Abstract
Objective:
This single-center study tested the hypothesis that preoperative risk factors and surgical complexity predict more variation in hospital costs than complications.
Background:
Complications after surgical operations have been shown to significantly increase hospital cost. The impact on complication-related costs of preoperative risk factors is less well known.
Methods:
The National Surgical Quality Improvement Program (NSQIP) preoperative risk factors, surgical complexity, and outcomes, along with hospital costs, were analyzed for a random sample of 5875 patients on 6 surgical services. Operation complexity was assessed by work RVUs (Centers for Medicare and Medicaid Services Resource Based Relative Value Scale). The difference in mean hospital costs associated with all variables was analyzed. Multiple linear regression was used to determine the cost variation associated with all variables separately and combined.
Results:
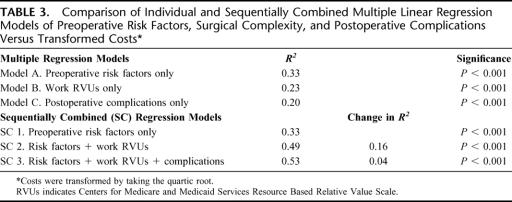
Fifty-one of 60 preoperative risk factors, work RVUs, and 22 of 29 postoperative complications were associated with higher variable direct costs (P < 0.05). Linear regressions showed that risk factors predicted 33% (P < 0.001) of cost variation, work RVUs predicted 23% (P < 0.001), and complications predicted 20% (P < 0.001). Risk factors and work RVUs together predicted 49% of cost variation (P < 0.001) or 16% more than risk factors alone. Adding complications to this combined model modestly increased prediction of costs by 4% for a total of 53% (P < 0.001).
Conclusion:
Preoperative risk factors and surgical complexity are more effective predictors of hospital costs than complications. Preoperative intervention to reduce risk could lead to significant cost savings. Payers and regulatory agencies should risk-adjust hospital cost assessments using clinical information that integrates costs, preoperative risk, complexity of operation, and outcomes.
This study used the NSQIP dataset to assess the impact of preoperative risk factors, surgical complexity, and postoperative complications on hospital costs at the University of Kentucky Hospital for 5875 surgical patients. Risk factors and complexity were found to be stronger predictors of hospital costs than complications.
Surgical complications have been shown to be associated with increased inpatient hospital costs.1,2 As a result, reducing complications has become a desirable objective for quality improvement initiatives to reduce hospital costs and simultaneously improve patient outcomes.3 For example, at the University of Kentucky Medical Center (UKMC), an outside consultant estimated that the institution sustained $6,000,000 in annually recurring surgical complication-related costs. It was proposed there was an opportunity to relatively “easily” reduce these costs by 30% to 40%. These estimates were based on data from the hospital's cost accounting and discharge abstraction coding systems.
Historically, studies from administrative datasets have demonstrated the significance of comorbidities in predicting complications and costs.4–6 However, several studies have shown that additional information and predictive power come from data obtained from review of the clinical record.7–11 The cost of such review has limited large-scale cost analyses using data from the clinical record.
Since 1999, private sector hospitals have successfully implemented the NSQIP to track patient risk factors and outcomes.12 The NSQIP in the private sector provides the advantage of a large random sample of clinical data, which has been demonstrated over time to predict complication and death in surgery patients. An initial study comparing the NSQIP and 2 administrative datasets in predicting surgical mortality demonstrated the NSQIP data was a better predictor.13 The NSQIP has been effectively used for over a decade in Veterans’ Affairs medical centers, but the organization and funding of the Veterans’ Affairs hospitals have made studies of cost using these data difficult. The application of the NSQIP in the private sector where more detailed cost accounting systems are common allows for a more clinically robust analysis of costs related to surgical care.
In this study, we analyzed the impact of the NSQIP preoperative risk factors, surgical complexity, and postoperative complications on costs for 6 services at UKMC. Specifically, we tested the hypothesis that preoperative risk factors and surgical complexity predict more variation in hospital costs than complications.
The Department of Surgery at UKMC provides a unique opportunity for examining the NSQIP data and costs. UKMC is a full-service teaching hospital and the primary healthcare facility for the Bluegrass area of central Kentucky and the Appalachian region of eastern Kentucky. The 473-bed facility includes the UK Hospital, the UK Children's Hospital, the Lucille Parker Markey Cancer Center, the UK Transplant Center, the Kentucky Clinic, and the Sanders-Brown Center on Aging. UKMC is designated as the region's only level I trauma center and provides a complete range of health care, but specializes in tertiary and quaternary care of very ill patients.
The UKMC Department of Surgery has participated in the NSQIP private sector initiative since its inception, first as an alpha site along with Emory University Hospital and the University of Michigan and then as one of 18 beta sites continuing the NSQIP implementation in the private sector. The Department is unique thus far among the NSQIP private sector sites in its application of the NSQIP to several different surgical services. This broad sampling of NSQIP data among surgical services along with the several years’ experience with the NSQIP in the private setting makes the Department of Surgery at UKMC particularly well suited for this study.
