Abstract
A mass-screening protocol for the diagnosis of anthrax from nasal swabs based on an enrichment step in liquid medium was devised. Incubation for growth was performed in autoclavable vials and racks which allow real-time PCR analysis of sterilized cultures. A dual-color PCR was set up with primers and probes for the chromosomal marker rpoB and the plasmid marker lef. Specific primer and probe sets were designed for the differentiation of Bacillus anthracis from B. cereus and for the differentiation of the Sterne vaccine strain from field isolates and the Ames strain, which was used in the recent anthrax bioterrorist attack. The present protocol thus combines the high specificity and sensitivity of real-time PCR with excellent biosafety and the low hands-on time necessary for the processing of large numbers of samples, which is extremely important during control programs involving the processing of large numbers of samples.
According to international (Centers for Disease Control and Prevention [CDC]) (6, 13, 24) and national (Istituto Superiore di Sanità [ISS], Rome, Italy) (5, 10) guidelines, microbiological diagnosis of anthrax is organized at several levels. Level A, routine laboratory diagnosis, should focus on exclusion of infection with Bacillus anthracis. When isolation of B. anthracis is suspected, the samples should be forwarded to higher-level regional or national reference laboratories, which will eventually confirm the diagnosis. This routine procedure faces a number of challenges in nonordinary situations such as those encountered in the recent letter-based attacks (12). During this period many institutions or subjects in most developed countries, including Italy, have received letters suspected of containing anthrax spores. In all cases the collection of nasal swabs was recommended, in combination with preventive antibiotic therapy, for epidemiological control of all possible contact exposure (see the anthrax-related web pages of CDC) (6, 10, 13, 24). This meant that huge numbers of swabs were delivered to the local diagnostic laboratories in a single working day, a situation which resulted in great logistic problems due to the large numbers of plates potentially growing B. anthracis. In particular, this situation raised biosafety concerns, especially for smaller or local (first- and second-level) laboratories where no biosafety level III facilities were available.
Detection of B. anthracis is required for different types of samples and situations including (i) species identification of colonies grown on plates in level A laboratories and suspected of being B. anthracis due to basic laboratory tests, (ii) detection and identification of vegetative cells from patients with clinically active cases of anthrax (pulmonary, cutaneous, or gastrointestinal), (iii) detection of spores in environmental samples (powdery substances, contaminated instrumentation, etc.), and (iv) detection of spores in nasal swabs during active surveillance programs. While the sensitivity of molecular detection may be sufficient for the first three examples, due to the large cell contents in the samples, in the case of spore detection in nasal swabs, direct application of molecular methods may not guarantee sufficient sensitivity.
The present report addresses this issue through the design and investigation of a reliable and simple diagnostic protocol for the detection of low numbers of B. anthracis spores in nasal swabs. This protocol meets three diagnostic priorities: (i) biosafety, (ii) ease of performance, and (iii) speed of completion of the diagnostic process. Due to biosafety problems concerning the production of anthrax spores, some of the experiments reported in this paper were carried out with B. cereus spores, taking advantage of the fact that B. anthracis appears to be genetically indistinguishable from members of the B. cereus-B. thuringiensis group (9).
MATERIALS AND METHODS
Bacterial strains.
The bacterial strains and plasmids used in this study are reported in Table 1. B. cereus and B. anthracis ΔSterne and Carbosap were grown in biosafety level II facilities, while B. anthracis strain Ferrara was grown in the biosafety level III facility of the Department of Bacteriology and Medical Mycology, ISS. B. cereus spores were commercially obtained from France, where Bactisubtil (Marion Merrell) is licensed for human use as an antidiarrhea preparation. Selective inactivation of vegetative cells was carried out at 80°C for 20 min (protocol for counting of spores). Any other sample was inactivated by using standard autoclaving cycle conditions, which were 121°C (250°F) and 15 pounds per square inch (psig) (1 bar) for 15 min. B. anthracis Carbosap spores were from the Italian live spore veterinary vaccine in 1% saponin (8). Carbosap spores were washed three times in sterile water and then resuspended in 0.1% Triton and directly used in real-time PCR experiments. To quantify the total number of bacterial cells, spores were spread on tryptic soy agar (Difco, Becton Dickinson and Company) plates and incubated at 37°C for 16 h. A control evaluated by microscopy demonstrated that the fraction of vegetative cells in the washed spore samples was less than 1%. Frozen bacterial stocks prepared from exponentially growing cells were used to inoculate liquid cultures.
TABLE 1.
Strains and plasmids used in the study
| Species or plasmid | Designationa | Comment | Source | Reference |
|---|---|---|---|---|
| B. anthracis | ΔSterne (pX01−, pX02−) | Plasmid-free derivative of vaccine strain Sterne | Patricia Worsham, USAMRIIDb, Ft. Detrick, Md. | 11 |
| B. anthracis | Carbosap (pX01+, pX02+) | Italian live spore vaccine | Laboratory of Veterinary Medicine, ISS | 2 |
| B. anthracis | Ferrara (pX01+, pX02+) | Pathogenic strain, Italian field isolate | Laboratory of Veterinary Medicine, ISS | 2 |
| B. cereus | ATCC 14893 or IP5832 | Bactisubtil; Marion Merrell | Jean Pierre Claverys, Toulouse, France | |
| B. cereus | BGSC6A2 or T-HT | Ezio Ricca, University of Naples, Naples, Italy | 25 | |
| B. circulans | CS-1 | Italian field isolate | Laboratory of Bacteriology and Medical Mycology, ISS | |
| B. subtilis | BGSC1A747 or PY79 | Prototroph | Ezio Ricca, University of Naples | 26 |
| B. anthracis plasmid | pGEX-2TK derivative | lef gene-carrying strain of strain Sterne | Cesare Montecucco, University of Padua, Padua, Italy | 22 |
The minus and plus signs with plasmid designations indicate the absence and presence of the indicated plasmid, respectively.
