Abstract
Background
Abdominal tuberculosis (TB) is endemic in the developing world and is reemerging in the West. Since computed tomography (CT) has the ability to demonstrate changes in the peritonium, mesentry, lymphnodes, bowel and solid organs and is being increasingly used for primary evaluation of abdominal conditions, it is important to be familiar with the CT features of the disease.
Methods
CT findings were retrospectively analysed in 49 patients with proved abdominal TB. Patients with genitourinary TB and with AIDS/HIV were not included in the study.
Results
Peritoneal involvement was the most common feature (77.5%) with ascites (wet peritonitis) seen in more than half the cases (55.2%). The rest showed peritoneal, mesenteric or omental thickening or mass formation but no ascites (dry peritonitis). Other findings included lymphadenopathy (46.9% mainly of diffuse nature, bowel wall thickening (38%) and solid organ involvement (20.4%).
Conclusions
CT reliably demonstrates the entire range of findings which need interpretation in the light of clinical and laboratory data.
Background
Tuberculosis (TB) is a re emerging global emergency which is further complicated by AIDS/HIV infection and the use of immunosuppressant drugs [1]. The disease may involve any body system and in the abdomen it can mimic many conditions, like inflammatory bowel disease, malignancy and other infectious diseases [2-4]. Untreated or delayed treatment can result in life long morbid complications. It is therefore necessary to recognize the disease early and initiate treatment for this curable disease. Abdominal TB may present varying imaging features depending upon the organs involved. CT offers the unique ability to image the entire abdominal structures in a single examination and is widely available. It is therefore important to be familiar with the CT features of the disease and its complications. Our retrospective study describes the CT features of abdominal TB in 49 proven cases.
Methods
Between April 1982 and February 2002, 49 consecutive patients with proven abdominal TB who had CT scans of the abdomen as part of their diagnostic work up were reviewed. There were 37 males and 12 females, with age range of 10 to 78 years (mean age 35.27 years). The scans were independently reviewed by 2 radiologists and any disagreement in findings was resolved by combine review of the scans and a consensus reached. The diagnosis was established on the basis of at least one of the following criteria:
a) Histological evidence of caseating granuloma.
b) Histological demonstration of acid fast bacilli in the lesion or ascetic fluid.
c) Growth of mycobacterium tuberculosis on culture of tissue or ascetic fluid.
d) Satisfactory therapeutic response to chemotherapy in patients with clinical, radiological and operative evidence of abdominal tuberculosis.