OBJECTIVE OF THE STUDY
This single-center study tested the hypothesis that preoperative risk factors and surgical complexity predict more variation in hospital costs than complications and also looked at the relationship among these factors in predicting costs.
METHODOLOGY
The UKMC Department of Surgery, as part of theNSQIP, conducted a random sample of 5875 general surgery, neurosurgery, orthopaedics, plastic surgery, thoracic surgery, and vascular surgery patients who underwent major surgery between October 1, 2001, and September 30, 2003, at UKMC. The inclusion of these 6 different surgical services added variability in patient characteristics to the data that ameliorates somewhat the single-site limitation to generalizability of this study. The NSQIP methodology in the private sector has been reviewed in detail by Fink et al.12
Briefly, the NSQIP includes major surgery patients as defined by those procedures having general, epidural, or spinal anesthesia along with some monitored anesthetic conscious sedation (MAC) procedures. The NSQIP excludes the primary admission related to trauma and patients less than 17 years of age. Certain low-morbidity, high-volume procedures such as hernia repairs, lumpectomies, and transurethral prostatectomies are limited in the sample to 5 per 8-day cycle. Patient selection at UKMC was randomized by taking the first 70 patients on 6 services from the operating room log every 8 days that matched the inclusion criteria. Using an 8-day cycle ensured a different daily operating room schedule was included as the majority of cases in consecutive cycles. Data collection for plastic surgery began in January 2002 and for thoracic surgery in February 2002, which reduced slightly their representation in this 2-year sample.
For each patient, clinical nurse reviewers recorded 60 preoperative risk factors, 18 intraoperative factors, and 29 postoperative complications, including death, for 30 days postoperatively. Information after discharge was obtained through hospital and clinic medical document review as well as follow-up contact by letter and phone.
These patients’ inpatient hospital variable direct costs were obtained from the hospital cost accounting system, TSI (Eclipsys Technologies Corp., Boca Raton, FL), by preoperative days, day of operation, and postoperative days. TSI uses direct acquisition costs to allocate supply costs and time-and-motion studies to allocate nursing and other labor costs. These are included in the variable direct costs used in this study. Variable direct costs do not include fixed overhead such as electricity and central administration, which do not change with small variations in care delivery. These costs are used in this study because they more accurately reflect potential cost savings from process and quality improvement efforts or other changes in care. For the rest of this article, they are simply referred to as costs.
Operation complexity was assessed by summing the 2002 work RVUs14 (Centers for Medicare and Medicaid Services Resource Based Relative Value Scale) for all current procedural terminology codes recorded for the surgery. Work RVUs have been shown in the private sector NSQIP to be better predictors of surgical outcomes than complexity scores established by panels of surgical subspecialists.
Variance in costs associated with all variables was performed using the appropriate analysis of variance, Pearson's correlation, or Student t test for means with a significance threshold P value of 0.05. Separate linear regression models were then used to determine the total variation in hospital costs associated with 1) preoperative risk factors, 2) surgical complexity, and 3) postoperative surgical complications. Sequential multiple regression was used to determine the cost variation associated with a combination of preoperative risk factors and surgical complexity, and then with a combination of risk, complexity, and postoperative complications.
RESULTS
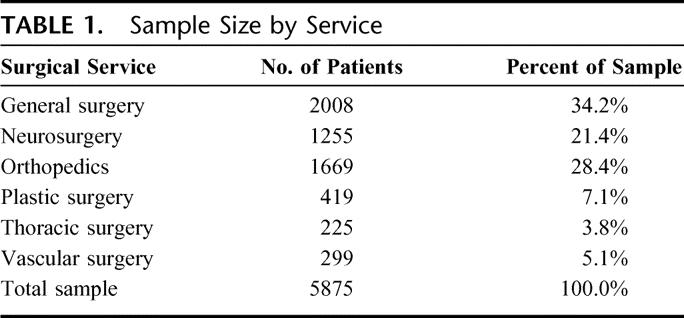
The total patient sample size by surgical service is listed in Table 1. The distribution by service matches the relative size of the services at UKMC and the impact of the NSQIP inclusion criteria of adult, nontrauma, and major surgery cases. This sample represented on average 34% of all procedures performed by those services at UKMC during that period. Service-specific analysis was performed and showed consistent but more predictive results compared with the all-services-combined results that are reported here. The more homogeneous patient population within a particular service allowed for stronger statistical modeling of clinical factors and costs than in the mixed population. This article focuses, however, on the results from the mixed service models to emphasize the power of the relationships across surgical services.
TABLE 1. Sample Size by Service
Perioperative Length of Stay and Costs
The median total length of stay was 2 days and the mean was 4.07 days. Among these 5875 patients, 1010 (17.2%) were admitted before the day of surgery; their median preoperative stay was 2 days and ranged from 1 to 49 days. Almost twice as many patients, 1962 (33.4%), were admitted and discharged on the same day of surgery. For the 3862 (65.7%) patients who did not go home on the day of surgery, the median postoperative length of stay was 2 days and ranged from 1 to 95 days. The mean total costs for all patients were $4088. These consisted of mean preoperative costs of $407, mean day of surgery costs of $2589, and mean postoperative costs of $1092. Most costs for these surgical patients accrued on the day of surgery.
