Abstract
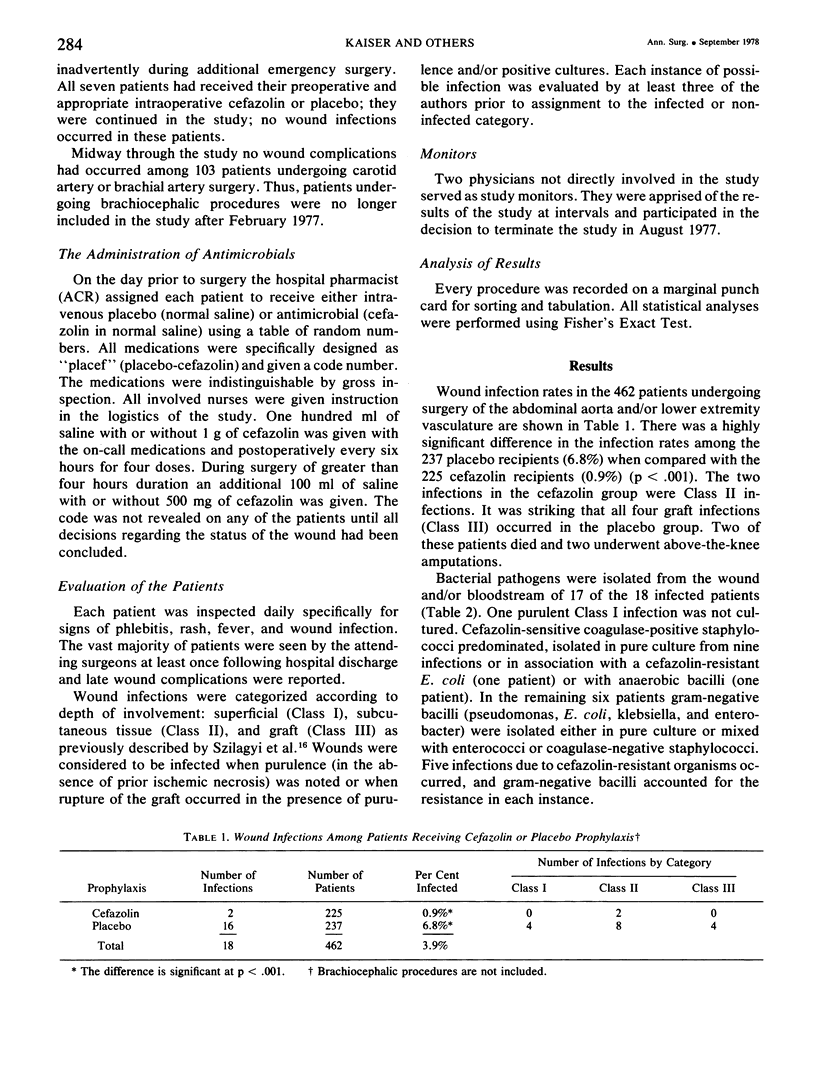
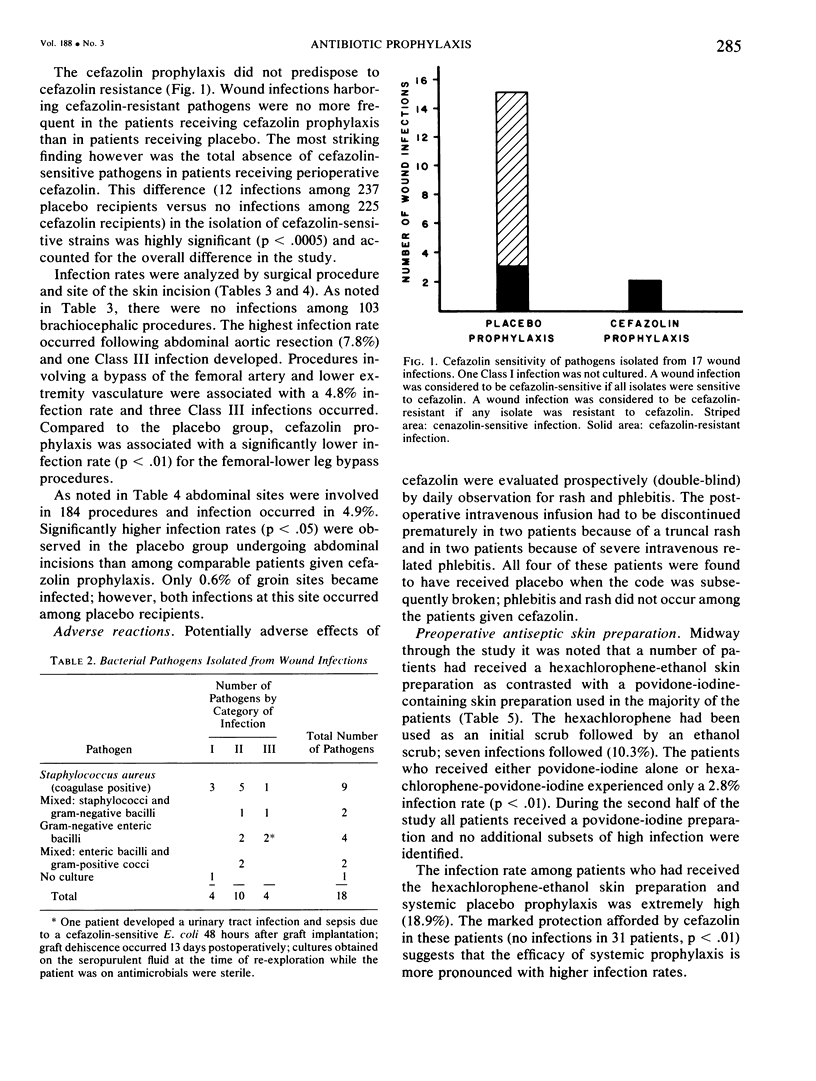
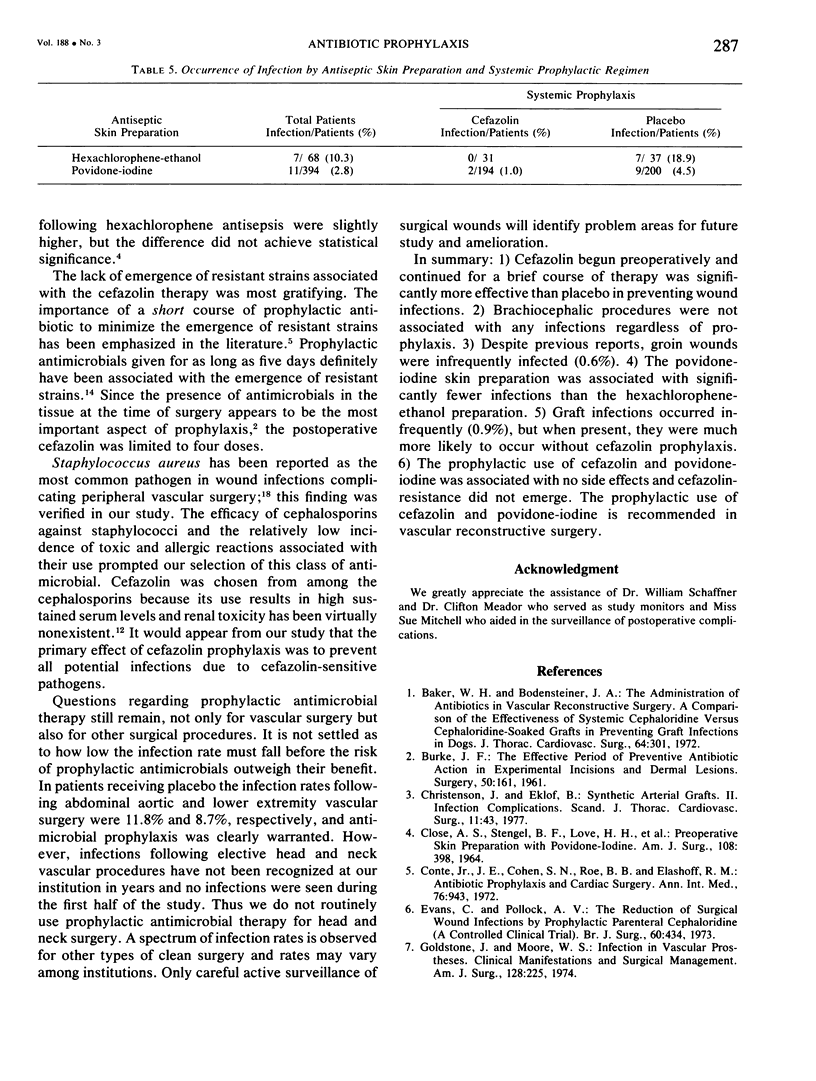
Preoperative and intraoperative antibiotic prophylaxis of infection in peripheral vascular surgery has been widely used although controlled studies have been lacking. A randomized, a prospective, double-blind study of cefazolin versus placebo during 565 arterial reconstructive operations was performed at this hospital from February 1976 through August 1977. Among the 462 patients undergoing surgery of the abdominal aorta and lower extremity vasculature, there was a highly significant difference in the infection rates: 6.8% for placebo recipients versus 0.9% for cefazolin recipients (p less than .001). Of the 18 infections, four involved vascular grafts and all four graft infections occurred in the placebo group. Over 8% of abdominal wounds of patients receiving placebo became infected versus 1.2% of cefazolin patients (p less than .05). Groin wounds were infected infrequently, 1.1% for placebo patients versus none for cefazolin patients. No infections occurred among 103 brachiocephalic procedures. Skin antisepsis was analyzed retrospectively. Infection rates were significantly higher (p less than .01) following hexachlorophene-ethanol versus a povidone-iodine skin preparation. Adverse effects of cefazolin were carefully monitored: no rash, phlebitis, or emergence of resistant strains was observed. A breif perioperative course of cefazolin and povidone-iodine skin antisepsis are recommended in vascular reconstructive surgery of the abdominal aorta and lower extremity vasculature.
