Short abstract
The benefits of new methods of prevention of HIV could be jeopardised if they are not accompanied by efforts to change risky behaviour
The recent finding that circumcision of men substantially reduces the risk of HIV infection is one of the most exciting developments in the history of HIV prevention.1 w1 w2 Nevertheless, this finding has quickly been clouded by concerns that risk compensation—increases in risky behaviour sparked by decreases in perceived risk—could undermine circumcision's protective benefits. Similar concerns might also be raised with regard to other promising innovations for HIV prevention. Microbicides, pre-exposure antiretroviral prophylaxis, and vaccines all have the potential to help combat the global spread of HIV but may also inhibit the uptake of safer behaviours by reducing people's perceptions of their risk of infection.
Potential innovations in HIV prevention
New approaches to combat the pandemic are particularly welcome in light of United Nations' estimates that almost five million people become infected with HIV, and more than three million people die of AIDS, each year.w3 Innovations in antiretroviral drug treatment have invigorated international efforts to curb the annual burden of AIDS deaths, but preventing new infections remains the key to breaking the back of the epidemic and curtailing the expanding need for treatment.w3 w4
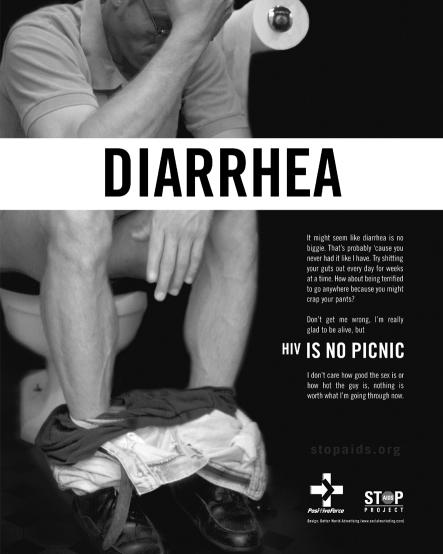
Figure 1.
Raising risk awareness in San Francisco nightclubs
Credit: STOPAIDS
Several innovations show promise for reducing the efficiency of HIV transmission (table).w5 However, for any of these approaches to reduce the rate of new infections, they must reach sufficient numbers of people who are likely to transmit or acquire infection, and their protective benefits must not be offset by increased riskier behaviour in the targeted community.6,7 Of particular concern is the possibility that the introduction of new methods of prevention could reduce perceptions of risk among a broader set of people who are not directly benefiting from these innovations. Some analysts have argued that an over-reliance on technological approaches to HIV infection may dampen people's perceptions of risk and make it more difficult to get them to adopt fundamental preventive behaviours.8-11
Table 1.
Expected risk reduction associated with techniques to prevent HIV infection
| Expected risk reduction (%) | Behavioural considerations | Availability | |
|---|---|---|---|
| Male circumcision1-3w1 w2 w6 w7 | 50-75 | One time procedure | Currently exists |
| Condoms4,5 | 80-90 | Must be used correctly and consistently | Currently exists |
| Microbicides5 | Up to 50 | Must be applied before each sex act | At least 5 years before widely available if current studies show efficacy |
| Pre-exposure antiretroviral prophylaxis (tenofovir)w8 | Unknown | Must take a pill each day | At least 5 years before widely available if current studies show efficacy |
| Vaccines6 | 25-75 | Current vaccine candidates are likely to require multiple doses | At least 10 years before widely available if current studies show efficacy |
Perils of risk compensation
Risk compensation has complicated the introduction of other preventive innovations. Although studies show that seatbelts help protect people in a collision, the evidence is less compelling that the diffusion of seatbelts as a public health measure has contributed to overall reductions in deaths from motor vehicle crashes in some settings.11 This may be because people presume that wearing a seatbelt will protect them from their risky driving.11 Similarly, studies have found an association between use of sunscreen and increased risk of melanoma, related to compensatory increases in exposure to the sun.12
These and other examples have led researchers to suggest that risk compensation may help explain the limited effect of promoting condoms on HIV rates in highly generalised epidemics, as opposed to its clear successes in epidemics that are primarily fuelled by sex work.4,11,13,14 w9 Consistent use of condoms has been shown to reduce the efficiency of transmission of HIV and various other sexually transmitted infections,4,15 but the perception that using condoms can reduce the risk of HIV infection may have contributed to increases in inconsistent use, which has minimal protective effect,4,13 as well as to a possible neglect of the risks of having multiple sexual partners. Thus, the protective effect of promoting condoms may be attenuated at the population level and could even be offset by aggregate increases in risky sexual behaviour.4,11,13,14 w9