USAMRIID, U.S. Army Medical Research Institute for Infectious Diseases.
Microbiological work in biosafety level III facility.
Pathogenic B. anthracis strain Ferrara (Laboratory of Veterinary Medicine, ISS) was grown on tryptic soy agar plates at 37°C for 16 h. A sterile toothpick was used to transfer a portion of a fresh colony into 170 μl of 20 mM Tris-HCl-2 mM EDTA-1% Triton (pH 8.0) containing 0.2 mg of lysostaphin (Sigma Chemical Co., St. Louis, Mo.) per ml. The cell suspension was incubated at 37°C for 1 h. DNA was extracted from the cell suspension with a NucleoSpin Tissue kit (Macherey-Nagel).
Materials for cultivation of swab specimens.
The swabs used to collect nasal samples were standard cotton swabs routinely used for throat culture, but no transport medium was used. Nalgene vials (2.0-ml bulk-packed sterile cryogenic vials; Nalge Nunc International) or Sarstedt vials (Micro Tube 2.0 ml with skirted base, screw cap assembled, sterile, with writing space and graduations; Sarstedt International, Nümbrecht, Germany) were used for bacterial growth from swabs. Culture media were brain heart infusion (BHI), Mueller-Hinton (MH), and tryptic soy broth (TSB) without glucose (all media were from Difco, Becton Dickinson and Company). The vials were inoculated, incubated, and autoclaved in heat-resistant boxes (Nalgene white polycarbonate CryoBoxes, nine-by-nine array; Nalge Nunc International).
MIC determination.
The MICs of trimethoprim and polymyxin B sulfate were determined (20; E. Eremenko, E. Afanasyev, V. Efremenko, A. Abgaryan, O. Tsygankova, E. Zhdanova, N. Sarkisova, and I. Zharnikova, Fourth Int. Conf. Anthrax, abstr. 22A, 2001) in microtiter plates (International PBI SpA, Milan, Italy). B. anthracis ΔSterne, B. cereus NCTC6A2, B. cereus IP5832, and B. subtilis 1A747 grown to the late exponential phase in MH were diluted; and 100 μl containing 105 cells/ml was distributed in each well of a microtiter plate. Antibiotic concentrations (twofold dilutions) ranged from 1,024 to 1 μg/ml for trimethoprim and from 256 to 0.25 μg/ml for polymyxin B sulfate. The trimethoprim stock solution contained trimethoprim at a concentration of 2,000 μg/ml, and the polymyxin B stock solution contained polymyxin B at a concetration of 400,000 μg/ml. The MIC was determined after 18 h of incubation at 37°C. The three strains belonging to the B. cereus group showed comparable levels of natural resistance, with MICs of >1,024 μg/ml for trimethoprim and 64 μg/ml for polymyxin B, which differed considerably from the MICs (2 μg/ml for both compounds) for the B. subtilis control strain.
Elution of spores from swabs.
Serial dilutions of B. cereus IP5832 spores, resuspended in 10 μl of distilled water, were spotted onto cotton swabs, and equivalent samples were directly plated for CFU enumeration. For determination of spore recovery, dried swabs were streaked onto agar plates or inoculated into liquid medium (both of which contained BHI). After incubation overnight at 37°C, the readout was the numbers of CFU for agar plates and the detection of turbidity for the liquid cultures.
Spore germination.
The loss of heat resistance was considered an indicator of spore germination and outgrowth. B. cereus IP5832 spores were inoculated (5,000 CFU/ml) into BHI medium at room temperature. Vials inoculated in parallel were subjected to heat inactivation at the following time intervals: time zero, 30 s, and 1, 2, 3, 10, and 30 min. After heat inactivation (water bath at 80°C for 15 min) the samples were plated for CFU determination.
Growth curve and lysis.
The growth curve for B. anthracis ΔSterne in liquid medium was constructed in 15-ml plastic tubes allowing direct optical density (OD) measurement. The OD (at 590 nm) was measured hourly in a spectrophotometer (Spectronic 20D; Milton Roy and Company). Cultures were incubated (i) at 37°C, (ii) at 30°C, (iii) in a vertical position, or (iv) horizontally on a shaker. The extent of autolysis was assayed by plating appropriate dilutions on BHI agar. The numbers of CFU were determined after incubation overnight.
Clinical samples.
In November 2001 different institutions in the province of Siena (Toscana, Italy) received letters suspected of containing anthrax spores. Such events occurred in most regions in Italy. Suspected material was submitted to the national reference laboratory (Istituto Zooprofilattico Sperimentale di Foggia) according to institutional guidelines (Ministero della Salute protocol 400.3/120.33/4786) (10). During this period local health authorities took 145 nasal swab specimens for control of anthrax contacts. On a daily basis, up to 60 samples (nasal swabs without transport medium) reached the Microbiology Unit of the University Hospital of Siena for 11 working days. Sampling by health authorities stopped when no positive results were detected.
Real-time PCR.
