Abstract
Objective
To assess the effects of an intervention programme designed to increase use of hip protectors in elderly people in nursing homes.
Design
Cluster randomised controlled trial with 18 months of follow up.
Setting
Nursing homes in Hamburg (25 clusters in intervention group; 24 in control group).
Participants
Residents with a high risk of falling (459 in intervention group; 483 in control group).
Intervention
Single education session for nursing staff, who then educated residents; provision of three hip protectors per resident in intervention group. Usual care optimised by brief information to nursing staff about hip protectors and provision of two hip protectors per cluster for demonstration purposes.
Main outcome measure
Incidence of hip fractures.
Results
Mean follow up was 15 months for the intervention group and 14 months for the control group. In total 167 residents in the intervention group and 207 in the control group died or moved away. There were 21 hip fractures in 21 (4.6%) residents in the intervention group and 42 hip fractures in 39 (8.1%) residents in the control group (relative risk 0.57, absolute risk difference −3.5%, 95% confidence interval −7.3% to 0.3%, P=0.072). After adjustment for the cluster randomisation the proportions of fallers who used a hip protector were 68% and 15% respectively (mean difference 53%, 38% to 67%, P=0.0001). There were 39 other fractures in the intervention group and 38 in the control group.
Conclusion
The introduction of a structured education programme and the provision of free hip protectors in nursing homes increases the use of protectors and may reduce the number of hip fractures.
What is already known on this topic
Nursing home residents are at particularly high risk of fracturing a hip
Hip protectors can effectively prevent hip fractures
Adherence to the use of hip protectors is poor
What this study adds
The use of hip protectors in nursing homes can be substantially increased by a single session education targeted at nursing staff and residents and provision of free hip protectors
Increasing the use of hip protectors resulted in a relative reduction of hip fractures of about 40%
Introduction
Hip fractures are a major cause of disability and functional impairment among elderly people.1 Residents in nursing homes are at particularly high risk.2 External hip protectors can effectively reduce the impact of falls and thereby the risk of the hip fracturing. Trials of hip protectors in nursing homes have reported a reduction of 50% in the incidence of hip fracture.3 In general, however, acceptance of hip protectors is poor.3 Adherence will be largely determined by the motivation and competence of staff in nursing homes.4 We developed a two part intervention, consisting of structured theory based education and provision of free equipment, directed at nursing staff and residents to encourage the use of hip protectors. We evaluated whether there were fewer hip fractures among elderly people in nursing homes that received the intervention programme compared with those in nursing homes with optimised usual care.
Participants and methods
Nursing homes and residents
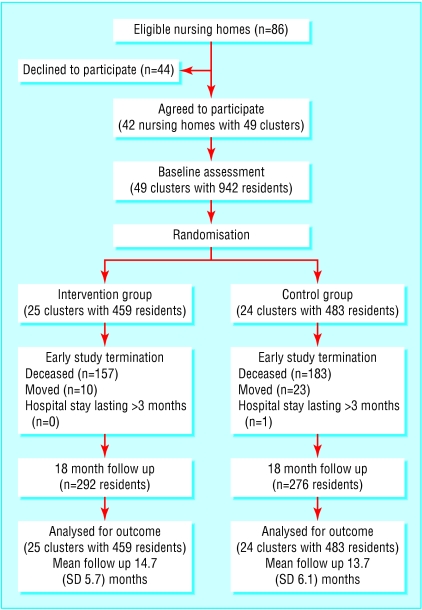
All 86 nursing homes in Hamburg with at least 70 residents were invited and 42 with 49 nursing home clusters agreed to participate (see figure). A cluster was defined as a nursing home by itself or an independently working ward of a large nursing home. Recruitment took place from March to November 1999. In each cluster a study coordinator was nominated. The nursing staff selected 15 to 30 residents according to predefined inclusion criteria: ⩾70 years old, not bedridden, and living in the nursing home for more than three months. Nursing staff collected baseline data supported by the investigators. For description of the functional and cognitive status we used degrees of disablement as assessed by expert raters of the medical service of the German statutory health insurance system (0=none, 1=considerable, 2=severe, 3=most severe).5
Randomisation
We used computer generated randomisation lists for concealed allocation of clusters by external central telephone. To obviate disparate sample sizes we used random permuted blocks of four, six, and ten.
