Abstract
The nasopharyngeal bacterial flora of healthy rhesus macaques was surveyed for the presence of Neisseria and Haemophilus species, as well as Moraxella catarrhalis. M. catarrhalis was found both in healthy rhesus macaques and in possibly immunocompromised rhesus macaques. Several Haemophilus spp. that are part of the normal nasopharyngeal bacterial flora of humans were found in many animals; these Haemophilus species included H. parahaemolyticus, H. segnis, and H. parainfluenzae. While Haemophilus influenzae was not identified, it is possible that the identification of H. influenzae types may have been thwarted by the growth of less fastidious species. A number of animals harbored Neisseria spp. such as N. sicca. However, Neisseria meningitidis was not found. In summary, it appears as though the rhesus macaque may be used as a model for M. catarrhalis infections. Moreover, in view of the susceptibility of macaques to organisms of the Haemophilus and Neisseria genera, it is possible that these animals may also accurately model nontypeable H. influenzae and N. meningitidis infections.
Animal models that accurately reproduce the signs, pathology, and the microbial milieu of infections with Moraxella catarrhalis, nontypeable Haemophilus influenzae (NTHi), and Neisseria meningitidis are needed, among other reasons, for reliable testing of the safety, immunogenicity, and efficacy of vaccines against these agents (1, 5, 6, 8). These organisms colonize the nasopharynx of healthy humans, and therefore their presence as part of the normal flora of animals of a given species is an important consideration in selecting such animals as a research model (1, 5, 6, 8).
As the first step to ascertain whether the rhesus macaque can serve as a suitable animal model for human infections with M. catarrhalis, N. meningitidis, or NTHi, the nasopharyngeal bacterial flora of 55 healthy rhesus macaques was surveyed by standard bacteriological methods. In addition, during the winter of 2002, the presence of M. catarrhalis in colony animals presenting with epistaxis was determined. The rationale for the latter search was based on the previous identification of M. catarrhalis as the etiologic agent of the “bloody-nose” syndrome in another macaque species, namely, Macaca fascicularis (7).
For the general survey, 55 healthy rhesus macaques (Macaca mulatta) were randomly selected with regards to sex and age from the colony of the Tulane National Primate Research Center. Animals were excluded if they had been subjected to antibiotic treatment within 1 year of this study. For the M. catarrhalis survey, rhesus macaques with epistaxis but otherwise with any history, sex, or age were included. Animals were anesthetized with ketamine hydrochloride (Ketaset; Fort Dodge Animal Health, Overland Park, Kans.); 10 mg of drug per kg of body weight was given intramuscularly. Both nares were sampled in each animal, with a single culture swab (Culturette; Becton Dickinson Microbiology Systems [BD], Sparks, Md.). The animal was then placed in ventral recumbency. With the help of an assistant to open the animal's mouth, a laryngoscope (Welch Allyn) was used to visualize the pharyngeal region. A second swab was carefully passed through the mouth, to avoid touching the oral cavity, and the pharyngeal region was sampled. Both nasal and pharyngeal swabs were immediately transported to the microbiology lab for culture.
