Abstract
Evidence suggests that Pseudomonas aeruginosa bacteria form biofilms within the airways of adults with cystic fibrosis (CF). The objective of this study was to determine whether clinical isolates of P. aeruginosa recovered from adults with CF have similar susceptibilities to individual antibiotics and to antibiotic combinations when grown as adherent monolayers or as biofilms compared to when they are grown using planktonic methods. Twelve multiresistant P. aeruginosa isolates, one mucoid and one nonmucoid from each of six CF patients, were grown conventionally under planktonic conditions, as adherent bacterial monolayers, and as biofilms. Each bacterial isolate remained genotypically identical despite being cultured under planktonic, adherent, or biofilm growth conditions. Isolates grown as adherent monolayers and as biofilms were less susceptible to bactericidal killing by individual antibiotics compared to those grown planktonically. More importantly, biofilm-grown bacteria, but not adherent monolayer-grown bacteria, were significantly less susceptible to two- and three-drug combinations of antibiotics than were planktonically grown bacteria (P = 0.005). We conclude that biofilm-grown bacteria derived from patients with CF show decreased susceptibility to the bactericidal effects of antibiotic combinations than do adherent and planktonically grown bacteria.
Considerable in vivo and in vitro evidence exists to suggest that Pseudomonas aeruginosa bacteria form biofilms within the airways of adults with chronic cystic fibrosis (CF) pulmonary infection (5, 9, 16, 26). Bacterial biofilms are dense communities of bacteria, encased in exopolysaccharide, that adhere to biological or prosthetic surfaces. To form biofilms, individual bacteria must first adhere, via bacterial surface flagella, to damaged tissue and form a monolayer (10). Subsequently, bacteria attach to the monolayer and form a biofilm colony on the monolayer surface (23).
Despite the evidence that P. aeruginosa grows in the airway of CF patients as a biofilm, conventional clinical microbiologic testing involves the culture of planktonically grown bacteria retrieved from sputum of CF patients. The bacteria are grown planktonically in broth, and antibiotic susceptibilities against individual antibiotics are assessed. The scientific paradox facing physicians treating CF patients is that therapeutic antibiotics are chosen based on the tests of antibiotic susceptibility of planktonic bacteria cultured from sputum. However, since bacteria may actually grow adherent to the airway and as biofilms within the airways of CF patients, the susceptibility pattern which is used clinically to direct antibiotic therapy may not be relevant to the actual susceptibilities of the bacteria which exist in the airway biofilm and cause clinical infection (10).
Another paradox illustrating the discrepancies between clinical practice and microbiology laboratory practice is that conventional antibiotic susceptibility tests evaluate P. aeruginosa organisms for susceptibility only against single antibiotics. However, many CF-associated P. aeruginosa strains are multiresistant to single antibiotics (11, 17) and acute CF exacerbations caused by P. aeruginosa infection are almost always treated clinically with combination antibiotic therapy (24, 27). Thus, traditional antibiotic susceptibility testing using single antibiotics has limited relevance in this clinical context.
In vitro techniques for culturing bacterial monolayers adherent to surfaces and for culturing bacterial biofilms have been described (6, 21). In contrast to conventional techniques performed in clinical microbiology laboratories, in which bacteria are grown planktonically, cultures of adherent bacteria and biofilm cultures allow the bacteria to attach to and grow on external surfaces. Our laboratory has also described and validated a method for testing planktonically grown bacteria against multiple combinations of antibiotics simultaneously. Our previous work using the multiple combination bactericidal test (MCBT) against the CF bacterial pathogens P. aeruginosa and Burkholderia cepacia showed that combinations of two or three antibiotics demonstrated in vitro activity when individual antibiotics showed little or none (1, 20).
In this study, we evaluated the results of susceptibility testing of single and combination antibiotics against bacteria grown planktonically, those grown adherent to microtiter wells early in the process of biofilm formation, and those grown as biofilms. The objective of the study was to determine whether P. aeruginosa recovered from adults with CF are more resistant to single antibiotics and to combination antibiotic therapy when grown as adherent monolayers and as biofilms, than when they are conventionally cultured using standard planktonic methods. This finding would be relevant to CF, since P. aeruginosa cells exist in the biofilm mode of growth in the airway of CF patients (5, 9, 16, 26) and susceptibility tests on biofilm-grown bacteria may provide clinicians with more relevant information on which to base antibiotic treatment.
MATERIALS AND METHODS
Bacterial isolates.
P. aeruginosa isolates recovered from the respiratory secretions of six patients with CF were studied. These multiresistant P. aeruginosa isolates had been referred to the Children's Hospital of Eastern Ontario from North American CF centers for multiple combination bactericidal testing. In total, 12 isolates, one nonmucoid and one mucoid from each of six CF patients, underwent testing.
Test procedures. (i) MIC and MBC determination.
MICs were determined by the microtiter method as described in NCCLS guidelines (22). Six antipseudomonal antibiotics (tobramycin, amikacin, meropenem, piperacillin, ceftazidime, and ciprofloxacin), representing agents from the β-lactam, aminoglycoside, and fluoroquinolone classes, used clinically against CF, were tested against the isolates. MBCs were determined by spreading 10 μl of suspension from wells showing no growth (i.e., no turbidity) at 24 h onto a blood agar plate, which was then incubated for 24 h at 35°C and examined for 99.9% killing.
(ii) MCBT.
MCBTs were done as previously described (1, 20). Combinations of 1, 2, or 3 of a total of 10 antibiotics were placed in 96-well round-bottom microtiter plates (Nunc Inc., Roskilde, Denmark), giving a total of 90 antibiotic combinations tested per isolate. The plates were incubated at 35°C for 48 h. At 48 h, the contents of nonturbid wells were subcultured by streaking 10 μl of suspension onto 5% Columbia sheep blood agar plates (PML Microbiologicals, Mississauga, Ontario, Canada), which were incubated overnight at 35°C and examined for 99.9% killing the next day.