Intervention
Hip protectors are not covered by German health insurance. In homes allocated to usual care (control group) the nominated study coordinator received brief information (10 minutes) about and demonstration of the hip protector, and two hip protectors were provided for demonstration purposes.
In the intervention group we aimed to prevent the number of hip fractures by increasing the use of hip protectors rather than by preventing falls. The intervention consisted of structured education of staff, who then taught residents, and provision of free hip protectors. We provided three hip protectors per resident (Safehip (Tytex, Denmark), the only evaluated hip protector available at the start of the study6).
The development of the programme followed the framework for design and evaluation of complex interventions as suggested by Campbell et al.7 Details of the initial development phases have been published.8 The programme was based on principles of the social learning theory, which considers modelling as a powerful means of transmitting values, attitudes, and patterns of thought and behaviour.9 Self efficacy is posited as a fundamental to behaviour change.10,11 The development of the curriculum followed approaches we have successfully tested for other teaching programmes.12,13
The education session lasted for 60-90 minutes, took place in small groups (average 12 members of staff from each cluster), and was delivered by two investigators. It covered information about the risk of hip fracture and related morbidity; strategies to prevent falls and fractures; effectiveness of hip protectors; relevant aspects known to interfere with the use of protector, such as aesthetics, comfort, fit, and handling; and strategies for successful implementation. The session included experience based, theoretical, and practical aspects. Staff members were encouraged to try wearing the hip protector. Apart from the printed curriculum we also developed and provided 16 coloured flip charts illustrating the main objectives and leaflets for residents, relatives, and physicians.
At least one nurse from each intervention cluster was then responsible for delivering the same education programme to residents individually or in small groups. Nursing staff were encouraged to wear a hip protector during these sessions and to include residents who readily accepted the hip protector as activating group members.
About two weeks later we visited the intervention clusters again to encourage the administration of the programme. Otherwise frequency and intensity of contacts were similar for intervention and control groups.
Study outcomes
Nursing staff used a specially developed documentation sheet on falls to collect outcome variables. We checked data every two months during personal visits. At the end of the study, one investigator and the nominated study coordinator from each cluster reviewed all records to verify the completeness of data.
Our primary outcome variable was hip fracture. Secondary outcome measure was use of hip protectors expressed as the proportion of falls with documented use of the protector and the proportion of fallers with documented use of the protector during at least one fall. Reasons for non-adherence were registered. We also recorded frequency of falls; other fractures related to falls; hospital admissions and consultations with a physician related to falls irrespective of the reason for falls; quality of life; and costs.
Sample size
As a previous randomised trial has shown that use of hip protectors reduces the incidence of hip fracture6 we chose the one sided hypothesis that our intervention would reduce the incidence of hip fracture. Under conditions of usual care the incidence of hip fracture is about 60 per 1000 residents per year.6 We calculated that we would need a sample size of 384 in each group to detect a reduction in relative risk of 50% at α=5% and 80% power. To allow for the methods of analysis required for clusters we increased this number to 477 in each group.14
Statistical methods
We analysed the main outcome “hip fracture” and the variable “other fractures” with χ2 test adjusted for cluster randomisation.14 Though the trial was designed with a one sided hypothesis, to follow statistical convention we report results for two sided 5% tests for the primary outcome and all other variables. The effect of the intervention is expressed as relative risk, difference in absolute risk, and number needed to treat.15 For risk differences we calculated 95% confidence intervals using a method appropriate for cluster randomised trials.16 For all other follow up data we used the cluster as the unit of analysis—that is, we averaged residents' values within clusters and calculated means (SD) of the cluster values within the groups. For statistical comparisons between the groups the Wilcoxon rank sum test was used. P<0.05 was regarded as significant. For computations we used SAS 6.12 and 8.02.