The case records were analysed according to age, sex, nationality clinical presentation and CT findings. Immunocompromised and AIDS/HIV patients were not included in the study. Genitourinary TB was also excluded except in those cases with co-existing abdominal lymphadenopathy.
Results
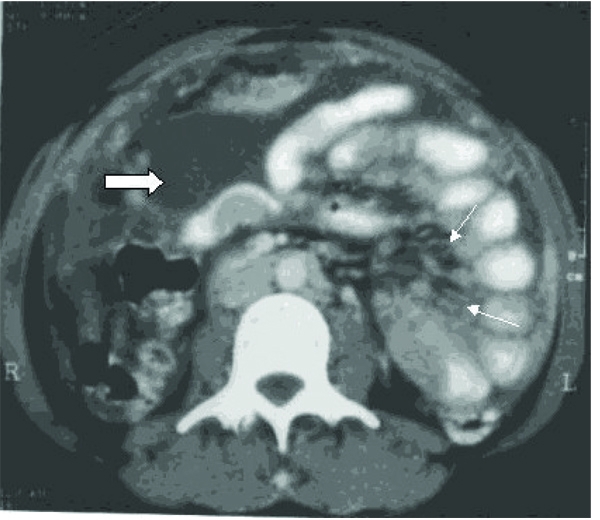
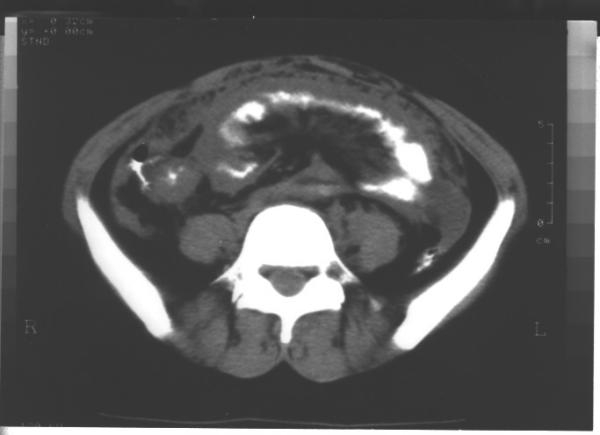
The majority (63.26%) of the patients were non-Kuwaitis. The symptoms of these patients on presentation are shown in Table 1. The common sites of involvement are shown in table 2. CT analysis of the pattern of abdominal TB revealed peritoneal involvement in 38/49 (77.5%) cases and was classified as "wet peritonitis" defined as free or loculated ascites of large or small volume, depending upon the depth of ascites (whether more or less than 3 cm respectively; Figs 1 &2) or "dry peritonitis" represented by peritoneal mesenteric or omental thickening or mass but without ascites (Fig 3). Wet peritonitis [21/38 cases (52.3%)] and the the "dry" type [17/38 (45.7%)] were both commonly seen. The details regarding the "free" and "loculated" nature and the volume of ascites (i.e. small or large), is shown in table 3. The pattern of mesenteric and omental disease with or without ascites revealed that stranding of the mesenteric fat (18 cases; 47.3%) and omental thickening (9 cases; 23.6%) (Fig 3 and Fig 4) was more common than mesenteric or omental mass (3 cases; 7.8%) Fig. 1.
Table 1.
| Symptoms | No. of patients n = 49 |
| Abdominal pain: | 37 (75.5%) |
| Fever: | 32 (65.3%) |
| Weight loss: | 18 (36.7%) |
| Vomiting: | 7 (14.2%) |
| Abdominal mass: | 5 (10.2%) |
| Diarrhoea: | 1 (2.0%) |
| Acute Abdominal pain: | 1 (2.0%) |
| Pneumaturia: | 1 (2.0%) |
| * Convulsions: | 1 (2.0%) |
* This patient had intracranial tuberculomas. A lower abdominal tubercular mass was diagnosed on routine examination.
Table 2.
Summary of CT Findings n = 49
| Peritonitis (Mesentry, omental and peritoneal disease): | 38 (77.5%) |
| Lymph nodes: | 23 (46.9%) |
| G.I.T: | 19 (38.7%) |
| Solid organ involvement: | 10 (20.4%) |
Figure 1.
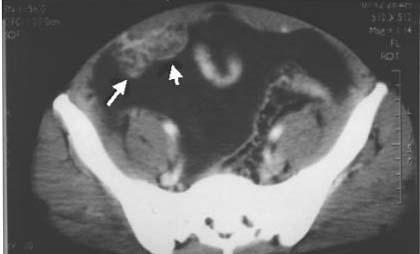
Wet peritonitis: CT scan of the pelvis showing large volume free ascites. Note omental mass (arrows).
Figure 2.
Wet peritonitis: CT scan mid-abdomen showing small volume loculated ascites (thick arrow) Note mesenteric strands and mesenteric nodes (thin arrow). Peritoneal thickening is seen in the right side.
Figure 3.
Dry peritonitis: CT scan showing diffuse mesenteric strands, mesenteric nodes and omental thickening.
Table 3.
CT features of Peritoneal TB (n = 38; wet = 21; dry = 17)
| Ascites + Mesenteric and/or omental disease n = 13 | Ascites only n = 8 | ||||||
| Free | Loculated | Free | Loculated | ||||
| LV | SV | LV | SV | LV | SV | LV | SV |
| 3 | 2 | 6 | 2 | 5 | 1 | 1 | 1 |
LV = large volume; SV = small volume
Figure 4.
Circumferencial thickening of the caecum and narrowing of the terminal ilium. Also note mesenteric strands and omental thickening.