The antibiotic concentrations selected for MCBT testing were based on the highest concentrations in serum achievable for intravenous or oral preparations (for example, tobramycin was tested at 10 μg/ml). In addition, for tobramycin, a concentration achievable in sputum of CF patients by aerosol administration (200 μg/ml) was evaluated. Antibiotics not commonly used to treat P. aeruginosa, such as chloramphenicol, were included in the MCBT template since we have previously shown that these antibiotics may exhibit in vitro bactericidal effects when combined with traditional antipseudomonal antibiotics (21). Azithromycin was chosen because it is being increasingly used as a chronic therapy for CF, and recent data indicate that its long-term use may improve lung function and decrease the number of respiratory exacerbations in patients with CF (33).
Adherent bacterial cultures.
Using the method of Miyake et al. (21), adherent monolayers of each of the 12 P. aeruginosa isolates were established as follows. Overnight growth of P. aeruginosa in Mueller-Hinton broth type II was diluted to a 0.5 McFarland standard and then further diluted 1:100 to give a bacterial concentration of 5 × 106 CFU/ml. A 50-μl volume of bacterial suspension was added to each well of a 96-well microtiter plate. The microtiter plates were centrifuged at 20°C for 10 min at 450 × g. The microtiter plates were then incubated at 35°C for 2 h. The broth was completely removed from each well and replaced with 70 μl of fresh sterile Mueller-Hinton broth type II. A 30-μl volume of the appropriate antibiotic in serial dilutions was added to the wells. The plates were incubated at 35°C overnight. The adherent bacteria were assessed by sampling directly from the monolayer and subculturing onto blood agar plates to determine the MBC.
Biofilm bacterial cultures.
In vitro biofilms were cultured using a modification of the Calgary biofilm device. This method of biofilm culture has been previously validated and shown to be reproducible (6). Briefly, the isolates were grown at 35°C for 4 h adherent to plastic pegs that sit in standard 96-well plates. A rocking table was used to produce shear forces across each peg, resulting in the formation of equivalent biofilms at each peg site. The biofilm-containing pegs were then transferred to a standard 96-well plate in which dilutions of specified antibiotics were prepared, and the plates were incubated overnight. The biofilms were removed from the pegs by sonication, and the viability of the biofilm bacteria were assessed by plate counts. The minimal biofilm eradication concentration was then defined as the minimal concentration of antibiotic required to eradicate the biofilm (6). This procedure was similarly used to assess combination bactericidal antibiotic susceptibilities of biofilms by MCBT methods.
Genotypic characterization of the isolates.
Molecular genotyping of each P. aeruginosa isolate was carried out by pulsed-field gel electrophoresis. Genomic DNA was prepared as described by Laing et al. (19). DNA was digested by the restriction enzyme SpeI and then electrophoresed in 1.0% agarose gels in 0.5× TBE buffer, using a CHEF Mapper XA apparatus (Bio-Rad, Hercules, Calif.). The gels were run for 20 h at 6 V/cm using switch times of 5 to 45 s ramped in a linear fashion.
Restriction fragment profiles were visually compared and were interpreted based on guidelines recommended by Tenover et al. (32). Isolates with identical restriction fragment profiles were considered to represent a single strain. Isolates with restriction profiles, which differed by one two three fragments (bands), were considered to be closely related strains that evolved from a single clone. Isolates with restriction profiles differing by four bands or more were considered to be different strains and therefore unrelated.
Statistical analysis.
SAS PROC MIXED was used to perform a repeated-measures factorial analysis of variance to analyze the multiple-antibiotic-combination data. There were two within-subject factors; type of isolate and culturing method. Covariance structures were used to model covariance across type of isolate and across type of culturing method. The only significant effect was that of the culture method; hence, all three pairwise comparisons were tested for significance using the Tukey-Kramer method of adjusting P values for multiple comparisons.
RESULTS
Biofilm formation.
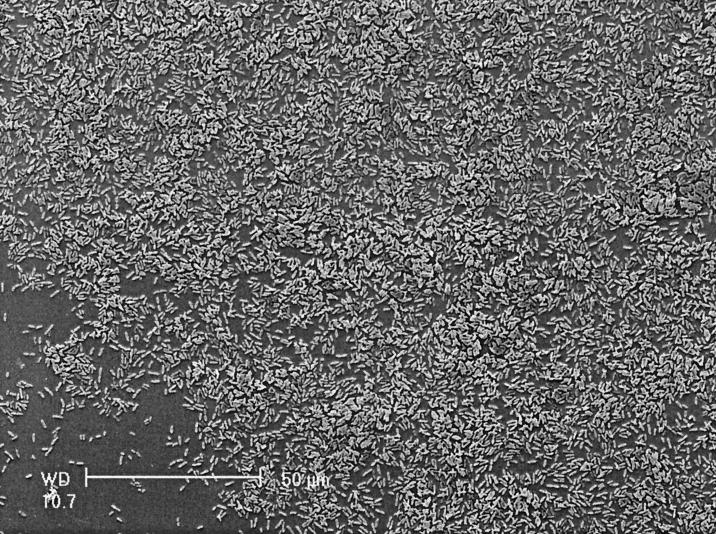
A scanning electron micrograph of a P. aeruginosa biofilm (nonmucoid isolate from patient 3) is shown in Fig. 1. The electron micrograph of the surface of the plastic peg reveals individual bacteria adherent to the peg, and in addition, microcolonies of bacteria heaped up on one another surrounded by a matrix of exopolysaccharide.
FIG. 1.
Scanning electron micrograph of P. aeruginosa (nonmucoid isolate from patient 3) grown as a biofilm attached to the plastic peg.
Single-antibiotic susceptibilities.