Several genetic markers are available for B. anthracis detection, including chromosomal and plasmid-based sequences (8, 17, 18). In the present study we choose a primer-probe set based on the lef gene (lethal factor gene carried by plasmid pX01) (18) for the detection of B. anthracis. For differentiation of B. cereus (used as a control) from B. anthracis, a primer-probe set based on the rpoB gene (the gene for the beta subunit of RNA polymerase) was designed (17). A further primer-probe set was designed on the basis of a single nucleotide polymorphism (SNP) differentiating the B. anthracis vaccine strain Sterne, used as the PCR control for lef, from other anthrax isolates sequenced (1, 19). The primers and probes are listed in Table 2.
TABLE 2.
Primers and probes used in real-time PCR
| Name | Target | Usea | Sequence (5′-3′) | GenBank accession no. | Position | Tm (°C) |
|---|---|---|---|---|---|---|
| OG132 | lef | Primer | TTTTTATGACAAGAAATATTGCCTTT | M29081 | 372-397 | 58.0 |
| OG133 | lef | Primer | CAGCTTCCTCCCCTTTTACTTC | M29081 | 718-739 | 62.0 |
| OG134 | lef | Probe Red 705 | TGTACAGGGGGCGGGCGGTC | M29081 | 544-561 | 72.8 |
| OG135 | lef | Probe FL | TTGAGTGGTCCCGTCTTTATCCCCC | M29081 | 570-589 | 69.3 |
| OG136 | rpoB | Primer | TTGCTTGAAATTTATGAGCGTCTAC | AF205323 | 285-309 | 61.5 |
| OG137 | rpoB | Primer | ATTGTTCCTTCTGCCGCTAAAA | AF205323 | 493-514 | 62.2 |
| OG138 | rpoB | Probe Red 640 | TGTAGGTCGCTACAAGATCAACAAG | AF205323 | 395-419 | 64.0 |
| OG140 | rpoB | Probe FL | AAGCGCTATGATTTAGCAA | AF205323 | 375-393 | 56.2 |
| OG144 | lefC | Primer | TATGTCATCTTTCTTTGGCTCAATAG | AJ413935 | 936-911 | 60.7 |
| FM22 | lefC | Primer | TTTATGCACCGGAAGCTTTTAA | AJ413935 | 719-740 | 60.2 |
| FM23 | lefC | Probe FL | CAACGGATGCTGTCAAGATATG | AJ413935 | 799-820 | 60.8 |
| FM24 | lefC | Probe Red 640 | AAATGGGAAAAGATAAAACAGCACTATCA | AJ413935 | 823-851 | 63.4 |
Probe Red 705, downstream probe marked with reporter dye Red 705; probe FL, upstream probe labeled with fluorescein; probe Red 640, downstream probe marked with reporter dye Red 640.
Hybridization probes (16) were designed (Table 2) for the detection of B. anthracis by real-time PCR. The real-time PCR mixture contained 1 μl of the DNA template sample, 1 μl (10 pmol) of primers, 2 μl (2 pmol) of probes FL and LC, 2.5 μl of MgCl2 (final concentration, 4 mM), 2 μl of the Master Hybridization Probes reaction mixture (Roche), and PCR-grade sterile water to a final volume of 20 μl. Up to 32 samples were run in parallel by performing an initial 30-s denaturation step at 95°C followed by 40 cycles of repeated denaturation (0 s at 95°C), annealing (10 s at 57°C), and polymerization (10 s at 72°C). The temperature transition rates were 20°C/s in the denaturation and annealing steps and 5°C/s in the polymerization step. In the final cycle the melting curves for the samples were determined by initially heating the mixture to 95°C, cooling it to 45°C, and subsequent controlled heating to 95°C with a temperature transition rate of 0.1°C/s. The two probes for lef and rpoB were used in a dual-color multiplex PCR and were labeled with Red705 and Red640, respectively, which are detected in different fluorescence channels of the LightCycler instrument (16). Since the size of the probe was reduced compared with the size of the probe of Qi and coworkers (17), the fluorescence derived from the rpoB probe is not detectable during the annealing steps of the real-time amplification but is detectable only during the melting curve analysis.
Theoretical determination of Tms.
The melting temperatures (Tms) of the probes and the differences in the Tms of the probes complementary to sequences showing point mutations were calculated by using Module 3 of the HYTHER program (http://ozone.chem.wayne.edu/) (4). Parameters set as hybridization conditions were a monovalent cation concentration of 0.05 mol/liter, an Mg2+ concentration of 0.004 mol/liter, a concentration of probe and target of 10−7 mol/liter, and a hybridization temperature of 37°C.
RESULTS
A mass-screening protocol for the diagnosis of anthrax from nasal swabs was devised. The protocol relies on an enrichment step in liquid medium which permits the direct molecular detection of bacilli without any purification step.
Real-time PCR.
A dual-color PCR was set up by using primers and probes for the chromosomal marker rpoB and the plasmid marker lef. Positivity was based on detection of red fluorescence of the lef probe during real-time PCR (Fig. 1A). Efficient probe hybridization was accomplished, since the Tms of the lef probes were more than 10°C higher than the primer annealing temperature (Table 2). As a positive control, purified chromosomal DNA of B. cereus mixed with a cloned lef gene (Sterne strain), harbored on an Escherichia coli plasmid, was used. Use of this control was preferred over use of B. anthracis DNA for easy distinction of possible contamination from a positive culture. Design of hybridization probes based on SNPs specific for the control DNA (see below) was chosen to permit detection of any possible contamination.
