Abstract
Background
This study advances the use of a utility model to model physician-patient interactions from the perspectives of physicians and patients.
Presentation of the hypothesis
In cases involving acute care, patient counseling involves a relatively straightforward transfer of information from the physician to a patient. The patient has less information than the physician on the impact the condition and its treatment have on utility. In decisions involving lifestyle changes, the patient may have more information than the physician on his/her utility of consumption; moreover, differences in discounting future health may contribute significantly to differences between patients' preferences and physicians' recommendations.
Testing the hypothesis
The expectation of differences in internal discount rate between patients and their physicians is discussed.
Implications of the hypothesis
This utility model provides a conceptual basis for the finding that educational approaches alone may not effect changes in patient behavior and suggests other economic variables that could be targeted in the attempt to produce healthier behavior.
Keywords: utility, patient education, counseling, risk behavior
Background
An important function of the medical community is to advise patients on healthy behavior. This occurs at the level of the physician-patient relationship and at the core level of public health activities. Health professionals have many years of training that provide them a great knowledge of the health effects of risk-taking behaviors. These behaviors may be interpreted by physicians as anti-health or irrational on the part of patients. Physicians and public health professionals attempt to educate patients concerning the risks of these activities in order to reduce the long-term adverse health effects associated with such anti-health behaviors as smoking, poor diet, indoor tanning, and sedentary lifestyle.
A number of studies use utility maximizing models to model health production and "irrational" behaviors at the individual level. [1-4]. These studies attempt to describe the factors underlying patients' health behavior decision making. The economic theory of consumer behavior indicates that a rational individual will maximize his or her utility subject to budget and time constraints and a health production function [1,3,5-7]. These models have been very effective in describing addictive behavior and the quantitative impact of price on consumption [8].
Presentation of the hypothesis
The utility theory incorporates beliefs about the probability of outcomes, the value, or utility, of these outcomes, and the timing at which outcomes occur. Incorporating the timing of the outcome is an essential feature as people place more value on present consumption of goods than they do on future consumption. The value of future goods are "discounted". The economic justification for discounting is firmly established in cost-effective analysis of health care programs [9,10]. Discount rates for health outcomes are greater than for monetary outcomes [11] and explain in part why people may fail to engage in preventive health measures [12,13].
A simple utility model can be used to describe the factors underlying the health behavior recommendations physicians give patients. This paper is based on the proposition that patients do choose behaviors based on maximization of utility. We explore how differences between the preferences of advisors and advisees may lead to advice from physicians that is "irrational" when viewed from the perspective of patients and result in poor compliance with physicians' lifestyle change recommendations.
Testing the hypothesis
In a medical market, a patient (a consumer) makes choices regarding whether he or she will follow physician's advice or treatments, based upon his or her preferences. The preferences of advisors (physicians) and advisees (patients) are described by their utility functions [1,3]. The function c represents a "consumptive activity" about which the physician is providing counseling (for example, a medical treatment or a lifestyle activity). This may be a harmful or beneficial activity (for example, beneficial goods like exercise or good diet or hazardous activities such as smoking, tanning bed, or sun exposure). The function y represents other goods, and in this case we consider y the state of health. There are effects of consumption of c on y. The utility of combinations of y and c are given by up [y(t), c(t)]. Patients make current decisions (time t = 0) on the consumption of c based on their utility function. Patients attempt to maximize the present value of their utility over their lifetime. The mathematical formulation of the patients' utility function is given by equation 1:
Up(0) = ∫ e-σpt up [y(t),c(t)]
This function discounts the value of future consumption based on the patient's time preference for health, σ. In the patient's self-assessment of their utility, the patient's perceived value of y(t) and c(t) are used. The subscript "p" is used to distinguish preferences of the patient from those of the doctor as described below.
In acting as the agent of the patient, the physician offers medical advice designed to improve patients' overall well being, that is, to maximize patients' utility. The physician's recommendations therefore can be modeled by a similar utility function. Physicians consider a utility function based on their own medical knowledge and preferences. The subscript d (for doctor) is used to distinguish this from the patient's utility function in equation 2.
Ud(0) = ∫ e-σ'dt ud [y(t),c(t)]
The central theme to be explored is that there are two potential sources of misunderstanding between physicians and patients: different valuations of u [y(t), c(t)] and different discount rates. While both are relevant, we will emphasize the importance of differences in discount rates on lifestyle decision counseling and behavior.
