Abstract
Objective:
We hypothesized that surgeon productivity is directly related to hospital operating margin, but significant variation in margin contribution exists between specialties.
Summary Background Data:
As the independent practitioner becomes an endangered species, it is critical to better understand the surgeon's importance to a hospital's bottom line. An appreciation of surgeon contribution to hospital profitability may prove useful in negotiations relating to full-time employment or other models.
Methods:
Surgeon total relative value units (RVUs), a measure of productivity, were collected from operating room (OR) logs. Annual hospital margin per specialty was provided by hospital finance. Hospital margin data were normalized by dividing by a constant such that the highest relative hospital margin (RHM) in fiscal year 2004 expressed as margin units (mu) was 1 million mu. For each specialty, data analyzed included RHM/OR HR, RHM/case, and RHM/RVU.
Results:
Thoracic (34.55 mu/RVU) and transplant (25.13 mu/RVU) were the biggest contributors to hospital margin. Plastics (−0.57 mu/RVU), maxillofacial (1.41 mu/RVU), and gynecology (1.66 mu/RVU) contributed least to hospital margin. Relative hospital margin per OR HR for transplant slightly exceeded thoracic (275.74 mu vs 233.94 mu) at the top and plastics and maxillofacial contributed the least (−3.83 mu/OR HR vs 9.36 mu/OR HR).
Conclusions:
Surgeons contribute significantly to hospital margin with certain specialties being more profitable than others. Payer mix, the penetration of managed care, and negotiated contracts as well as a number of other factors all have an impact on an individual hospital's margin. Surgeons should be fully cognizant of their significant influence in the marketplace.
Key Words: hospital margin, relative value units, operating room productivity, hospital financial data, surgeon productivity, surgeon contribution to hospital margin
Operating room data and hospital financial data were analyzed during fiscal year 2004 to determine what relationships existed between surgeon productivity and hospital margin.
The traditional mission of an academic medical center is a 3-tiered goal to engage in tertiary clinical care, education, and research. However, the decline of the fee-for-service reimbursement system, the encroachment of managed care, the cost-containment strategies of payers, and the malpractice crisis have all contributed to the increasing difficulty of sustaining and fulfilling this mission. In addition, in the past 2 years, both academic medical centers and physician practices have had to cope with the imposition of resident work hour limitations, forcing many hospitals and practices to hire costly nurse practitioners and physician assistants to perform the work lost because of the duty hour restrictions.1 The cost to employ these healthcare providers is significantly greater than that expended for a resident, and it effectively takes 4 of these individuals to compensate for the loss of a single resident from a clinical service, often mandated by the shifts required in resident allocation to compensate for the lost work hours. These nonphysician providers work only one-half the number of hours as a resident and usually see only one-half as many patients.
Both hospitals and physician practices are suffering as reimbursement continues to fall, costs continue to climb, and the malpractice crisis looms large. Many academic medical centers are struggling financially as a result of the current environment, and if financial conditions do not improve, the traditional academic mission may be forced to change.2 From a financial standpoint, options include further reductions in costs or even elimination of certain service lines found to be unprofitable. Although possible on a small scale, widespread adoption of this kind of policy would truly jeopardize the mission of academic medical centers across the country.
The resource-based relative value system (RBRVS) was instituted in the late 1980s as Medicare set out to contain increasing costs in the healthcare system. However, several academic institutions have demonstrated that the system reimburses too little such that hospitals and practices may be losing money by performing certain types of procedures. The RBRVS system was instituted with the goal of containing costs, but the calibration was not intended to reimburse below costs. One obvious explanation for this discrepancy is that physician effort has been underestimated and thus underpaid. In addition, because academic medical centers usually are in the position that they accept all patients as part of their mission and thus tend to have more complex, more highly variable, and more costly cases than community hospitals, they have higher financial risk that is inadequately compensated by the RBRVS.3
Costs continue to increase and reimbursement remains inadequate. Although many academic medical centers continue to focus on cost containment at a macro level, there has been inadequate investigation into the relationship between hospital margin and the clinical practices. An unfortunate explanation for this is that most hospitals do not have adequate cost-accounting systems, and the information that is shared between medical centers and clinical practices is insufficient. Taheri and colleagues rigorously examined a trauma service line margin, finding that although losses were rare on fee-for-service patients, they were common on fixed-fee patients.4 This group proposed that payers potentially could game the system by moving patients to hospitals in which they had more favorable contracts, using as an example their own medical center where a fixed-fee trauma patient, on average, would result in a $500 loss for the hospital and trauma service. Academic medical centers are vulnerable to this kind of strategy by payers because of their obligation to accept all patients.