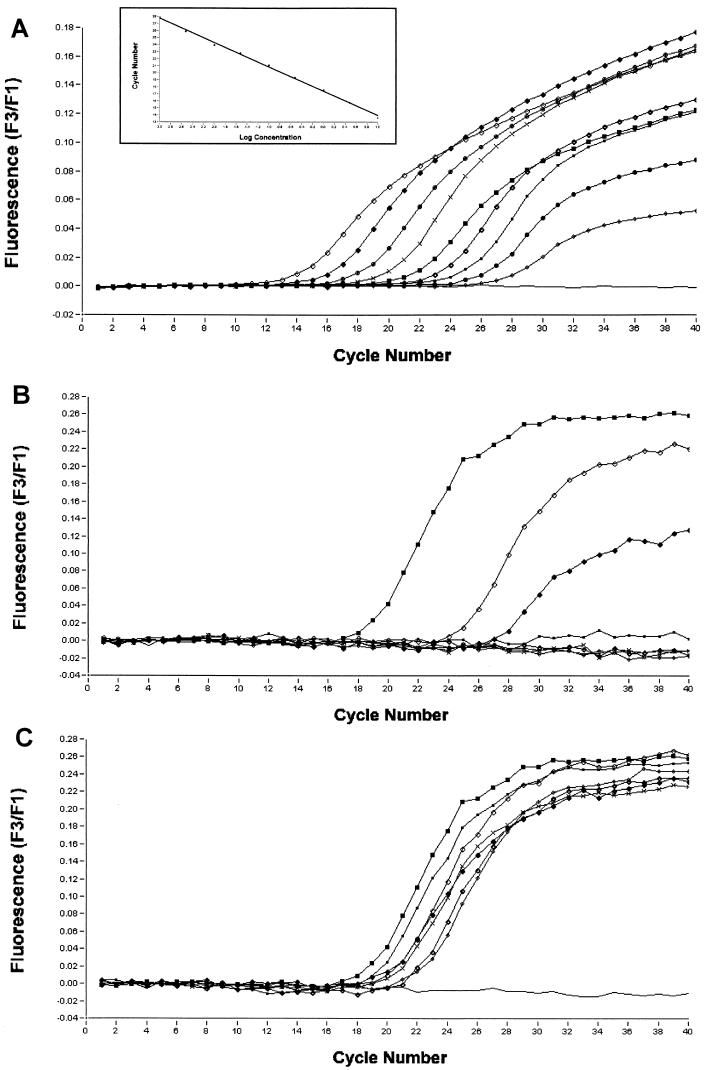
FIG. 1.
Quantitative analysis of fluorescence signal during real-time PCR with the lef primer-probe set and serial dilutions of the target. (A) Amplification of serial dilutions of purified B. anthracis Carbosap DNA. Dilutions of DNA ranged from 3 to 0.0003 ng. ◊, 3 ng; ⧫, 1 ng; ○, 0.3 ng; ×, 0.1 ng; ▪, 0.03 ng; small ⋄, 0.01 ng; ▪, 0.003 ng; •, 0.001 ng; smaller ⋄, 0.0003 ng; line at the bottom, negative control (no DNA). (B) Amplification of serial dilutions of nonlysed B. anthracis Carbosap spores. Dilutions ranged from 20,000 to 2 spores. ◊, 20,000 spores; ⧫, 2,000 spores; ▪, 200 spores; ×, 20 spores; small ◊, 2 spores; ▪, positive control (1 ng of B. anthracis Carbosap DNA; line, negative control (no DNA). (C) Amplification of stationary-phase cultures inoculated with serial dilutions of B. anthracis Carbosap spores. Dilutions of inocula ranged from 30,000 to 3 spores. ◊, 30,000 spores; ⧫, 3,000 spores; ▪, 300 spores; ×, 30 spores; small ◊, 3 spores; ▪, positive control (1 ng of B. anthracis Carbosap DNA); line at the bottom, negative control (no DNA). The inset in panel A refers to the standard curve of the amplification reactions on serial dilutions reported in panel A (the regression coefficient is 1, as calculated with LightCycler software [version 3.0]).
Sensitivity of real-time PCR.
After the amplification conditions were established, real-time PCR was performed with (i) purified DNA, (ii) B. anthracis spores, and (iii) stationary-phase cultures of spore-containing samples. Positive amplification results were obtained for all samples with the lef primer-probe set, including nonlysed spores (Fig. 1). The main difference in the results was detected in assays with serial dilutions of the various templates. When purified DNA (3 to 0.0003 ng) was used, the detection limit was found to be about 50 genome equivalents (Fig. 1A), with an exceptional linearity of the experimental outcome, as shown by the standard curve (inset in Fig. 1A). The detection limit fell by 2 logarithms to about 2,000 cell equivalents when spores were directly used as the template for PCR (Fig. 1B). In the case of amplification with 1 μl of a bacterial stationary-phase culture as the DNA template, positivity was detected irrespective of the initial inoculum size (3 to 30,000 spores) (Fig. 1C).
Differentiation of B. anthracis from B. cereus.
Control amplification of the chromosomal rpoB gene and species identification were accomplished by performing a melting curve analysis at the end of the real-time PCR amplification. Amplification primers were designed on the basis of the sequences common to Bacillus species of the B. cereus group. The distinction between B. anthracis and B. cereus was based on the published species-specific SNP in the rpoB gene (17). The change of a single nucleotide in the sequence complementary to the fluorescent probe results in a theoretical difference in the Tms between B. anthracis and B. cereus of 3.6°C. Experimentally, this difference in Tms was found to be 3.5°C (Fig. 2A; Table 2). No hybridization of the rpoB probe to the DNA of other bacilli such as B. subtilis and B. circulans or to E. coli and human DNA templates was observed (Fig. 2A).