Preoperative Risk Factors and Costs
Mean costs were significantly higher (P < 0.05) for 51 of the 60 NSQIP preoperative risk factors. The 25 risk factors associated with a mean difference in variable direct costs greater than $5000 (P < 0.001) are shown in Table 2. The mean cost differences shown are for independent tests and may not be additive. A multivariate regression of all the preoperative risk factors versus transformed costs resulted in a model (model A, Table 3), which predicted 33% of the variation in costs (P < 0.001). Importantly, a separate regression analysis on patients who survived and whose postoperative course was uncomplicated predicted 27% of cost variation (P < 0.001). The data demonstrated an exponential relationship between combined risk factors and costs, so costs were transformed by taking the quartic root. This transformation yielded a higher R2 and more normally distributed residuals than the more frequently used log transformation. A scatterplot of the risk factor prediction of transformed costs versus actual is shown in Figure 1.
TABLE 2. The 25 Preoperative Risk Factors Associated With the Greatest Increase in Mean Variable Direct Costs
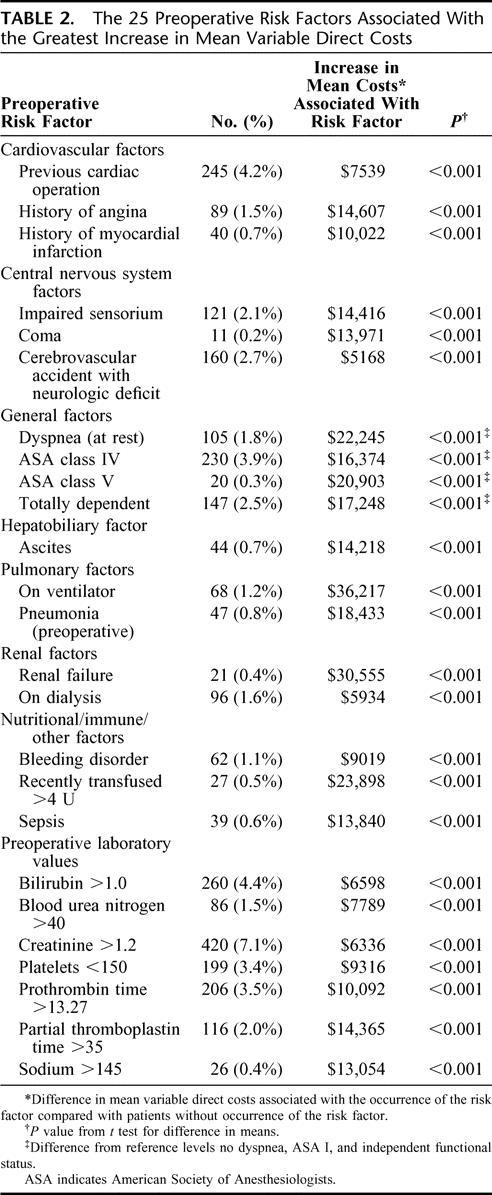
TABLE 3. Comparison of Individual and Sequentially Combined Multiple Linear Regression Models of Preoperative Risk Factors, Surgical Complexity, and Postoperative Complications Versus Transformed Costs
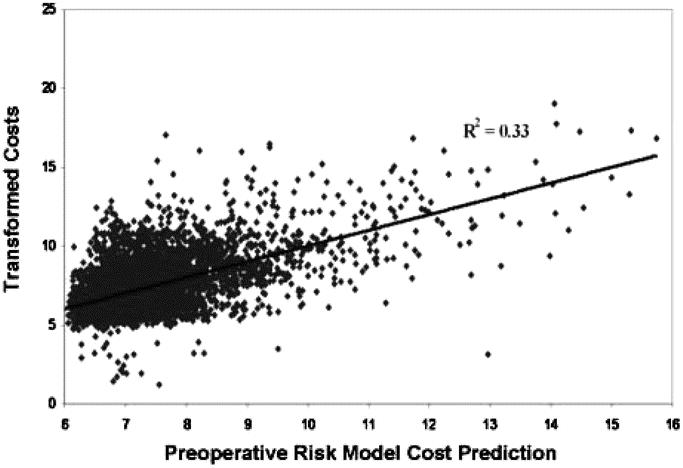
FIGURE 1. Preoperative risk factor cost predictions versus actual transformed costs. A multivariate regression of all the preoperative risk factors predicted 33% of the variation in costs (P < 0.001). The quartic root transformation yielded the best fit of the data.
Surgical Complexity (Work RVUs) and Costs
Surgical complexity as measured by total work RVUs predicted 23% (model B, Table 3) of cost variation (P < 0.001). Work RVUs correlated more strongly with day of surgery costs (r = 0.46, P < 0.001) than preoperative costs (r= 0.03, P = 0.045) or postoperative costs (r = 0.16, P < 0.001). Adding work RVUs to the preoperative risk model yielded a predictive gain of 16% and resulted in a combined model prediction of 49% of costs variation (model SC 2, Table 3). This combined predictive power was less than the sum of the individual risk factor (R2 = 0.33, model A, Table 3) and work RVU (R2 = 0.23, model B, Table 3) models indicating interdependence between the risk factors and surgical complexity.