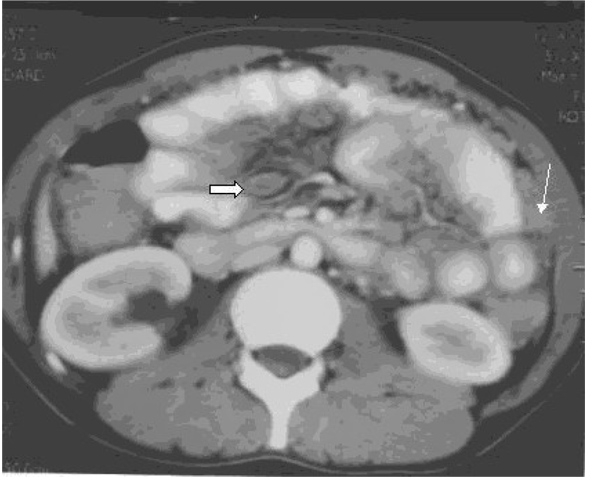
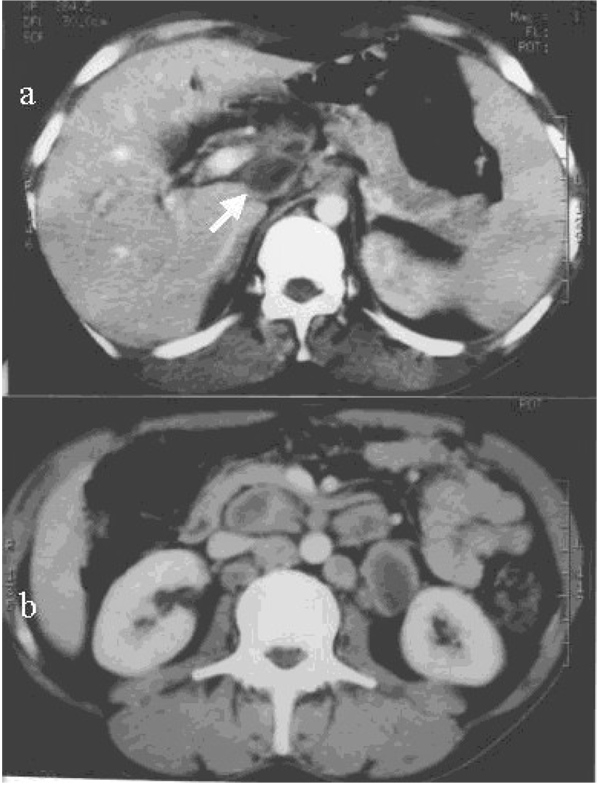
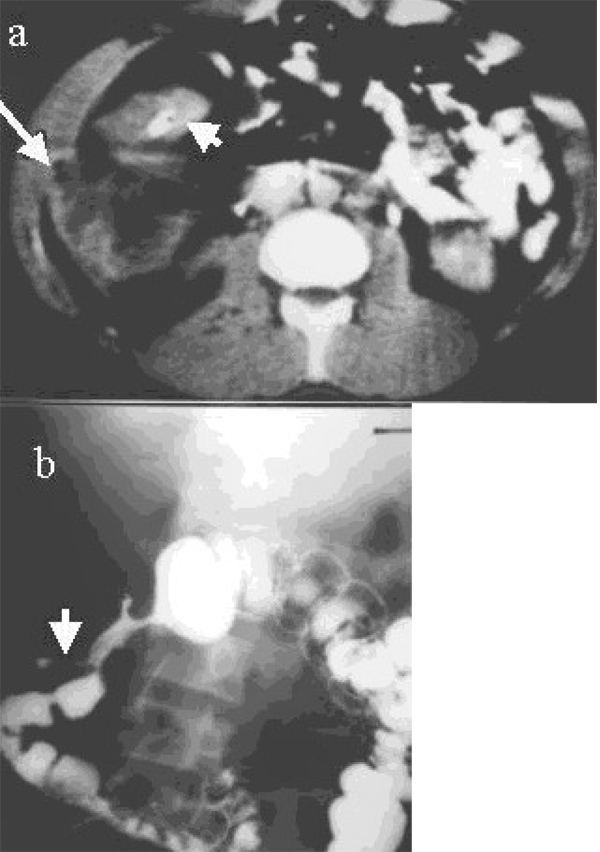
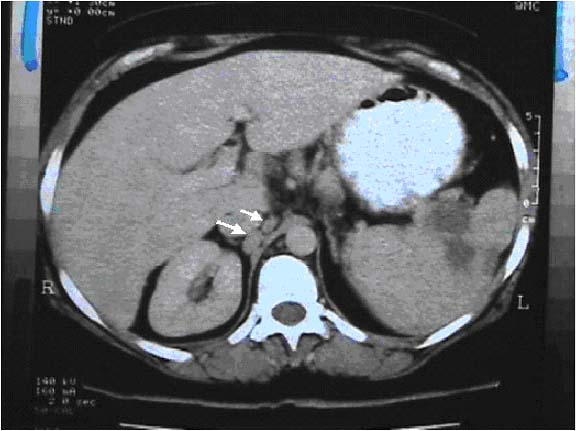
Lymphnode involvement was detected in 23/49 (46.9%) patients of whom 11 cases (47.8%) had diffuse involvement throughout the abdomen [Fig. 5]. Localised or regional adenopathy was seen in several sites including mesentric (6/23; 26%) peripancreatic/portal (3/23, 13%) and para aortic (3/23; 13%) (Table 4). GIT disease was noted in 19/49 (38.7%) cases. Majority of the cases (17/20; 86.8%) involved the small bowel, with or without the caecum. (Table 5) showing strictures and thickening of the bowel wall [Figs. 4 &6]. Isolated large bowel disease was less frequent (2/19 cases; 10.5%). Perforation of the gut was seen in 3 cases, 2 of the large bowel leading to a parietal abscess in 1 patient [Fig. 6] and hydropneumo-peritomium in the other. The third case was a perforating tuberculous gastric ulcer, resulting in an inflammatory mass of the lesser sac and the pancreas [Fig. 7]. Vesico-colic fistula was seen in 1 case. The solid organ disease occurred in 10/49 cases (20.4%) and the distribution is shown in Table 6. The liver and spleen involvement was seen as multi focal hypodense lesions [Fig. 8 and Fig. 9] where as the pancreas showed focal absecess, one of which was due to direct involvement from perforating TB gastric ulcer [Fig. 7]. A combination of these findings was seen in 21/49 cases (42,8 %) involving more than one system in varying combination.
Figure 5.
Necrotic lymph nodes with lucent center seen in the (a) portal/peri pancreatic region (arrow) and (b) para-aortic area.
Table 4.
Distribution of Lymph nodes (n = 23)
| Diffuse (Peripancreatic ± Mesentric ± paraaortic) | 11 (48%) |