Ethical approval
As the unit of intervention was the cluster we obtained informed consent from all nursing home clusters rather than from residents. The protocol was approved by the ethics committee of the Hamburg chamber of physicians and the regional data protection office.
Results
The figure shows the flow of study clusters and participants through the trial. Baseline characteristics of clusters and residents were similar between the study groups (tables 1 and 2). Data on fractures are summarised in table 3. The relative risk of hip fractures was 0.57 and the absolute risk difference was −3.5%, 95% confidence interval −7.3% to 0.3%, P=0.072; number needed to treat=29 (number needed to treat to benefit 14 to ∞ to number needed to treat to be harmed 350). Frequency of other fractures (table 3) and falls (table 4) were not significantly different between groups. After we adjusted for cluster randomisation hip protectors were used on average by 15% of people who fell in the control group compared with 68% in the intervention group (40/274 v 158/237, P=0.0001) (table 4). There were more hospital admissions related to falls in the control group than in the intervention group (P=0.015), whereas the difference in consultations was not significant (P=0.27) (table 4).
Table 1.
Baseline characteristics of nursing home clusters. Figures are means (SD) unless stated otherwise
| Characteristic
|
Intervention group (n=25)
|
Control group (n=24)
|
|---|---|---|
| Ownership of homes (%): | ||
| State owned | 6 (24) | 4 (17) |
| Non-profit | 14 (56) | 16 (67) |
| Private | 5 (20) | 4 (17) |
| No of residents per home | 137 (72) | 116 (69) |
| Proportion of women | 82 (8) | 84 (10) |
| Proportion of residents according to degree of disablement: | ||
| None | 12 (11) | 10 (11) |
| Considerable | 31 (9) | 28 (10) |
| Severe | 39 (11) | 41 (12) |
| Most severe | 16 (12) | 19 (11) |
| Not available | 2 (5) | 1 (3) |
| No of residents per caregiver | 3.4 (0.8) | 3.3 (1.2) |
| No (%) of homes using hip protectors: | ||
| Any | 6 (24) | 8 (33) |
| For 1 resident | 4 (16) | 3 (13) |
| For 2 or more residents | 2 (8) | 5 (21) |
Table 2.
Baseline characteristics of nursing home residents. Values are numbers (percentage) of residents unless stated otherwise
| Characteristic
|
Intervention group (n=459)
|
Control group (n=483)
|
|---|---|---|
| Women | 405 (88) | 408 (84) |
| Mean (SD) age (years) | 87 (6) | 86 (7) |
| Median (interquartile range) length of residence (months) | 25 (9-52) | 24 (9-51) |
| Degrees of disablement: | ||
| None | 13 (3) | 19 (4) |
| Considerable | 173 (38) | 161 (33) |
| Severe | 218 (47) | 242 (50) |
| Most severe | 44 (10) | 58 (12) |
| Not available | 11 (2) | 3 (1) |
| Urinary incontinence | 321 (70) | 370 (77) |
| Indwelling catheter | 13 (3) | 8 (2) |
| Use walking aid | 345 (75) | 346 (72) |
| Falls during preceding 12 months: | ||
| Any | 347 (76) | 344 (71) |
| Not available | 17 (4) | 10 (2) |
| Falls during preceding 4 weeks: | ||
| Any | 158 (34) | 133 (28) |
| 1 fall | 74 (16) | 58 (12) |
| ⩾2 falls | 84 (18) | 75 (16) |
| History of hip fracture: | ||
| Any | 117 (25) | 106 (22) |
| Not available | 14 (3) | 8 (2) |
| Other fractures during preceding 12 months: | ||
| Any | 52 (11) | 48 (10) |
| Not available | 16 (3) | 12 (2) |
Table 3.
Fracture data
| Intervention group (n=459)*
|
Control group (n=483)†
|
Relative risk
|
Absolute risk difference‡ (95% CI§)
|
P value§ (adjusted χ2 test)
|
|
|---|---|---|---|---|---|
| No of hip fractures | 21 | 42 | — | — | — |
| No (%) of residents with hip fractures | 21 (4.6) | 39 (8.1) | 0.57 | −3.5% (−7.3% to 0.3%) | 0.072 |
| No of other fractures | 39 | 38 | — | — | — |
| No (%) of residents with other fractures | 35 (7.6) | 32 (6.6) | 1.15 | 1.0% (−4.0% to 6.0%) | 0.695 |
Mean follow up 15 months.