Tables 1 and 2 illustrate the differences in single-antibiotic susceptibilities demonstrated by the adherent and biofilm-grown P. aeruginosa compared to the same isolates when grown in planktonic broth culture. The mucoid and nonmucoid planktonically grown isolates had a relatively high level of resistance to individual antibiotics at baseline; however, when these isolates were grown in adherent monolayers and as biofilms, the MICs and MBCs of the antibiotics were even higher (i.e., the adherent and biofilm isolates were less susceptible to growth inhibition and killing by individual antibiotics).
TABLE 1.
Susceptibility of mucoid P. aeruginosa isolates to single antibioticsa
| Isolate and mode of growth | Tobramycin
|
Amikacin
|
Meropenem
|
Ceftazidime
|
Piperacillin
|
Ciprofloxacin
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MIC | MBC | MIC | MBC | MIC | MBC | MIC | MBC | MIC | MBC | MIC | MBC | |
| Isolate 1 | ||||||||||||
| Planktonic | 8 | 32 | 32 | 64 | 16 | 32 | 64 | 64 | >256 | >256 | 4 | 8 |
| Adherent | 16 | 256 | 32 | >256 | 16 | >128 | >256 | >256 | >256 | >256 | 4 | 32 |
| Biofilm | 8 | 128 | 16 | 128 | 32 | 128 | >256 | >256 | >256 | >256 | 4 | 32 |
| Isolate 2 | ||||||||||||
| Planktonic | 16 | 16 | 64 | 64 | 32 | 64 | 32 | 32 | >256 | >256 | 4 | 4 |
| Adherent | 64 | 256 | 256 | >256 | 32 | 128 | 256 | 256 | >256 | >256 | >32 | >32 |
| Biofilm | 64 | >256 | 256 | >256 | 64 | 128 | >256 | >256 | >256 | >256 | >32 | >32 |
| Isolate 3 | ||||||||||||
| Planktonic | 1 | 4 | 4 | 8 | 128 | >128 | 16 | 16 | >256 | >256 | 0.5 | 1 |
| Adherent | 2 | 64 | 4 | 128 | 128 | >128 | >256 | >256 | >256 | >256 | >32 | >32 |
| Biofilm | 1 | 64 | 4 | 64 | 128 | >128 | >256 | >256 | >256 | >256 | >32 | >32 |
| Isolate 4 | ||||||||||||
| Planktonic | 8 | 16 | 32 | 64 | 2 | 8 | 64 | 64 | 64 | >256 | 4 | 8 |
| Adherent | 16 | 256 | 32 | 128 | 2 | 128 | 64 | 64 | 64 | >256 | 4 | 8 |
| Biofilm | 16 | 128 | 32 | 128 | 2 | 64 | 64 | 64 | 64 | 128 | 4 | 16 |
| Isolate 5 | ||||||||||||
| Planktonic | 32 | 32 | 64 | 128 | 16 | 32 | 8 | 8 | >256 | >256 | 0.5 | 4 |
| Adherent | 16 | >256 | 64 | 256 | 16 | 128 | 128 | 128 | >256 | >256 | 0.5 | 4 |
| Biofilm | 32 | 256 | 128 | 128 | 16 | 128 | 128 | 128 | 256 | >256 | 0.5 | 4 |
| Isolate 6 | ||||||||||||
| Planktonic | 64 | 64 | 64 | 128 | 4 | 8 | 8 | 8 | 2 | 128 | 4 | 16 |
| Adherent | >256 | >256 | 128 | >256 | 16 | 128 | 8 | 8 | 1 | 128 | >32 | >32 |
| Biofilm | 256 | >256 | 128 | >256 | 16 | 128 | 16 | 16 | 2 | >256 | >32 | >32 |
Values are numbers of micrograms per milliliter. Values in bold indicate a >twofold-dilution increase in the MIC or MBC for adherent or biofilm-cultured isolates compared to planktonic isolates.
TABLE 2.
Susceptibility of nonmucoid P. aeruginosa isolates to single antibioticsa
| Isolate and mode of growth | Tobramycin
|
Amikacin
|
Meropenem
|
Ceftazidime
|
Piperacillin
|
Ciprofloxacin
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MIC | MBC | MIC | MBC | MIC | MBC | MIC | MBC | MIC | MBC | MIC | MBC | |
| Isolate 1 | ||||||||||||
| Planktonic | 4 | 8 | 16 | 32 | 16 | 64 | 32 | 64 | >256 | >256 | 8 | 8 |
| Adherent | 8 | >256 | 32 | >256 | 16 | >128 | 256 | >256 | >256 | >256 | >32 | >32 |
| Biofilm | 8 | >256 | 32 | >256 | 16 | >128 | >256 | >256 | >256 | >256 | >32 | >32 |
| Isolate 2 | ||||||||||||
| Planktonic | 8 | 16 | 32 | 64 | 1 | 16 | 16 | 128 | >256 | >256 | 4 | 16 |
| Adherent | 8 | 128 | 64 | 256 | 8 | 128 | 64 | 256 | >256 | >256 | >32 | >32 |
| Biofilm | 16 | 128 | 64 | 256 | 16 | 128 | 128 | >256 | >256 | >256 | >32 | >32 |
| Isolate 3 | ||||||||||||
| Planktonic | 1 | 4 | 4 | 8 | 128 | >128 | 16 | 32 | >256 | >256 | 0.5 | 4 |
| Adherent | 2 | 64 | 4 | 128 | 128 | >128 | >256 | >256 | >256 | >256 | >32 | >32 |
| Biofilm | 1 | 32 | 2 | 64 | 128 | >128 | >256 | >256 | >256 | >256 | >32 | >32 |
| Isolate 4 | ||||||||||||
| Planktonic | 0.5 | 2 | 1 | 4 | 32 | >128 | 8 | 16 | >256 | >256 | 4 | 4 |
| Adherent | 0.5 | 32 | 2 | 256 | 32 | >128 | 128 | >256 | 256 | >256 | >32 | >32 |
| Biofilm | 1 | 32 | 4 | 128 | 64 | >128 | 256 | >256 | >256 | >256 | >32 | >32 |
| Isolate 5 | ||||||||||||
| Planktonic | >256 | >256 | >256 | >256 | 16 | 32 | 32 | 128 | >256 | >256 | 8 | 16 |
| Adherent | >256 | >256 | >256 | >256 | 32 | >128 | >256 | >256 | >256 | >256 | >32 | >32 |
| Biofilm | >256 | >256 | >256 | >256 | 16 | >128 | 256 | >256 | 128 | >256 | >32 | >32 |
| Isolate 6 | ||||||||||||
| Planktonic | >256 | >256 | >256 | >256 | 64 | 128 | >256 | >256 | >256 | >256 | 8 | 16 |
| Adherent | >256 | >256 | >256 | >256 | 64 | >128 | >256 | >256 | >256 | >256 | 8 | >32 |
| Biofilm | >256 | >256 | >256 | >256 | 64 | >128 | >256 | >256 | >256 | >256 | 8 | >32 |
Values are numbers of micrograms per milliliter. Values in bold indicate a >two-fold-dilution increase in the MIC or MBC for adherent or biofilm-cultured isolates compared to planktonic isolates.