| Mesentric: | 6 (26%) |
| Peripancreatic/Portal: | 3 (13%) |
| Para aortic: | 3 (13%) |
Table 5.
GIT Tuberculosis (n = 20)
| Ileocecal and distal ileum: | 10 (50%) |
| Small bowel: | 7 (36.8%) |
| Large bowel: | 2(10.5%) |
| Stomach (ulcer): | 1 (5.2%) |
| * Perforation: | 2 |
| * Fistulae: | 1 |
Figure 6.
(a) CT scan showing circumferential thickening of the ascending colon (short arrow). Note right parietal abscess with free air (long arrow). (b) This was due to a fistula (arrow) of the ascending colon confirmed by barium enema.
Figure 7.

CT of the upper abdomen showing large necrotic inflammatory mass in the lesser sac and involving the pancreas. This was due to perforating gastric TB ulcer.
Table 6.
Solid Organ Involvement (n = 10)
| Spleen: | 3 (30%) |
| Liver: | 2 (20%) |
| Liver + Spleen: | 2 (20%) |
| Pancreas: | 2 (20%) |
| Kidneys*: | 1 (10%) |
*This patient with abdominal lympadenopathy had coexistent kidney disease.
Figure 8.

CT of the upper abdomen showing multiple focal hypodense lesions in the liver.
Figure 9.
CT of the upper abdomen focal lesions in the spleen. Note associated para aortic nodes (arrows).
Discussion
The causative organism for abdominal TB is usually mycobacterium tuberculosis or mycobacterium avium – intracellularie, the latter being more common in immuno-compromised hosts [5]. Abdominal TB is usually caused by injestion of bacilli in infected sputum or contaminated food. The bacilli cause caseation necrosis in the intestine, followed by spread to the mesenteric lymph nodes that may rupture into the peritoneum causing TB peritonitis [6-8]. Another mechanism behind is the hematogenous spread of the bacilli from localized foci of recent or old infection [9,10].