Medical centers and practices across the country are putting considerable effort into cost containment, but as a result of the complexity of clinical care and the separation of hospital and practice operational data, little is known about what case mixes are profitable for practices, medical centers, or both. Because most hospitals and surgical services have only crude cost-accounting systems, neither hospitals nor practices have enough information to make appropriate and advantageous strategic decisions, giving payers a clear information advantage. As the financial situation becomes more precarious for both practices and medical centers, this information becomes increasingly important. Standard operational management from other industries demonstrates that optimizing a value chain in its entirety is always the best financial strategy for a whole system. Increasing the transparency and accuracy of the cost-accounting systems for both practices and hospitals, in addition to sharing more information, should lead us closer to this goal.
The question remains which specialties produce high margins on the professional fee side and which produce high margins on the hospital side. Although few academic medical centers likely would consider managing risk by dropping entire surgical service lines, this information would allow hospitals and practices to see where better-negotiated reimbursement contracts need to be created, where further cost cutting might be most helpful, and where resources should be allocated. At a minimum, those service lines with high margins for both the hospital and the practice should be strongly supported, whereas those with negative margins for both should be more closely monitored. In certain situations, depending on the employment model, this creates a need for transfer of dollars between the institution and individual practices. This becomes particularly important for those services providing a high margin to the hospital where the professional fees generated do not adequately support the individual practitioners. Unfortunately, this situation is becoming all too common among surgical specialties where hospital reimbursement has remained strong and the Medicare payment to the practitioner has continued to be cut on a yearly basis. It is well known that other third party payers tend to follow Medicare's lead when it comes to physician reimbursement, thus creating the crunch on the professional fee side that the majority of surgeons now face. It is a sad commentary when the costs to a cardiac surgical practice exceed the payment received for performing a coronary artery bypass, a situation that currently exists in a number of regions in this country. Cardiac surgery, as well as a number of other surgical specialties, has provided a particularly vulnerable target to professional fee reductions despite the best efforts of the specialty societies to resist these changes. The dichotomy that exists between hospital reimbursement and professional fees has to be addressed, in many situations, by a funds flow model, and surgeons should be aware of their leverage when entering into negotiations regarding these types of models.
METHODS
All operative cases performed at the Hospital of the University of Pennsylvania in fiscal year 2004 (FY04) were recorded in the operating room case log database. Data were available for surgical specialties, including neurosurgery, cardiac surgery, gynecologic surgery, otorhinolaryngology, endocrine and oncologic surgery, transplant surgery, urologic surgery, vascular surgery, plastic surgery, thoracic surgery, orthopedic surgery, trauma surgery/surgical critical care, oral maxillofacial surgery, gastrointestinal surgery, and colorectal surgery. Pediatric surgery and ophthalmology cases are performed outside of the Hospital of the University of Pennsylvania and thus are not included. Urology clinic procedures were included in the study, because they use the operating room case log database. However, plastic surgery and oral and maxillofacial surgery clinic procedures, performed outside of the operating room, are not included in this study. These cases represent a small minority of cases for those specialties, however.
Operative case length (patient in room to patient out of room) and scheduled Current Procedural Terminology (CPT) codes were obtained from the case log database for each case performed in FY04. Using the April 2004 Revision file (www.cms.hss.gov/providers/pufdownload/rvudown.asp), the resource-based relative value scale (RBRVS) scale was used to translate each scheduled CPT into total relative value units (RVU).5 Operative statistics were available on cases in the operative log, but not from the hospital billing system. To verify that the scheduled case RVU and billed RVUs were correlated, total RVUs calculated from scheduled CPT versus billed CPT for all cases in FY04 were compared by linear regression, with R2 = 0.70 and P = 0.0000, so scheduled CPTs were used in all further calculations. Therefore, neither postprocedure coding optimization nor secondary procedure codes were captured. However, because the RVUs corresponding to billed CPT codes correlated closely with those corresponding to the scheduled primary procedure CPT codes, this method is not only valid, but provides advantages, including the ability to link RVUs to operating room data, the fact that no differences in postprocedure optimization strategies by specialties interfere with the analysis, and the fact that many payers put much or all weight on the primary procedure for reimbursement.
