Abstract
Objective:
This study describes medical students’ perceptions about resident teaching on a surgery clerkship and examines student perceptions before and after the implementation of duty hours regulations (DHR).
Summary Background Data:
There has been much discussion about the impact of DHR on surgical education. One area that merits evaluation is the effect that DHR have had on student education. Learners perceive the clinical teacher role as comprised of 4 roles: teacher, person, physician, and supervisor. This model served as the basis for examining resident teaching before and after DHR.
Methods:
Students completed end-of-rotation evaluations about residents’ teaching effectiveness, amount of feedback, and quality of interactions. Student comments were compiled into individual resident reports, and reports were collected from pre- (2002–2003) and post- (2003–2004) DHR. A coding scheme was developed to describe resident performance in 4 roles: teacher, person, physician, and supervisor. Three coders independently reviewed 124 resident reports maintaining an interrater agreement of 80%. Analyses of variance were conducted to compare data from pre- and post-DHR.
Results:
After implementation of DHR, there were significantly more negative comments (P = 0.005), including comments about residents as supervisor (P = 0.001), teacher (P = 0.027), and teaching activities (P = 0.001). Positive comments about bedside teaching decreased (P = 0.007). Although total positive comments about resident as person increased (P = 0.01), total negative comments about resident as person also increased (P = 0.02).
Conclusions:
Findings of this study indicate that DHR have had a negative impact on medical students’ perceptions of resident teaching. Surgical educators must develop programs that address resident teaching skills in a different environment.
This study describes medical students’ perceptions about resident teaching on a third-year surgery clerkship and examines these student perceptions before and after the implementation of duty hours regulations.
Since the implementation of duty hours regulations (DHR), there has been a great deal of discussion about their effect on surgical education. These regulations were designed to enhance patient safety, resident education, and resident working conditions.1 Researchers have been interested in the effects of DHR on continuity of patient care and resident education,2 and studies have demonstrated the positive impact that DHR has had on patient care3,4 and resident quality of life.2,5 Furthermore, early studies of resident operative experience have indicated that DHR have had no impact on the number of operative procedures residents perform.6,7 Surgical programs have seemingly maintained or enhanced resident education after DHR, and to date, no substantial decrease in clinical or operative experience has been documented.2
In addition to evaluating the effects on resident education, it is important to study the impact of the ACGME's DHR mandate on student education. Surgical residents play a crucial role in educating medical students. It has been shown that students are more satisfied with their clerkship experience when residents actively fulfill their teaching role.8 Many medical and surgical educators have studied clinical teaching roles and teaching effectiveness.9–12 An exploration of learners’ perceptions of the clinical teaching role has yielded a model describing 4 roles of the clinical teacher:
The teacher role—being interested in teaching, making an effort to teach, being available and spending time with the resident, explaining, discussing and answering questions.
Instructor as a person—supportive, easy and fun to work with, helpful, and friendly.
The physician role—the clinical teacher is knowledgeable and clinically competent, is seen as a role model, has good rapport with patients, and has an appropriate attitude.
The supervisor role—the clinical teacher gives the resident responsibility for patient care and opportunities to do procedures, involves the resident, and reviews patients with the resident.12
In evaluating the effects that DHR have had on surgical education, medical students’ experiences cannot be overlooked. The purpose of this study is to describe medical students’ perceptions about surgical residents as teachers and examine students’ perceptions before and after the implementation of DHR.
METHODS
This is a retrospective review of medical student evaluations of their third-year surgery clerkship. This study was approved by the Rush University Institutional Review Board as exempt from continuing review.
Study Sample
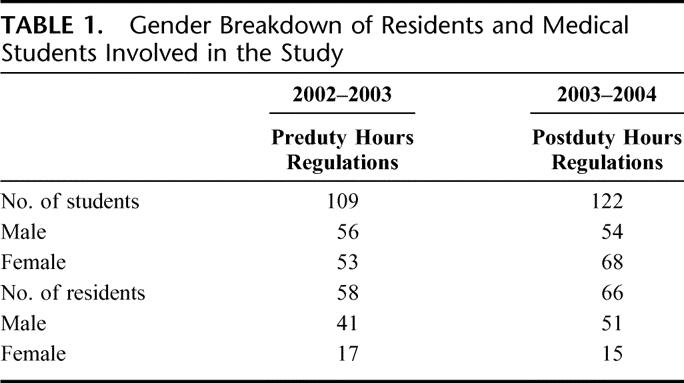
Third-year medical students (M3) rotate through an 8-week surgery clerkship. On the last day of their clerkship, each student is given an end-of-rotation survey to evaluate their experiences and the surgical faculty and residents with whom they worked. In 2002–2003 (pre-DHR), 109 students (56 male, 53 female) completed the clerkship evaluating the 58 residents (41 male, 17 female) with whom they worked. In 2003–2004 (post-DHR), 122 students (54 male, 68 female) completed the clerkship and evaluated the 66 residents (51 male, 15 female) with whom they worked (Table 1). The number of students who evaluated each resident was also tallied on each resident teaching report. In 2002–2003 (pre-DHR), there was an average of 18.8 student evaluations per resident. In 2003–2004 (post-DHR), there was an average of 16 student evaluations per resident. Because this study of resident teaching was conducted over 2 consecutive years, 27 of the residents comprised the study sample in both 2002–2003 and 2003–2004.