Peritoneal TB is the most common form of abdominal TB and involves alone or in combination the peritoneal cavity, mesentry and omentum. Three types of peritoneal TB are described [7,11]. A wet type with ascites or pockets of loculated fluid; a dry type with bulky mesenteric thickening and lymph adenopathy; and a third type with mass formation due to omental thickening which may be mistaken for a tumour. In our series, peritonitis was equally likely to be either of the wet or dry type and the ascites (both free and loculated) was more commonly large volume. Isolated omental disease was not seen in any of our cases, though the omentum was involved in a vast majority of our cases in combination with other features of the disease. Ascites in abdominal TB can be due to an earlier transudate stage of immune reaction or due to late cell mediated immunity when the fluid is complex with strands, septation and debris [9]. Unlike US the complex nature of the ascites is difficult to demonstrate by CT, [12] however CT is useful in determining the density of the ascitic fluid which is reported to be high; presumably due to the complex nature of the fluid. The high density nature of the fluid is reported by some authors [13,14] as specific for TB where as other [15] suggest that it is not a reliable factor and can overlap with peritoneal carcinomatosis. The differential diagnosis of complex ascites includes wide spread lymphoma and carcinomatous as well as pyogenic peritonitis [14]. Mesenteric disease is an important and common manifestation of early stage abdominal TB [16]. The mesentery is initially thickened with a few discrete lymph nodes interspersed within it and, the later stage mesenteric disease represents irregular inflammatory masses of caseating lymph nodes [16]. CT offers the distinct advantage of demonstrating these features unlike US where the bowel gas may prevent adequate visualization of the mesentry [17].
Abdominal lymph adenopathy commonly involves mesenteric, portal and peripancreatic sites reflecting the lymphatic drainage of the small bowel [5]. The retroperitoneal lymph nodes are relatively spared [16] and their involvement rarely occurs in isolation. In disseminated TB however diffuse lymphadenopathy without prelidiction to any site may be seen, though the retroperitoneal node's size is out of proportion to the lymph adenopathy elsewhere in the abdomen [6]. The nodes are usually matted together with hypodence centers which probably is due to caseation and many occasionally contain calcification [18,19]. Lymphnode enlargement is non specific and occurs in metastatic disease, lymphoma Whipple's disease and pyogenic infection [20]. In our series 47% of patients had a lympadenopathy pattern similar to that reported by others [6]. Central necrosis with rim enhancement, though not pathognomonic, is a useful sign and readily seen in the current generation of CT scanners.
The commonest sites of gastro intestinal tract TB are terminal ileum and cecum [21-24]. Other sites in which the disease occurs are, in descending order of frequency, the ileum, cecum, ascending colon, jejunum, other parts of colon, rectum, duodenum and stomach [25]. GIT TB may be ulcerative type, hyperplastic type or a combination of the two. The ileo-cecal TB is often hyperplastic type [26]. In early stage disease a few regional nodes and circumferencial thickening of the wall of the cecum and terminal ileum are seen. In later stages of the disease the ileocecal value and adjacent medial wall of the cecum are predominently and symmetrically thickened. These changes are however nonspecific and may also be seen in cecal carcinoma, Crohn's disease, lymphoma and amebiasis. In advanced ileocecal disease gross wall thickening, adherent small bowel loops, large regional lymphnodes and exophytic mesenteric thickening together from a complex mass of varied density, which is characteristic of CT appearance of TB and is reproted to be seen in 45% of the cases [22]. Isolated colonic, duodenal and gastric TB are rare [25]. There was one case of gastric TB in our study. Although mucosal changes are best evaluated by barium examinations, evidence of extramucosal disease is both indirect and incomplete and CT is valuable in evaluating directly the extramucosal component of the disease.
Visceral TB is rarely seen in isolation and is more frequently part of multifocal or disseminated disease [9,11,27,28]. Liver and spleen are the main organs involved and their involvement can occur in the form of micro abscesses in miliary TB, pattern represented by CT as diffuse low density focal lesions, or in the form of larger abscesses [29,30]. Often the only feature of visceral TB is organomegaly with calcified granulomas visible in the late stage disease or after healing. Pancreatic TB is rare and may result from either hematogenous dissemination or direct spread of the disease from adjacent nodes. There were 2 cases of pancreatic TB in our series, one of them was due to direct spread from a penetrating tuberculous gastric ulcer. Two more cases of perforations of large bowel was seen in our study, one in the ascending colon presenting as a parietal abscess and other in the colon leading to hydropneumoperitonim and peritonitis. One case of vesico-colic fistula was also seen which presented as pneumoturia.