For the general survey, bacteria present on nasal or pharyngeal swabs were plated both on Trypticase soy agar with 5% sheep blood (TSA/blood) (BD) and chocolate II agar (BD). TSA/blood is a wide-spectrum, permissive medium for both gram-negative and -positive bacteria. Hemolytic organisms are apparent on this medium. Chocolate II agar permits, in addition, growth of fastidious genera such as Haemophilus and pathogenic Neisseria. Growth was enhanced on both media by placing plates under 5 to 10% carbon dioxide. Selected colonies were Gram stained to assess staining pattern and morphology. The coagulase test (Murex Biotech Ltd., Dartfor, United Kingdom), which qualitatively assesses the ability to clot plasma, was used to identify pathogenic staphylococci such as S. aureus, S. intermedius, and S. hyicus. The catalase test (presence of bubbles in a 3% H2O2 bacterial suspension) was used to discriminate between staphylococci (catalase positive) and streptococci (catalase negative). The oxidase test (Taxo N-discs; BD), based on the presence within a bacterium of a cytochrome oxidase electron transport chain, was used to help discriminate between organisms of the genus Neisseria and other gram-negative cocci. P discs (Optochin [ethyl hydrocupreine] disks; BD) were used to identify Streptococcus pneumoniae. To identify organisms of the Neisseriaceae family (namely, the genera Neisseria, Moraxella [including the Branhamella subgenus], Acinetobacter, and Kingella) or of the Haemophilus genus, the RapID NH system (Remel, Norcross, Ga.) was used. This system identifies and differentiates Haemophilus species and biochemically types Haemophilus influenzae and Haemophilus parainfluenzae. Modified Thayer Martin agar (BD) was used to grow bacteria from the swabs of five animals. Thayer Martin agar is a selective and enriched medium for the isolation and cultivation of pathogenic Neisseria spp. (N. gonorrhoeae and N. meningitidis) from mixed flora (4). The inclusion of hemoglobin, Bio-X, and dextrose as nutrients facilitates growth of fastidious microorganisms. Antibiotics are added to inhibit the growth of normal flora such as yeast and gram-positive and gram-negative bacteria. Trimethoprim lactate inhibits Proteus swarming (4).
For the M. catarrhalis survey, swabs were plated on TSA/blood. M. catarrhalis was tentatively identified by colony morphology and Gram staining and positively identified to the species level using Catarrhalis test disks (butyrate esterase production) (Remel, Lenexa, Kans.).
Haemophilus spp. were very prevalent, as they could be isolated from 54 of 55 animals (Table 1). They were cultivated from pharyngeal swabs but appeared not to be present in nasal swabs. The predominant species was Haemophilus parahaemolyticus, which is part of the normal respiratory flora in humans. Also, Haemophilus segnis and H. parainfluenzae were occasionally found. No H. influenzae was isolated.
TABLE 1.
Bacterial genera and types found in the nose and pharynx of healthy rhesus macaques
| Bacteria | Animals with bacteriaa
|
||
|---|---|---|---|
| Nose | Pharynx | Nose and pharynx | |
| Haemophilus | 0/55 | 54/55 | |
| Neisseria | 1/55 | 7/55 | |
| Moraxella | 0/55 (1/5) | 0/55 (0/5) | |
| Streptococcus | |||
| Alpha-hemolytic | 0/55 | 55/55 | |
| Beta-hemolytic | 1/55 | 1/55 | |
| Staphylococcus | 41/55 | 50/55 | |
| Staphylococcus aureus | 48/55 | 33/55 | |
| Diphtheroids | 22/55 | 15/55 | |
| Kingella spp. | 26/55 | 0/55 | |
| Rod-shaped | |||
| Gram-positive | 34/55 | ||
| Gram-negative | 3/55 | ||
The number of animals with bacteria/total number of animals is shown. Samples of bacteria from the nose or pharynx or both were taken. The values in parentheses are for swabs cultured on TSA/blood plates at room temperature.
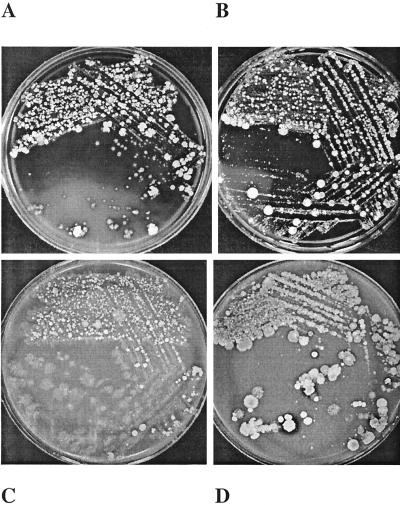
Nonpathogenic Neisseria spp. were identified on the basis of Gram staining and morphology. They were present in the pharynxes of 7 animals and the nose of 1 of 55 animals (Table 1). In two cases where the morphology was unclear, identification to the species level was performed and yielded Neisseria sicca as the identity of both isolates. Pathogenic Neisseria spp. were therefore not observed. However, considering the profusion of organisms that were typically observed on our primary swabs (Fig. 1) and since pathogenic Neisseria spp. (e.g., N. gonorrhoeae and N. meningitidis) are fastidious, it is possible that their presence was overlooked. For this reason, the pharyngeal and nasal swabs of five animals were also cultured on modified Thayer Martin agar. No Neisseria growth was observed.
