deprived). Table 1 describes these patient characteristics before and after the launch of the network.
Table 1.
Summary of patient characteristics (values are numbers (%) of participants unless stated otherwise)
| Characteristic | Pre MCN | Post MCN | |
|---|---|---|---|
| Gender | Men | 59 (60.8) | 76 (72.4) |
| Women | 38 (39.2) | 29 (27.6) | |
| Mean (SD) age at event | 63 (9) | 63 (9) | |
| Attend rural practice | 41 (42.3) | 38 (36.2) | |
| Have co-morbidity | 29 (29.9) | 28 (26.9) | |
| Median Carstairs Depcat score | 3 | 3 | |
Table 2 details the quality indicators of the MCN protocols for myocardial infarction and related care observed. In the majority of areas a non-significant trend of modestly improving standards was noted. Although pre hospital thrombolysis administration had been extensively targeted in the MCN training programme, during the observation period the number of patients treated remained very small (n=4), and no further analysis was carried out on this aspect of care. However, two areas: immediate aspirin administration in the community and pain to needle times showed statistically significant improvements following the MCN launch as detailed in Table 3.
Table 2.
Summary of clinical data in relation to MCN protocols
| Area | MCN Protocol | Result |
Difference between pre and post MCN p-value* | |
|---|---|---|---|---|
| Pre MCN (n=97) | Post MCN (n=105) | |||
| Immediate aspirin | All to receive immediate aspirin | 63.6% | 67.7% | 0.56 |
| Thrombolysis | All to be considered for thrombolysis | 48.3% | 59% | 0.14 |
| 50% to achieve door to needle target (≤30 minutes) | 31% | 45.6% | 0.14 | |
| Achieve pain to needle target (≤90 minutes) | 15% | 32.7% | 0.05 | |
| Median pain to needle times (hh:mm [range]) | 2:27 [10:45] | 2:09 [10:17] | 0.2° | |
| Discharge medication | 70% on antiplatelet agents | 97.6% | 97.9% | 0.89 |
| 70% on betablockade | 60.2% | 68.1% | 0.28 | |
| 70% on ACEI | 90.2% | 88.4% | 0.70 | |
| 70% on Statin (with cholesterol >5.00) | 78.6% | 88.7% | 0.10 | |
| Cardiac rehabilitation | All seen by rehab nurse pre discharge | 96.4% | 96.8% | 0.87 |
| All have out-patient rehab arranged pre discharge | 88.8% | 92.4% | 0.41 | |
| All attend out-patient rehab programme | 75.9% | 76.4% | 0.94 | |
| Secondary prevention at 6 months post MI | 70% on antiplatelet agents | 98.8% | 97.8% | 0.62 |
| 70% on betablockade | 61.3% | 75% | 0.05 | |
| 70% on ACEI | 87.3% | 85.4% | 0.71 | |
| 70% on Statin (with cholesterol >5.00) | 80.3% | 95.5% | 0.007 | |
Refers to chi-squared test of difference for pre-post comparisons.
°: Refers to Mann-Whitney test of difference for pre-post comparisons.
Table 3.
Results of multiple linear regression* of aggregated weekly outcomes pre and post introduction of the MCN
| Outcome | Difference in level post vs. pre |
Difference in slope post vs. pre |
||
|---|---|---|---|---|
| Regression Coefficient (se) | p-value* | Regression coefficient (se) | p-value* | |
| Immediate aspirin | −35.9 (16.9) | 0.037 | 0.937 (0.561) | 0.099 |
| Median pain to needle time (log transformed) | −1.207 (0.605) | 0.051 | 0.025 (0.010) | 0.014 |
Adjusted for time trends, autocorrelation and co-morbidity.
Economic implications of the MCN
Set-up and operational costs
The total set-up costs of the MCN were £52,615 during its pilot year. Following its launch in July 2001, a further £50,000 was allocated for administrative support and time of the clinical lead. Because of the difficulty of obtaining data on the time costs for informal meetings and the other resources used to run the network that were not routinely recorded, both of these estimates are likely to underestimate the true costs of setting up and running the MCN.
Resource costs
As detailed in Table 4, the cost of hospital care at time of MI did not change, the median length of stay being 7 days (range: 57) both before and after the MCN launch. Of those surviving to discharge, the number of review contacts in the 6-month period post MI ranged from 0 (for nine patients) to 36 (for one). Overall, the MCN had no impact on NHS resource use with median resource costs per patient of £2,055 before and £2,053 after its launch.
