Abstract
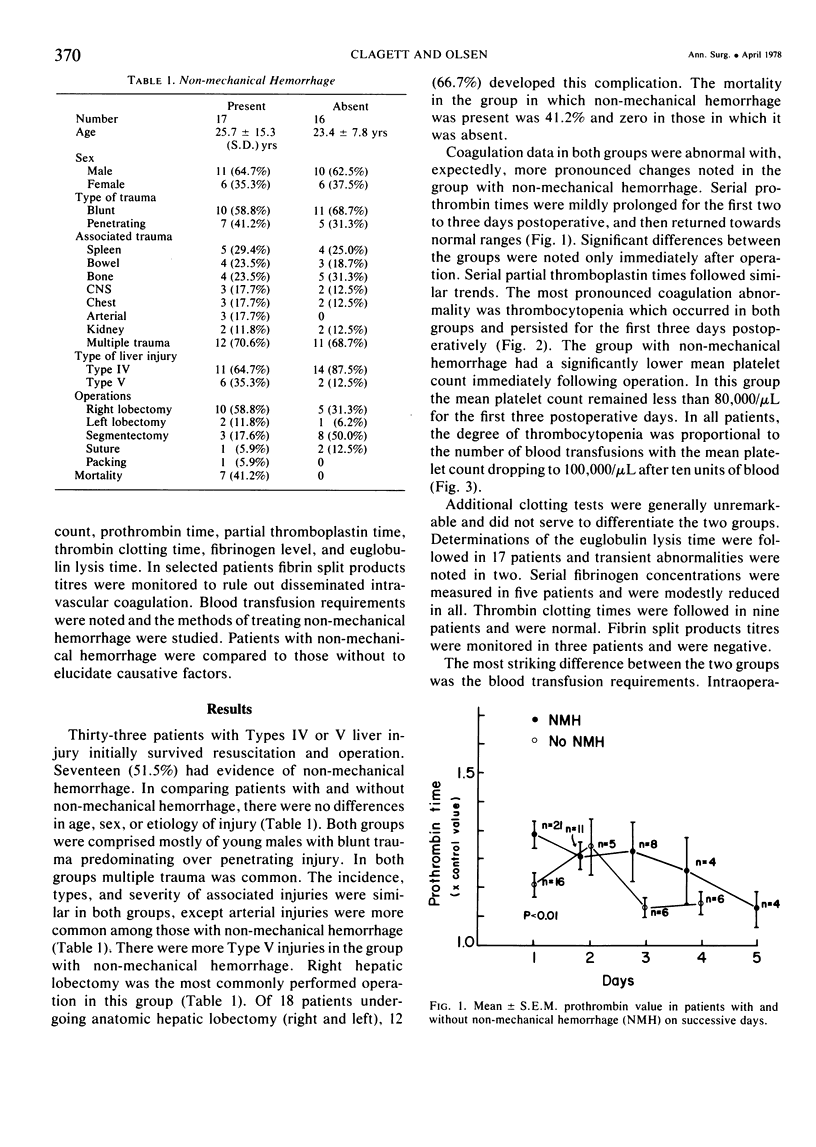
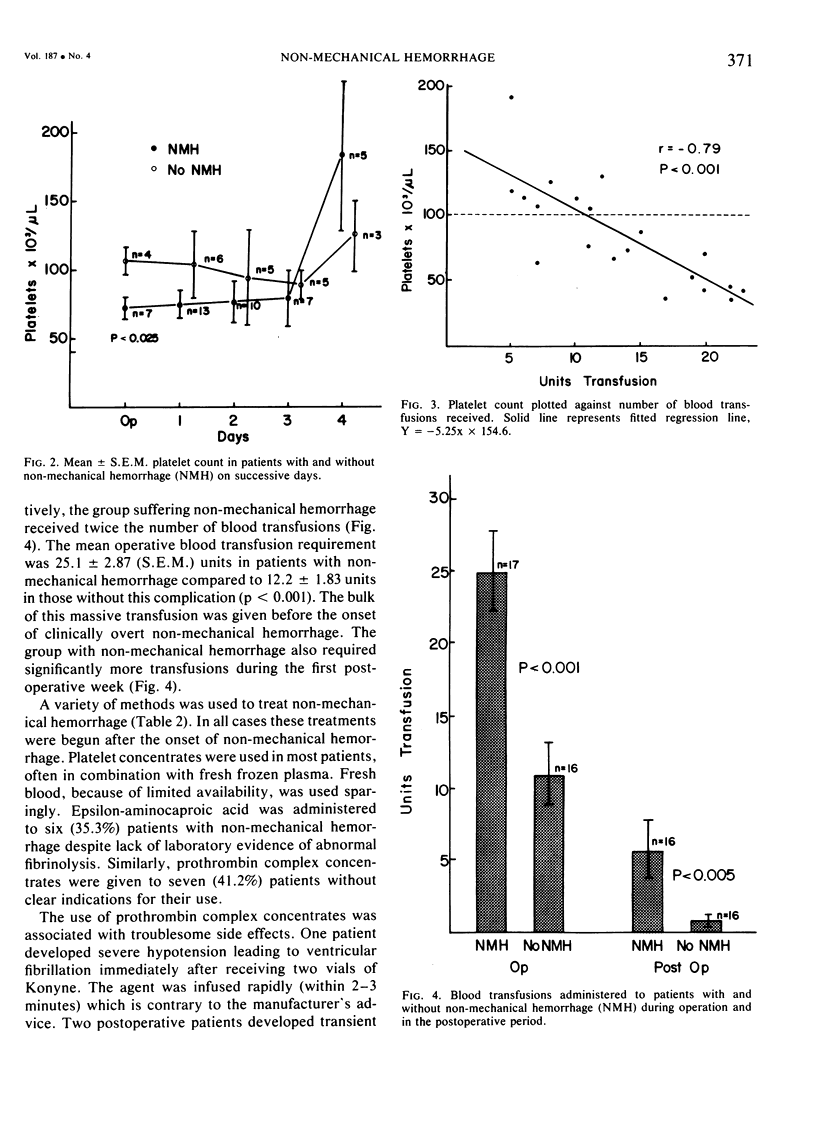
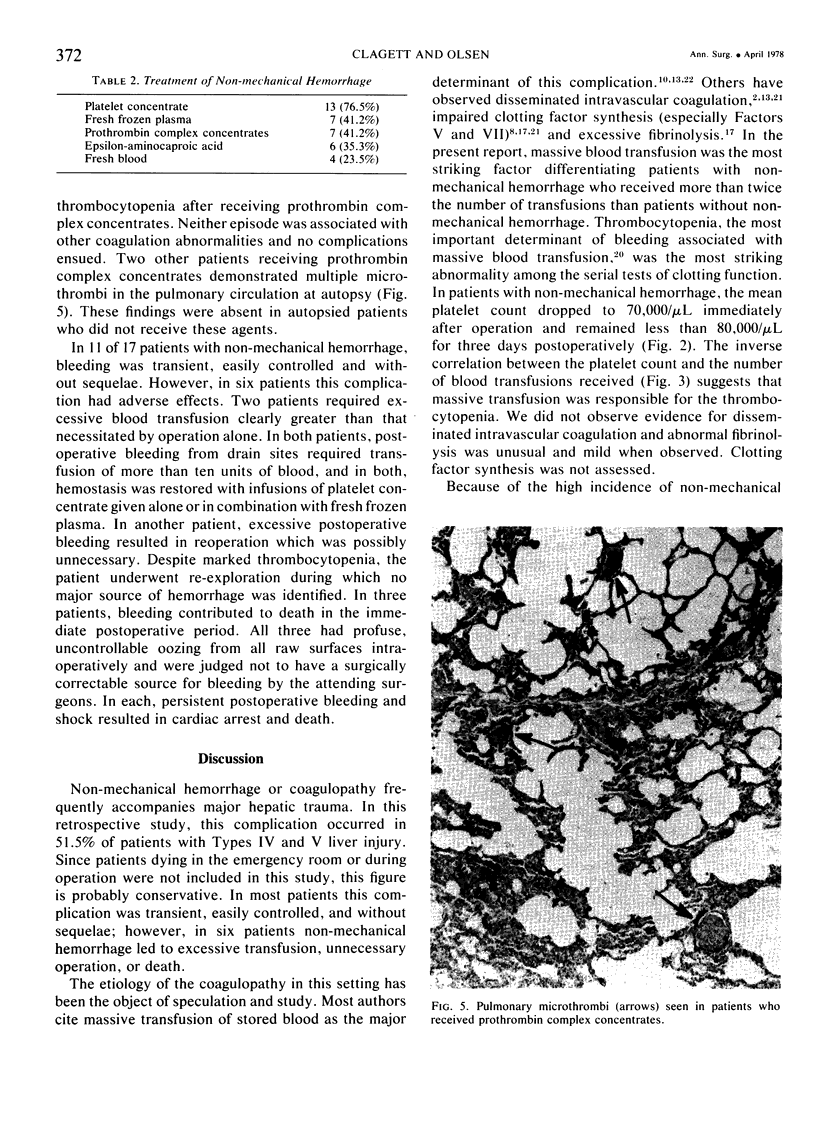
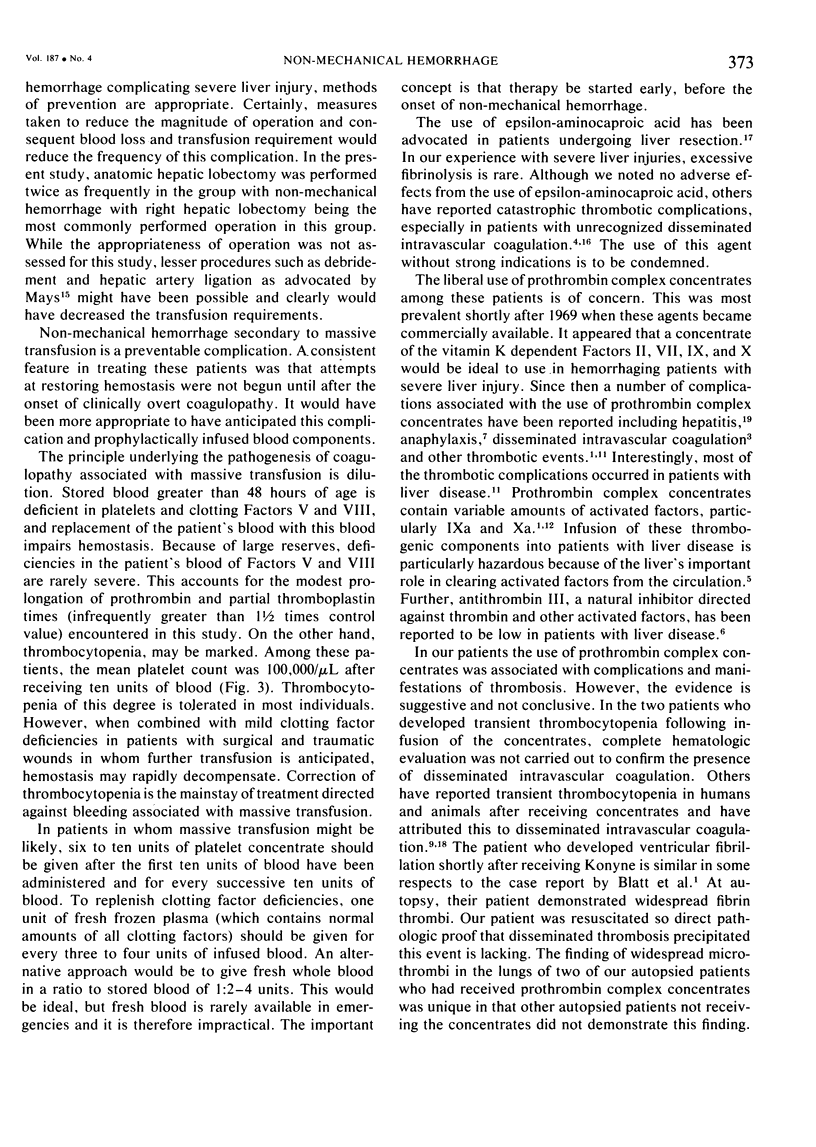
Coagulopathy, or non-mechanical hemorrhage, complicated the operative course of 17 of 33 (51.5%) patients suffering severe liver trauma. The highest incidence of non-mechanical hemorrhage (66.7%) occurred in patients undergoing anatomic lobectomy. Serial hemostatic parameters were assessed and thrombocytopenia was the most striking abnormality in patients with non-mechanical hemorrhage. The degree of thrombocytopenia was directly correlated with the number of blood transfusions administered. The mean operative blood transfusion requirement was significantly greater in patients with non-mechanical hemorrhage, 25.1 ± 2.87 (S.E.M.) units, than in those without, 12.2 ± 1.83 units (p < 0.001). The bulk of this transfusion was given before the onset of clinically overt coagulopathy. Massive transfusion of stored blood was felt to be the most important factor in causing non-mechanical hemorrhage. Convincing evidence for disseminated intravascular coagulation was lacking, and abnormal fibrinolysis was infrequent and mild when observed. Although uneventful in most, in six patients non-mechanical hemorrhage resulted in excessive blood transfusion, unnecessary operation or death. Infusions of platelet concentrate, fresh frozen plasma, and fresh blood were used to successfully treat most cases of non-mechanical hemorrhage. In all cases, these components