Postoperative Complications and Costs
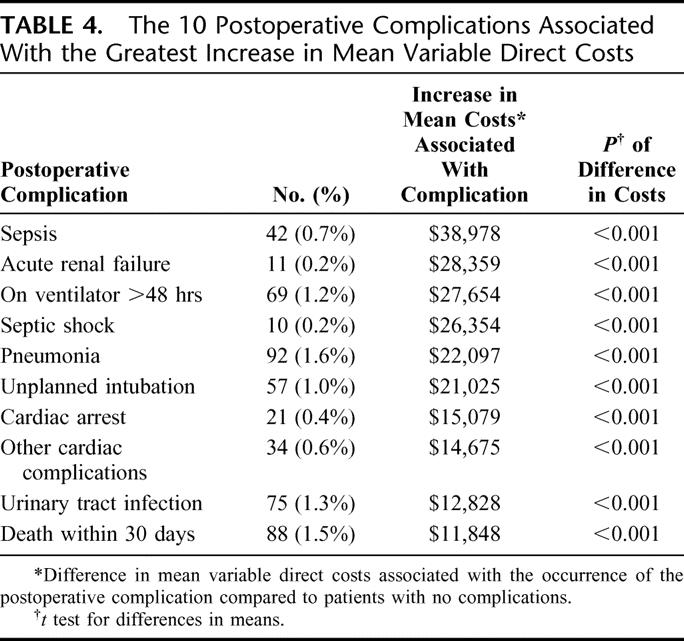
In this study, 5485 (93.3%) patients had no complications, 215 (3.7%) had a single complication, 173 (3.0%) had 2 or more complications, and 88 (1.5%) died within 30 days. A single patient had up to 8 complications recorded in the NSQIP. Mean costs for individual complications versus uncomplicated patients were higher for 22 of the 29 complications. The 10 postoperative complications associated with greatest increase in costs are shown in Table 4. The mean cost differences shown are for independent tests and may not be additive. For all complicated patients, the mean length of stay was 9.9 days (283%) longer than uncomplicated patients, total costs were $11,202 (323%) higher, and daily costs were $997 (11%) higher.
TABLE 4. The 10 Postoperative Complications Associated With the Greatest Increase in Mean Variable Direct Costs
A multiple regression of all the complications versus transformed costs resulted in a model (model C, Table 3), which predicted 20% of costs variation (P < 0.001) as compared with the 33% predicted by risk factors (model A, Table 3) and the 23% predicted by surgical complexity (model B, Table 3). Importantly, as a result of the ability of the risk factors to predict complication, the addition of complications to the combined risk factor and complexity model increased the predictive power only an additional 4% (model SC 3, Table 3).
DISCUSSION
This study demonstrated that the NSQIP preoperative risk factors, surgical complexity as measured by work RVUs, and the NSQIP postoperative complications were all significant predictors of hospital costs. Interestingly, preoperative risk and surgical complexity were more predictive of hospital costs than surgical complications. In fact, complications added minimally to the predictive power of a preoperative risk and surgical complexity cost model resulting from the interdependence of the complication and risk factor variables. This interdependence is to be expected because the risk factors were designed to predict complications and have been shown to do so.15
At UKMC, the observed number of complicated patients was below the NSQIP expected rate for the time period studied, implying that the complication-related costs were not the result of variation in quality but preoperative risk factors and complexity of the operation. Validation by a larger, multicenter risk-adjusting cost model is needed to confirm this assertion. If confirmed, efforts to decrease the majority of complication-related costs would therefore require development of new, more cost-effective surgical treatments and/or preoperative interventions to reduce the number and severity of preexisting risk factors.
Preoperative Risk Factor Costs Independent of Complication
The importance of preoperative management of risk factors is demonstrated by the observation that the risk factors were associated with higher costs in uncomplicated patients. Risk factors appeared to influence costs in uncomplicated patients in 2 ways. First, they identified patient comorbid conditions that were more expensive to treat regardless of whether a postoperative complication occurred. Management of an insulin-treated diabetic patient, for instance, is more costly than other patients, and insulin-treated diabetes is one of the NSQIP preoperative risk factors. Second, it is also possible that risk factors predicted costs associated with minor postoperative complications not recorded in the NSQIP. For example, an elevated temperature is not tracked in the NSQIP as a complication but could result in a prolonged hospital stay and may be associated with preoperative risk factor(s). In either case, improved management of the preoperative state could result in cost savings, which has already been proposed, for instance, in the cases of nutritional supplementation16 and hypertension.17 One study on the preoperative optimization of oxygen delivery demonstrated a decrease in complications, length of stay, and cost.18 Because hospitalization before surgery occurred infrequently in our study, it is likely that a process to reduce the number of preoperative risk factors or their severity will need to occur in the outpatient setting.