Table 4.
Summary of economic data
| Cost | Median (Range) Cost Per Patient |
Difference between pre and post MCN p-value1 | |
|---|---|---|---|
| Pre MCN | Post MCN | ||
| Hospital costs | £1,601 (£629,£7,290) | £1,565 (£805,£9,845) | 0.18 |
| Follow up costs | £424 (£231,1,246) | £413 (£212,£1,445) | 0.61 |
| Total costs | £2,055 (£629,£7,290) | £2,053 (£805,£9,845) | 0.35 |
Refers to p-value from linear regression.
Discussion
The managed clinical network for cardiac services in Dumfries and Galloway was the first in Scotland and the research described here is unusual in that it has collected both process and outcome data. The development of clinical networks is now firmly embedded in UK health policy and similar approaches to integration are occurring throughout the developed world [23–29]. This discussion debates the study findings and the limitations of the data, before going on to consider the network's structure and management in light of current understanding, and summarising lessons for future development of clinical networks.
Set-up and operation of the network
The evaluation of the set-up and initial operation of the Dumfries and Galloway MCN depicts a relatively unstable foundation phase in which its development depended largely upon the enthusiasm and commitment of the lead clinician. However, his efforts may not have sustained the progress of the network had it not been for the change in the network structure as it moved from mainly enclave-like (with a flat internal structure based on shared commitment to improving cardiac care) to mainly hierarchical (with its organisational core established as part of the NHS Dumfries and Galloway and the role of the lead clinician confirmed). In making this move, it became more stable and more accepted by managers and clinicians. This shift is not uncharacteristic of network development, as indicated by Goodwin et al. who describe three types of network structure: enclave, hierarchical and individualistic, although they suggest that in practice most show characteristics of more than one ‘type’ [1, 8].
Two contextual features probably influenced this change in structure and acceptance. First, the local NHS was reorganised towards the latter part of the evaluation so that previously separate planning (the NHS Board) and providing (the acute and primary care trusts) functions were incorporated into one vertically integrated organisation called NHS Dumfries and Galloway. This enabled the MCN to be incorporated into accepted administrative structures. Second, over the life of the evaluation the use of MCNs to improve service integration and quality of care became even more firmly rooted in Scottish Health Policy and further guidance was issued [11]. In short, MCNs moved from being a voluntary to a mandated activity. The influence of strong, coherent, national policy on the success of complex innovations in the health service has previously been demonstrated [30–32]. In this case, Dumfries and Galloway began to be seen as a ‘flagship’ network. In this context the tendency of professionals in partnerships to take on ‘clannish’ tendencies was reinforced and the clinicians began to be proud of their position in ‘the first local cardiac network’ in Scotland [33].
Impact of the network on quality of care
Due to resource and other practical constraints, the evaluation was designed as a single case, before and after study of clinical indicators of outcomes of care, with concurrent process evaluation. This design has a number of limitations, not least of which concerns the attribution of causality in relation to any observed changes in clinical indicators of care. We attempted to overcome this difficulty by examining clinical care which had been specifically targeted through the MCN protocols. However, in the UK, in common with elsewhere, there were many other approaches to improving the management and secondary prevention of MI and we cannot be confident that changes observed were because of the work of the MCN [17, 34–37].
Most of the indicators of quality of clinical care improved following the launch of the network; however, the differences are small and could be accounted for by chance. Given the size of Dumfries and Galloway a lengthier study or a comparative evaluation with elsewhere would be necessary to reduce this chance factor.
A number of projects dedicated to improvements in cardiac care were in place before the set up of the network in Dumfries and Galloway and patients were already receiving standards of care as high as the best Northern European Countries reported in Euroaspire II [38]. Thus, it is possible that this ‘ceiling effect’ meant that few improvements were possible. However, in keeping with comparative evaluations of other health service innovations, the prior experience of staff in quality initiatives for cardiac care was likely to have influenced the network's approach [31–32]. This may not be the case in other areas developing mandated clinical networks and the potential for improvement may be greater.
Economic implications of the network
No differences in NHS resource use were observed after the MCN was launched. However, the set up and transaction costs were dependent on the resources estimated to run this specific network. The actual budget allocated to support the administration and leadership of the network is almost certainly an underestimate and other managed clinical networks may require different amounts depending on the existing level of co-ordination of services.