We can describe medical counseling as a process in which physicians give patients information on the components of the utility function. Counseling entails to some extent educating the patient about the true value of y(t) and the effect of c(t) on y(t). The physician advises the patient based on medical knowledge of the effect of consumption of c on y. When c is a treatment, the physician may help the patient determine expected effects of c(t) based on the physician's knowledge of the effects of c on patients. For short run decisions, the effect of the discounting term e-σt is not important.
As an example of this, consider a physician treating a patient who has an acute bacterial pneumonia. The physician educates the patient about the expected outcome y(t) in case the patient is left untreated (progression of the infection) or if treated with antibiotic c (in which case the infection will very likely be cured). The physician also educates the patient about other effects of c(t), including the potential adverse effects of treatment on utility (that is, the physician provides medical knowledge about potential drug rashes or gastrointestinal upset). The physician provides medical knowledge about the disease and its expected outcomes with and without treatment and about the treatment itself. Because the physician has more information than the patient on both the disease and its treatment, patients generally follow physician advice (notwithstanding missing an occasional dose) in such a situation. This example of medical counseling represents an "information inequality" problem, solved by patient education.
Counseling patients about "lifestyle" decisions involves greater complexity. This manifests by several ways in which physicians' impressions of utility may be distinctly different than those of patients. In considering lifestyle decisions, similar to the example above, the physician may have medical information concerning the effect of c(t) on y(t). However, often this medical information is defined by statistical effects in large populations. There is less certainty of a specific effect for the particular patient; for an individual patient, we do not know if smoking cessation or decreased fat intake will significantly change lifespan or other components of health. Moreover, the physician knows less about the patients' value of c(t) than does the patient; information inequality exists but in the opposite direction. Indeed, the physician may have a very different impression of c(t) than does the patient (the physician may experience less euphoria/benefit from smoking, hamburger consumption or tanning bed use or may feel more vitalized from exercise). Moreover, the effects of c(t) on y(t) may have prolonged time horizons for these lifestyle activities. Because physicians and their patients may not share similar values of σ, there may be large differences in the effects of discounting future utility between physicians and their patients.
Time preferences for health outcomes can vary considerably among different people [13]. There is reason to expect that physicians may have lower than average values of σ (that is, they discount the future less) than the general population. Physicians have chosen a profession requiring a great degree of "delayed gratification", sacrificing years of current income during the prolonged training period for higher income later in life. One would also expect that having chosen a health services career, physicians and other health professionals likely ascribe higher values to health and lower health discounting than the general population. Physicians' understanding of research linking risk factors and health may also give them a greater sense of certainty than their patients have of the long-term effects of consumption c(t) on health y(t); this would result in physicians discounting these future events less than their patients do.
Physicians likely base their health recommendations on their own perception of utility. There is a tendency for people to assume that other people discount the future similar to themselves [14]. If physicians make such an assumption, they may offer advice that would not appear rational from the perspective of a patient who perceives a very different utility function.
The potential differences between patients' and physicians' impressions of the utility function can be well demonstrated by tanning bed counseling. Physicians may be dumbfounded that, despite their tireless efforts to educate patients about the long-term adverse effects of ultraviolet light exposure [educating patients about the effect of c(t) on y(t)], patients still "don't get it" and continue to expose themselves to the sun and to use tanning beds. This may result from two differences between the physician and patient: one, differences in utility preferences for consumption, and two, differences in discount rates. First, the physician may not recognize the utility to patients of having a tan (and its social implications). Second, the physician may be utilizing the physicians' discount rate for future health (rather than the patient's) in assessing the importance of future health risks on patients' utility. This is no longer simply an "information inequality" problem and may reflect deeper differences between the physician and the patient. Patient counseling that is based on transferring information on the condition may not be adequate for changing patient behavior.