FIG. 1.
Primary bacterial cultures of pharyngeal (A and C) and nasal (B and D) swabs from a healthy rhesus macaque. TSA/blood (A and B) and chocolate II agar (C and D) cultures are shown.
In the initial survey of 50 animals, Moraxella spp. were not found. Following the same rationale as for the failure to find pathogenic Neisseria spp., i.e., the notion that overgrowth of primary cultures by normal flora might occlude visualization or altogether impede growth of pathogenic species, the pharyngeal and nasal swabs of five additional animals also were cultured on TSA/blood plates but at room temperature. Under these conditions, the nose of one animal (one of five) yielded a Moraxella colony which was identified as M. catarrhalis (Table 1). This animal did not have epistaxis. In addition, during the winter of 2002, animals that presented with epistaxis were specifically examined for M. catarrhalis. A total of 33 animals from a colony of 968 rhesus macaques showed the “bloody-nose” sign. All of these animals were infected with M. catarrhalis. Of these 33 animals, 16 (48%) were experimentally infected with simian or simian/human immunodeficiency virus, and 6 (18%) were antibody and/or PCR positive for simian retrovirus type D (SRV), a virus enzootic in the colony, for a total of 19 infected animals (3 animals were doubly infected). All three of these viruses may have a suppressive effect on the immune system (2, 3). Of the 33 animals with epistaxis, 14 (42%) were free from immunosuppressive virus.
Alpha-hemolytic streptococci were grown from pharyngeal samples from all of the animals in the general survey (all 55 animals) but not from any samples from noses of the animals (Table 1). These organisms were not identified as S. pneumoniae, as the specific test for this organism was negative. They were loosely identified on the basis of their resistance to optochin as part of the viridans group, which contains many species. In contrast, beta-hemolytic streptococci were very rare, as they were cultivated from the pharynx of only one animal and the nose of one other monkey (Table 1).
Staphylococcus spp. other than S. aureus were found in the pharynxes of 50 animals and in the noses of 41 of 55 animals (Table 1). S. aureus, as confirmed by the coagulase test, was very prevalent. It was cultivated from pharyngeal swabs of 33 animals and nose swabs of 48 of 55 animals (Table 1). Miscellaneous species such as gram-positive coryneform bacilli, also known as diphtheroids, were found in several animals, as revealed by both pharyngeal (15 of 55) and nasal (22 of 55) cultures (Table 1). Bacteria of the genus Kingella (Neisseriaceae family) were identified in none of the pharyngeal cultures but in 26 of 55 of the nasal cultures (Table 1). Yeasts were rarely found (2 of 55). Several animals harbored gram-positive (34 of 55) and gram-negative (3 of 55) rod-shaped bacteria (Table 1). The former were not identified further. Two of the latter isolates were organoleptically identified as Proteus spp., and the third one was not a Haemophilus species.