TABLE 1. Gender Breakdown of Residents and Medical Students Involved in the Study
Our residents’ teaching performance has traditionally been an emphasis of our program. Surgery residents being evaluated during the study period were prepared for their teaching role in the following manner:
Interns completed Residents as Teachers sessions during their orientation program,
Residents receive annual feedback on their teaching performance through resident teaching reports,
Resident teaching reports are used in each resident's annual performance review with the Program Director and the Educational Specialist, and
Residents have the opportunity to consult with the Educational Specialist regarding teaching concerns or questions. Many residents take advantage of this resource.
Additionally, per a review of resident duty hours reports, the resident work environment pre-DHR included an 80- to 110-hour work week, and post-DHR, a 70- to 85-hour work week.
Instrumentation
End-of-Rotation Survey Instrument
All M3 students at Rush Medical College are required to complete an 8-week general surgery clerkship. All students spend 4 weeks on 2 different general surgery services. During their rotation on these 2 services, the students typically work with at least 10 different surgical residents. At the conclusion of their clerkship, all students are asked to complete a web-based survey about their clerkship experience. One of the questions on the end-of-rotation survey is designed to evaluate individual resident teaching performance, specifically prompting students to describe the “teaching effectiveness, amount of feedback, and the quality of interactions with” each of the general surgery residents with whom they have worked. Each resident name, relevant to their assigned service, is provided next to a space for free text response. The evaluation forms contained no scaled items on teaching behaviors that would be likely to cue responses.9 In addition, the web-based format provided for medical student anonymity. Student comments were compiled into individual resident teaching reports.
Coding Instrument
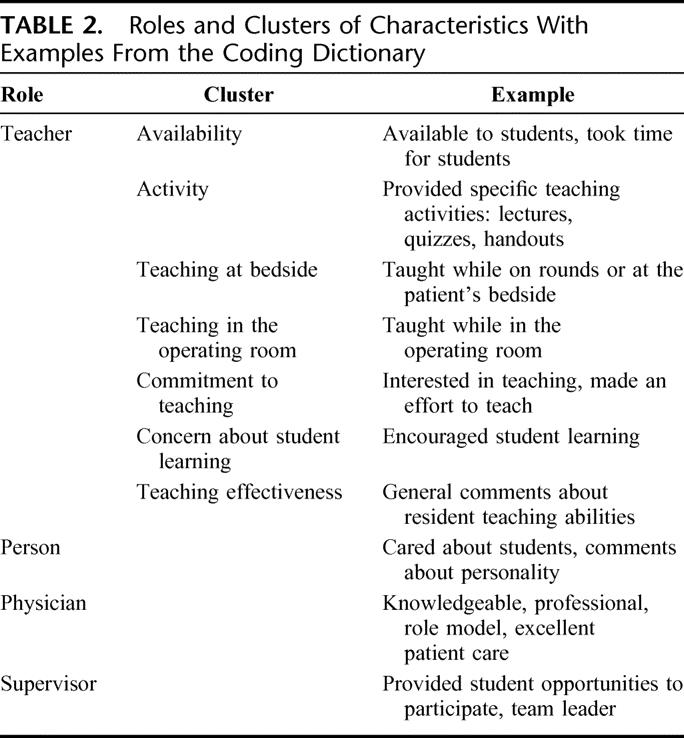
An instrument for coding teaching reports was designed and piloted for use in this study. The unit of analysis for this investigation is the word, phrase, or sentence that expresses a single characteristic or teacher attribute. An initial coding dictionary was constructed using data from the literature on clinical teaching effectiveness along with the coding scheme developed in Ullian's study. The 4 major clinical teaching roles include teacher, person, physician, and supervisor (Table 2). Because our study focuses on teaching behaviors, the role of teacher is subdivided into 7 clusters that expressed similar characteristics of the following categories: availability, specific teaching activities, teaching at bedside, teaching in the operating room, commitment to teaching, concern about students’ learning, and teaching effectiveness. Examples of each are given in Table 2. The coding instrument was piloted on a sample of 6 resident evaluation reports. Pilot data was analyzed to refine the coding system and train coders.