Mean follow up 14 months.
Intervention minus control.
Calculated according to methods of Donner and Klar,14 16 which take cluster randomisation into account.
Table 4.
Falls, use of hip protectors, and medical attention related to falls during study period. Values are means (SD) unless stated otherwise
| Variables
|
Intervention group (25 clusters, 459 residents)
|
Control group (24 clusters, 483 residents)
|
Mean difference between groups* (95% CI)†
|
P value† (Wilcoxon rank sum test)
|
|---|---|---|---|---|
| Fallers and falls‡ | ||||
| Residents with ⩾1 fall | 237 | 274 | ||
| Proportion of fallers | 0.50 (0.20) | 0.56 (0.16) | −0.06 (−0.16 to 0.05) | 0.32 |
| No of falls | 946 | 1409 | ||
| Falls per resident | 1.99 (1.53) | 2.79 (2.07) | −0.80 (−1.85 to 0.24) | 0.14 |
| Falls per resident per month | 0.17 (0.13) | 0.22 (0.15) | −0.05 (−0.13 to 0.03) | 0.23 |
| Use of hip protectors | ||||
| Residents who used hip protector | 158/459 (34%) | 40/483 (8%) | ||
| Proportion of residents who used hip protector | 0.35 (0.21) | 0.08 (0.12) | 0.27 (0.17 to 0.36) | <0.0001 |
| Fallers who used hip protector | 158/237 (67%) | 40/274 (15%) | ||
| Proportion of fallers who used hip protector | 0.68 (0.26) | 0.15 (0.25) | 0.53 (0.38 to 0.67) | <0.0001 |
| Falls in which hip protector was used | 552/946 (58%) | 160/1409 (11%) | ||
| Proportion of falls in which hip protector was used | 0.54 (0.25) | 0.08 (0.15) | 0.46 (0.34 to 0.59) | <0.0001 |
| Medical attention related to falls | ||||
| Residents with ⩾1 hospital admission | 96 | 135 | ||
| No of admissions | 121 | 211 | ||
| Admissions per resident | 0.26 (0.16) | 0.46 (0.33) | −0.20 (−0.35 to −0.05) | 0.015 |
| Admissions per faller | 0.58 (0.37) | 0.81 (0.54) | −0.23 (−0.50 to 0.04) | 0.12 |
| Residents with ⩾1 consultation with physician | 93 | 119 | ||
| No of consultations | 117 | 234 | ||
| Consultations per resident | 0.25 (0.16) | 0.47 (0.55) | −0.22 (−0.45 to 0.01) | 0.27 |
| Consultations per faller | 0.51 (0.25) | 0.81 (0.96) | −0.30 (−0.70 to 0.10) | 0.61 |
Intervention minus control.
Confidence intervals and P values calculated on basis of data summarised at cluster level.
Fall data of one control cluster with 15 residents not available.
In the intervention group there were four cases of hip fracture with reported use of the hip protector. However, we could not determine whether a hip protector was being used at the time because of incomplete records or because staff or relatives refused to allow further inquiries. The most common reason for non-adherence in the intervention group was that residents declined to use the protector (249 of 394 unprotected falls).
Discussion
We have shown that the use of hip protectors can be substantially increased among residents in nursing homes, resulting in a relative reduction of hip fractures of more than 40% at borderline significance. The intervention comprised structured education of nursing staff, encouragement of residents to use the protector, and provision of hip protectors free of charge.