Full text
PDF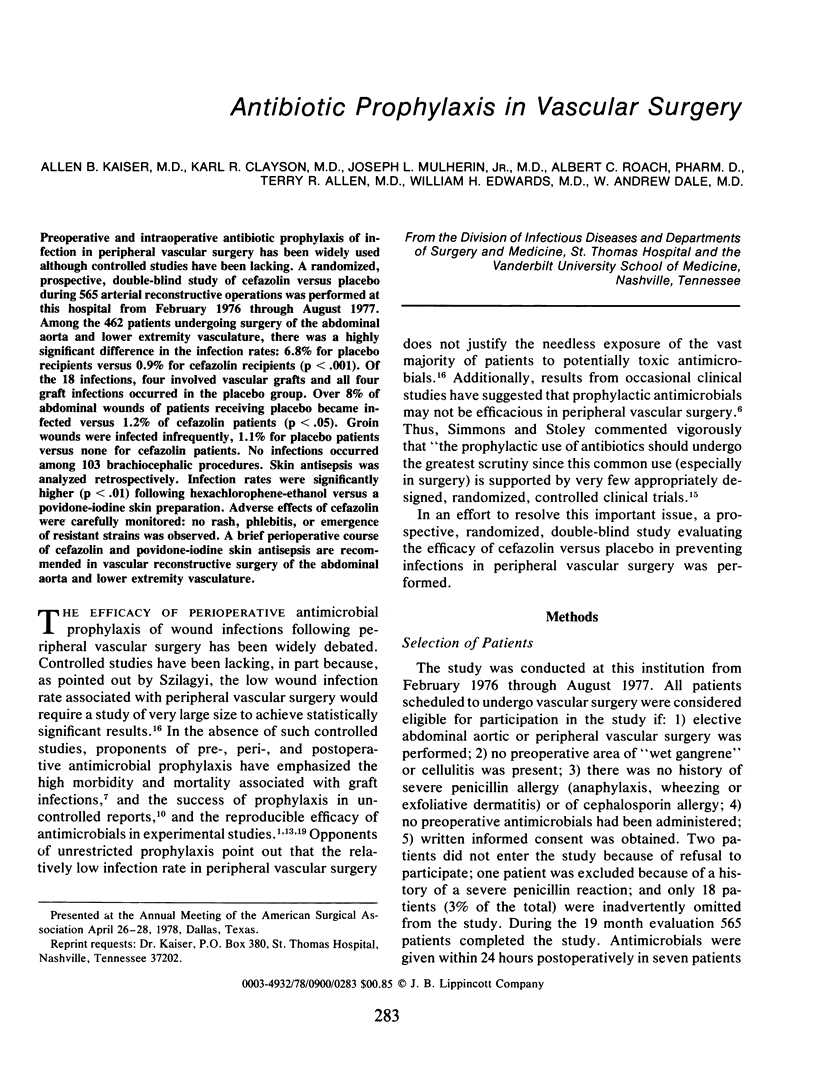

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baker W. H., Bodensteiner J. A. The administration of antibiotics in vascular reconstructive surgery. A comparison of the effectiveness of systemic cephaloridine versus cephaloridine-soaked grafts in preventing graft infections in dogs. J Thorac Cardiovasc Surg. 1972 Aug;64(2):301–303. [PubMed] [Google Scholar]
- Burke J. F. The effective period of preventive antibiotic action in experimental incisions and dermal lesions. Surgery. 1961 Jul;50:161–168. [PubMed] [Google Scholar]
- CLOSE A. S., STENGEL B. F., LOVE H. H., KOCH M. L., SMITH M. B. PREOPERATIVE SKIN PREPARATION WITH POVIDONE-IODINE. Am J Surg. 1964 Sep;108:398–401. [PubMed] [Google Scholar]
- Christenson J., Eklöf B. Synthetic arterial grafts. II. infection complications. Scand J Thorac Cardiovasc Surg. 1977;11(1):43–50. doi: 10.3109/14017437709167812. [DOI] [PubMed] [Google Scholar]
- Conte J. E., Jr, Cohen S. N., Roe B. B., Elashoff R. M. Antibiotic prophylaxis and cardiac surgery. A prospective double-blind comparison of single-dose versus multiple-dose regimens. Ann Intern Med. 1972 Jun;76(6):943–949. doi: 10.7326/0003-4819-76-6-943. [DOI] [PubMed] [Google Scholar]
- Evans C., Pollock A. V. The reduction of surgical wound infections by prophylactic parenteral cephaloridine. A controlled clinical trial. Br J Surg. 1973 Jun;60(6):434–437. doi: 10.1002/bjs.1800600605. [DOI] [PubMed] [Google Scholar]
- Goldstone J., Moore W. S. Infection in vascular prostheses. Clinical manifestations and surgical management. Am J Surg. 1974 Aug;128(2):225–233. doi: 10.1016/0002-9610(74)90097-x. [DOI] [PubMed] [Google Scholar]
- HOFFERT P. W., GENSLER S., HAIMOVICI H. INFECTION COMPLICATING ARTERIAL GRAFTS: PERSONAL EXPERIENCE WITH 12 CASES AND REVIEW OF THE LITERATURE. Arch Surg. 1965 Mar;90:427–435. doi: 10.1001/archsurg.1965.01320090105024. [DOI] [PubMed] [Google Scholar]