TABLE 2. Roles and Clusters of Characteristics With Examples From the Coding Dictionary
Data Collection
The individual resident teaching reports were collected from the academic years 2002–2003 (pre-DHR) and 2003–2004 (post-DHR). Three coders worked independently to code 124 resident teaching reports that included over 7300 descriptors. The primary coder (PC) coded all evaluation forms. The 2 other coders (coder A and coder B) were trained to use the coding scheme and each coded approximately one half of the resident teaching reports.
Data Analysis
A content analysis was performed on the comments comprising the resident teaching reports. The primary coder coded approximately 462 comments into 210 codes. Each comment was placed into its appropriate category and also classified as positive, negative, or neutral. The dictionary was then revised to fit the data and eventually grew to 239 codes in a total of 11 categories (the 7 teacher clusters, and person, physician, supervisor, and miscellaneous). The miscellaneous category was added to include all the comments that were too vague to be placed into another category. This dictionary was then used as a coding reference for the study.
Interrater agreement between the primary coder and the additional 2 coders was approximately 90% (PC and coder A) and 84% (PC and coder B) with an average reliability of 87.5%. This level of agreement is above the acceptable level of 80% for content analytic research.
The frequencies of the coded units for each category and for each cluster in the teacher role were summed. In addition, analyses of variance were used to compare the results from pre-DHR to the results from post-DHR to determine if the new regulations had an impact on medical students’ perceptions of resident teaching behaviors.
RESULTS
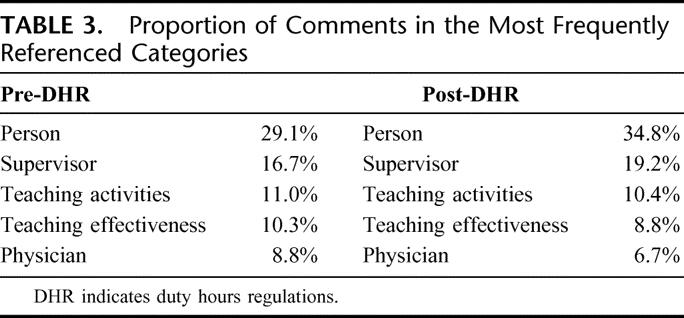
Over the course of both years, medical students’ comments focused on similar components of resident behavior. The 5 most referenced categories were the same before and after the implementation of DHR (Table 3). These top 5 categories include person, supervisor, teaching activities, teaching effectiveness, and physician.
TABLE 3. Proportion of Comments in the Most Frequently Referenced Categories
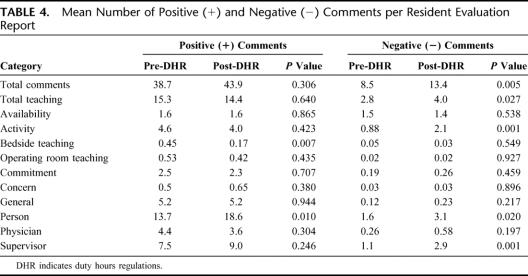
In comparing pre-DHR with post-DHR evaluations, there were significant differences in the number of negative comments in several categories after DHR were implemented. Each of the values listed refers to the mean number of comments per each resident teaching report (Table 4). These include the number of negative comments in the following categories: teacher, teaching activity, person, and supervisor. The mean total negative comments about the residents’ role as teacher (sum of all 7 clusters) increased from 2.8 pre-DHR to 4.0 post-DHR (P = 0.027). The mean total positive comments about the teacher role did not significantly differ (pre-DHR mean = 15.3, post-DHR mean = 14.4, P = 0.64). Second, concerning the teacher role, the number of negative comments made in the teacher activity category increased from a mean of 0.88 pre-DHR to 2.09 post-DHR (P = 0.001). The number of positive comments about teacher activity did not differ significantly (pre-DHR mean = 4.6, post-DHR mean = 4.0, P = 0.423). The number of negative comments about residents’ role as person increased from 1.6 pre-DHR to 3.1 post-DHR (P = 0.02). However, the number of positive comments about residents’ role as person also increased significantly from 13.7 pre-DHR to 18.6 post-DHR (P = 0.01). The number of negative comments about the residents’ role as supervisor increased from 1.1 pre-DHR to 2.9 post-DHR (P = 0.001). There was a significant decrease in the number of positive comments made about residents’ bedside teaching (P = 0.007), declining from a mean of 0.45 pre-DHR to 0.17 post-DHR.