were not started until non-mechanical hemorrhage was clinically apparent. The value of prophylactic use of blood components is stressed. Because of troublesome side effects associated with the use of prothrombin complex concentrates, these agents are contraindicated in patients with severe liver injury. After receiving concentrates, one patient developed severe hypotension leading to ventricular fibrillation, two developed transient thrombocytopenia and two others demonstrated multiple pulmonary microthrombi at autopsy, a finding not observed in autopsied patients not receiving the concentrates.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blatt P. M., Lundblad R. L., Kingdon H. S., McLean G., Roberts H. R. Thrombogenic materials in prothrombin complex concentrates. Ann Intern Med. 1974 Dec;81(6):766–770. doi: 10.7326/0003-4819-81-6-766. [DOI] [PubMed] [Google Scholar]
- Blumgart L. H., Vajrabukka T. Injuries to the liver: analysis of 20 cases. Br Med J. 1972 Jan 15;1(5793):158–164. doi: 10.1136/bmj.1.5793.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cederbaum A. I., Blatt P. M., Roberts H. R. Intravascular coagulation with use of human prothrombin complex concentrates. Ann Intern Med. 1976 Jun;84(6):683–687. doi: 10.7326/0003-4819-84-6-683. [DOI] [PubMed] [Google Scholar]
- Charytan C., Purtilo D. Glomerular capillary thrombosis and acute renal failure after epsilon-amino caproic acid therapy. N Engl J Med. 1969 May 15;280(20):1102–1104. doi: 10.1056/NEJM196905152802006. [DOI] [PubMed] [Google Scholar]