Both the ceftazidime and ciprofloxacin MICs and MBCs were significantly greater (by at least a twofold dilution) for adherent and biofilm bacteria than for planktonically grown bacteria (this was true for the majority of the isolates) (Table 3). In contrast, the MICs of the aminoglycoside antibiotics and meropenem for most adherent and biofilm-grown isolates were not significantly higher than for planktonically grown isolates. However, the MBCs increased by at least two dilutions for at least 50% of the adherent and biofilm-grown isolates compared to planktonically grown isolates. For piperacillin, comparisons were impossible since the planktonically grown isolates were extremely resistant to piperacillin to begin with.
TABLE 3.
Summary of the number of isolates (mucoid and nonmucoid) giving a twofold-dilution MIC or MBC increase from adherent to planktonic, biofilm to planktonic, and biofilm to adherent
| Antibiotic | Adherent to planktonic
|
Biofilm to planktonic
|
Biofilm to adherent
|
|||
|---|---|---|---|---|---|---|
| MIC (n = 12) | MBC (n = 12) | MIC (n = 12) | MBC (n = 12) | MIC (n = 12) | MBC (n = 12) | |
| Tobramycin | 2 (17%) | 10 (83%) | 2 (17%) | 10 (83%) | 0 (0%) | 0 (0%) |
| Amikacin | 1 (8%) | 7 (58%) | 2 (17%) | 6 (50%) | 0 (0%) | 0 (0%) |
| Meropenem | 2 (17%) | 6 (50%) | 2 (17%) | 6 (50%) | 0 (0%) | 0 (0%) |
| Ceftazidime | 9 (75%) | 7 (58%) | 9 (75%) | 6 (50%) | 0 (0%) | 0 (0%) |
| Piperacillin | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Ciprofloxacin | 8 (67%) | 6 (50%) | 8 (67%) | 6 (50%) | 0 (0%) | 0 (0%) |
There were no significant differences in susceptibilities to single antibiotics between adherently grown and biofilm-grown isolates (Table 3). Results were reproducible when testing was repeated 8 weeks later.
Combination antibiotic susceptibilities.
Ninety double and triple antibiotic combinations were tested for bactericidal activity against the planktonic, adherent, and biofilm-grown P. aeruginosa isolates in MCBT. The MCBT antibiotic template used is shown in Table 4. The combination antibiotic susceptibility profile was identical for the planktonic, adherent, and biofilm-grown isolates for two of six mucoid isolates and one of six nonmucoid isolates. However, for the other nine isolates, the biofilm-grown bacteria showed decreased susceptibility to killing by combination antibiotics compared with the corresponding adherent and planktonically grown forms (Table 4 illustrates this phenomenon for one isolate). In total, biofilm-grown isolates were killed by an average of 14 ± 11 (of a total of 90) fewer bactericidal antibiotic combinations than were the corresponding planktonically grown isolates (P = 0.005) (Table 5). Adherent isolates were more susceptible to combination antibiotics than were biofilm-grown isolates. Although adherent isolates were killed by an average of 7 ± 7 fewer combinations than were planktonic isolates, this difference was not significant (P = 0.14). This pattern was identical for both mucoid and nonmucoid isolates (Table 5). Results were reproducible when the tests were repeated 8 weeks later.
TABLE 4.