Conclusions
Manifestations of TB in the abdomen are variable. CT reliably demonstrates the entire range of findings. Although no single CT feature is diagnostic of the disease, CT findings, interpreted in the light of clinical and laboratory data can be a valuable tool in the diagnosis of abdominal tuberculosis.
Competing interest
None declared
Author's contributions
Authors TS and MS contributed case material from Mubarak Al-Kabeer Hospital. Authors SR and SS contributed case material from Adan Hospital. MS drafted the manuscript. Author AB participated in the coordination of the study. All the authors read the manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
The authors would like to thank Sally Roy for recording the patients data base and Delphine D'Souza for typing this manuscript.
Contributor Information
Tariq Sinan, Email: drtariq999@yahoo.com.
Mehraj Sheikh, Email: mehraj@hsc.kuniv.edu.kw.
Salwa Ramadan, Email: salwafais@yahoo.com.
Sukhpal Sahwney, Email: sukh48@yahoo.com.
Abdulla Behbehani, Email: quick_behbehani@yahoo.com.
References
- Dye C, Scheele S, Dolin P, Pathania V, Raviglione MC. Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. WHO Global Surveillance and Monitoring Project. JAMA. 1999;282:677–686. doi: 10.1001/jama.282.7.677. [DOI] [PubMed] [Google Scholar]
- Suri S, Gupta S, Suri R. Computed tomography in abdominal tuberculosis. B J Radiol. 1999;72:92–8. doi: 10.1259/bjr.72.853.10341698. [DOI] [PubMed] [Google Scholar]
- Jadvar H, Mindelzun RE, Olcott EW, Levitt DB. Still the great mimicker: Abdominal tuberculosis. AJR Am J Roentgenol. 1997;168:1455–60. doi: 10.2214/ajr.168.6.9168707. [DOI] [PubMed] [Google Scholar]
- Akhan O, Pringot J. Imaging of abdominal tuberculosis. Eur Radiol. 2002;12:312–23. doi: 10.1007/s003300100994. [DOI] [PubMed] [Google Scholar]
- Batra A, Gulati MS, Sarma D, Paul SB. Sonographic appearances in abdominal tuberculosis. J of Clin Ultrasound. 2000;28:233–245. doi: 10.1002/(SICI)1097-0096(200006)28:5<233::AID-JCU5>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- Hulnick DH, Megibow AJ, Naidich DP, Hilton S, Cho KC, Balthazar EJ. Abdominal tuberculosis: CT evaluation. Radiology. 1985;157:199–204. doi: 10.1148/radiology.157.1.4034967. [DOI] [PubMed] [Google Scholar]
- Hanson RD, Hunter TB. Tuberculous peritonitis: CT appearance. AJR Am J Roentgenol. 1985;144:931–932. doi: 10.2214/ajr.144.5.931. [DOI] [PubMed] [Google Scholar]
- Dahlene DH, Jr, Stanley RJ, Koehler RE, et al. Abdominal tuberculosis: CT findings. J Comput Assist Tomogr. 1984;8:443–445. doi: 10.1097/00004728-198406000-00014. [DOI] [PubMed] [Google Scholar]
- Lee DH, Lim JH, Ko YT, et al. Sonographic findings of tuberculous peritonitis of wet ascitic type. Clin Radiol. 1991;44:306–10. doi: 10.1016/s0009-9260(05)81264-4. [DOI] [PubMed] [Google Scholar]
- AI-Hilaly MA, Abu Zidan FM, Zayed FF, et al. Tuberculous appendicitis with perforation. Br J Clin Pract. 1990;44:632–3. [PubMed] [Google Scholar]
- Thoeni RF, Margulis AR. Gastrointestinal tuberculosis. Semin Roentgenol. 1979;14:283. doi: 10.1016/0037-198x(79)90025-7. [DOI] [PubMed] [Google Scholar]
- Ozkan K, Gurses N. Ultrasonic appearance of tuberculous peritonitis: Case report. J Clin Ultrasound. 1987;15:350–2. doi: 10.1002/jcu.1870150511. [DOI] [PubMed] [Google Scholar]