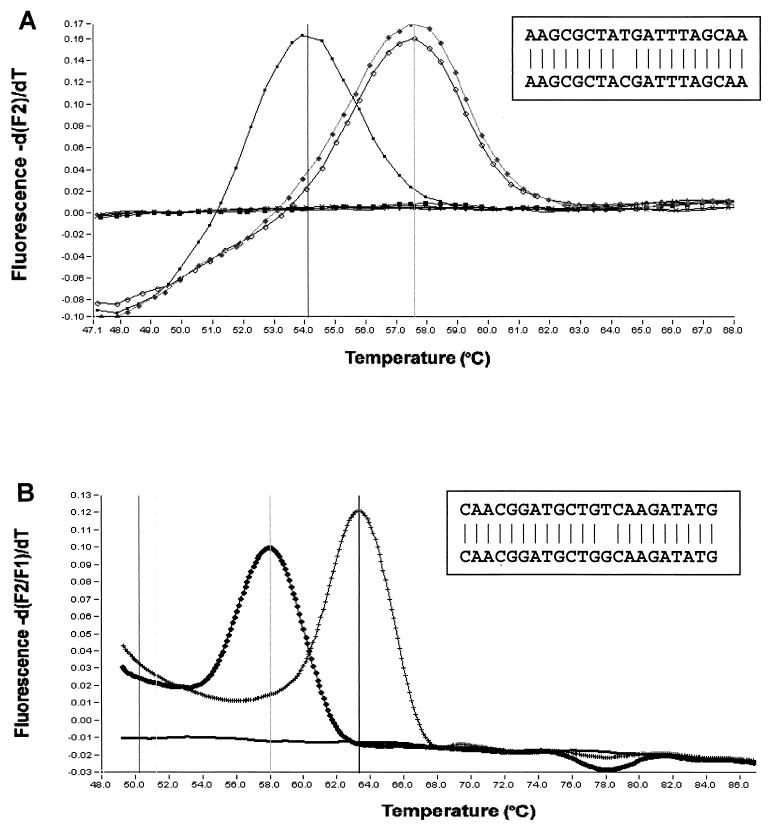
FIG. 2.
Qualitative detection of SNPs exploiting changes in Tms during melting curve analysis. (A) The SNP in which the rpoB-specific FL probe target of B. anthracis differs from that of B. cereus (17) is efficiently detected due to a Tm difference of 3.5°C. No amplicon is detected for B. circulans, B. subtilis, E. coli, and human DNA. ▪, B. cereus; ⧫, B. anthracis Carbosap; ◊, B. anthracis Ferrara. The sequence of the probe that annealed to the SNP containing the target (the B. cereus rpoB gene) is shown in the box. (B) The SNP distinguishing the Sterne strain from the Italian strains is efficiently detected by the lefC-specific FL probe (Table 2) since it determines a Tm difference of 5.2°C. ×, lef gene of Sterne strain (cloned gene; Table 2); ⧫, B. anthracis Ferrara lef gene (whole chromosomal DNA). The sequence of the probe that annealed to the SNP containing the target (lef genes of Italian isolates Ferrara and Carbosap and of the Florida strain) is boxed.
Differentiation of Sterne strain from other isolates.
In order to distinguish the vaccine strain and/or the control DNA from a strain used as a biological weapon, a probe designated lefC (Table 2) was designed on the basis of an SNP that distinguishes the lef gene of the Sterne strain (GenBank accession numbers M29081, M30210, and AF065404) from the recently deposited sequences of an Italian field isolate (GenBank accession number AJ413934), the Italian attenuated vaccine strain (GenBank accession number AJ413935) (1), and the Florida isolate (the Ames-derived strain of the letter-based attack in Florida in 2001; GenBank accession number AE011190) (19). As for rpoB, the result of this PCR was also determined by melting curve analysis. The theoretical difference in Tms of 6.3°C was found to be 5.2°C, which easily permitted the distinction of the field isolates from the Sterne vaccine strain used as a control (Fig. 2B).
Bacteriological parameters for enrichment in liquid.
Nasal swabs for epidemiological control of anthrax contacts may contain only a few spores, which are inadequate for molecular detection because of the small amount of genetic material. Since real-time PCR has a detection limit of 2,000 spores/sample and swabs would be eluted in at least 300 μl of liquid, this would bring the detection limit of direct real-time PCR with swabs to 600,000 spores/swab when 1 μl of the eluted spore suspension is used. After overnight growth, liquid cultures obtained from swabs spotted with serial dilutions of spores reached the stationary phase, irrespective of the number of spores carried by the swab (the minimal inoculum tested was 5 spores/swab). In the case of stationary-phase cultures of vegetative cells, the number of microorganisms present per microliter was sufficient to guarantee the reproducibility of amplification, irrespective of the inoculum size (Fig. 1C). Since liquid culture is the method of choice for the present standard protocol, parameters for B. anthracis growth were checked. All experiments regarding growth media, autolysis, and sporulation were performed with B. anthracis ΔSterne.
Different media and growth conditions were assayed to identify parameters which would ensure the reproducibility of the system. The bacteria were grown in TSB or BHI at 30 or 37°C, with or without aeration of the medium. No significant difference was seen when the bacteria were grown in different media or at different temperatures, while aeration of the medium significantly influenced the doubling times of the bacteria (data not shown).
In order to confirm sample quality, bacteria were plated to control viability with the attempt to rule out massive autolysis, which could determine the release of DNases from cells. The counts reported in Table 3 indicate that there is autolysis of B. anthracis cells, with the viable count decreasing 2 to 3 logarithms in samples grown in the shaker.
TABLE 3.