Lessons for future development of clinical networks
The management briefing based on Goodwin et al.'s research suggests ten key lessons for managing networks, listed in Box 3 [8].
Box 3. Ten key lessons for managing networks (Drawn from NHS Service Delivery and Organisation R&D Programme Networks Briefing. Key lessons for network management in health care [39]).
Achieve a position of centrality within the network
Have a clear mission statement and unambiguous rules of engagement
Be inclusive – ensure all agencies and individuals gain ownership of the network
Avoid large networks
Develop strategies for network cohesions
Consider formalised contracts and agreements to facilitate ownership
Actively engage respected professional leaders
Avoid network capture by a professional elite or dominant organisation
Ensure the networks remains relevant and worthwhile
Ensure that professionals allow network managers to manage and govern their activities.
Although the Dumfries and Galloway MCN was developed at least four years before the publication of the review and management briefing paper, it did exhibit many of the suggested characteristics of successful network management, each of which are addressed to follow.
The lead clinician established his centrality very early on, his position was pivotal, and despite a considerable workload and lack of project management support, he was dedicated, energetic and enthusiastic. The importance of clinical leadership to facilitate organisational change and quality improvement is now widely recognised as is the importance of sfc project management [7, 31, 40–41]. In this case, the clinical lead acted as the co-ordinator and ‘boundary spanner’ (someone who works across existing professional enclaves or with isolates in historically established practice [39]), using interpersonal relationships, working contacts to gain information, understanding values and undertaking negotiations. However, if the organisation depends too heavily on single individuals, or if the leader does not have access to significant leverage, this model may not be sustainable, and investment in multi-professional leadership teams may provide more stability [40, 42].
The MCN did not have clear operational goals from the outset, however, it did have clear and accepted vision, and all of its activities were underpinned by the principles of collaboration, communication, quality, and equity. In attempting health care reform, it is important to understand what motivates professionals in their daily work [41]. The network's principles had widespread support from those involved in the Scottish NHS and it is likely its goals were also congruent with those of the individuals and organisations involved in the network [1]. It is also likely that it harnessed the intrinsic motivations of professionals to do well by their patients, and of patients to do what they can for the NHS as a whole so that the lack of operational goals was not problematic. Future managed clinical networks may also be able to harness extrinsic motivations as well as intrinsic motivations, for example, the financial need to reduce length of hospital stay [43] or the economic incentives offered by the new contract for UK general practice [44]. In addition, networks may consider devoting specific resources to networks which can be used to incentivise the delivery of high quality care [45].
The Dumfries and Galloway MCN was set up and operated to ensure inclusion of all professionals and organisations and put particular effort into engaging with patient, carer and public groups but also with lead clinicians for cardiac care (from both nursing and medical professions). This process of engagement was aided by the size of Dumfries and Galloway. Physicians already knew one another and it was relatively easy to start the public engagement process through local self-help groups. Network cohesion was facilitated not only through the role of the lead clinician as ‘boundary spanner’ but also through investment in communication, which did seem to energise participants. It may have helped clinicians and managers to make the essential step for quality improvement in developing ‘the ability to see services from the patient's point of view’ (page 1979, [41]).
The MCN did not use formalised contracts and agreements, although it did seek accreditation from NHS Quality Improvement Scotland at an early stage and thus established itself as a legitimate organisation. It managed to avoid ‘capture’ by any one organisation probably because the lead clinician was a GP rather than a cardiac specialist and because he was so successful at working across the boundaries between existing organisations from a relatively marginal position. The core business of the MCN—to improve quality of care—is the core business of individual professionals as well as their organisations and so it was not difficult for the MCN to maintain its relevance to all concerned (and not least the patients). Finally, although professionals in the MCN did not mandate the lead clinician or manager to govern their activities, accreditation and monitoring was provided by NHS QIS, which may have alleviated this need.
Conclusions
Managed Clinical Networks are complex initiatives with an increasing profile in health care policy [1]. The Dumfries and Galloway network addressed practical issues of network development with clinicians from all backgrounds and sectors working across traditional boundaries. In addition through working group activity, it actively involved the public and patients in service design and focus. It had broad aims rather than explicit goals and proceeded organically, responding to locally identified needs and making the most of opportunities. It made modest changes to patient care and had no impact on NHS resource use. The MCN took a full two years to set up and become accepted into local structures. Complex organisational changes take time to develop and improvements are likely to be slow and incremental. These features may not be what politicians and reformers want, but require recognition in setting up similar complex interventions elsewhere. As Ham et al. write ‘the Quality Chasm is most likely to be crossed through a long slow journey rather than a single massive leap’ (page 438, [31]).