Risk Adjustment of Costs Using the NSQIP Clinical Cost Profile
The strength of the relationship between preoperative risk and costs suggests that adequate risk adjustment needs to be performed when federal and private payers assess the cost performance of hospitals. As an example, in this study of a tertiary referral center, 1.2% of the patients were on the ventilator before surgery with an average increase in variable direct costs of $36,217 per patient. If this incidence of preoperative ventilator support is high relative to the national mean, it could unfavorably skew the assessment of cost-effectiveness at UKMC.
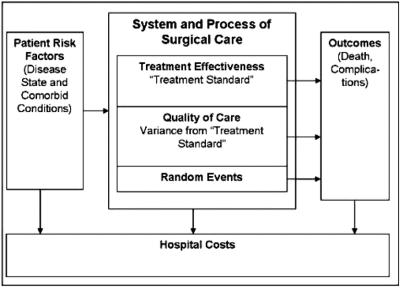
The sensitivity of costs to almost all of the NSQIP clinical risk factors in this study indicates that adequate risk adjustment of costs requires inclusion of significant relevant clinical information, more than that available in administrative datasets. In the same way that the NSQIP model has been shown to be a better predictor of mortality than some administrative datasets, additional studies need to be undertaken to evaluate cost prediction by clinical versus administrative models. Applying the NSQIP outcomes assessment model to costs to adequately adjust for preoperative risk results in the NSQIP clinical cost profile shown in Figure 2.
FIGURE 2. The NSQIP Clinical Cost Profile. Applying the NSQIP outcomes assessment model to costs may more adequately adjust for preoperative risk when assessing hospital surgical cost performance.
In the NSQIP clinical cost profile, outcomes are considered a function of 1) patient-related risk factors, 2) treatment effectiveness, 3) quality of care, and 4) random events.19 Annual statistical analysis of preoperative risk, operative and outcome variables results in a model that estimates outcomes at each site. These estimates become a de facto standard for treatment effectiveness, allowing measurement of variance from that standard and identification of potential areas for quality improvement. Integrating this methodology with costs would result in a cost standard for a particular patient risk profile that more accurately accounts for preoperative cost risk. Variance from this standard would allow for more informed targeting of cost and quality improvement efforts.
Underinformed cost improvement efforts based on the relatively scarce clinical information in administrative datasets could lead to ineffective results or worse, reduction of clinical resources at the point they are needed for both quality care and effective cost improvement. As an example, the insurer United Health is providing incentives to patients who choose “high-quality, low-cost” providers based on the analysis of their claims data. The intent is to improve quality and cost-effectiveness; however, their reliance on claims data for risk adjustment may have ineffective and costly consequences, not the least of which is limiting access to care.20 Likewise, the Center for Medicare and Medicaid Services is actively developing hospital “pay for performance” measures related to surgical outcomes. Again, adequate risk adjustment will need to be performed using a methodology similar to the NSQIP clinical cost profile presented here to avoid unintended adverse consequences on surgical care in America.
Limitations
This study used only one of the 6 operative variables available in the NSQIP for measuring surgical complexity, specifically work RVUs. Inclusion of the other operative variables may have predicted even more cost variation because, in this study, most costs occurred on the day of surgery. Additionally, this study was performed at a single site, UKMC, and therefore caution must be taken in generalizing the findings. This limitation is somewhat ameliorated by the large sample size. Also, the inclusion of 6 different services helped to reduce any service-specific bias.
CONCLUSIONS
The findings of this study demonstrate the importance of including preoperative risk and surgical complexity in addition to postoperative complications when assessing costs in the surgical setting. Understanding their importance could lead to the development of more effective clinical strategies to enhance patient outcomes and reduce costs. For example, preoperative intervention to reduce risk may lead to significant cost savings. Additionally, with the national trend to develop pay-for-performance standards in surgery, in part based on outcomes, it is important to recognize the contribution of preoperative risk to costs. One methodology that could provide an adequate, more clinically robust assessment of surgical costs is the NSQIP Clinical Cost Profile described previously.
ACKNOWLEDGMENTS
The data collection was performed by 2 dedicated and skilled nurse coordinators, Ms. Mary Beth Rice and Ms. Devauna Riley. Part of the data collection for this study was funded under a grant from the Agency for Healthcare Research and Quality through the American College of Surgeons under the direction of the National Surgical Quality Improvement Program.
Discussions
Dr. J. David Richardson (Louisville, Kentucky): I rise to congratulate Mr. Davenport and Drs. Henderson, Mentzer, and Khuri for what I believe is an important and much-needed study which focuses on patient factors such as preoperative risks and complexity of operations required. It seems to me there has been a tacit assumption in many quarters that the high cost of medical care is primarily related to complications and an assumption particularly among payors for health care that such problems are related to inherent quality issues within the health care delivery system itself. Therefore, this paper's findings that preoperative risk factors and operative complexity are much more predictive of cost variability than complications are indeed interesting.