MCBT template and active antimicrobial drug combinationsa
| Template or isolate and microtiter plate row | Antibiotic combination in indicated well of microtiter plate column:
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
| Template | ||||||||||||
| 1 | tob, az | tob, mer | tob, chl | tob, taz | tob, sxt | tob, ak | tob, tim | tob, caz | tob, cip | tob, az, mer | tob, az, chl | tob, az, taz |
| 2 | tob, az, sxt | tob, az, ak | tob, az, tim | tob, az, caz | tob, az, cip | tob, mer, chl | tob, mer, taz | tob, mer, sxt | tob, mer, ak | tob, mer, tim | tob, mer, caz | tob, mer, cip |
| 3 | tob, chl, taz | tob, chl, sxt | tob, chl, ak | tob, chl, tim | tob, chl, caz | tob, chl, cip | tob, taz, sxt | tob, taz, ak | tob, taz, tim | tob, taz, caz | tob, taz, cip | tob, sxt, ak |
| 4 | tob, sxt, tim | tob, sxt, caz | tob, sxt, cip | tob, ak, tim | tob, ak, caz | tob, ak, cip | tob, tim, caz | tob, tim, cip | tob, caz, cip | az, mer | az, chl | az, taz |
| 5 | az, sxt | az, ak | az, tim | az, caz | az, cip | mer, chl | mer, taz | mer, sxt | mer, ak | mer, tim | mer, caz | mer, cip |
| 6 | chl, taz | chl, sxt | chl, ak | chl, tim | chl, caz | chl, cip | taz, sxt | taz, ak | taz, tim | taz, caz | taz, cip | sxt, ak |
| 7 | sxt, tim | sxt, caz | sxt, cip | ak, tim | ak, caz | ak, cip | tim, caz | tim, cip | caz, cip | |||
| 8 | T10, az | T10, mer | T10, sxt | T10, caz | T10, cip | T10, mer, az | T10, mer, sxt | T10, mer, caz | T10, mer, cip | Growth control | Sterility control | |
| Planktonic mucoid P. aeru- ginosa isolate | ||||||||||||
| 1 | tob, az | tob, mer | tob, tim | tob, az, mer | tob, az, taz | |||||||
| 2 | tob, az, sxt | tob, az, ak | tob, az, tim | tob, az, caz | tob, az, cip | tob, mer, chl | tob, mer, taz | tob, mer, sxt | tob, mer, ak | tob, mer, tim | tob, mer, caz | tob, mer, cip |
| 3 | tob, chl, taz | tob, taz, sxt | tob, taz, ak | tob, taz, tim | tob, taz, caz | tob, taz, cip | ||||||
| 4 | tob, sxt, tim | tob, sxt, cip | tob, ak, tim | tob, tim, caz | az, mer | |||||||
| 5 | az, sxt | |||||||||||
| 6 | ||||||||||||
| 7 | ||||||||||||
| 8 | T10, mer, az | T10, mer, sxt | T10, mer, caz | T10, mer, cip | Growth control | Sterility control | ||||||
| Adherent mucoid P. aeru- ginosa isolate | ||||||||||||
| 1 | tob, mer | tob, az, mer | ||||||||||
| 2 | tob, az, caz | tob, mer, chl | tob, mer, taz | tob, mer, sxt | tob, mer, ak | tob, mer, tim | tob, mer, caz | tob, mer, cip | ||||
| 3 | tob, chl, taz | tob, taz, caz | tob, taz, cip | |||||||||
| 4 | tob, tim, caz | az, mer | ||||||||||
| 5 | T10, mer, az | T10, mer, sxt | T10, mer, caz | T10, mer, cip | Growth control | Sterility control | ||||||
| 6 | ||||||||||||
| 7 | ||||||||||||
| 8 | ||||||||||||
| Biofilm-grown mucoid P. aeruginosa isolate | ||||||||||||
| 1 | tob, mer | tob, az, mer | ||||||||||
| 2 | tob, mer, tim | tob, mer, cip | ||||||||||
| 3 | tob, taz, caz | tob, taz, cip | ||||||||||
| 4 | ||||||||||||
| 5 | ||||||||||||
| 6 | ||||||||||||
| 7 | ||||||||||||
| 8 | Growth control | Sterility control | ||||||||||
Each entry represents a single well in a 96-well microtiter plate, and column and row numbers indicate well positions. Two- and three-drug antibiotic combinations were contained in each well. For the mucoid P. aeruginosa isolate grown under the different conditions, the data listed indicate active antimicrobial combinations; where no data is shown, the combination was not bactericidal. Abbreviations: az, azithromycin; mer, meropenem; tim, ticarcillin-clavulinic acid; taz, piperacillin-tazobactam; sxt, trimethoprim-sulfamethoxazole; ak, amikacin; caz, ceftazidime; cip, ciprofloxacin; chl, chloramphenicol; tob, tobramycin (200 μg/ml); T10, tobramycin (10 μg/ml).
TABLE 5.
Mean number of bactericidal combinations for isolates grown under planktonic, adherent, and biofilm conditions
| Patient no. and isolate type | Mean no. of bactericidal combinations (maximum = 90) for:
|
||
|---|---|---|---|
| Planktonic isolate | Adherent isolate | Biofilm isolates | |
| Mucoid isolates | |||
| 1 | 45 | 45 | 45 |
| 2 | 45 | 43 | 9 |
| 3 | 67 | 50 | 47 |
| 4 | 23 | 23 | 23 |
| 5 | 45 | 29 | 24 |
| 6 | 33 | 19 | 6 |
| Nonmucoid isolates | |||
| 1 | 45 | 45 | 43 |
| 2 | 30 | 30 | 19 |
| 3 | 68 | 50 | 48 |
| 4 | 64 | 61 | 52 |
| 5 | 21 | 11 | 10 |
| 6 | 0 | 0 | 0 |
| Mean no. of bactericidal combinations | 41 ± 20 | 34 ± 18a | 27 ± 19b |
P = 0.14 for comparison between adherent and planktonic isolates.
P = 0.005 for comparison between biofilm and planktonic isolates.
Antagonism.
Antagonism (growth of an organism when a third antibiotic is added to a previously bactericidal double-antibiotic combination) was rarely observed but was more common among biofilm-grown isolates than planktonically grown isolates. For instance, three (43%) of seven biofilm isolates but zero (0%) of eight planktonically grown isolates exhibited antagonism when a third antibiotic was added to tobramycin plus meropenem. Similar results were seen with tobramycin-plus-ceftazidime combinations, in which antagonism occurred in 43% of biofilm-grown isolates but only 13% of planktonically grown isolates. The addition of chloramphenicol or amikacin as the third antibiotic to an aminoglycoside-β-lactam combination was most likely to cause antagonism.
Bacterial genotyping.
Pulsed-field gel electrophoresis of the P. aeruginosa organisms revealed that the mucoid and nonmucoid paired isolates from patients 2 and 6 were derived from different clonal strains of P. aeruginosa. The other four pairs of mucoid and nonmucoid isolates had identical pulsed-field gel electrophoresis banding patterns.