Acknowledgments
We are grateful to interviewees; to patients for permission to use information from their NHS records; to all general practices in Dumfries and Galloway for enabling access to patients’ records; to staff in Dumfries and Galloway Royal Infirmary for assistance in data retrieval and to L. Staffell who created the computer-based query. This study was funded by the Coronary Heart Disease taskforce of the Scottish Executive Health Department. The Health Economics Research Unit is funded by the Chief Scientist Office of the Scottish Executive Health Department. The views are those of the authors and not the Scottish Executive.
Appendix A: Inclusion criteria for clinical and economic analysis
Age <76 years at time of event*
Confirmed discharge diagnosis of Myocardial Infarction between 01/07/2000-31/06/2002 verified by casesheet retrieval by the Research Fellow (KH) and a cardiologist using any two of the following three diagnostic criteria:
typical pain
typical ECG – sequential changes, with or without Q waves (if cardiac enzymes negative has to have Q waves)
typical cardiac enzyme rise – 2 × (ULN for AST.
Not temporarily resident in Dumfries and Galloway
*to allow comparability with other studies.
Appendix B: Study profile for clinical and economic analysis
Contributor Information
Karen E StC Hamilton, Tayside Centre for General Practice, University of Dundee, Kirsty Semple Way, Dundee, DD2 4BF Scotland.
Frank M Sullivan, Tayside Centre for General Practice, University of Dundee, Kirsty Semple Way, Dundee, DD2 4BF Scotland.
Peter T Donnan, Tayside Centre for General Practice, University of Dundee, Kirsty Semple Way, Dundee, DD2 4BF Scotland.
Rex Taylor, Crichton Campus, University of Glasgow, Bankend Road, Dumfries, Scotland.
Divine Ikenwilo, Health Economics Research Unit, Polwarth Building, University of Aberdeen, Foresterhill, Aberdeen AB25 2ZD Scotland.
Anthony Scott, Health Economics Research Unit, Polwarth Building, University of Aberdeen, Foresterhill, Aberdeen AB25 2ZD Scotland.
Chris Baker, Dumfries and Galloway Managed Clinical Networks for Coronary Heart Disease Crichton Royal Hospital, Dumfries DG14TG Scotland.
Sally Wyke, Central and North Alliance for Self-Care, Department of Nursing and Midwifery, University of Stirling, Stirling FK9 4LA Scotland.
Reviewers
Alene Hokenstad, MSSA, Project director, United Hospital Fund, New York, USA.
Mirella Minkman, R.N., MSc, Projectleader Integrated care, Senior advisor Dutch Institute for Healthcare Improvement CBO, Utrecht, The Netherlands.
Neil Campbell, Dr., Senior lecturer in General Practice, University of Aberdeen, United Kingdom.
References
- 1.Goodwin N, Perri 6, Peck E, Freeman T, Posaner R. Managing across diverse networks: lessons from other sectors. Final report. Health services management centre. Birmingham:: University of Birmingham; 2003. [Google Scholar]
- 2.Calman K, Hine D. A Policy framework for commissioning cancer. London: Department of health; 1995. [Google Scholar]
- 3.Scottish Executive Health Department. Acute services review report. Edinburgh: Stationery Office; 1998. [Google Scholar]
- 4.Alter C, Hage J. Organisations working together. Newbury Park: Sage; 1993. [Google Scholar]
- 5.Easton G, Georgieva C, Wilkinson I. On the edge of chaos: towards evolutionary models of industrial networks. In: Gemunden HG, Ritter T, Walter A, editors. Relationships and networks in international markets. London: Pergamon Press; 1997. pp. 273–94. [Google Scholar]
- 6.Institute of Medicine. Crossing the quality chasm: a new health system for the 21st Century [Online] [cited 2005 Feb 28]. Available from: URL: http://books.nap.edu/html/quality_chasm/reportbrief.pdf.