TABLE 4. Mean Number of Positive (+) and Negative (−) Comments per Resident Evaluation Report
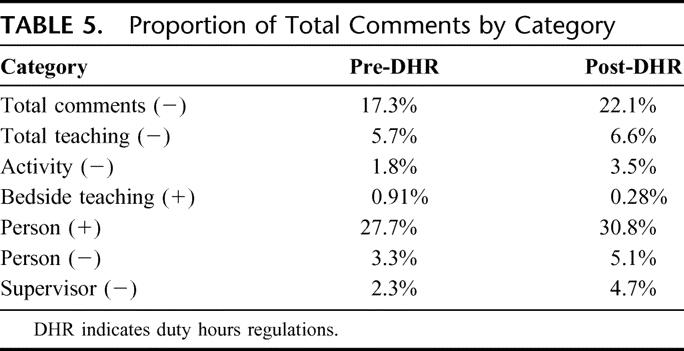
Overall, medical students made more negative comments after the DHR went into effect. The mean number of negative comments per resident report was 8.5 pre-DHR compared with 13.4 post-DHR (P = 0.005). These findings are not likely a result of more total comments made post-DHR because the proportion of negative comments also increased from 17.3% pre-DHR to 22.1% post-DHR (Table 5). Total positive comments increased from a mean of 38.8 pre-DHR to 43.9 post-DHR. However, this value was not statistically significant (P = 0.306). Table 5 depicts the proportion of comments made in each category with a significant change to the total number of comments made throughout.
TABLE 5. Proportion of Total Comments by Category
DISCUSSION AND CONCLUSIONS
Our findings are an interesting addition to the literature on resident teaching. Several others have studied how the interaction with faculty and residents impacts medical students’ educational experience.9–13 Paukert and Richards have documented medical students’ perceptions about clinical teachers as role models.9 They describe how beliefs about clinical role models have positively influenced students’ medical education. Wright and colleagues have demonstrated a strong correlation between contact with role models and the fields that medical students select for residency.13 Students identified 3 important traits that were used to define an “excellent role model” in their study: clinical skills, personality, and teaching ability. Cochran and colleagues obtained similar results in their study of medical students’ perceptions of surgical mentors. Students were asked to describe the characteristics of attending surgeons that were the best mentors.10 The 2 most frequently cited characteristics were “commitment to teaching” and “personality attributes.” Cox and Swanson collected evaluations of their surgery resident teachers over a period of 5 years and describe a superior surgical teacher as someone who:
Demonstrates surgical technical expertise and up-to-date knowledge,
Allows and encourages resident participation in patient procedures, and
Maintains a learning climate of respect and support.11
The results of our study have built on findings about clinical teaching, and indicate a consistent and concerning change in students’ perceptions about the quality and quantity of resident teaching after implementation of DHR. Of greatest concern is the significant increase in negative comments in the teacher, teaching activity, person, and supervisor categories and the significant decrease in positive comments about resident roles as bedside teachers.
Medical students in both years studied seem to emphasize similar aspects of resident teaching. The top 5 most frequently referenced categories did not change across years with most comments being coded into the person 29% (pre-DHR) versus 35% (post-DHR), supervisor 17% (pre-DHR) versus 19% (post-DHR), teaching activity 11% (pre-DHR) versus 10% (post-DHR), teaching effectiveness 10% (pre-DHR) versus 9% (post-DHR) and physician 9% (pre-DHR) versus 7% (post-DHR) roles. Previous studies have shown that medical students refer to similar traits when describing their role models.5 Third-year medical students in our study consistently focus on certain resident teaching traits, and this focus did not seem to change with the shortened resident work week resulting from DHR.
After implementation of DHR, medical students made significantly more negative comments overall (P = 0.005) along with those relating to resident roles as supervisor (P = 0.001) and teacher (P = 0.027). Student perceptions about teaching activities (P = 0.001) and bedside teaching (P = 0.007) were also negatively impacted. The number of negative comments about teaching activities increased post-DHR, whereas the number of positive comments about bedside teaching decreased post-DHR. Although total positive comments about resident as person increased (P = 0.01), total negative comments about resident as person also increased (P = 0.02). The number of positive comments made about the residents’ availability, teaching activity, operating room teaching, commitment to teaching, concern for student learning, teaching effectiveness, and about their roles as physician and supervisor did not significantly change across the 2 academic years. Similarly, there was no significant difference in the number of negative comments about the residents’ availability, bedside teaching, operating room teaching, commitment to teaching, concern for student learning, teaching effectiveness, or their role as physician.
Our findings indicate that although some aspects of resident teaching have not changed, DHR have had a negative impact on medical students’ perceptions of resident teaching. It is encouraging that student references to resident teachers as person are positive, because those traits are difficult to remediate. Furthermore, these traits are important to consider in recruiting residents and valued by faculty, staff, patients, and students. One explanation for this change may be that because duty hours are now restricted, there is simply less time for residents to perform all pre-DHR responsibilities, including the teaching of medical students. Resident contact with medical students remains high, although many different priorities compete for resident time. It is important to ensure, in the face of a changing work environment, that residents are sufficiently prepared and motivated to capitalize on “teachable moments” with students. Residents may need greater support to incorporate student learning activities into their daily work schedule.