Regarding lifestyle decisions, discounting differences are extremely important because over time they make large contributions to differences in the value assigned to future health states. Assume now that the only differences between the physician and patient utility functions are in the discount rates. In this case, there is no difference in information or utility preferences between the patient and the physician. The utility at a given time t is given by equation 3:
Ut = e-σt u [y(t),c(t)]
The assumption of consistent preferences between patients and physicians implies equation 4:
up [y(t),c(t)] = ud [y(t),c(t)]
The difference in the utility of the future health care state assigned by the patient and the physician at any time can be assessed as the ratio of patient to physician utility and is given by equation 5:
e-σpt up [y(t),c(t)]/ e-σdt ud [y(t),c(t)] = e-σpt/ e-σdt = e-(σp-σd)t = e-σp't
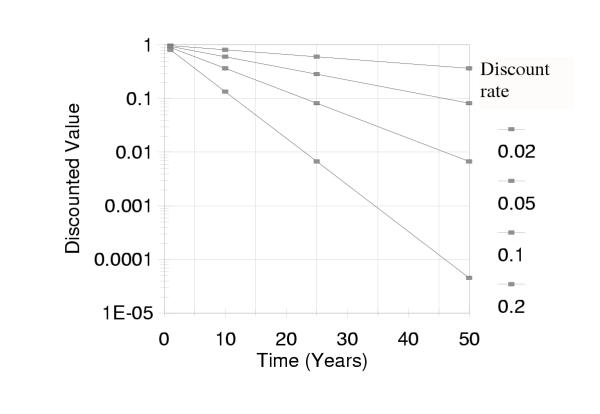
where the value σ' is the difference between the physician's and patient's discount rate. For short periods of time and typical discount rates, the patient/physician discounting ratio is approximately unity (Figure 1). For longer times, as might be involved in decisions reflecting life-style changes, even small differences in discount rate result in very large differences in patient and physician preferences at later times (Figure 1).
Figure 1.
The impact of discount rate differences between patients and physicians is large for outcomes that occur in the distant future. For short periods of time and typical discount rates, discounting does not result in much difference in the value assigned by patients and physicians to future health states. For longer times, as might be involved in decisions reflecting life-style changes, even small differences in discount rate between patients and physicians result in large differences in the value assigned to future health states.
Thus, even if patients fully understand the risks that are likely to occur after long periods of time (such as the risk of skin cancer associated with tanning bed use or coronary vascular disease from excessive dietary fat), differences in discount rate alone will result in those long-term risks having a very low present value to patients. A physician may feel reducing the risk of lung cancer in a smoker is critical. The patient may discount that future risk of lung cancer to the point that it is does not have sufficient magnitude to change their choice of current behavior.
The effect of discounting is less but still considerable for effects that have a probability of occurring at any age. For such conditions, the cumulative effect of discounting over time is given by summing (integrating) the discounted value over time in equation 6:
∫ e-σ't dt = [1 - e-σ't'] / σ'
For t' up to 1 year, there is less than 10% difference in cumulative effect for differences in annual discount rate σ' up to 20% (Table 1). Over 50 years, the cumulative reduction in utility is 90% for σ' of 20%. The magnitude of discounting for conditions that may occur over time, while considerable, is not nearly as great as for those conditions that occur only in the distant future. Discounting of most medical conditions would be expected to fall between these two extremes.
Table 1.
Discounting for effects that have a probability of occurring at any age*
| Annual Discount Rate | ||||
| Years of Exposure | 0.02 | 0.05 | 0.1 | 0.2 |
| 1 | 0.99 | 0.91 | 0.79 | 0.63 |
| 10 | 0.98 | 0.79 | 0.57 | 0.37 |
| 25 | 0.95 | 0.63 | 0.37 | 0.20 |
| 50 | 0.91 | 0.43 | 0.20 | 0.10 |
*For a given annual discount rate and a given number of years over which an event may occur, this table provides the ratio of the discounted weight assigned to the event and the weight that would have been assigned had there been no discounting of future events. For example, if a patient with a discount rate of 0.2 is weighing the importance of a heart attack that may occur at any time over the next 10 years, he or she assigns only 37% as much importance to the possibility as would someone who does not discount the future.
Implications of the hypothesis
The utility model in this study provides a ready understanding of the difficulties encountered by physicians who try to modify patients' current behavior to improve long-term health outcomes. This analysis demonstrates that provision of medical knowledge alone may be insufficient to change patients' "rational" utility-maximizing behavior patterns and that differences between physician and patient preferences may contribute to physicians' erroneous perception of "irrational" behavior on the part of patients.
Physicians should consider the patient's "value system" in developing a "rational" counseling strategy. Cultural factors can be considered: in some countries/cultures there may be a more general "live for today" (high discount rate) attitude that could contribute to higher rates of smoking and other medically risky behaviors. Cultural differences in discount rates may be economically sensible if they are due to differences in life expectancies. Alternatively, high discount rates may contribute to behaviors associated with lower life expectancies in these cultures.
Is there a role for physicians to try to change patients' discount rate for future health in order to maximize long-term health outcomes? Are there strategies for changing the time preferences of patients? Unfortunately, time preferences are an inherently difficult internal measure to quantify. If we accept that patients' time preferences are not subject to change and that they find an immediate benefit from lifestyle activities that have long-term adverse effects, we should expect that there will be a certain level of continued consumption of the activity despite all efforts at patient education. On the other hand, if future health discounting can be changed, it would provide a novel means to improve compliance with life enhancing behavior changes.