- 7.NHS Confederation. Clinical networks. vol 8. NHS Confederation; 2002. [Google Scholar]
- 8.Goodwin N, Perri 6, Peck E, Freeman T, Posaner R. Managing across diverse networks: lessons from other sectors. Research and policy report. Birmingham: University of Birmingham, Health services management centre; 2004. [Google Scholar]
- 9.Scottish Executive Health Department. Coronary heart disease/Stroke task force report. Edinburgh: Scottish Executive Health Department; 2001. [Google Scholar]
- 10.Peterson S, Rayner M. Coronary heart disease statistics. London: British Heart Foundation; 2002. [Google Scholar]
- 11.Scottish Executive Health Department. Introduction of managed clinical networks within the NHS in Scotland. [Online] 1999. Feb 9, [cited 2005 May 01]. Available from: URL: http://www.show.scot.nhs.uk/sehd/mels/1999_10.htm.
- 12.Scottish Executive Health Department. Our national health: a plan for action, a plan for change. Edinburgh: Scottish Executive Health Department; 2001. [Google Scholar]
- 13.NHS Quality Improvement Scotland. MCN quality assurance framework guidance. [Online] [cited 2005 May 01]. Available from: URL: http://www.nhshealthquality.org/nhsqis/files/Draft%20guidance%20manual.pdf.
- 14.Dumfries and Galloway NHS Board. Dumfries and Galloway NHS Board. [Online] [cited 2005 May 01]. Available from: URL: http://www.nhsdg.scot.nhs.uk/dumfries/NHSD_DT_TOP_frontpage.jsp;jsessionid=6BC0DF2E601F478A08E0169A5FB06D58?p_applic=CCC&p_service=Content.show&pContentID=10388&.
- 15.Baker CD, Lorimer AR. Cardiology: the development of a managed clinical network. British Medical Journal. 2000;321(7269):1152–3. doi: 10.1136/bmj.321.7269.1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, Arveiler D, Rajakangas A-M, Pajak A. Myocardial infarction and coronary deaths in the World Health Organisation MONICA project: registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994;90(1):583–612. doi: 10.1161/01.cir.90.1.583. [DOI] [PubMed] [Google Scholar]
- 17.Department of Health. National service framework for coronary heart disease. [Online] [cited 2005 May 01]. Available from: http://www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID=4094275&chk=eTacxC.
- 18.McCain LJ, McCleary R. The statistical analysis of the simple interrupted time series quasi-experiment. In: Cook TD, Campbell DT, editors. Quasi-experimentation: design & analysis issues for field settings. Chicago: Rand McNally; 1979. [Google Scholar]
- 19.Carstairs V, Morris R. Deprivation and health in Scotland. Aberdeen: Aberdeen University Press; 1992. [Google Scholar]
- 20.Locock L. Redesigning health care: new wine from old bottles. Journal of Health Services Research and Policy. 2003;8(2):120–22. doi: 10.1258/135581903321466102. [DOI] [PubMed] [Google Scholar]
- 21.Dumfries and Galloway Managed Clinical Networks for Coronary Heart Disease. MCN: about us. [Online] [cited 2005 May 01]. Available from: URL: http://www.show.scot.nhs.uk/mcn/
- 22.Dumfries and Galloway Managed Clinical Networks for Coronary Heart Disease. Managed clinical network in coronary heart disease pilot project in Dumfries and Galloway: interim report. [Online] [cited 2005 May 01]. Available from: URL: http://www.show.scot.nhs.uk/mcn/
- 23.Kodner DL, Kyriacou CK. Fully integrated care for frail elderly: two American models. International Journal of Integrated Care [serial online] 2000 Nov 1; doi: 10.5334/ijic.11. Available from:URL: http://www.ijic.org. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ahgren B. Chains of care: a counterbalance to fragmented health care. Journal of Integrated Care Pathways. 2001;5:126–32. [Google Scholar]
- 25.Gröne O, Garcia-Barbero M. Trends in integrated care–Reflections on conceptual issues. EUR/02/5037864. Copenhagen: World Health Organisation; 2002. [Google Scholar]
- 26.Scottish Executive Health Department. Promoting the development of managed clinical networks in NHS Scotland. [Online] 2002. Sep 18, [cited 2005 May 01]. Available from: UR: http://www.show.scot.nhs.uk/sehd/mels/HDL2002_69.pdf.