Total operating room (OR) time was calculated for each specialty by summing the OR case length for every procedure performed in FY04. Annual cumulative RVU was calculated for each specialty by adding the total RVUs performed by each surgeon. RVU/OR HR was calculated for each specialty by dividing the total cumulative RVUs by the total OR time used by each individual surgeon and specialty.
The hospital finance department calculated hospital margin for fiscal years FY03 and FY04 for each clinical division and department based on primary physician specialty. Margin, as used here, is defined as what remains after subtracting both direct and indirect costs from the operating revenue collected by specialty. Revenue used in calculations included all payments collected for each patient, including payments for preadmission testing, operative services, and postoperative care. No attempt was made to divide the hospital diagnosis-related group (DRG) payment between services, but instead the entire DRG payment and the entire cost of the patient stay in the hospital was allocated to the primary service. Costs are assigned to each patient using standard costing methods for healthcare organizations. Nursing costs are assigned using the average cost per day and the length of stay of each patient on each specialty specific patient floor. Operating room costs are allocated to patients based on the individual case time multiplied by the average cost per OR minute. High-cost devices and implantables are not included in the OR time-based averages, but instead specifically assigned to each patient. Ancillary testing is allocated using hospital department-specific costs per RVU multiplied by the actual RVUs each department provided. All of these costs are summed to come up with direct patient care costs. Indirect costs are assigned to patients using standard stepdown method of cost accounting used for Medicare cost reporting to the Center for Medicare and Medicaid Services (CMS). Indirect costs include, most significantly, overhead of operations and administration, interns and residents, building and equipment depreciation, housekeeping, dietary, and other space-related costs.
In FY04, neurosurgery was the most profitable specialty overall for the hospital. To maintain some level of confidentiality for the University of Pennsylvania Health System that kindly provided the type of financial information rarely provided to physician practices, we devised a relative hospital margin (RHM) that is calculated by dividing true hospital margin by a constant to normalize all specialty hospital margins such that the margin for neurosurgery was 1 million margin units (mu). We have chosen not to use the dollar sign because we are referring to a relative margin, and not dollars of margin and thus use the term margin unit. The comparison between specialties and the magnitudes of each value remain valid, although we are not referring directly to dollars of hospital margin. Relative hospital margin per RVU was calculated by dividing total annual relative margin by total annual RVU for each specialty. Relative hospital margin per case was calculated by dividing total annual relative margin by total number of cases performed by each clinical service in FY04. Relative hospital margin per OR HR was calculated by dividing total annual relative margin by the sum of all cases performed by each specialty in FY04. JMP software (JMP IN 4; SAS Institute, Cary, NC) was used to perform linear regressions for RHM and annual divisional RVU, average RVU per case, and average RVU per OR HR.
For all calculations, average institutional quantities reflect mean values with all individual specialties weighted equally. For all figures containing quadrants, boundary lines represent mean values for both axes.
RESULTS
Fifteen surgical services at our institution performed 21,050 cases in FY04. The average number of cases per service was 1403 (standard deviation [SD] = 772) with a range from 509 (oral maxillofacial surgery) to 3161 (urology). As shown in Table 1, the total annual RVUs for all operative cases was 461,671 with a mean 30,778 per clinical service (SD = 16,263). Cumulative annual RVUs per service ranged from 9849 (oral maxillofacial surgery) to 67,220 (neurosurgery). The mean number of RVUs per case for the institution was 24.49 (SD = 12.88) with a range of 9.04 (urology) to 57.12 (transplant).