- Hunt T. K., Alexander J. W., Burke J. F., MacLean L. D. Antibiotics in surgery. Arch Surg. 1975 Feb;110(2):148–155. doi: 10.1001/archsurg.1975.01360080014002. [DOI] [PubMed] [Google Scholar]
- Lowbury E. J., Lilly H. A., Ayliffe G. A. Preoperative disinfection of surgeons' hands: use of alcoholic solutions and effects of gloves on skin flora. Br Med J. 1974 Nov 16;4(5941):369–372. doi: 10.1136/bmj.4.5941.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madhavan T., Quinn E. L., Freimer E., Fisher E. J., Cox F., Burch K., Pohlod D. Clinical studies of cefazolin and comparison with other cephalosporins. Antimicrob Agents Chemother. 1973 Nov;4(5):525–531. doi: 10.1128/aac.4.5.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore W. S., Rosson C. T., Hall A. D. Effect of prophylactic antibiotics in preventing bacteremic infection of vascular prostheses. Surgery. 1971 Jun;69(6):825–828. [PubMed] [Google Scholar]
- Roberts N. J., Jr, Douglas R. G., Jr Gentamicin use and Pseudomonas and Serratia resistance: effect of a surgical prophylaxis regimen. Antimicrob Agents Chemother. 1978 Feb;13(2):214–220. doi: 10.1128/aac.13.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons H. E., Stolley P. D. This is medical progress? Trends and consequences of antibiotic use in the United States. JAMA. 1974 Mar 4;227(9):1023–1028. doi: 10.1001/jama.227.9.1023. [DOI] [PubMed] [Google Scholar]
- Szilagyi D. E., Smith R. F., Elliott J. P., Vrandecic M. P. Infection in arterial reconstruction with synthetic grafts. Ann Surg. 1972 Sep;176(3):321–333. doi: 10.1097/00000658-197209000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White J. J., Duncan A. The comparative effectiveness of iodophor and hexachlorophene surgical scrub solutions. Surg Gynecol Obstet. 1972 Dec;135(6):890–892. [PubMed] [Google Scholar]
- Willwerth B. M., Waldhausen J. A. Infection of arterial prostheses. Surg Gynecol Obstet. 1974 Sep;139(3):446–452. [PubMed] [Google Scholar]