Surgery departments will likely continue to rely on residents to serve a major role in teaching medical students. Almost 30 years ago, Lowry declared that resident teaching accounts for approximately one third of the total knowledge that medical students acquire on their general surgery clerkship.14 Since that time, the amount of resident teaching has remained at least as substantial if not a more important component of medical student education. This is supported by several studies, which report that medical students feel that surgery residents are more active teachers than surgical attending physicians.15,16 De and coworkers agree that residents have the important task of teaching medical students the fundamentals of a general surgery service and ensuring that they understand the pre- and postoperative management of a variety of surgical patients.17 Medical students also rely on residents to teach them basic technical skills such as suturing, preparing patients for the operating room, and handling surgical emergencies.15 Because residents play such an enormous role in medical student education, residents need to take time to clearly communicate their expectations to medical students, to increase the amount of teaching in the clinical environment, and to emphasize teamwork.17 How can surgery departments attend to this challenge?
Our findings emphasize the need for enhanced residents as teachers initiatives to address changes in the teaching environment created by DHR. Professional educators and their clinical colleagues have established guidelines and recommendations for successful residents as teachers programs in surgery.18–21 An important starting point in helping residents teach more effectively is to increase resident awareness of the importance of their role as a teacher.8 Needs assessments and well-designed educational programs can help residents define their role as a teacher and improve their teaching behaviors.22 These efforts should be enhanced to prepare residents to be teachers and leaders in the new work environment.22 Residents must be equipped to provide feedback, supervision of clinical skills, and team instructions more efficiently. Surgical residency programs could benefit from collaborations with professional educators to offer programs on how to address these teaching needs. Residents as teachers courses are often highly regarded by residents and are an effective way to enhance skills and raise resident awareness about their teaching responsibilities.18 Resident teaching performance may also be enhanced by receiving and reviewing feedback on their teaching skills. Medical students and faculty can serve as valuable feedback sources for residents so that effective teaching behaviors are reinforced.
In addition to providing greater support to residents in their teacher role, attention must be paid to their role as supervisor. The new constraints on resident time emphasize the need to enhance residents’ time management skills. Residents need to recognize their role as a supervisor and implement their leadership skills. How they organize and manage their surgery service will impact the quality of patient care and the quality of medical student experiences. Effective time management skills will ensure greater availability to teach medical students. Kort and colleagues suggest that transformational change is required to ensure quality patient care and to develop competent surgeons. To meet these goals and comply with the DHR, institutions may need to adopt innovative strategies such as working cooperatively with medical administrators to educate residents on reducing medical errors. For example, a systematic approach to information exchange will benefit surgical teams’ pursuit of excellent patient care as well as communication with students and other team members. In addition, using good demonstrations and mental rehearsal techniques will help residents and students develop technical skills in a manner that is more efficient than the trial-and-error technique.23
Weinstein has recommended a comprehensive review of resident activities and a limit on those activities that lack educational value. Several strategies have been recommended, including the use of improved technology and alternative healthcare providers to minimize some of the “activities that residents perform more often than required for educational purposes.”24 Participants in the Northwestern University Think Tank Consortium on Resident Work Hours25 proposed eliminating a variety of tasks from surgical residents’ clinical responsibilities, including prerounding, moonlighting, first assisting or observing in the operating room on procedures, routine admission and preoperative histories and physicals, discharge paperwork, including discharge summaries, most repetitive service procedures such as blood drawing, and most administrative activities. All “scut work” such as patient transport was also considered expendable. Resident tasks with educational value to be preserved include morning rounds, operative procedures as surgeons and teaching assistant, clinic/office attendance for new and selected established patients, research blocks for 1 year or more, ward-based teaching of junior residents and medical students, effective and efficient transfer of care between resident teams, and personal time. These recommendations are aimed at structuring the surgical residency program so that maximal emphasis is placed on educational activities.
After analyzing the comments that M3 students made on end-of-rotation evaluation of resident teaching, we are encouraged by aspects of resident teaching that remained the same or improved. However, our findings indicate that DHR have had a negative impact on our medical students’ perceptions of resident teaching. In the current era of DHR, there is a clear need for programs to raise resident awareness about the value of their role as teacher and supervisor, to enhance their teaching and leadership skills in a new environment, and to develop alternatives to better serve students’ educational needs. Our departmental efforts to address this issue have included:
An increase in course director communication with residents about their teaching responsibilities;
Increased resident participation in formal student programs such as student orientation, student lecture series, and skills labs;
An enhanced focus on providing midrotation feedback to students;
Initiation of chief residents’ roundtable sessions for senior residents on teaching, evaluation, and team leadership;
Enhanced feedback mechanisms about resident teaching, which incorporates the use of web-based survey technology and the need to hire a clerkship coordinator with educational technology skills;
Continuous program review to monitor resident and student progress; and
Encouragement and support for residents to attend surgical education meetings.