Individual isolates from the same patient grown under planktonic, adherent, and biofilm culture conditions were consistently genotypically identical by pulsed-field gel electrophoresis (Fig. 2).
FIG. 2.
Pulsed-field gel electrophoresis of P. aeruginosa isolates. Nonmucoid isolate 1 has an identical banding pattern when grown as a biofilm (lane 2) and when grown planktonically (lane 3). Similar results are pictured for mucoid isolate 5 (lanes 4 and 6). Lanes 1 and 7 are control lanes, lane 5 represents results from another planktonic isolate; its biofilm equivalent had an identical banding pattern but is not shown in the figure.
DISCUSSION
Recent anatomical evidence of a biofilm mode of growth in the airway of CF patients and rigorous biochemical data demonstrating biofilm quorum-sensing signals in the sputum of CF patients support the contention that biofilms are present in the airways of adult patients with CF (10, 13, 16, 18, 26). Autopsy immunohistopathologic studies of lungs from CF patients demonstrate biofilm-like aggregates of P. aeruginosa organisms enclosed by circular profiles of exudate arranged in colonies and, in some cases, adherent to the walls of airways (5). Electron microscopy studies of sputum from CF patients have shown clusters of aggregated P. aeruginosa encased in densely stained matrix, suggesting that small biofilm communities may be recoverable in the sputum of adults with CF (26). Physiologic evidence of a biofilm mode of growth of P. aeruginosa in the lungs of CF patients has also been demonstrated, and the magnitude and chemical profile of intercellular bacterial homoserine lactone signaling molecules found in the sputum of CF patients is very similar to that found in in vitro-grown biofilms (26).
This study shows that P. aeruginosa bacteria that are recovered from the sputum of CF patients are less susceptible to single antibiotics when they are grown in vitro as adherent bacterial monolayers or as biofilms than when they are grown planktonically. In addition, we found that most biofilm-grown isolates are less susceptible to two- and three-drug combinations of antibiotics than adherent-grown isolates, which are themselves less susceptible than planktonically grown isolates. Mucoid and nonmucoid isolates exhibited similar behaviour.
The failure of conventional culture techniques to predict antibiotic susceptibilities may explain part of our failure to eradicate lung infection in adult patients with CF. Sputum cultures of planktonically grown bacteria may lead clinicians to believe that an organism is susceptible to antibiotics, whereas under in vivo conditions of biofilm growth the organism may be considerably more resistant to the bactericidal effect of antibiotics (8). Biofilm-based sensitivity testing mimics the physiology of airway infection in CF patients. It has not yet been demonstrated that it better predicts the response to antibiotic therapy than does conventional testing. However, preliminary data from studies of prosthetic joint infections, another type of infection where biofilms are key to pathogenesis, have shown dramatic response to therapy active in vitro against biofilms (35).
Several studies have shown that laboratory isolates of P. aeruginosa can be less susceptible to growth inhibition by single antibiotics when grown in biofilm conditions than when grown planktonically (2, 4, 34). This study is unique in that we explored clinical isolates of P. aeruginosa taken from CF patients, and we not only assessed MICs and MBCs against single antibiotics but also assessed the bactericidal effects of double- and triple-antibiotic combinations against these bacteria grown under planktonic, adherent, and biofilm conditions. The study findings are relevant, since in clinical practice P. aeruginosa infection is always treated with a minimum of two antipseudomonal drugs, and to be most useful, antibiotic susceptibility testing should assess the efficacy of the antibiotics as they are used under clinical conditions. This is the first study to assess the susceptibility of biofilm bacteria to combination antibiotic therapy and is also the first study to compare in vitro antibiotic susceptibilities of adherent versus biofilm-grown bacteria.
We grew biofilms of P. aeruginosa using a modification of the Calgary biofilm device (6). As depicted in Fig. 1, electron micrographs of the surface of the plastic pegs reveal microcolonies of bacteria, heaped up on one another and surrounded by a matrix of exopolysaccharide. Clearly, our method does produce in vitro biofilms; however, the height of the biofilm using this method is less than the 50-μm height of biofilms which are generated using continuous-flow cell slide culture chambers (3). This is a potential limitation of our technique, since biofilms grown on the Calgary biofilm device may be less mature than multilayered biofilms grown using continuous-flow cell slide culture chambers and may therefore exhibit different metabolic properties. However, the use of an individual flow cell culture method to grow biofilms for this study would have been extremely impractical, since this technology is not suited for rapid antibiotic susceptibility testing and since flow cell technology would have been impossible to apply to test multiple combinations of antibiotics simultaneously against each isolate. The advantage of the Calgary biofilm method is that it provides a relatively easy, reproducible assay to measure single and combination antibiotic activity against a biofilm.
Investigators have used adherent bacterial monolayers as a proxy for biofilms (21). Our study suggests that although single-antibiotic susceptibility results of adherent monolayers are similar to biofilms, the susceptibility of biofilms to the bactericidal effects of double and triple combinations of antibiotics is lower than that of adherent bacteria for the majority of isolates.
In the United States, synergy testing of planktonically grown bacteria is frequently performed to determine appropriate therapy against multiresistant bacterial isolates from CF patients (25). However, it is unclear whether in vitro results of MCBT testing, or synergy testing, of bacteria will translate into improved patient clinical responses to antibiotic therapy. Currently, in Canada, a multicenter clinical trial evaluating patient responses to MCBT-directed therapy against planktonic bacteria is under way. Clinical studies evaluating combination antibiotic therapy based on biofilm susceptibilities of pathogenic bacteria are also needed to ensure that in vitro susceptibilities translate to improved clinical responses in patients.
Biofilm resistance to antibiotics is likely to be multifactorial (15, 30). When bacteria are dispersed from a biofilm, they usually rapidly become susceptible to single antibiotics (4, 34), which suggests that the resistance of bacteria in biofilms is not acquired via mutations. Similarly, studies have shown that some antibiotics readily penetrate bacterial biofilms, suggesting that the physical barrier of the biofilm is not the only feature which protects biofilm bacteria against antibiotic killing (29).