It is difficult to compare adherence to the use of hip protectors across studies.6,17–22 There is no generally accepted definition of adherence, and methods of assessment differ. The most valid method would be to observe the use of hip protectors during unscheduled visits, but in a pilot study this turned out to be unfeasible.8 Often residents were not present or members of staff were too busy to spend time answering questions. Preselection of participants is a further source of variance in adherence. Kannus et al included only residents who agreed to wear the protector.19 They reported that in 74% of falls the hip protector had been worn. In our study the programme was offered to all eligible residents in those homes allocated to the intervention group. This approach resulted in the use of protectors during 54% of falls compared with 8% in the control group (proportions adjusted for cluster randomisation). Lauritzen et al found a compliance rate of 24% associated with a 56% reduction in hip fractures.6 This finding was explained by a preferential use of the protector by residents at the highest risk and with the highest possible benefit. Thus, an increase in compliance may not necessarily relate to an equivalent decrease in fractures. On the other hand, it is likely that even the limited use of hip protectors in the control group of the present study was effective in preventing hip fractures. In other studies people in control groups did not use hip protectors.6,17–21 Thus, the relative risk reduction in hip fractures might have been more pronounced in our study if hip protectors had been unavailable in the control group.
The apparent benefit of a lower rate of hospital admissions related to falls in the intervention group should not be overinterpreted, as there was a trend of fewer falls in the intervention group that remains open to various explanations.
The present study has several strengths. To avoid violation of randomisation and selection bias we did not exclude participants who declined to use the hip protector. In contrast, Kannus et al excluded 31% of participants who were assigned to the hip protector group but who declined to participate after randomisation, and people who dropped out were replaced from a “waiting list.”19 In contrast with former studies6,17,20,21 we used properly concealed allocation. Cluster randomisation was essential because the intervention programme relied on changes to nursing techniques. We also recruited a large number of clusters and performed statistical analyses taking cluster randomisation into account.
In conclusion, we have shown that a structured education programme and provision of free hip protectors can increase use. Long term implementation of the intervention requires the provision of hip protectors on prescription for elderly people at high risk of hip fracture.
Figure.
Flow of nursing home clusters and participants through trial
Acknowledgments
We thank the study coordinators, nursing staff, and participating residents of 49 nursing home clusters in Hamburg; Hubert Overmann, University Düsseldorf, for the external allocation of clusters; and Anke Delakowitz and Brigitte Gerloff for assistance in data collection and administration.
Footnotes
Funding: Public Health Research Network Northern Germany (project TP III-1). Rölke Pharma (Hamburg, Germany) provided the hip protectors for this study and has given a grant to the University of Hamburg.
Competing interests: AW was formerly an employee and is at present a consultant of Rölke Pharma, the German distributor of Safehip. AW and GM have received travel grants from Rölke Pharma.
References
- 1.Keene GS, Parker MJ, Pryor GA. Mortality and morbidity after hip fractures. BMJ. 1993;307:1248–1250. doi: 10.1136/bmj.307.6914.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cumming RG. Nursing home residence and risk of hip fracture. Am J Epidemiol. 1996;143:1191–1194. doi: 10.1093/oxfordjournals.aje.a008706. [DOI] [PubMed] [Google Scholar]
- 3. Parker MJ, Gillespie LD, Gillespie WJ. Hip protectors for preventing hip fractures in the elderly. Cochrane Database Syst Rev 2002;4:CD001255. [DOI] [PubMed]
- 4.Cameron ID. Hip protectors. Prevent fractures but adherence is a problem. BMJ. 2002;324:375–376. doi: 10.1136/bmj.324.7334.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dalichau G, Grüner H, Müller-Alten L. SGB XI - Pflegeversicherung. Kommentar und Rechtssammlung [ SGB XI—Statutory care insurance. Comment and collection of statutes]. Starnberg: RS Schulz; 2002. [Google Scholar]
- 6.Lauritzen JB, Petersen MM, Lund B. Effect of external hip protectors on hip fractures. Lancet. 1993;341:11–13. doi: 10.1016/0140-6736(93)92480-h. [DOI] [PubMed] [Google Scholar]
- 7.Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, et al. Framework for design and evaluation of complex interventions to improve health. BMJ. 2000;321:694–696. doi: 10.1136/bmj.321.7262.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Warnke A. Prävention von Hüftgelenksfrakturen durch externen Hüftschutz. Entwicklung, Evaluation und Implementierung eines strukturierten Informationsprogramms [Prevention of hip joint fractures through external hip protectors. Development, evaluation, and implementation of a structured information programme]. Hamburg: University of Hamburg; 2002 (PhD dissertation).