Surgical educators have the responsibility to institute programmatic changes that will best serve student and resident learning. There are several excellent resources available to surgical educators interested in implementing programs to develop and enhance resident teaching and leadership skills. Applying these resources to residents’ academic development will well serve all of the stakeholders in medical education. Resident teachers and leaders will enter the ranks of academic surgery as better prepared faculty members. Enhancing medical student education will attract the best and brightest to surgery and help them become more competent physicians. Moreover, improved medical student education will have obvious benefits for our patients. Our students and our patients deserve the best possible education we can provide.
ACKNOWLEDGMENTS
The authors thank Eulonda Lacy for preparing the resident teaching reports for use in this study.
Discussions
Dr. Leigh A. Neumayer (Salt Lake City, Utah): My congratulations to the authors for designing a study to objectively evaluate the impact of resident duty hour restrictions on medical student teaching, and specifically to Ms. Brasher, because her presence on stage was just amazing for a medical student.
The authors have shown that the concept that residents are seen in the role of person, and I think the manuscript reported it more frequently than as teacher, supervisor, or physician, is consistent with the work of others, including ours from the University of Utah, and in some ways validates this data set. The authors, however, seem to take “the glass is half empty look” at their data rather than “the glass is half full.” I would like to point out to you some of the positives in their study.
The commitment and availability of the residents to teach did not change despite the decrease in resident duty hours. The OR teaching and bedside teaching however scant only decreased a little bit. Bedside teaching had a slight increase in comments. And the residents concern for the students did not seem to change. Additionally, the increase in positive comments about the resident's person increased by 5 comments per resident while the negative increased only by 1.5.
I have several questions for the authors, varying from very concrete to rhetorical.
Was there a change in the overall rating of the resident or of the clerkship between the 2 years studied, or in the comments of individual residents that had to have been in your program for both of those years?
Second, what percentage of the 2 medical student classes who completed these evaluations chose careers in surgery? Did they differ in their evaluations; ie those who surgery, did they evaluate the residents more positively than those who didn't?
Number 3, did you have attending surgeon evaluations for the same time period and how did these change?
Number 4, were there any differences in the comments between the junior residents and the senior residents?
Number 5, based on your data do you plan on any interventions to improve the results? I think you already do more at Rush than most of us do in our programs for residents.
Six, with duty hours regulations should we be relying on the residents to do most of the teaching of our medical students? Do they really have the time?
And lastly, could your results reflect a generational change rather than the effect of duty hour restriction?
Dr. Linnea S. Hauge (Chicago, Illinois): Thank you, Dr. Neumayer, for your insight. I agree with you that helping residents to change their teaching activities is going to be much easier than trying to change their commitment or concern about teaching. That tends to be more what you get when you recruit residents than what you can help them with when they get to you.
I appreciate the questions on student outcomes. The 2004 class, which is our preduty hours group, had 23% of students choosing to do surgery. Nine percent of that class actually entered general surgery. With the postduty hours group, only 20% of the class entered surgery, but 9.3% of them entered general surgery. So a cursory review of that is there doesn't seem to be a difference. What those numbers don't typically capture, though, is the students we missed perhaps that were interested in surgery when they arrived to the university.
Our miniboard performances don't appear to be different either. The preduty hours mean was 69.6, the postduty hours mean was 71.4. The comparable group national average for 8-week clerkships is 70.4 with a standard deviation of 8. So we are not too concerned about their performance being impacted yet.
However, as you suggest, our residents do need some attention in this. And some of the plans that we have for them are, first of all, to continue to reward their teaching. Each year we give awards for junior and senior resident teaching, a recognition based on resident teaching reports. We have a long-held value in our program for rewarding teaching.
A couple years ago, 1 of our residents earned the Inaugural Award given by the American College of Surgeons for resident teaching, and for the third consecutive year the Rush Medical College graduating class will give the resident teaching award for the entire institution to a surgery resident. The finalists this year were both surgery residents.
So we have some positive things happening. But we do need to make some changes in helping our residents prepare better for more compressed days.
First of all, they need to teach differently. The luxury of sitting down with a team for a long period of time is, by and large, a thing of the past and they will need to teach in smaller segments more frequently. We will design this into our Internal Orientation course.
We will also be redesigning our chief orientation program for PGY 3 through 5 residents because they are the people who establish that team dynamic quickly. And those changes will include a focus on leading teams, setting expectations, and providing important feedback.
Dr. Christopher C. Baker (Boston, Massachusetts): Once again congratulations on a superb presentation. I guess I will carry Dr. Neumayer's “our glass is half empty” versus “half full” comment a little bit further. George Carlin said “the glass is twice as big as it needs to be.” And maybe that is part of the problem with the 80-hour workweek.