I also congratulate the authors on their use of chart-based data. In the early 1980s, I was part of a project that examined quality outcomes in a number of operations or diseases in every general hospital in Kentucky as a part of a Medicare demonstration project. We examined and published studies on carotid endarterectomy, myocardial infarction, Nissen fundoplication and other operations and serious medical problems. In trying to compare information obtained from administrative and particularly financial data sets versus those from patient charts, we found that administrative data were certainly not reliable in determining issues of quality of care delivered or measuring factors and variables such as complications that would increase costs. As we move forward in the rush to pay for performance, or, as you noted, in the words of one Kentucky insurer, “we want to reward high quality, low cost care,” it is vital that we understand the relative contributions of multiple factors that impact on quality and cost. This paper provides important information in that regard.
I do have a couple of questions for the authors. Several questions relate to a comparison of NSQIP data versus administrative datasets.
Can we or should we expect that NSQIP or other similar data that require chart abstraction will be used on a national level when such data are so much more expensive to collect than administrative data? Do we really get a bang for our buck with NSQIP? Are there ways for NSQIP to track fewer variables and still provide for adequate risk adjustment? Since you did not do, as far as I could tell from looking at the manuscript, any direct comparison of NSQIP to administrative data sets in your patient population, how confident are you that you can really make assertions or assumptions that NSQIP is really superior? Have you in fact done those kinds of studies and just not reported them here?
Secondly, in examining multiple services, were there any surprises or lessons to be learned from a service-by-service analysis?
Finally, “the quartic root transformation” and “transformed costs” does sort of smack of statistical mumbo jumbo and they are generally not used in a lot of these analyses. What is your justification for their inclusion in this study and are they really as accurate as some other methods that might have been used in other studies?
Dr. Robert M. Mentzer, Jr. (Lexington, Kentucky): Dr. Richardson, thank you for your comments and insightful questions. Certainly, the issue of administrative data versus clinical databases is one of controversy, and yet one where I think we as clinicians and surgeons strongly believe that the clinical databases are superior.
With respect to the objective of this particular analysis, it was not our intent to compare administrative data specifically with clinical data. On the other hand, we have almost 20 years of experience comparing clinical and administrative data thanks to colleagues like yourself. There is strong evidence in the literature that the clinical record provides superior and more reliable information than that which comes from administrative databases.
Regarding the costliness of the data, one has to look at both expenditures and the cost savings that result. The whole intent here is to be able to risk-adjust cost outcomes using an NSQIP approach in order to better target cost improvement opportunities. Our own institutional return would suggest that there certainly is “a bang for the buck.” The challenge is to be able to demonstrate this on a national level.
In terms of utilizing fewer variables, over time one would expect that as the NSQIP expands to the private sector, it may be possible that we will be able to reduce the number of variables and still provide adequate risk adjustment. Also, increasing use of the electronic medical record may allow easier and less expensive capture of these variables.
In terms of the service-specific analyses, yes we did perform them. We found that the ability of preoperative risk factors to predict cost variation was greater on an individual service basis, no doubt related to the greater homogeneity of the patient population. But for the purposes of this paper and this presentation, we wanted to emphasize the importance of the relationships across surgical services.
And finally, we do recognize that the log transformation is used more frequently when representing exponentially increasing outcome variables. One reason is that the mathematics of logarithms allows for greater analysis of the effects of individual factors in the resulting models. In this case we were more interested in the overall effects and impact of the three groups of variables. This allowed us to search for the transformation that gave us the best statistical fit of the data both in terms of predictive power and the normalcy of distribution in the residual terms. The quartic root was superior to the log transformation in both counts in our data. The fit demonstrated in the slide presented by Mr. Davenport, which indicated a good correlation between work RVUs, for instance, and transformed costs in over 5000 patients.
Dr. Richard J. Shemin (Boston, Massachusetts): I have 3 quick questions.
Number 1, can you discuss the potential problems with using RVUs, which is very practical, but are RVUs a reliable surrogate for procedural complexity? I notice on the graph there is quite a bit of scatter for every RVU.
Number 2, were you only looking at in-house complications or did you also look at readmissions and later complications within the first 30 days? Depending upon the type of surgery and the type of specialty, you may have underestimated the cost of complications if you did not look at readmissions.
The third question relates to the comment that there was consistent finding among all specialties. I noticed that thoracic and cardiac surgery was only 3.5% of the total group. So was there consistency among all specialties or not?
Dr. Robert M. Mentzer, Jr. (Lexington, Kentucky): Regarding our selection of work RVUs as the measure of surgical complexity, it was 1 parameter out of a possible 15 operative variables recorded in the NSQIP database. Of these, 6 could be alluded to as markers of surgical complexity. The NSQIP Executive Committee compared work RVUs as a measure of surgical complexity to scores developed by groups of subspecialist surgeons and found that work RVUs were the better predictors of morbidity and mortality so we used them here. On the other hand, 1 of the limitations of this study certainly would be that we used only 1 of the 6 available NSQIP markers for surgical complexity.
With respect to 30-day follow-up and hospital readmission, the NSQIP does track readmissions and complications up to 30 days postoperatively, but our analysis only examined the costs related to the primary surgical admission. Thus it may have indeed underestimated total costs. To the extent that the preoperative risk factors predict readmissions, which they do, further analysis that included costs related to readmissions would likely only increase their importance.