TABLE 1. Relative Value Units (RVUs) Were Determined From Scheduled Current Procedural Terminology Codes for Every Operative Case During Fiscal Year 2004
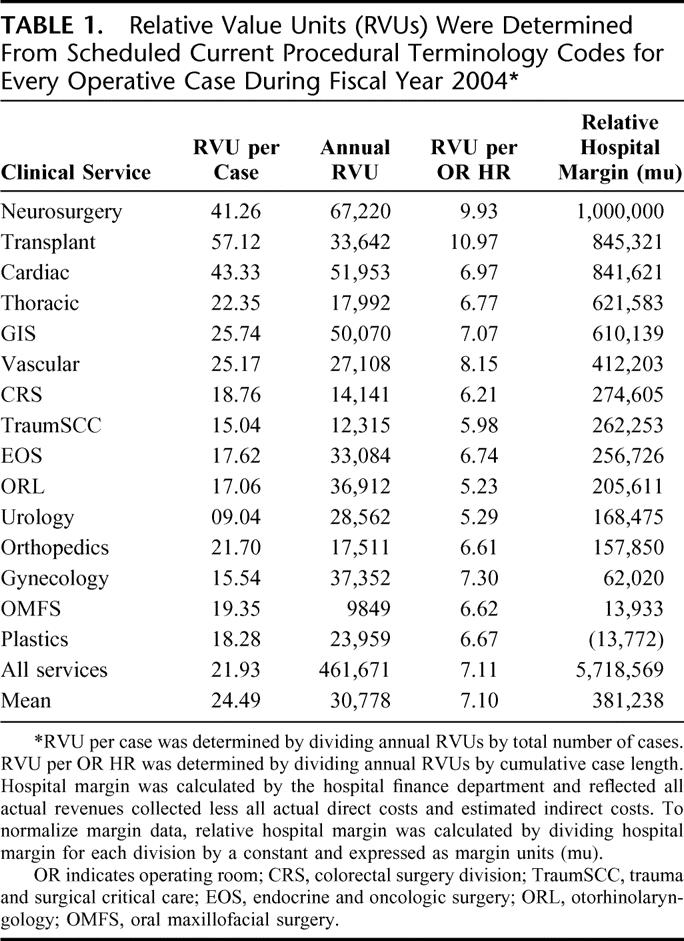
The total cumulative operating room time (time in room to time out of room) used in FY04 was 64,905 hours. The OR time used by each clinical service ranged from 1489 hours (oral maxillofacial surgery) to 7451 hours (cardiac surgery) with a mean of 4327 hours (SD = 2054). Average case length (total cumulative operating room time divided by total number of cases) ranged from 1.71 hours (urology) to 6.15 hours (cardiac surgery) with a mean of 3.32 hours (SD = 1.14). The mean number of RVUs per OR HR for the institution was 7.10 (SD = 1.56) and ranged from 5.23 (otorhinolaryngology) to 10.97 (transplant).
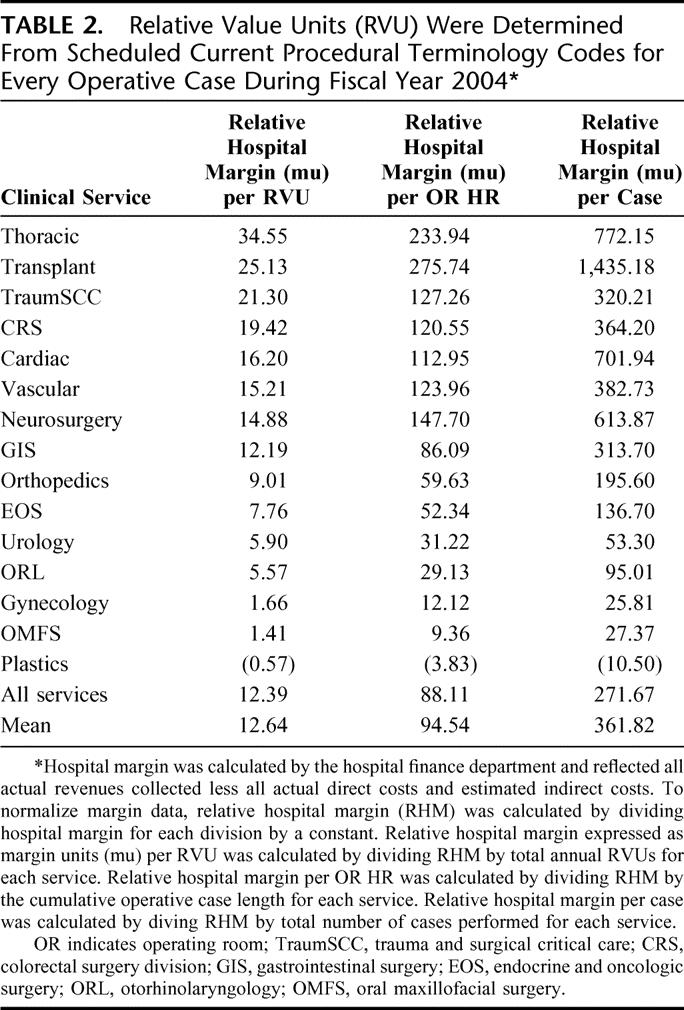
Relative hospital margin (RHM) expressed as margin units (mu) in FY04 ranged from a loss of 13,772 mu (plastic surgery) to a gain of 1,000,000 mu (neurosurgery) with overall institutional RHM of 5,718,569 mu. The mean RHM per service was 381,238 mu (SD = 325,270). As shown in Table 2, the mean RHM per RVU for the entire institution was 12.64 mu (SD = 9.76), with services ranging from a loss of 0.57 mu per RVU (plastic surgery) to a gain of 34.55 mu per RVU (thoracic surgery). The mean RHM per OR HR was 94.54 mu/h (SD = 81.56) with a range of (3.83) mu/h (plastic surgery) to a gain of 275.74 mu/h (transplant surgery) (parentheses around a number indicates a loss). On a per-case basis, the mean institutional RHM per case was 361.82 mu (SD = 388.42) ranging from (10.50 mu) per case (plastic surgery) to a gain of 1435.18 mu per case (transplant surgery).
TABLE 2. Relative Value Units (RVU) Were Determined From Scheduled Current Procedural Terminology Codes for Every Operative Case During Fiscal Year 2004
Hospital margin includes revenue only from cash actually received and finalized financial data lags behind operative data by at least several months, and perhaps up to 6 months. Thus, when we initially looked at the operative data for FY04, the FY03 hospital finance data were used rather than the FY04 data now available. It was proposed at that time that there should be strong correlation between relative hospital margin per service on a year-to-year ongoing basis. This is demonstrated in Figure 1, which shows an R2 of 0.88 and P < 0.001.
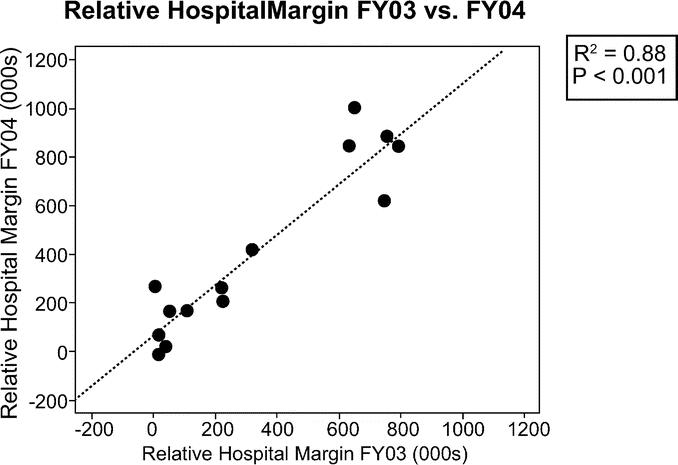
FIGURE 1. Relative hospital margin (RHM) in margin units (mu) for FY03 and FY04 were calculated by the hospital finance department and reflect all actual collected revenue less all direct and indirect costs, normalized by the same constant for both years. The relative hospital margins for these 2 years were closely correlated with R2 = 0.88 (P < 0.001).