- 9.Bandura A. Social learning theory. Englewood Cliffs, NJ: Prentice-Hall; 1977. [Google Scholar]
- 10.Bandura A. Self-efficacy: the exercise of control. New York: Freeman; 1997. [Google Scholar]
- 11.Clark NM, Dodge JA. Exploring self-efficacy as a predictor of disease management. Health Educ Behav. 1999;26:72–89. doi: 10.1177/109019819902600107. [DOI] [PubMed] [Google Scholar]
- 12.Kronsbein P, Mühlhauser I, Venhaus A, Jörgens V, Scholz V, Berger M. Evaluation of a structured treatment and teaching programme on non-insulin-dependent diabetes. Lancet. 1988;ii:1407–1411. doi: 10.1016/s0140-6736(88)90595-8. [DOI] [PubMed] [Google Scholar]
- 13.Mühlhauser I. Verbesserung der Behandlungsqualität der chronischen Krankheiten Diabetes mellitus, arterielle Hypertonie und Asthma bronchiale durch strukturierte Therapie- und Schulungsprogramme [ Improvement of the quality of treatment of the chronic diseases diabetes mellitus, arterial hypertension, and bronchial asthma through structured treatment and training programmes]. Munich: Urban und Schwarzenberg; 1993. [Google Scholar]
- 14.Donner A, Klar N. Methods for comparing event rates in intervention studies when the unit of allocation is a cluster. Am J Epidemiol. 1994;140:279–289. doi: 10.1093/oxfordjournals.aje.a117247. [DOI] [PubMed] [Google Scholar]
- 15.Altman DG. Confidence intervals for the number needed to treat. BMJ. 1998;317:1309–1312. doi: 10.1136/bmj.317.7168.1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Donner A, Klar N. Confidence interval construction for effect measures arising from cluster randomization trials. J Clin Epidemiol. 1993;46:123–131. doi: 10.1016/0895-4356(93)90050-b. [DOI] [PubMed] [Google Scholar]
- 17.Ekman A, Mallmin H, Michaelsson K, Ljunghall S. External hip protectors to prevent osteoporotic hip fractures. Lancet. 1997;350:563–564. doi: 10.1016/S0140-6736(05)63140-6. [DOI] [PubMed] [Google Scholar]
- 18.Cameron ID, Venman J, Kurrle SE, Lockwood K, Birks C, Cumming RG, et al. Hip protectors in aged-care facilities: a randomized trial of use by individual higher-risk residents. Age Ageing. 2001;30:477–481. doi: 10.1093/ageing/30.6.477. [DOI] [PubMed] [Google Scholar]
- 19.Kannus P, Parkkari J, Niemi S, Pasanen M, Palvanen M, Järvinen M, et al. Prevention of hip fracture in elderly people with use of a hip protector. N Engl J Med. 2000;343:1506–1513. doi: 10.1056/NEJM200011233432101. [DOI] [PubMed] [Google Scholar]
- 20.Chan DK, Hillier G, Coore M, Cooke R, Monk R, Mills J, et al. Effectiveness and acceptability of a newly designed hip protector: a pilot study. Arch Gerontol Geriatr. 2000;30:25–34. doi: 10.1016/s0167-4943(99)00048-5. [DOI] [PubMed] [Google Scholar]
- 21.Villar MTA, Hill P, Inskip H, Thompson P, Cooper C. Will elderly rest home residents wear hip protectors? Age Ageing. 1998;27:195–198. doi: 10.1093/ageing/27.2.195. [DOI] [PubMed] [Google Scholar]
- 22.Parkkari J, Heikkilä J, Kannus P. Acceptability and compliance with wearing energy-shunting hip protectors: a 6-month prospective follow-up in a Finnish nursing home. Age Ageing. 1998;27:225–229. doi: 10.1093/ageing/27.2.225. [DOI] [PubMed] [Google Scholar]