- Deykin D., Cochios F., DeCamp G., Lopez A. Hepatic removal of activated factor X by the perfused rabbit liver. Am J Physiol. 1968 Feb;214(2):414–419. doi: 10.1152/ajplegacy.1968.214.2.414. [DOI] [PubMed] [Google Scholar]
- Duckert F. Behaviour of antithrombin 3 in liver disease. Scand J Gastroenterol Suppl. 1973;19:109–112. [PubMed] [Google Scholar]
- Edell S. Anaphylaxis after Konyne. N Engl J Med. 1971 Sep 2;285(10):580–580. doi: 10.1056/nejm197109022851015. [DOI] [PubMed] [Google Scholar]
- Furnival C. M., Mackenzie R. J., MacDonald G. A., Blumgart L. H. The mechanism of impaired coagulation after partial hepatectomy in the dog. Surg Gynecol Obstet. 1976 Jul;143(1):81–86. [PubMed] [Google Scholar]
- Hedner U., Nilsson I. M., Bergentz S. E. Various prothrombin complex concentrates and their effect on coagulation and fibrinolysis in vivo. Thromb Haemost. 1976 Apr 30;35(2):386–395. [PubMed] [Google Scholar]
- Heslop J. H. Complications of liver resection for trauma. Aust N Z J Surg. 1974 Nov;44(4):329–335. doi: 10.1111/j.1445-2197.1974.tb03898.x. [DOI] [PubMed] [Google Scholar]
- Kasper C. K. Thromboembolic complications. Thromb Diath Haemorrh. 1975 Jun 30;33(3):640–644. [PubMed] [Google Scholar]
- Kingdon H. S., Lundblad R. L., Veltkamp J. J., Aronson D. L. Potentially thrombogenic materials in factor IX concentrates. Thromb Diath Haemorrh. 1975 Jun 30;33(3):617–631. [PubMed] [Google Scholar]