As shown in Figure 2, relative hospital margin and annual RVUs per specialty are correlated with R2 = 0.44, P < 0.007, demonstrating that although there is a positive correlation between total hospital margin and annual departmental RVUs, this correlation explains less than half of the total variability. Some specialties such as neurosurgery are clear winners for both the hospital and generate significant RVU production. Other services such as oral and maxillofacial surgery add little to the hospital margin and result in relatively few annual RVUs. However, there were some services that add substantial hospital margin but generated fewer RVUs (thoracic surgery) and others that produced above-average RVUs but contribute little to overall hospital margin (gynecologic surgery).
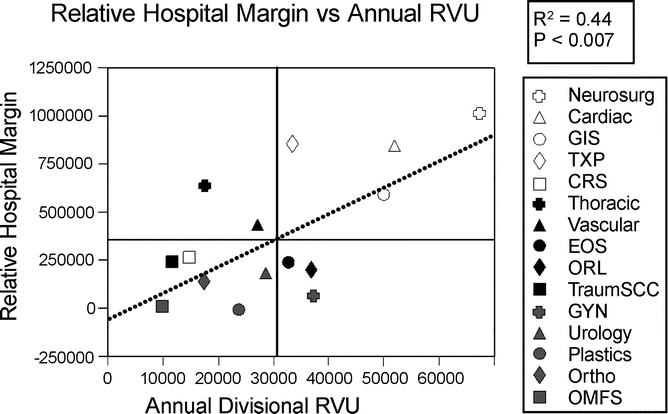
FIGURE 2. There is a significant positive correlation between relative hospital margin (RHM) (mu) and annual cumulative RVU for each surgical service, with R2 = 0.44 and P < 0.007. Quadrant boundaries reflect mean RHM and annual RVU for the clinical services, with mean RHM 381.238 mu and mean annual RVU 30,778. GIS, gastrointestinal surgery; TXP, liver, kidney, and pancreas transplant surgery; CRS, colorectal surgery; EOS, endocrine and oncologic surgery; ORL, otorhinolaryngology; TraumSCC, trauma and surgical critical care; GYN, gynecologic surgery; Ortho, orthopedic surgery department; OMFS, oral maxillofacial surgery department.
Part of the variation in Figure 2 can be explained by the fact that some services provide greater hospital margin per RVU than others. As shown in Figure 3, relative hospital margin per RVU varies greatly. For the institution, the mean RHM per RVU was 12.64 mu (SD = 9.76) with a range of (0.57) mu/RVU (plastic surgery) to 34.55 mu/RVU (thoracic surgery).
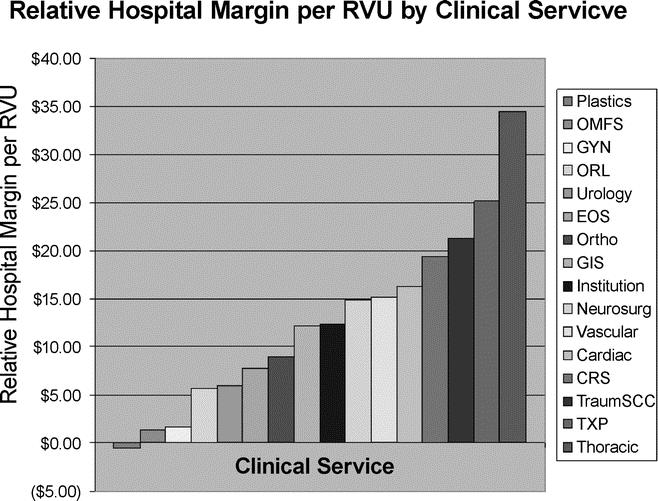
FIGURE 3. Relative hospital margin (RHM0 per RVU varies greatly by service. Mean RHM per RVU was 12.64 mu (standard deviation = 9.76 mu) with range from a loss of 0.57 mu per RVU (plastic surgery) to a gain of 34.55 mu per RVU (thoracic surgery). GIS, gastrointestinal surgery; TXP, liver, kidney, and pancreas transplant; CRS, colorectal surgery division; EOS, endocrine and oncologic surgery; ORL, otorhinolaryngology; TraumSC, trauma and surgical critical care; GYN, gynecologic surgery; Ortho, orthopedic surgery; OMFS, oral maxillofacial surgery.