One hypothesis explaining biofilm resistance is that there is an altered chemical microenvironment within the biofilm which antagonizes antibiotic effects. Studies have shown that oxygen can be completely consumed in the surface layers of the biofilm, leading to anaerobic conditions in the deep layers of the biofilm (14). Many antibiotics, such as aminoglycosides, are less effective against the same organism under anaerobic conditions than under aerobic conditions (31). Another hypothesis is that there is a subpopulation of bacteria within the biofilm which do not replicate and which are metabolically inactive and therefore are not killed by antibiotics (7, 12). This hypothesis is supported by findings from our study that show antibiotic resistance in newly formed adherent monolayers, even though they are too thin to pose a barrier to the penetration of antibiotics or metabolic substrates. These survivor cells may persist despite continued exposure to antibiotics and may serve to repopulate the biofilm. A recent study suggests that nonreplicating planktonic bacteria, grown in dense concentrations in the stationary phase, exhibit tolerance to antibiotics similar to that of biofilms (28). The authors found that the mechanism of this tolerance was dependent on the presence of persistor cells found in the stationary phase cultures and in the biofilm cultures. This observation has been supported by another study demonstrating that antibiotic-resistant phenotypic variants of P. aeruginosa with an enhanced ability to form biofilms arose at high frequency both in vitro and in the lungs of CF patients (16).
For all these reasons, it would appear reasonable and appropriate to develop a standardized susceptibility testing method for biofilm forms of pathogens that are associated with CF. Our study suggests that for determination of single-antibiotic susceptibilities, adherent-grown isolates will yield MIC and MBCs similar to biofilm-grown isolates, and thus testing of adherent isolates may be adequate. However, to obtain an adequate representation of the susceptibility of the organism to combination antibiotic therapy, it is necessary to test bacteria when grown as biofilms.
Acknowledgments
We acknowledge Ann Fook Yang for assistance with the scanning electron microscopy photos and Jennifer Clinch for statistical assistance.
REFERENCES
- 1.Aaron, S. D., W. Ferris, D. A. Henry, D. P. Speert, and N. E. MacDonald. 2000. Multiple combination bactericidal antibiotic testing for patients with cystic fibrosis infected with Burkholderia cepacia. Am. J. Respir. Crit. Care Med. 161:1206-1212. [DOI] [PubMed] [Google Scholar]
- 2.Anderl, J. N., M. S. Franklin, and P. S. Stewart. 2000. Role of antibiotic penetration limitation in Klebsiella pneumoniae biofilm resistance to ampicillin and ciprofloxacin. Antimicrob. Agents Chemother. 44:1818-1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anwar, H., J. L. Strap, and J. W. Costerton. 1992. Establishment of aging biofilms: possible mechanism of bacterial resistance to antimicrobial therapy. Antimicrob. Agents Chemother. 36:1347-1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anwar, H., T. van Biesen, M. Dasgupta, K. Lam, and J. W. Costerton. 1989. Interaction of biofilm bacteria with antibiotics in a novel in vitro chemostat system. Antimicrob. Agents Chemother. 33:1824-1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baltimore, R. S., C. D. C. Christie, and G. J. W. Smith. 1989. Immunohistopathologic localization of Pseudomonas aeruginosa in lungs from patients with cystic fibrosis. Am. Rev. Respir. Dis. 140:1650-1661. [DOI] [PubMed] [Google Scholar]
- 6.Ceri, H., M. E. Olson, C. Stremick, R. R. Read, D. Morck, and A. Buret. 1999. The Calgary biofilm device: new technology for rapid determination of antibiotic susceptibilities of bacterial biofilms. J. Clin. Microbiol. 37:1771-1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cochran, W. L., G. A. McFeters, and P. S. Stewart. 2000. Reduced susceptibility of thin Pseudomonas aeruginosa biofilms to hydrogen peroxide and monochloramine. J. Appl. Microbiol. 88:22-30. [DOI] [PubMed] [Google Scholar]
- 8.Costerton, J. W. 1999. Introduction to biofilm. Int. J. Antimicrob. Agents 11:217-221. [DOI] [PubMed] [Google Scholar]
- 9.Costerton, J. W., K.-J. Cheng, G. G. Geesey, T. I. Ladd, J. C. Nickel, M. Dasgupta, and T. J. Marrie. 1987. Bacterial biofilms in nature and disease. Annu. Rev. Microbiol. 41:435-464. [DOI] [PubMed] [Google Scholar]
- 10.Costerton, J. W., P. S. Stewart, and E. P. Greenberg. 1999. Bacterial biofilms: a common cause of persistent infections. Science 284:1318-1322. [DOI] [PubMed] [Google Scholar]
- 11.Dahl, M., A. Tybjærg-Hansen, P. Lange, and B. G. Nordestgaard. 1998. ΔF508 heterozygosity in cystic fibrosis and susceptibility to asthma. Lancet 351:1911-1913. [DOI] [PubMed] [Google Scholar]
- 12.Das, J. R., M. Bhakoo, M. V. Jones, and P. Gilbert. 1998. Changes in the biocide susceptibility of Staphylococcus epidermidis and Escherichia coli cells associated with rapid attachment to plastic surfaces. J. Appl. Microbiol. 84:858.. [DOI] [PubMed] [Google Scholar]