Another potentially sobering case in point relates to the increased availability of antiretroviral therapy in the United States, Europe, and Australia. Studies among men who have sex with men,16 w10 w11 injecting drug users,17 and heterosexuals,18 w12 have shown that the mere promise of expanded access to treatment or to post-exposure antiretroviral prophylaxis has been associated with significant increases in risky behaviour.16 A recent meta-analysis of studies on the effects of treatment on preventive behaviour found that although rates of unprotected sex did not differ significantly among those receiving antiretroviral treatment and those who were not, those who perceived that treatment might reduce the risk of HIV transmission had significantly higher rates of risky sex.19 Remarkably, this association was observed among people who were HIV positive and HIV negative, as well as among people with unknown HIV serostatus.19
The notion that people may engage in a kind of unnerving horse trading with respect to their HIV risk has also attracted attention in the popular media. A recent article in the Los Angeles Times reports that 7% of uninfected men surveyed at gay pride events in four US cities had taken an HIV drug before engaging in risky behaviour and that tenofovir is being sold under the table—sometimes together with ecstasy and methamphetamines—at some gay clubs and dance parties as an assumed means of reducing the risk of HIV infection.20
Increases in risk behaviour accompanying the expansion of access to antiretroviral therapy may also have grim effects on HIV treatment initiatives.w13 Recent surveillance data from the United Kingdom estimate that 27% of those infected with HIV in 2000 acquired drug resistant virus, ostensibly by having unprotected sex with HIV infected individuals who had developed resistance while taking antiretroviral therapy.21 As a result, the range of low cost and effective HIV treatment options available to many newly infected individuals may become constrained.
Tackling risk compensation
The prospect of risk compensation should not deter us from pursuing promising methods of prevention or treatment, but it is imperative that we plan ahead to ensure that the benefits will significantly exceed any potentially offsetting limitations. Although microbicides and pre-exposure prophylaxis have already garnered global attention, a relatively small minority of those at risk of infection are likely to benefit from them if and when they are first introduced as it will take some time to achieve widespread distribution. Given that awareness of these new methods may be high while coverage may initially be low, and that risk will not be eliminated even among those receiving the interventions, we must begin to work with service providers, and the communities they serve, to address two basic issues.
Firstly, it is vital to manage potential optimism about innovations in HIV prevention by communicating clearly and broadly that they will not eliminate the risk of HIV infection.w14 Perceptions of personal risk seem to be strongly associated with motivation to adopt behaviour change.22,23 Service providers should therefore promote behaviour change as an integral foundation of their service. Efforts to promote emerging prevention innovations at the community level should clearly identify the limitations of these approaches and should place a strong emphasis on the adoption of safer behaviours.
Secondly, we must build on the successes of Thailand, Cambodia, Uganda, Kenya, Zimbabwe, and other settings to cultivate a deeper appreciation of the fact that behaviour change is a feasible and effective approach to preventing new HIV infections. The continued spread of HIV has resulted in pessimism about changing behaviour, and it is perhaps little appreciated that some existing prevention approaches have been successful in slowing the spread of HIV in some settings.w3 w15 w16 Promotion of condoms seems to have had a key role in reducing infections in high risk groups, and a remarkably consistent element of success across all of these settings seems to have been reductions in sexual partnerships.8,10,15,23,24 w3 w15-w17
A key aspect of Uganda's early success was the collaborative development of a widespread perception that all sexually active people were personally at risk and that changing sexual behaviour was the best way to reduce this risk (box).8,10,23 The experience of Uganda suggests that by working with individuals, leaders, and institutions throughout communities, we can help foster and reinforce shared perceptions that certain risk behaviours are both personally unwise and raise the burden and effects of disease for all. Other settings in which community norms have been changed—for example, regarding the issues of drinking and driving and smoking in public places—may provide useful inspiration.