In regards to service-specific analysis, we performed the high level modeling only for this study to ensure there were not significant differences in the findings across services. At that level the similarities were striking in the relative predictive power of the risk factors versus complications. However, the service-specific models were more predictive than the all-services models likely due to the increased patient homogeneity as mentioned earlier. More detailed reporting on the various services will be done at a later date. It is important to note that the thoracic surgery cases included in this study are general thoracic cases only and do not include cardiac surgery.
Dr. Carlos A. Pellegrini (Seattle, Washington): One of your conclusions is that understanding the weight of the risk factors in the cost of medical care may increase the amount of money that third parties pay for patients with those risk factors.
Knowing that payers are unlikely to I wonder if it is possible that, as an unintended consequence, this will decrease access to care for a significant portion of the American public because of the existence of risk factors, which would, therefore, increase the costs, and the physician services, et cetera. If you are trying to provide a “more effective cost” you may not wish to have a lot of risk factors in your patient and it may in fact shy away from operating on patients that have significant risk factors, which happen to be the ones that need the operation the most?
Dr. Robert M. Mentzer, Jr. (Lexington, Kentucky): Yes, I think there is always a risk in these kinds of analyses as to whether they are interpreted favorably with respect to access to medical care. The novelty of this particular study is the emphasis of the role of the preoperative risk factors. Our intent would certainly be the development of methods to more effectively manage preoperative risk in order to improve surgical outcomes as well as reduce costs, not the screening out of high-risk patients from care. The result of inadequate risk adjustment in the assessment of hospital and provider cost performance could reduce access to care as well, and we are seeing that in some of the provider profiling across the nation. Clearly, access to care needs to continue to be a priority as we address quality and cost effectiveness.
Dr. William W. Turner, Jr. (Jackson, Mississippi): I fear that the use of charge data in the analysis may have introduced variability that was not considered. Secondly, early mortality in-hospital almost certainly influenced the cost of complications, and I wonder if that was taken into account.
Dr. Robert M. Mentzer, Jr. (Lexington, Kentucky): With respect to estimating costs based on charge data, the TSI cost accounting system used in this study directly allocated costs based on supply and work hour allocation. These cost accounting systems have been shown to be superior to the systems to which I think you are referring which estimate costs based on charges and a charge-to-cost ratio as is done in some studies. There is still no difficulty in determining actual costs and potential cost savings due to any particular clinical action or intervention.
Regarding the impact of postoperative mortality, we have not yet examined its interaction with the other factors in predicting costs but did include it in the complication model. One could theorize that the earlier the death the less cost involved but we have not studied this.
Dr. Jean C. Emond (New York, New York): I congratulate you on this paper. I think it is an important step forward in terms of refining risk adjustment for policy makers.
I have an issue with a statistical choice that either was overtly or implicitly made. I am not sure that you adequately considered the confounding effects of covariates. When you presented the risks such as ventilator dialysis, sepsis, it occurred to me that many of those risks have a high correlation with some of the things that were called complications such as postoperative ventilator, dialysis, sepsis, pneumonia, or preoperative bad lungs. So the question is: Perhaps 1 of the reasons why complications added relatively little to the model is because many of the effects that you were looking at were correlated. Did you consider this effect?
Dr. Robert M. Mentzer, Jr. (Lexington, Kentucky): We did consider the effect and that correlation is the reason that complications alone had more cost predictive power than they added to the risk-factor and complexity model as reported. We also were particularly surprised and impressed by the observation that preoperative risk factors predicted 27% of the cost variability in patients who did not have any complications after surgery. These data indicate preoperative risks impact costs either through their association with increased complications or by directly increasing costs unrelated to complications. The former is the strongest reason we need to risk-adjust complication occurrence rates and their associated costs.
As a technical note regarding preoperative risk factors that may also be classified as postoperative complications, a patient with preoperative pneumonia, for example, in the NSQIP does not have postoperative pneumonia counted as a complication unless a new organism is identified.
Dr. Jean C. Emond (New York, New York): Looking at it the other way as well, patients with few risk factors who had complications might be the group in which to detect the true effect of complications.
Dr. Robert M. Mentzer, Jr. (Lexington, Kentucky): This is an intriguing analytical perspective. We certainly don't want to give the impression that among these 3, 1 of them is not important. But recently we've focused on the postoperative complications as being the primary drivers of cost and therefore the targets for process improvement. Our study indicates we need to focus on the preoperative condition of the patient and the complexity of the operation as well as preventing postoperative complication in our efforts to improve quality and decrease costs.
Dr. Arthur H. Aufses (New York, New York): This is a fascinating study. Two questions which may have been partially answered. These were all incremental costs. What is the incremental cost if a patient has more than 1 preoperative complication? And what is this as an increase over the base cost? You didn't show us any of the base costs without complications.