- 27.Scottish Executive Health Department. Coronary heart disease and stroke strategy for Scotland. Edinburgh: Scottish Executive Health Department; 2002. [Google Scholar]
- 28.Scottish Executive Health Department. Partnership for care. Edinburgh: Stationery Office; 2003. [Google Scholar]
- 29.Ugolini C, Nobilio L. Vertical integration and contractual network in the cardiovascular sector: the experience of the Italian region Emilia Romagna. International Journal of Integrated Care [serial online] 2003 Jun 26; doi: 10.5334/ijic.82. Available from: URL: http://www.ijic.org. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pettigrew AM, Ferlie EB, McKee L. Shaping strategic change: making change in large organisations – the case of the NHS. London: Sage; 1992. [Google Scholar]
- 31.Ham C, Kipping R, McLeod H. Redesigning work processes in health care: lessons from the national health service. The Milbank Quarterly. 2003;81(3):415–39. doi: 10.1111/1468-0009.t01-3-00062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wyke S, Mays N, Street A, Bevan G, McLeod H, Goodwin N. Should general practitioners purchase health care for their patients? The total purchasing experiment in Britain. Health Policy. 2003;65:243–59. doi: 10.1016/s0168-8510(03)00040-x. [DOI] [PubMed] [Google Scholar]
- 33.Sullivan H, Skelcher C. Working across boundaries: collaboration in public services. Basingstoke: Palgrave; 2002. [Google Scholar]
- 34.Young W, Rewa G, Goodman SG, Jaglal SB, Cash L, Lefkowitz C, et al. Evaluation of a community-based inner-city disease management program for postmyocardial infarction patients: a randomised controlled trial. Canadian Medical Association Journal. 2003;169:905–10. [PMC free article] [PubMed] [Google Scholar]
- 35.Murchie P, Campbell NC, Ritchie LD, Simpson JA, Thain J. Secondary prevention clinics for coronary heart disease: four year follow up of a randomised controlled trial in primary care. British Medical Journal. 2003;326(7380):84. doi: 10.1136/bmj.326.7380.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pedley DK, Bissett K, Connolly EM, Goodman CG, Golding I, Pringle TH, et al. Prospective observational cohort study of time saved by prehospital thrombolysis for ST elevation myocardial infarction delivered by paramedics. British Medical Journal. 2003;327(7405):22–6. doi: 10.1136/bmj.327.7405.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, De Backer G, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. European Heart Journal. 2003;24(11):987–1003. doi: 10.1016/s0195-668x(03)00114-3. [DOI] [PubMed] [Google Scholar]
- 38.Euroaspire 11 Study Group. Lifestyle and risk factor management and use of drug therapies in coronary patients from 15 countries. Principal results from EUROASPIRE II Euro heart survey programme. European Heart Journal. 2001;22(7):554–72. doi: 10.1053/euhj.2001.2610. [DOI] [PubMed] [Google Scholar]
- 39.NHS Service Delivery and Organisation R&D Programme. Networks briefing. Key lessons for network management in healthcare. [Online] [cited 2005 May 01]. Available from: URL: http://www.sdo.lshtm.ac.uk/pdf/studyinghealthcare_goodwin_briefingpaper.pdf.
- 40.Denis JL, Lamothe L, Langley A. The dynamics of collective leadership and strategic change in pluralistic organisations. Academy of Management Journal. 2001;44(4):809. [Google Scholar]
- 41.Ham C. Improving the performance of health services: the role of clinical leadership. The Lancet. 2003;361:1978–80. doi: 10.1016/S0140-6736(03)13593-3. [DOI] [PubMed] [Google Scholar]
- 42.Degeling P, Maxwell S, Kennedy J, Coyle B. Medicine, management, and modernisation: a ‘danse macabre’? British Medical Journal. 2003;326(7390):649–52. doi: 10.1136/bmj.326.7390.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vanheacht K, Sermeus W. The Leuven clinical pathway compass. Journal of Integrated Care Pathways. 2001;7:2–7. [Google Scholar]
- 44.Lewis R, Gillam S. A fresh new contract for general practitioners. British Medical Journal. 2002;324(7345):1048–9. doi: 10.1136/bmj.324.7345.1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kewell B, Hawkins C, Ferlie E. Calman-Hine reassessed: a survey of cancer network development in England, 1999–2000. Journal of Evaluation in Clinical Practice. 2002;8(3):303–11. doi: 10.1046/j.1365-2753.2002.00350.x. [DOI] [PubMed] [Google Scholar]