Conclusion
Emerging innovations may soon supply us with some promising new tools to prevent the spread of HIV. Nevertheless, the complex nature of the HIV pandemic presents us with a challenge that far exceeds the promise of any single prevention approach. The potential for risk compensation highlights the need for a renewed prioritisation and coordination of approaches to change sexual behaviour. From a practical perspective, efforts to maximise the benefits of new and existing risk reducing technologies should also seek to minimise the possibility of risk compensation by sustaining high levels of personal risk perception throughout the communities served. Furthermore, successful approaches to change behaviour must be studied, adapted, and applied with at least the same vigour as the promising host of technological innovations under development.
Seven lessons from Uganda's early response to HIV
Foster a personalisation of risk
Use clear, consistent messages
Combat stigma
Seek out and support indigenous approaches and solutions
Use multiple communication channels
Secure the participation of individuals and organisations throughout society
Reach out to male populations
Summary points
Innovations such as vaccines, microbicides, and male circumcision hold promise to reduce the risk of HIV infection
The perceived reduced risk from such innovations could be compensated for by an increase in risky behaviour
New and existing methods of prevention and treatment must be accompanied by measures to reinforce individuals' perceptions of HIV risk
Programming to change the sexual behaviour will remain fundamental to preventing the spread of HIV
Supplementary Material
 References w1-w17 are on bmj.com
References w1-w17 are on bmj.com
This work does not necessarily represent the views of the United States Agency for International Development. We thank Matthew Barnhart and Gillian Cassell for their useful comments.
Contributors and sources: The authors are all experts in HIV prevention with long experience in the developing world. MMC conceived the paper following discussions with his co-authors and other colleagues about the evolving role of behaviour change in HIV prevention. The other authors contributed importantly in reformulating and revising the paper. MMC is willing to serve as guarantor.
Competing interests: None declared.
References
- 1.Auvert B, Taljaard D, Lagarde E, Tambekou-Sobngwi J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 trial. PLoS Med 2005;2(11): 1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weiss HA, Quigley MA, Hayes RJ. Male circumcision and risk of HIV infection in sub-Saharan Africa: a systematic review and meta-analysis. AIDS 2000;14: 2361-70. [DOI] [PubMed] [Google Scholar]
- 3.Quinn TC, Wawer MJ, Sewankambo N, Serwadda D, Li C, Wabwire-Mangen F, et al. Viral load and heterosexual transmission of human immunodeficiency virus type 1. N Engl J Med 2000;342: 921-9. [DOI] [PubMed] [Google Scholar]
- 4.Hearst N, Chen S. Condom promotion for AIDS prevention in the developing world: is it working? Stud Fam Plann 2004;35: 39-47. [DOI] [PubMed] [Google Scholar]
- 5.Foss AM, Vickerman PT, Heise L, Watts CH. Shifts in condom use following microbicide introduction: should we be concerned? AIDS 2003;17: 1227-37. [DOI] [PubMed] [Google Scholar]
- 6.Gray RH, Li X, Wawer MJ, Gange SJ, Serwadda D, Sewankambo NK. Stochastic simulation of the impact of antiretroviral therapy and HIV vaccines on HIV transmission; Rakai, Uganda. AIDS 2003;17: 1941-51. [DOI] [PubMed] [Google Scholar]
- 7.Blower SM, Ma L, Farmer P, Koenig S. Predicting the impact of antiretrovirals in resource poor settings: preventing HIV infections whilst controlling drug resistance. Curr Drug Targets Infect Disord 2003;3: 345-53. [DOI] [PubMed] [Google Scholar]
- 8.Wilson D. Partner reduction and the prevention of HIV/AIDS: the most effective strategies come from communities. BMJ 2004;328: 848-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allen T, Heald S. HIV/AIDS policy in Africa: What has worked in Uganda and what has failed in Botswana? J Int Dev 2004;16: 1141-54. [Google Scholar]
- 10.Green EC. Rethinking AIDS prevention. Westport, CT: Praeger, 2003.