One comment to follow up – Dr. Polk mentioned this yesterday and I think it needs to be mentioned again – is that the 80-hour workweek has required of us a paradigm shift, and yet we have not made a paradigm shift, in the way we handle information between residents, among residents, and the way in which we teach students.
So my question relates to something you alluded to. When I was at UNC for the last 13 or 14 years we had a resident teacher course that Dr. Sheldon instituted. I think it was one of the earliest in the country. I would ask you what components you plan to change in that course in order to address these issues?
Dr. Linnea S. Hauge (Chicago, Illinois): Most of our work will be dealing with how they can teach in a quick way. The 1-minute preceptor model for medical education may be something that needs to be adopted for our surgery residents. Providing feedback and setting expectations are also 2 other activities that students value, and they are tasks that can be done on the fly.
Dr. David I. Soybel (Boston, Massachusetts): I wanted to ask 3 questions in order to make sure that we are not misinterpreting the information that you have given us.
There is no doubt that there is collateral damage coming out of this change. But I wonder whether the disruption itself, the change in the routine, the change in routine structure or dynamic, is in fact the problem. I think all of us know anytime we go forward with a major change in the structure of a residence team or its activities, there could well be some unintended consequences, which then you follow over time, monitor as you do, and then propose solutions. So I am not sure that the constriction of time is necessarily the culprit here, likely, but not necessarily.
The second question, to follow up on Dr. Neumayer's question, is whether there is some sort of control? For example, do you have comments about attending teaching and whether or not comments about attendings did not change in the same way? Presumably it would not have changed it because their interactions are similar to the students before and after the 80-hour workweek.
Lastly, I just wanted to ask you, knowing this information that there is in fact a negative perception about teaching of the residents, and begging the question that Dr. Neumayer asked also about whether residents have the time to teach, my question is, have you thought about restructuring the team's activities so that in fact the students are part of the team and can actually get a lot out of that interaction? Otherwise, I fear they won't know how to be a member of the team when they get to be residents.
Dr. Linnea S. Hauge (Chicago, Illinois): I will take the last question first. The restructuring of the teams may not be necessary, but making certain that each of the chief resident leaders has the same approach to involving the team, I think, is important. We probably have some variation there.
Regarding the data about faculty, we do collect data about faculty in the same manner we do with residents, individually. And we will be looking at that data and hope to have some findings to report in the coming year.
Dr. Julie Ann Freischlag (Baltimore, Maryland): What I have noticed with young students and residents mainly came from watching my 10-year-old son, who actually uses his GameBoy more than he likes to read a book. And if you look at the way we are progressing in surgical training, he is going to be very good on the robot and I am going to be worthless because I would still rather read a book.
My students and my residents love electronics and they love media. We have developed web sites. We videotape our lectures. We have them up working on simulators and on the robots. Have you thought about having teaching aids like that, that actually the students might like better? The residents certainly are much better at doing it. And it can actually cut down on what time you need. Because they can watch the movie of the operation the night before, they can get on the web site and they can actually watch a talk that a professor at grand rounds gave which we are videotaping. Then the next day, the 15 minutes they have with me or the resident, they have already seen an hour lecture and therefore they are better prepared to be taught the next day.
Dr. Linnea S. Hauge (Chicago, Illinois): That is a good point that perhaps our learners are not as tolerant of passive learning activities as we have been and the hands-on approach to teaching is much more important to them. We have begun to incorporate in our Thursday morning skills lab simulators, both high tech and low tech kinds of tasks that I think our students have really enjoyed. That has been a greater part of their learning experience in the past year.
Prof. J. Hans Jeekel (Rotterdam, Netherlands): Should the residents have a teacher role? Or should we take that off their shoulders – because of the dramatic reduction in working hours to 80 hours, which is in Europe by law an unacceptable amount of hours. We had to restructure our resident program because of the reduction in hours. Should you take the task of teaching from the shoulders of the residents and reconstruct the training of the resident?
Dr. Linnea S. Hauge (Chicago, Illinois): That is a good question. There was a paper published in Surgery by DaRosa, Bell, and Dunnington on their Think Tank Consortium on Shortened Work Hours that listed a number of tasks that need to stay on the table for residents, those things that can be moved, and those things that should be eliminated.
I think we are in agreement with them that resident teaching needs to stay on the table. These residents are the people we are preparing to serve in your roles. We know that role modeling is very important and residents do need interaction with students. In our current structure of surgery teams it will be really difficult to avoid. So we see them as an important part of our teaching program.
Footnotes
Reprints: Aimee Elizabeth Brasher, BS, 1117 W Vernon Park Place, Unit B, Chicago, IL 60607. E-mail: Aimee_Brasher@rush.edu.