Dr. Robert M. Mentzer, Jr. (Lexington, Kentucky): We have not yet examined the interdependency of the various factors, so we can't answer the question of, for instance, if you have acute renal failure and diabetes what is the combined effect? The exponential impact on costs of combined factors in the regression model indicates that multiple factors are more than simply additive, but to what degree and what the specific interactions are will be determined in the future.
Footnotes
Reprints: Daniel L. Davenport, MBA, Office of Decision Support, Department of Surgery, University of Kentucky, 800 Rose Street, Lexington, KY 40536-0298. E-mail: dldave0@email.uky.edu.
REFERENCES
- 1.Dimick JB, Chen SL, Taheri PA, et al. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg. 2004;4:531–537. [DOI] [PubMed] [Google Scholar]
- 2.Kalish RL, Daley J, Duncan CC, et al. Costs of potential complications of care for major surgery patients. Am J Med Qual. 1995;10:48–54. [DOI] [PubMed] [Google Scholar]
- 3.Dimick JB, Pronovost PJ, Cowan JA, et al. Complications and costs after high-risk surgery: where should we focus quality improvement initiatives? J Am Coll Surg. 2003;196:671–678. [DOI] [PubMed] [Google Scholar]
- 4.Jencks SF, Williams DK, Kay TL. Assessing hospital-associated deaths from discharge data: the role of length of stay and comorbidities. JAMA. 1988;260:2240–2246. [PubMed] [Google Scholar]
- 5.Iezzoni LI, Shwartz M, Ash AS, et al. Using severity-adjusted stroke mortality rates to judge hospitals: how severity is measured may affect perceptions of hospital performance. Int J Qual Health Care. 1995;7:81–94. [DOI] [PubMed] [Google Scholar]
- 6.Shwartz M, Iezzoni LI, Moskowitz MA, et al. The importance of comorbidities in explaining differences in patient costs. Med Care. 1996;34:767–782. [DOI] [PubMed] [Google Scholar]
- 7.Romano PS, Roos LL, Jollis JG. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol. 1993;46:1075–1079. [DOI] [PubMed] [Google Scholar]
- 8.Malenka DJ, McLerran D, Roos N, et al. Using administrative data to describe casemix: a comparison with the medical record. J Clin Epidemiol. 1994;47:1027–1032. [DOI] [PubMed] [Google Scholar]
- 9.Jollis JG, Ancukiewicz M, DeLong ER, et al. Discordance of databases designed for claims payment versus clinical information systems. Ann Intern Med. 1993;119:844–850. [DOI] [PubMed] [Google Scholar]
- 10.Romano PS, Roos LL, Luft HS, et al. A comparison of administrative versus clinical data: coronary artery bypass surgery as an example. J Clin Epidemiol. 1994;47:249–260. [DOI] [PubMed] [Google Scholar]
- 11.Best WR, Khuri SF, Phelan M, et al. Identifying patient preoperative risk factors and postoperative adverse events in administrative databases: results from the Department of Veterans Affairs National Surgical Quality Improvement Program. J Am Coll Surg. 2002;194:257–266. [DOI] [PubMed] [Google Scholar]
- 12.Fink AS, Campbell DA Jr, Mentzer RM, et al. The National Surgical Quality Improvement Program in non-veterans administration hospitals: initial demonstration of feasibility. Ann Surg. 2002;236:344–353; discussion 353–354. [DOI] [PMC free article] [PubMed]
- 13.Atherly A, Fink AS, Campbell DC, et al. Evaluating alternative risk-adjustment strategies for surgery. Am J Surg. 2004;188:566–570. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Medicare and Medicaid Services (CMS). National Physician Fee Schedule Relative Value File. October 2002. Available at: http://www.cms.hhs.gov/physicians/pfs/RVU02_a.zip. Accessed January 1, 2005.
- 15.Daley J, Khuri SF, Henderson WG, et al. Risk adjustment of the postoperative morbidity rate for the comparative assessment of the quality of surgical care: results of the National Veterans Affairs Surgical Risk Study. J Am Coll Surg. 1997;185:339–352. [PubMed] [Google Scholar]
- 16.Smedley F, Bowling T, James M, et al. Randomized clinical trial of the effects of preoperative and postoperative oral nutritional supplements on clinical course and cost of care. Br J Surg. 2004;91:983–990. [DOI] [PubMed] [Google Scholar]
- 17.Weksler N, Klein M, Szendro G, et al. The dilemma of immediate preoperative hypertension: to treat and operate, or to postpone surgery? J Clin Anesth. 2003;15:179–183. [DOI] [PubMed] [Google Scholar]
- 18.Wilson J, Woods I, Fawcett J, et al. Reducing the risk of major elective surgery: Randomized controlled trial of preoperative optimization of oxygen delivery. BMJ. 1999;318:1099–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Iezzoni LI. Reasons for risk adjustment. In: Iezzoni LI, ed. Risk Adjustment for Measuring Health Care Outcomes. Chicago: Health Administration Press; 2003:1–17. [Google Scholar]
- 20.Rubenstein S. Doctors criticize health insurer over provider-ratings program. Wall Street Journal–Eastern Edition. 2005;245:D3. [Google Scholar]