- 13.Davies, D. G., M. R. Parsek, J. P. Pearson, B. H. Iglewski, J. W. Costerton, and E. P. Greenberg. 1988. The involvement of cell-to-cell signals in the development of a bacterial biofilm. Science 280:295-298. [DOI] [PubMed] [Google Scholar]
- 14.de Beer, D., P. Stoodley, F. Roe, and Z. Lewandowski. 1994. Effects of biofilm structure on oxygene distribution and mass transport. Biotechnol. Bioeng 43:1131-1138. [DOI] [PubMed] [Google Scholar]
- 15.Donlan, R. M. 2000. Role of biofilms in antimicrobial resistance. ASAIO J. 46:S47-S52. [DOI] [PubMed] [Google Scholar]
- 16.Drenkard, E., and F. M. Ausubel. 2002. Pseudomonas biofilm formation and antibiotic resistance are linked to phenotypic variation. Nature 416:740-743. [DOI] [PubMed] [Google Scholar]
- 17.Hancock, R. E. W., and D. P. Speert. 2000. Antibiotic resistance in Pseudomonas aeruginosa: mechanisms and impact on treatment. Drug Resist. Updates 3:255.. [DOI] [PubMed] [Google Scholar]
- 18.Hoiby, N. 2002. New antimicrobials in the management of cystic fibrosis. J. Antimicrob. Chemother. 49:235-238. [DOI] [PubMed] [Google Scholar]
- 19.Laing, F. P. Y., K. Ramotar, R. R. Read, N. Alfieri, A. Kureishi, E. A. Henderson, and T. J. Louie. 1995. Molecular epidemiology of Xanthomonas maltophilia colonization and infection in the hospital environment. J. Clin. Microbiol. 33:513-518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lang, B. J., S. D. Aaron, W. Ferris, P. C. Hebert, and N. E. MacDonald. 2000. Multiple combination bactericidal antibiotic testing for patients with cystic fibrosis infected with multiresistant strains of Pseudomonas aeruginosa. Am. J. Respir. Crit. Care Med. 162:2241-2245. [DOI] [PubMed] [Google Scholar]
- 21.Miyake, Y., S. Fujiwara, T. Usul, and H. Suginaka. 1992. Simple method for measuring the antibiotic concentration required to kill adherent bacteria. Chemotherapy 38:286-290. [DOI] [PubMed] [Google Scholar]
- 22.National Committee for Clinical Laboratory Standards. 2001. Method for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard M7-A5. NCCLS, Wayne, Pa.
- 23.O'Toole, G., and R. Kolter. 1998. Flagellar and twitching motility are necessary for Pseudomonas aeruginosa biofilm development. Mol. Microbiol. 30:295-304. [DOI] [PubMed] [Google Scholar]
- 24.Regelmann, W., G. Elliott, W. Warwick, and C. Clawson. 1990. Reduction of sputum Pseudomonas aeruginosa density by antibiotics improves lung function in cytic fibrosis more than do bronchodilators and chest physiotherapy alone. Am. Rev. Respir. Dis. 141:914-921. [DOI] [PubMed] [Google Scholar]
- 25.Saiman, L., F. Mehar, W. W. Niu, H. C. Neu, K. J. Shaw, G. Miller, and A. Prince. 1996. Antibiotic susceptibility of multiply resistant Pseudomonas aeruginosa isolated from patients with cystic fibrosis, including candidates for transplantation. Clin. Infect. Dis. 23:532-537. [DOI] [PubMed] [Google Scholar]
- 26.Singh, P. K., A. L. Schaefer, M. R. Parsek, T. O. Moninger, M. J. Welsh, and E. P. Greenberg. 2000. Quorum-sensing signals indicate that cystic fibrosis lungs are infected with bacterial biofilms. Nature 407:762-764. [DOI] [PubMed] [Google Scholar]
- 27.Smith, A. L., C. Doershuk, D. Goldmann, E. Gore, B. Hilman, M. Marks, R. Moss, B. Ramsey, G. Redding, T. Rubio, J. Williams-Warren, R. Wilscott, D. Wilson, and R. Yogen. 1999. Comparison of a β-lactam alone versus β-lactam and an aminoglycoside for pulmonary exacerbation in cystic fibrosis. J. Pediatr. 134:413-421. [DOI] [PubMed] [Google Scholar]
- 28.Spoering, A. L., and K. Lewis. 2001. Biofilms and planktonic cells of Pseudomonas aeruginosa have similar resistance to killing by antimicrobials. J. Bacteriol. 183:6746-6751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stewart, P. S. 1996. Theoretical aspects of antibiotic diffusion into microbial biofilms. Antimicrob. Agents Chemother. 40:2417-2422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stewart, P. S., and J. W. Costerton. 2001. Antibiotic resistance of bacteria in biofilms. Lancet 358:135-138. [DOI] [PubMed] [Google Scholar]
- 31.Tack, K. J., and L. D. Sabath. 1985. Increased minimum inhibitory concentrations with anaerobiasis for tobramycin, gentamicin, and amikacin, compared to latamoxef, piperacillin, chloramphenicol, and clindamycin. Chemotherapy 31:204-210. [DOI] [PubMed] [Google Scholar]
- 32.Tenover, F. C., R. D. Arbeit, and R. V. Goering. 1995. Interpreting chromosomal DNA restriction patterns produced by pulse-field gel electrophoresis: criteria for bacterial stain typing. J. Clin. Microbiol. 33:2233-2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Walter, J., S. Seeney, S. Bell, S. Bowler, P. Masel, and J. McCormack. 2002. Effect of long term treatment with azithromycin on disease parameters in cystic fibrosis: a randomised trial. Thorax 57:212-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Williams, I., W. A. Venables, Lloyd D., F. Paul, and I. Critchley. 1997. The effects of adherence to silicone surfaces on antibiotic susceptibility in Staphylococcus aureus. Microbiology 143:2407-2413. [DOI] [PubMed] [Google Scholar]
- 35.Zimmerli, W., A. F. Widmer, M. Blatter, R. Frei, and P. E. Ochsner. 1998. Role of rifampin for treatment of orthopedic implant-related staphylococal infections. A randomized controlled trial. JAMA 279:1537-1541. [DOI] [PubMed] [Google Scholar]