REFERENCES
- 1.Steinbrook R. The debate over residents’ work hours. N Engl J Med. 2002;347:1296–1302. [DOI] [PubMed] [Google Scholar]
- 2.Hassett JM, Nawotniak R, Cummiskey D, et al. Maintaining outcomes in a surgical residency while complying with resident working hour regulations. Surgery. 2002;132:635–639. [DOI] [PubMed] [Google Scholar]
- 3.Gaba DM, Howard SK. Fatigue among clinicians and the safety of patients. N Engl J Med. 2002;347:1249–1255. [DOI] [PubMed] [Google Scholar]
- 4.Lockley SW, Cronin JW, Evans EE, et al. Effect of reducing interns’ weekly work hours on sleep and attention failures. N Engl J Med. 2004;351:1829–1837. [DOI] [PubMed] [Google Scholar]
- 5.Awad SS, Fagan S, Cameron K, et al. The Impact of the 80 hour work week policy on surgical resident quality of life. J Am Coll Surg. 2004;199(suppl):S74. [Google Scholar]
- 6.Bair S, Hauge L, Oleske D, et al. The Effect of Duty Hour Regulations on Resident Operative Experience. Poster presented at the Rush Research Forum; April 2004; Chicago, IL.
- 7.Spencer AU, Teitelbaum D. Surgical residents’ operative experience: impact of the 80-hour work week. J Am Coll Surg. 2004;199(suppl):S74. [Google Scholar]
- 8.Bing-You R, Edwards J. Residents as teachers. Teaching and Learning in Medical and Surgical Education. 2000:169–182. [Google Scholar]
- 9.Paukert J, Richards B. How medical students and residents describe the roles and characteristics of their influential clinical teachers. Acad Med. 2000;75:843–845. [DOI] [PubMed] [Google Scholar]
- 10.Cochran A, Paukert J, Scales E, et al. How medical students define surgical mentors. Am J Surg. 2004;187:698–701. [DOI] [PubMed] [Google Scholar]
- 11.Cox S, Swanson M. Identification of teaching excellence in operating room and clinic settings. Am J Surg. 2002;183:251–255. [DOI] [PubMed] [Google Scholar]
- 12.Ullian J, Bland C, Simpson D. An alternative approach to defining the role of the clinical teacher. Acad Med.1994;69:832–838. [DOI] [PubMed] [Google Scholar]
- 13.Wright S, Wong A, Newill C. The impact of role models on medical students. J Gen Intern Med. 1997;12:53–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lowry SF. The role of house staff in undergraduate surgical education. Surgery. 1976;80:624–628. [PubMed] [Google Scholar]
- 15.Pelletier M, Belliveau P. Role of surgical residents in undergraduate surgical education. Can J Surg. 1999;42:451–456. [PMC free article] [PubMed] [Google Scholar]
- 16.Minor S, Poenaru D. The in-house education of clinical clerks in surgery and the role of housestaff. Am J Surg. 2002;184:471–475. [DOI] [PubMed] [Google Scholar]
- 17.De SK, Henke P, Ailawadi G, et al. Attending, house officer, and medical student perceptions about teaching in the third-year medical school general surgery clerkship. J Am Coll Surg. 2004;199:932–942. [DOI] [PubMed] [Google Scholar]
- 18.Rockey P, Dunnington G, DaRosa D. A Multidisciplinary approach to teaching residents to teach. Acad Med. 2000;75:545. [DOI] [PubMed] [Google Scholar]
- 19.Wipf JE, Pinsky LE, Burke W. Turning interns into senior residents: preparing residents for their teaching and leadership roles. Acad Med. 1995;70:591–596. [DOI] [PubMed] [Google Scholar]
- 20.Edwards J, Friedland J, Bing-You R. Residents’ Teaching Skills. New York: Springer; 2002. [Google Scholar]
- 21.Morrison E, Friedland J, Hitchcock M, et al. The residents’ teaching skills website. Available at: http://www.residentteachers.com. Accessed March 4, 2005.
- 22.DaRosa D, Folse R, Sachdeva A, et al. Description and results of a needs assessment in preparation for the ‘surgeons as educators’ course. Am J Surg. 1995;169:412–415. [DOI] [PubMed] [Google Scholar]
- 23.Kort KC, Pavone LA, Jensen E, et al. Resident perceptions of the impact of work- hour restrictions on health care delivery and surgical education: time for transformational change. Surgery. 2004;136:861–871. [DOI] [PubMed] [Google Scholar]
- 24.Weinstein DF. Duty hours for resident physicians-tough choices for teaching hospitals. N Engl J Med. 2002;347:1275–1277. [DOI] [PubMed] [Google Scholar]
- 25.DaRosa D, Bell R, Dunnington G. Residency program models, implications, and evaluation: results of a think tank consortium on resident work hours. Surgery. 2003;133:13–23. [DOI] [PubMed] [Google Scholar]