Current literature describes M. catarrhalis as a parasite of humans exclusively (5). However, as already mentioned, previous research in primates uncovered this organism as the etiologic agent of the “bloody-nose” syndrome in Macaca fascicularis (7), and we have now found M. catarrhalis not only in possibly immunocompromised rhesus macaques but also in animals not detectably infected with immunosuppressive virus species. In fact, 42% of the animals with epistaxis were not infected either with SRV or with simian or simian/human immunodeficiency virus. Moreover, the proportion of SRV-infected animals in the subpopulation of colony animals that were also infected with M. catarrhalis (18% [this study]) was comparable to the prevalence of SRV in the colony of 968 animals that were specifically surveyed for M. catarrhalis (14% [unpublished results]). Therefore, it is not likely that the presence of SRV increased the incidence of the bloody-nose syndrome. The results suggest that M. catarrhalis is part of the normal flora of rhesus monkeys. As with humans, under certain circumstances as yet undefined, the organism may become pathogenic. In this regard, the rhesus monkey appears to mimic the situation in humans.
Several Haemophilus spp. that are part of the normal nasopharyngeal bacterial flora of humans also were found. These species included H. parahaemolyticus, H. segnis, and H. parainfluenzae. While H. influenzae was not identified, it remains possible, as with the case of the M. catarrhalis colony that was isolated after restricting the growth of other organisms, that the identification of H. influenzae types may have been thwarted by the growth of less fastidious species. Of note was the high prevalence of Haemophilus spp. among the animals, since virtually all animals harbored such organisms in their pharynx.
Fewer animals harbored Neisseria spp. such as N. sicca. Despite the use of the selective Thayer Martin medium, N. meningitidis was not found. It should be pointed out, however, that this more thorough approach was used with only five animals.
In summary, the rhesus macaque might be useful as a model for M. catarrhalis infections. In view of the susceptibility of macaques to organisms of the Haemophilus and Neisseria genera, it is possible that these animals also may accurately model NTHi and N. meningitidis infections.
Acknowledgments
This work was supported in part through a research agreement with GlaxoSmithKline and by grant RR00164 from the National Institutes of Health.
We thank Kathrine Phillippi for kindly providing animal census information.
REFERENCES
- 1.Foxwell, A. R., J. M. Kyd, and A. W. Cripps. 1998. Nontypeable Haemophilus influenzae: pathogenesis and prevention. Microbiol. Mol. Biol. Rev. 62:294-308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hirsch, V. M., and J. D. Lifson. 2000. Simian immunodeficiency virus infection of monkeys as a model system for the study of AIDS pathogenesis, treatment, and prevention. Adv. Pharmacol. 49:437-477. [DOI] [PubMed] [Google Scholar]
- 3.Lackner, A. A., M. H. Rodriguez, C. E. Bush, R. J. Munn, H. S. Kwang, P. F. Moore, K. G. Osborn, P. A. Marx, M. B. Gardner, and L. J. Lowenstine. 1988. Distribution of a macaque immunosuppressive type D retrovirus in neural, lymphoid, and salivary tissues. J. Virol. 62:2134-2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martin, J. E., T. E. Billings, J. F. Hackney, and J. D. Thayer. 1967. Primary isolation of N. gonorrhoeae with a new commercial medium. Public Health Rep. 82:361-363. [PMC free article] [PubMed] [Google Scholar]
- 5.Murphy, T. F. 1996. Branhamella catarrhalis: epidemiology, surface antigenic structure, and immune response. Microbiol. Rev. 60:267-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salit, I. E., and L. Tomalty. 1986. A neonatal mouse model of meningococcal disease. Clin. Investig. Med. 9:119-123. [PubMed] [Google Scholar]
- 7.VandeWoude, S. J., and M. B. Luzarraga. 1991. The role of Branhamella catarrhalis in the “bloody-nose syndrome” of cynomolgus macaques. Lab. Anim. Sci. 41:401-406. [PubMed] [Google Scholar]
- 8.Verduin, C. M., C. Hol, A. Fleer, H. van Dijk, and A. van Belkum. 2002. Moraxella catarrhalis: from emerging to established pathogen. Clin. Microbiol. Rev. 15:125-144. [DOI] [PMC free article] [PubMed] [Google Scholar]