Other economic factors also may contribute to systematic differences between patients' and physicians' perspectives. Income effects may favor consumption of one good over another. Disparities in income between physicians and their patients may thus lead to systematic differences between physician preferences and patient preferences such that physician recommendations may not maximize the patients' utility function. Physicians' established positions in society may also contribute to differing perspectives. For example, physicians may not have the same need for a "tan look" [lower c(t)] that a young, unmarried patient involved in the dating game might have. Another bias that may lead to different preferences between physicians and their patients is selection of individuals who care more about health (that is, individuals who exhibit greater u [y(t), c(t)] with higher y(t) relative to other goods) for health profession careers.
This analysis has been couched in medical terms, but it is also applicable to other advisor/advisee relationships. For example, consider the context of corporate managers making decisions about benefits for employees. When the benefit involves a short time horizon and the manager has greater information than the employee about the effects of the benefit, it may be sensible for the manager to make a decision about the benefit in the employee's behalf. For pension plan decisions, however, where there is a long time horizon and where the value ascribed to the benefit may be very different between the employer and the employee, the manager may make an "irrational" choice from the employee's perspective. A highly educated high school counselor may also wish to consider the value system of students and their families when providing counseling concerning students' long-term plans and ambitions. Such considerations may also hold at the geopolitical level when the acute needs of a developing area or country are in conflict with the long-term goals of a more fully developed nation.
Terms such as "rational" and "irrational" have favorable and pejorative connotations, respectively. How these terms are applied to the physician's advice or to the patient's behavior is dependent on one's frame of reference, and there may be no one "correct" answer. When a patient acts as though σ = ∞, that is, when they act as if there is no tomorrow at all, we would describe their behavior as irrational. Some time preference (σ > 0) for current consumption is sensible, however, even if just from the standpoint that lifespan is not infinite. When physicians provide advice based on a σ  0 for future health without regard to patients' preferences, the advice may also be considered "irrational" when viewed from the patient's perspective.
0 for future health without regard to patients' preferences, the advice may also be considered "irrational" when viewed from the patient's perspective.
Physicians often rate patients' health status differently than do patients, and it is already widely recognized that physicians should listen to and try to consider the values of their patients [15]. The economic approach presented here provides a framework for quantification of this principle and makes clear some of the components that must be considered. Moreover, it makes clear that many current patient education approaches may be inadequate to address recognized problems in health behavior that have impact on long term health.
This analysis is not meant to suggest that physicians should give up on efforts to reduce anti-health behaviors. The analysis does mean to suggest that factors underlying patients' decision to engage in such behaviors need to be considered. What may appear irrational to the physician may appear quite rational to the patient. Simply educating the patient of the physician's view will not likely suffice to change patient behaviors. Other approaches that change patients' preferences are needed.
Clearly, we have presented a purely theoretical model, and the strength and validity of this model can be shown only through empiric analysis. The model is in keeping with data on tanning bed use. Tanning bed users are better informed about the damaging effects of UV light than non-tanning bed users, but they continue to engage in unprotected UV exposure [8,16]. This information suggests that education of long-term outcomes by itself is not sufficient to cause changes in behavior, at least in part because of discounting the value of these future outcomes. Moreover, our model clearly points to the need to change societal beliefs concerning the value of a tan – that is, change c(t). Until then, public health efforts to reduce tanning are likely doomed to failure. The model presented here provides a simple mathematical framework for understanding why all lifestyle change public health efforts need to consider the current value of consumption (as perceived by the consumer) and the impact of patients' discounting future events.
Discounting the future has important implications for understanding patients' choices in health behaviors. The phenomenon of discounting the future is a complex one, inherent to humans and other animals [17,18]. Our analysis is based on the assumption of exponential discounting of future events, a simplifying assumption that does not always hold in experiments analyzing discounting behavior [11]. Nevertheless, other models of discounting behavior also show strong discounting of future events [17]. Whether discounting is normative or not, the differences in discount rates between different people have the potential to make a significant contribution to differences in behavioral choices. Use of the utility maximizing model illustrates the difficulties of changing patients' behavior now for the benefit of future health. It is essential both that physicians recognize this potential when counseling patients and that public health programs take this phenomenon into account.