- Sheikh M, Mossa I, Hussein FMY, Qurttom MAF, Behbehani AI. Ultrasonographic diagnosis in abdominal tuberculosis. Australasian Radiology. 1999;43:175–179. doi: 10.1046/j.1440-1673.1999.00630.x. [DOI] [PubMed] [Google Scholar]
- Seshul MB, Coulam CM. Pseudomyxoma peritonei: Computed tomography and sonography. AJR Am J Roentgenol. 1981;136:803–6. doi: 10.2214/ajr.136.4.803. [DOI] [PubMed] [Google Scholar]
- Bankier AA, Fleischman D, Wiesmayr MN, Wiesman MN, Putz D, Kontrus M, et al. Update: Abdominal tuberculosis – unusual findings on CT. Clin Radiol. 1995;50:223–228. doi: 10.1016/s0009-9260(05)83474-9. [DOI] [PubMed] [Google Scholar]
- Jain R, Sawhney S, Bhargava DK, et al. Diagnosis of abdominal tuberculosis: sonographic findings in patients with early disease. AJR Am J Roentgenol. 1995;165:1391. doi: 10.2214/ajr.165.6.7484572. [DOI] [PubMed] [Google Scholar]
- Sheikh M, Abu Zidan FM, Al-Hilaly MA, Behbehani AI. Abdominal Tuberculosis. Comparison of sonography and computed tomography. J Clin Ultrasound. 1995;23:413–17. doi: 10.1002/jcu.1870230704. [DOI] [PubMed] [Google Scholar]
- Epstein BM, Mann JH. CT of abdominal tuberculosis. AJR Am J Roentgenol. 1982;139:861–6. doi: 10.2214/ajr.139.5.861. [DOI] [PubMed] [Google Scholar]
- Gulati MS, Sarma D, Paul SB. CT appearances in abdominal tuberculosis: A pictorial essay. Clinical Imag. 1999;23:51–59. doi: 10.1016/S0899-7071(98)00090-4. [DOI] [PubMed] [Google Scholar]
- Li DKD, Rennie CS. Abdominal computed tomography in Whipple's disease. J Comput Assist Tomogr. 1980;4:630–633. doi: 10.1097/00004728-198104000-00017. [DOI] [PubMed] [Google Scholar]
- Lundstedt C, Myman R, Brismar J, Hugosson C, Kagevi I. Imaging of tuberculosis II. Abdominal manifestations in 112 patients. Acta Radiol. 1996;37:489–405. doi: 10.1177/02841851960373P213. [DOI] [PubMed] [Google Scholar]
- Balthazar EJ, Gordon R, Hulnick D. Ileocecal tuberculosis: CT and radiologic evaluation. AJR Am J Roentgenol. 1990;154:499–503. doi: 10.2214/ajr.154.3.2106212. [DOI] [PubMed] [Google Scholar]
- Underwood MJ, Thompson MM, Sayers RD, Hall AW. Presentation of abdominal tuberculosis to general surgeons. Br J Surg. 1992;79:1077–1079. doi: 10.1002/bjs.1800791030. [DOI] [PubMed] [Google Scholar]
- Aston NO, de Costa AM. Abdominal tuberculosis. Br J Clin Pract. 1990;44:58–61. [PubMed] [Google Scholar]
- Paustian FF, Marshal JB. Intestinal tuberculosis. In: Berk JE, editor. Gastroenterology. Philadelphia: WB Saunders Co; 1985. p. 2018. [Google Scholar]
- Lim JH, Ko YT, Lee DH, et al. Sonography of inflammatory bowel disease: findings and value in differential diagnosis. AJR Am J Roentgenol. 1994;163:343. doi: 10.2214/ajr.163.2.8037027. [DOI] [PubMed] [Google Scholar]
- Bhansali SK. Abdominal tuberculosis. Experience with 300 cases. Am J Gastroenterol. 1977;67:324–337. [PubMed] [Google Scholar]
- Denath FM. Abdominal Tuberculosis in children: CT findings. Gastrointest Radiol. 1990;15:303–306. doi: 10.1007/BF01888804. [DOI] [PubMed] [Google Scholar]
- Jain R, Sawhney G, Gupta RG, et al. Sonographic appearances and percutaneous management of primary tuberculous liver abscess. J Clin Ultrasound. 1999;27:159. doi: 10.1002/(SICI)1097-0096(199903/04)27:3<159::AID-JCU11>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- Zisper RD, Rav JE, Ricketts RR, Lynn CB. Tuberculous pseudotumors of the liver. Am J Med. 1976;61:946–951. doi: 10.1016/0002-9343(76)90420-4. [DOI] [PubMed] [Google Scholar]