Some of the variation can also be explained by the fact that not all cases generate the same number of RVUs per unit time, this being a function of both case complexity and the subjectivity in how the cases are valued by the relative value system. The mean number of RVUs per case by clinical service was 24.49 (SD = 12.88) with a range of 9.04 (urology) to 57.12 (transplant surgery). On a per-case basis, relative hospital margin per case ranged from a loss of 10.50 mu/case (plastic surgery) to a gain of 1435.18 mu/case (transplant surgery) with a mean of 361.82 mu/case (SD = 388.42). As shown in Figure 4, relative hospital margin per case was highly correlated with RVU per case, with R2 = 0.76 (P < 0.0001).
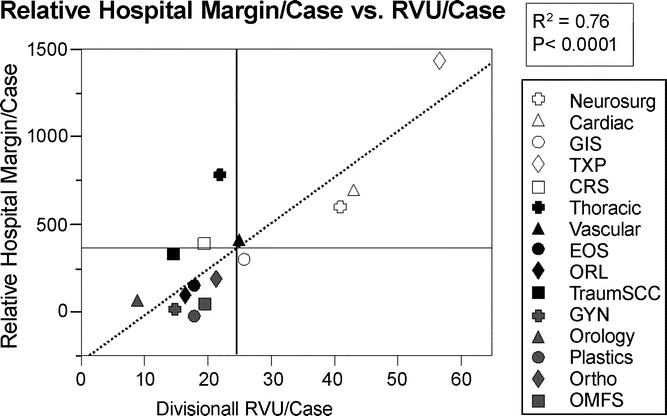
FIGURE 4. Relative hospital margin per case is strongly correlated with relative value units per case with R2 = 0.76 and P < 0.0001. The mean RVU per case by clinical service was 24.49 (standard deviation = 12.88) with a range from 9.04 (urology) to 57.12 (transplant surgery). The mean relative hospital margin per case was 361.82 mu (standard deviation = 388.42 mu) with a range from a loss of 10.50 mu/case (plastic surgery) to a gain of 1435.18 mu/case (transplant surgery). GIS, gastrointestinal surgery; TXP, liver, kidney, and pancreas transplant; CRS, colorectal surgery division; EOS, endocrine and oncologic surgery; ORL, otorhinolaryngology; TraumSC, trauma and surgical critical care; GYN, gynecologic surgery; Ortho, orthopedic surgery; OMFS, oral maxillofacial surgery.
In addition, not all cases that produce a similar margin for the hospital or generate the same number of RVUs require the same amount of time in the operating room (Fig. 5). The mean RVU/OR HR for all services was 7.10 (SD = 1.56), with a range of 5.23 RVUs per OR HR (otorhinolaryngology) to 10.97 RVUs per OR HR (transplant surgery). Mean relative hospital margin per OR HR was 94.54 mu/OR HR (SD = 81.56) with a range of (3.83) mu/OR HR (plastic surgery) to 275.74 mu/OR HR (transplant surgery). Some services do equally well on an hourly basis for both hospital margin and RVUs (transplant surgery), whereas some contribute little to either (otorhinolaryngology, urology). Of note, those services far from the regression line in the upper left and lower right quadrants contribute relatively more to the hospital margin (thoracic surgery) or generate more OR RVUs (gynecology) on a per-hour basis.