Autolysis in overnight liquid cultures of B. anthracis
| Growth conditions | No. of CFU
|
% Survival | |
|---|---|---|---|
| In early stationary phase | After overnight growth | ||
| BHI, 37°C, shakera | 1.7 × 108 | 2.0 × 106 | 1 |
| BHI, 37°C | 5.8 × 107 | 1.2 × 107 | 20 |
| BHI, 30°C, shaker | 8.1 × 107 | 7.0 × 105 | 0.8 |
| BHI, 30°C | 5.0 × 107 | 3.7 × 107 | 74 |
| TSB, 37°C, shaker | 1.9 × 108 | 5.0 × 106 | 2 |
| TSB, 37°C | 5.6 × 107 | 1.4 × 107 | 25 |
| TSB, 30°C, shaker | 1.5 × 108 | 3.3 × 106 | 2.2 |
| TSB, 30°C | 3.0 × 107 | 2.2 × 107 | 73 |
Shaker, growth with aeration.
To exclude significant sporulation during overnight growth, CFU were enumerated after exposure to 95°C for 20 min. In some samples heat-resistant forms could be recovered, but the counts for the spores detected did not exceed 30 CFU/ml, regardless of the type of culture condition used. A viability check of autoclaved cultures never yielded any colonies (standard autoclave cycle conditions were used).
The prime method for decontamination of spore-containing samples of other bacteria is heat inactivation, which effectively kills vegetative cells. The standard condition of spore heating at 80°C for 20 min was used, as it is also recommended for induction of germination of bacterial spores. The main problem encountered was due to the prompt germination of Bacillus spores in medium prior to heat inactivation. We observed the germination of 70% of B. cereus IP5832 spores in 3 min and the germination of over 99% of spores after 10 min in liquid medium at room temperature.
Protocol for direct identification of B. anthracis spores from nasal swabs.
On the basis of our experience and previously described findings, the following experimental procedure was set up: (i) spores are released from swabs by suspension in autoclavable vials (1.5- to 2-ml vials with O rings positioned in an autoclavable rack) with 300 μl of TSB containing 100 μg of trimethoprim per ml and 15 μg of polymyxin B sulfate per ml; (ii) the spore suspension is incubated at 37°C overnight without shaking; (iii) vials are autoclaved in a box without prior opening; and (iv) 1 μl of the autoclaved culture is used in 19 μl of the real-time PCR mixture (standard autoclave cycle conditions are used). We recommend that the original swab be discarded only after the real-time PCR result is available to allow the recovery of the bacterial strain for further confirmation and analysis in case of positive PCR results. By this protocol, a single operator analyzed 145 nasal swabs in 11 working days, with a maximum of 60 samples analyzed per day. All clinical samples turned out to be negative for B. anthracis. Positive controls containing B. cereus DNA and a cloned lef gene were consistently detected (data not shown). Due to the small amount of hands-on time required, all diagnostic reports were given within 24 h.
DISCUSSION
Various rapid tests for the detection of B. anthracis by real-time PCR are available in the scientific literature and commercially. These include the Laboratory Response Network assays, The Mayo Clinic/Roche Rapid Anthrax test, and the assay of Idaho Technology (http://www.bt.cdc.gov/) (3, 5, 7, 8, 14, 15, 17, 18, 21; M. M. Vaillancourt, M. Boissinot, F. J. Picard, D. E. Bader, E. Leblanc, and M. G. Bergeron, Abstr. 101st Gen. Meet. Am Soc. Microbiol., abstr. C-34, 2001). The central feature common to all these tests is well described by a sentence from the CDC web page, which states that “the results are only as good as the method used to prepare the sample for analysis.” This fact is especially pertinent in the case of tests which start from nasal swabs for epidemiological control of spore contacts. The present work is thus intended as a proposal for a protocol for molecular detection of B. anthracis spores after enrichment of the clinical sample under stringent biosafety conditions. Due to the small amount of hands-on time required for this protocol, the protocol enables local diagnostic facilities to efficiently analyze large numbers of samples and to contribute to a more rational and widespread control in critical situations, as in the case of bioterrorist attacks.
In any type of molecular protocol for detection of spores in nasal swabs the first step is elution of the spores from the swab into liquid. Even in the case of nearly complete elution, the spores would be diluted into at least 200 to 300 μl of liquid. Because 1 μl is generally the maximal volume of sample to be used for capillary-based PCR and a limit of 200 to 2,000 spores is required, in our hands, for consistent detection, the sensitivity of direct real-time PCR with swabs rises to 60,000 to 600,000 spores/swab, i.e., a sensitivity limit that makes no sense for the purpose of detecting anthrax contacts during attacks with an aerosol. A centrifugation step would increase the detection limit considerably, but it would also increase the risk of aerosol generation considerably. To solve this problem, microbiological parameters of growth in liquid medium were analyzed to permit the use of an enrichment step, which is also recommended by CDC (23) and other (2, 3; Eremenko et al., Fourth Int. Conf. Anthrax, 2001) protocols.
The present work exemplifies (Fig. 1A to C) how a primer-probe set, even if it is able to amplify satisfactorily purified DNA, may be completely unsatisfactory when dealing directly with spore samples, especially when this is coupled to the need for high sensitivity for the detection of spores in the original sample. The execution of an enrichment step in broth efficiently resolves any sensitivity-related problems, as shown in Fig. 1C. The need for an overnight incubation may not be mandatory, since bacteria of the genus Bacillus have quite short doubling times, but an 18-h incubation better adapts the protocol to work schedules in a standard clinical laboratory (samples may arrive late in the morning or even in the afternoon). When an 18-h incubation is considered, the practical advantage of growing bacteria without agitation (avoidance of spills is extremely important for biosafety considerations) is coupled to the fact that these cells tend to have lower degrees of lysis. Even if prevention of autolysis may not be essential, it enhances the sample quality for successive molecular analysis. Data on the promptness with which spores tended to germinate, and thus loose their heat resistance, prompted us to rule out the use of the selective decontamination prior to enrichment used by other protocols (3). In the case of batch decontamination after multiple inoculations, there would have been a concrete risk that heat inactivation would kill B. anthracis cells that had also germinated together with the contaminating flora.