Competing interests
None declared
Authors' contributions
SRF conceived of the study, participated in its design and coordination, and drafted the manuscript. GJC participated in the design of the study and developed the equations. JYH participated in the coordination and review of the manuscript. ABF participated in the design and coordination of the study.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
Financial support for this study was provided by an unrestricted grant from Bristol-Myers Squibb Dermatology.
Contributor Information
Steven R Feldman, Email: sfeldman@wfubmc.edu.
G John Chen, Email: gchen@wfubmc.edu.
Judy Y Hu, Email: jyhu@wfubmc.edu.
Alan B Fleischer, Email: afleisch@wfubmc.edu.
References
- Becker G, Murphy K. A theory of rational addiction. J Political Economy. 1988;96:675–700. doi: 10.1086/261558. [DOI] [Google Scholar]
- Chaloupka F. Rational addictive behavior and cigarette smoking. J Political Economy. 1991;99:722–742. doi: 10.1086/261776. [DOI] [Google Scholar]
- Grossman M. On the concept of health capital and the demand for health. J Political Economy. 1972;80:223–255. doi: 10.1086/259880. [DOI] [Google Scholar]
- Selden T. Uncertainty and health care spending by the poor: the health capital model revisited. Journal of Health Economics. 1993;12:109–115. doi: 10.1016/0167-6296(93)90043-E. [DOI] [PubMed] [Google Scholar]
- Becker G. A theory of the allocation of time. The Economic Journal. 1975;75:493–517. [Google Scholar]
- Michael R, Becker G. On the new theory of consumer behavior. Swedish Journal of Economics. 1973;75:378–396. [Google Scholar]
- Muurinen J. Demand for health: a generalized Grossman model. Journal of Health Economics. 1982;1:5–28. doi: 10.1016/0167-6296(82)90019-4. [DOI] [PubMed] [Google Scholar]
- Mawn VB, Fleischer AB., Jr A survey of attitudes, beliefs, and behavior regarding tanning bed use, sunbathing, and sunscreen use. J Am Acad Dermatol. 1993;29:959–962. doi: 10.1016/0190-9622(93)70274-w. [DOI] [PubMed] [Google Scholar]
- Redelmeier DA, Heller DN. Time preference in medical decision making and cost-effectiveness analysis. Med Decis Making. 1993;13:212–217. doi: 10.1177/0272989X9301300306. [DOI] [PubMed] [Google Scholar]
- Weinstein MC. Time-preference studies in the health care context. Med Decis Making. 1993;13:218–219. doi: 10.1177/0272989X9301300307. [DOI] [PubMed] [Google Scholar]
- Chapman GB, Elstein AS. Valuing the future: temporal discounting of health and money. Med Decis Making. 1995;15:373–386. doi: 10.1177/0272989X9501500408. [DOI] [PubMed] [Google Scholar]
- Chapman GB, Coups EJ. Time preferences and preventive health behavior: acceptance of the influenza vaccine. Med Decis Making. 1999;19:307–314. doi: 10.1177/0272989X9901900309. [DOI] [PubMed] [Google Scholar]
- Ganiats TG, Carson RT, Hamm RM, Cantor SB, Sumner W, Spann SJ, et al. Population-based time preferences for future health outcomes. Med Decis Making. 2000;20:263–270. doi: 10.1177/0272989X0002000302. [DOI] [PubMed] [Google Scholar]
- Cairns J, van der PM. Do people value their own future health differently from others' future health? Med Decis Making. 1999;19:466–472. doi: 10.1177/0272989X9901900414. [DOI] [PubMed] [Google Scholar]
- Becker GS, Grossman M, Murphy KM. Rational addiction and the effect of price on consumption. In: Loewenstein G, Elster J, editor. In Choice Over Time. New York: Russell Sage Foundation; 1992. pp. 361–370. [Google Scholar]
- Suarez-Almazor ME, Conner-Spady B, Kendall CJ, Russell AS, Skeith K. Lack of congruence in the ratings of patients' health status by patients and their physicians. Med Decis Making. 2001;21:113–121. doi: 10.1177/02729890122062361. [DOI] [PubMed] [Google Scholar]
- Ainslie G, Haslam N. Hyperbolic discounting. In: Loewenstein G, Elster J, editor. In Choice Over Time. New York: Russell Sage Foundation; 1992. pp. 57–92. [Google Scholar]
- Rachlin H, Raineri A. Irrationality, impulsiveness, and selfishness as discount reversal effects. In: Loewenstein G, Elster J, editor. In Choice Over Time. New York: Russell Sage Foundation; 1992. pp. 93–118. [Google Scholar]