- 11.Richens J, Imrie J, Copas A. Condoms and seat belts: the parallels and the lessons. Lancet 2000;355: 400-3. [DOI] [PubMed] [Google Scholar]
- 12.Autier P, Dore J, Cattaruzza MS, Renard F, Luther H, Gentiloni-Silverj F, et al. Sunscreen use, wearing clothes, and number of nevi in 6- to 7-year-old European children. J Natl Cancer Inst 1998;90: 1873-80. [DOI] [PubMed] [Google Scholar]
- 13.Ahmed S, Lutalo T, Wawer M, Serwadda D, Sewankambo NK, Nalugoda F, et al. HIV incidence and sexually transmitted disease prevalence associated with condom use: a population study in Rakai, Uganda. AIDS 2001;15: 2171-9. [DOI] [PubMed] [Google Scholar]
- 14.Kajubi P, Kamya M, Kamya S, Chen S, McFarland W, Hearst N. Increasing condom use without reducing HIV risk: results of a controlled community trial in Uganda. J Acquir Immune Defic Syndr 2005;40: 77-82. [DOI] [PubMed] [Google Scholar]
- 15.Halperin DT, Steiner M, Cassell MM, Green EC, Hearst N, Kirby D, et al. The time has come for common ground on preventing sexual transmission of HIV. Lancet 2004;364: 1913-5. [DOI] [PubMed] [Google Scholar]
- 16.Stolte IG, Dukers NHTM, Geskus RB, Coutinho RA, de Wit JBF. Homosexual men change to risky sex when perceiving less threat of HIV/AIDS since availability of highly active antiretroviral therapy: a longitudinal study. AIDS 2004;18: 303-9. [DOI] [PubMed] [Google Scholar]
- 17.Tun W, Celentano DD, Vlahov D, Strathdee SA. Attitudes toward HIV treatments influence unsafe sexual and injection practices among injecting drug users. AIDS 2003;17: 1953-62. [DOI] [PubMed] [Google Scholar]
- 18.Grémy I, Beltzer N. HIV risk and condom use in the adult heterosexual population in France between 1992 and 2001: return to the starting point? AIDS 2004;18: 805-9. [DOI] [PubMed] [Google Scholar]
- 19.Crepaz N, Hart TA, Marks G. Highly active antiretroviral therapy and sexual risk behavior: a meta-analytic review. JAMA 2004;292: 224-36. [DOI] [PubMed] [Google Scholar]
- 20.Costello D. AIDS pill tenofovir as party drug? Los Angeles Times 2005. Dec 19.
- 21.UK Collaborative Group on Monitoring the Transmission of HIV Drug Resistance. Analysis of prevalence of HIV-1 drug resistance in primary infections in the United Kingdom. BMJ 2001;322: 1087-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Glanz K, Rimer BK, Lewis FM, eds. Health behavior and health education: theory, research and practice. 3rd ed. San Francisco, CA: Jossey-Bass, 2002.
- 23.Stoneburner R, Low-Beer D. Population-level HIV declines and behavioral risk avoidance in Uganda. Science 2004;304: 714-8. [DOI] [PubMed] [Google Scholar]
- 24.Shelton JD, Halperin D, Nantulya V, Potts M, Gayle HD, Holmes KK. Partner reduction is crucial for balanced “ABC” approach to HIV prevention. BMJ 2004;328: 891-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.