Two sets of primers and probes were designed for the control of positive samples. Both sets, one specific for the sequence on the lef gene of plasmid pX01 (1, 19) and one specific for the sequence on the chromosomal rpoB gene (17), were designed based on SNPs distinguishing the control DNAs from any positive sample. The lefC probe distinguishes the Sterne strain, used in our protocol as a positive control, from wild-type isolates, including the recently sequenced Italian isolate and the Florida isolate (from the 2001 letter-based attack in Florida). The rpoB probe, designed on the basis of the SNP described by Qi et al. (17), distinguished B. cereus, used as a source of control chromosomal DNA, from B. anthracis. The availability of these controls permits a positive and flexible readout specific for a variety of conditions which include amplification of B. anthracis wild-type strains, B. anthracis strain Sterne (veterinary vaccine strain), contaminating control plasmid DNA, and contaminating control chromosomal DNA. The choice to base characterization of the experimental readout on the shift in Tm provides a versatile tool for the positive discrimination of all these DNAs. This flexibility is not present in PCR protocols aimed solely at the detection of B. anthracis (3, 5, 7, 8, 14, 15, 17, 18, 21; Vaillancourt et al., Abstr. 101st Gen. Meet. Am Soc. Microbiol.).
Present guidelines indicate that standard microbiological analysis is the method of choice for analysis of nasal swabs possibly containing anthrax spores. In this context it should not be underestimated that visual inspection and follow-up analysis for control of dozens of plates possibly growing anthrax bacilli are extremely difficult to combine with the routine work of most level A microbiology laboratories. Especially in the case of nonreference laboratories in which the biosafety level is below level III and the workload is an important parameter, a protocol which permits analysis of dozens of samples with a negligible workload is extremely appealing. The present work thus presents an analysis of some basic bacteriological and molecular parameters that can be used in a protocol for exclusion of anthrax contacts with minimal hands-on time. This fact, coupled to the guaranteed biosafety of the procedure, makes the present approach a valuable alternative to plating as a tool for active surveillance in cases of suspected anthrax contamination.
Acknowledgments
We are grateful to Ida Luzzi and Annalisa Pantosti for continuous advice and many helpful suggestions. We also thank Patricia Worsham, Jean Pierre Claverys, Ezio Ricca, Gian Maria Rossolini, Cesare Montecucco, and Franco Ciuchini for provision of strains.
This work was supported in part by grants from the Italian Ministry of Health (AIDS project—Opportunistic Infections and TB [grants 50D23 and 40D74] and National Tubercolosis Project [grant 50D3]).
REFERENCES
- 1.Adone, R., P. Pasquali, G. La Rosa, C. Marianelli, M. Muscillo, A. Fasanella, M. Francia, and F. Ciuchini. 2002. Sequence analysis of the genes encoding for the major virulence factors of Bacillus anthracis vaccine strain "Carbosap." J. Appl. Microbiol. 93:117-121. [DOI] [PubMed] [Google Scholar]
- 2.Beyer, W., P. Glockner, J. Otto, and R. Bohm. 1995. A nested PCR method for the detection of Bacillus anthracis in environmental samples collected from former tannery sites. Microbiol. Res. 150:179-186. [DOI] [PubMed] [Google Scholar]
- 3.Beyer, W., S. Pocivalsek, and R. Bohm. 1999. Polymerase chain reaction-ELISA to detect Bacillus anthracis from soil samples—limitations of present published primers. J. Appl. Microbiol. 87:229-236. [DOI] [PubMed] [Google Scholar]
- 4.Bommarito, S., N. Peyret, and J. SantaLucia, Jr. 2000. Thermodynamic parameters for DNA sequences with dangling ends. Nucleic Acids Res. 28:1929-1934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carattoli, A., A. Ciervo, G. Pozzi, and M. R. Oggioni. 2002. Applicazioni di biologia molecolare nella diagnostica di Bacillus anthracis e altri batteri. Notiz. Ist. Superiore Sanità 15:4-7. [Google Scholar]
- 6.Centers for Disease Control and Prevention. 2001. Interim guidelines for investigation of and response to Bacillus anthracis exposures. Morb. Mortal. Wkly. Rec. 50:987-990. [PubMed] [Google Scholar]
- 7.Cheun, H. I., S. I. Makino, T. Shirahata, I. Uchida, K. Takeshi. 2001. A simple and sensitive detection system for Bacillus anthracis in meat and tissue. J. Appl. Microbiol. 91:421-426. [DOI] [PubMed] [Google Scholar]
- 8.Fasanella, A., S. Losito, T. Trotta, R. Adone, S. Massa, F. Ciuchini, and D. Chiocco. 2001. Detection of anthrax vaccine virulence factors by polymerase chain reaction. Vaccine 19:4214-4218. [DOI] [PubMed] [Google Scholar]
- 9.Helgason, E., O. A. Okstad, D. A. Caugant, H. A. Johansen, A. Fouet, M. Mock, I. Hegna, and A. B. Kolsto. 2000. Bacillus anthracis, Bacillus cereus, and Bacillus thuringiensis: one species on the basis of genetic evidence. Appl. Environ. Microbiol. 66:2627-2630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Istituto Superiore di Sanità. 2001. Protocollo diagnostico per il laboratorio di microbiologia per l'identificazione presuntiva di Bacillus anthracis. Istituto Superiore di Sanità, Rome, Italy.