- Lucas C. E., Ledgerwood A. M. Prospective evaluation of hemostatic techniques for liver injuries. J Trauma. 1976 Jun;16(6):442–451. doi: 10.1097/00005373-197606000-00003. [DOI] [PubMed] [Google Scholar]
- Lucas C. E., Walt A. J. Critical decisions in liver trauma. Experience based on 604 cases. Arch Surg. 1970 Aug;101(2):277–283. doi: 10.1001/archsurg.1970.01340260181027. [DOI] [PubMed] [Google Scholar]
- NAEYE R. L. Thrombotic state after a hemorrhagic diathesis, a possible complication of therapy with epsilon-aminocapproic acid. Blood. 1962 Jun;19:694–701. [PubMed] [Google Scholar]
- Niléhn J. E., Nilsson I. M., Aronsen K. F., Ericsson B. Studies on blood clotting factors in man after massive liver resection. Acta Chir Scand. 1967;133(3):189–195. [PubMed] [Google Scholar]
- Preston F. E., Winfield D. A., Malia R. G., Blackburn E. K. Serial changes in the coagulation system following clotting factor concentrate infusion. Thromb Diath Haemorrh. 1975 Nov 15;34(2):475–482. [PubMed] [Google Scholar]
- Roberts H. R., Blatt P. M. Post-transfusion hepatits following the use of prothrombin complex concentrates. Thromb Diath Haemorrh. 1975 Jun 30;33(3):610–616. [PubMed] [Google Scholar]
- Vajrabukka T., Bloom A. L., Sussmann M., Wood C. B., Blumgart L. H. Postoperative problems and management after hepatic resection for blunt injury to the liver. Br J Surg. 1975 Mar;62(3):189–200. doi: 10.1002/bjs.1800620306. [DOI] [PubMed] [Google Scholar]
- Walt A. J. The surgical management of hepatic trauma and its complications. Ann R Coll Surg Engl. 1969 Dec;45(6):319–339. [PMC free article] [PubMed] [Google Scholar]