- 11.Ivins, B. E., J. W. J. Ezzell, J. Jemski, K. W. Hedlund, J. D. Ristroph, and S. H. Leppla. 1986. Immunization studies with attenuated strains of Bacillus anthracis. Infect. Immun. 52:454-458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jernigan, J. A., D. S. Stephens, D. A. Ashford, C. Omenaca, M. S. Topiel, M. Galbraith, M. Tapper, T. L. Fisk, S. Zaki, T. Popovic, R. F. Meyer, C. P. Quinn, S. A. Harper, S. K. Fridkin, J. J. Sejvar, C. W. Shepard, M. McConnell, J. Guarner, W. J. Shieh, J. M. Malecki, J. L. Gerberding, J. M. Hughes, and B. A. Perkins. 2001. Bioterrorism-related inhalational anthrax: the first 10 cases reported in the United States. Emerg. Infect. Dis. 7:933-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kortepeter, M., G. Christopher, T. Cieslak, R. Culpepper, R. Darling, J. Pavlin, J. Rowe, K. J. McKee, and E. Eitzen. 2001. USAMRIID's medical management of biological casualties handbook, 4th ed. U.S. Army Medical Research Institute for Infectious Diseases, Ft. Detrick, Md.
- 14.Lee, M. A., G. Brightwell, D. Leslie, H. Bird, and A. Hamilton. 1999. Fluorescent detection techniques for real time multiplex strand specific detection of Bacillus anthracis using rapid PCR. J. Appl. Microbiol. 87:218-223. [DOI] [PubMed] [Google Scholar]
- 15.Makino, S. I., H. I. Cheun, M. Watarai, I. Uchida, and K. Takeshi. 2001. Detection of anthrax spores from the air by real-time PCR. Lett. Appl. Microbiol. 33:237-240. [DOI] [PubMed] [Google Scholar]
- 16.Meuer, S., C. Wittwer, and K. Nakawara. 2001. Rapid cycle real-time PCR. Methods and applications. Springer-Verlag, Heidelberg, Germany.
- 17.Qi, Y., G. Patra, X. Liang, L. E. Williams, S. Rose, R. J. Redkar, and V. G. Del Vecchio. 2001. Utilization of the rpoB gene as a specific chromosomal marker for real-time PCR detection of Bacillus anthracis. Appl. Environ. Microbiol. 67:3720-3727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ramisse, V., G. Patra, H. Garrigue, J. L. Guesdon, and M. Mock. 1996. Identification and characterization of Bacillus anthracis by multiplex PCR analysis of sequences on plasmids pX01 and pX02 and chromosomal DNA. FEMS Microbiol. Lett. 145:9-16. [DOI] [PubMed] [Google Scholar]
- 19.Read, T. D., S. L. Salzberg, M. Pop, M. Shumway, L. Umayam, L. Jiang, E. Holtzapple, J. D. Busch, K. L. Smith, J. M. Schupp, D. Solomon, P. Keim, and C. M. Fraser. 2002. Comparative genome sequencing for discovery of novel polymorphism in Bacillus anthracis. Science 296:2028-2033. [DOI] [PubMed] [Google Scholar]
- 20.Reva, O. N., V. A. Vyunitskaya, S. R. Reznik, L. A. Kozachko, and V. V. Smirnov. 1995. Antibiotic susceptibility as a taxonomic characteristic of the genus Bacillus. Int. J. Syst. Bacteriol. 45:409-411. [DOI] [PubMed] [Google Scholar]
- 21.Uhl, J. R., C. A. Bell, L. M. Sloan, M. J. Espy, T. F. Smith, J. E. Rosenblatt, and F. R. Cockerill III. 2002. Application of rapid-cycle real-time polymerase chain reaction for the detection of microbial pathogens: the Mayo-Roche Rapid Anthrax Test. Mayo Clin. Proc. 77:673-680. [DOI] [PubMed] [Google Scholar]
- 22.Vitale, G., R. Pellizzari, C. Recchi, G. Napolitani, M. Mock and C. Montecucco. 1998. Anthrax lethal factor cleaves the N-terminus of MAPKKs and induces tyrosine/threonine phosphorylation of MAPKs in cultured macrophages. Biochem. Biophys. Res. Commun. 248:706-711. [DOI] [PubMed] [Google Scholar]
- 23.Weyant, R. S., J. W. J. Ezzell and T. Popovic. 2002. Basic laboratory protocols for presumptive identification of Bacillus anthracis. Centers for Diseases Control and Prevention, Atlanta, Ga.
- 24.Weyant, R. S., J. W. Ezzelland, Jr., and T. Popovic. 2001. Basic laboratory protocols for the presumptive identification of Bacillus anthracis. Centers for Diseases Control and Prevention, Atlanta, Ga.
- 25.Zeigler, D. R. 1999. Bacillus Genetic Stock Center catalog of strains, 7th ed., vol. 2, Bacillus thuringiensis and Bacillus cereus. Bacillus Genetic Stock Center, Columbus, Ohio.
- 26.Zeigler, D. R. 2000. Bacillus Genetic Stock Center catalog of strains, 7th ed., vol. 1, Bacillus subtilis 168. Bacillus Genetic Stock Center, Columbus, Ohio.