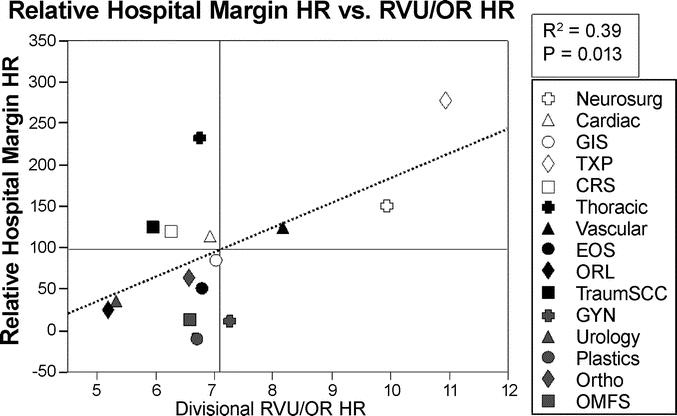
FIGURE 5. Relative hospital margin per OR HR is correlated with RVU per OR HR, but less so on a per-case basis, with R2 = 0.39 and P = 0.013. Mean RVU/OR HR was 7.10 (standard deviation = 1.56) with a range from 5.23/hr (otorhinolaryngology) to 10.97/hr (transplant surgery). Mean RHM/OR HR was 94.54 mu/hr (standard deviation = 81.56) with a range from a loss of 3.83 mu/hr (plastic surgery) to a gain of 275.74 mu/hr (transplant surgery). GIS, gastrointestinal surgery; TXP, liver, kidney, and pancreas transplant; CRS, colorectal surgery division; EOS, endocrine and oncologic surgery; ORL, otorhinolaryngology; TraumSC, trauma and surgical critical care; GYN, gynecologic surgery; Ortho, orthopedic surgery; OMFS, oral maxillofacial surgery.
DISCUSSION
We embarked on this study because it became clear to us that OR activity drives the margin of any hospital, and we felt that surgeons needed to be made aware of this, although we assumed that many surgeons already have some idea that this is the case. However, when one looks at the literature, there are few if any studies dealing with surgical contribution to hospital margin, and it soon becomes clear why this is the case. Most hospital administrators either are unwilling or unable, because of inadequate cost-accounting systems, to provide cost data, not to mention margin data. Charge data usually is easier to come by but has significantly less meaning. We are fortunate in having a hospital administration that not only is willing to provide margin data by specialty, but also by individual surgeon and physician. Many hospitals resist providing such information because of the possibility that too much information is a bad thing; the thought of having surgeons use these data as leverage in any type of negotiation scares many administrators away from providing this information. Recognizing that in the current healthcare environment the individual practitioner of surgery is an endangered species and sensing that likely we will see more full-time employment models between hospitals and surgeons, we thought it timely and important for surgeons to realize the role they play in generating the hospital bottom line. Although certain specialists may think that the lucrative nature of their practice must mean that the hospital is “making a fortune” off of them, the data often show otherwise. The busiest surgeon in the hospital may not be anywhere near the biggest generator of margin for the hospital and thus may not realize that his leverage in a negotiation, whatever the issue, may not be as great as presumed.
What differentiates the current study from others2,4 is our use of actual payments collected, not presumed collections or costs that obviate the need to look at payer mix or individual contracts and calculate likely collections. We have chosen to use what we term relative hospital margin as measured in margin units (mu) derived from neurosurgery, the specialty responsible for the largest margin for the hospital in FY04, generated by dividing by a constant that pegs the margin at 1 million margin units. Margin for all specialties are reported in margin units, and this allows for comparison among specialties without violating the confidentiality of hospital margin data and inviting third party payers to try to reduce payment for specialties that might be thought to be “too lucrative.” Others have commented on the potential negative impact if payers recognize the high margin generated by certain procedures and use this information against a hospital in subsequent negotiations.4 Thus, there is some sensitivity to reporting margin data. It must be kept in mind, however, that hospital margin is dependent on a number of variables intrinsic to each hospital and includes direct costs and efforts at controlling costs, allocation of indirect costs, controlling length of stays, efficiency and effectiveness of the revenue cycle, operating room throughput, and a number of other factors in addition to revenue generated.
It has become increasingly clear to us and others that a significant dichotomy exists between what payers, including the federal government, pay in professional fees and what they pay to the hospital.2 In our own environment, the difference is quite significant with the hospital reimbursement being significantly greater on a relative basis than professional fees, making every clinical department somewhat dependent on funds transferred from the health system to the practice for the practice to remain viable. This is possible because of the organization of our health system, in which the practice is a business unit of the health system but is within the system itself and does not exist as either a unique for profit or not-for-profit corporation. The practice entity has a joint reporting relationship both to the chief executive officer of the health system and to the dean of the school of medicine, but it sits separate from both entities. Thus, dollars flow to the practice for purchased services, program support, support for teaching, and support for a percentage of nonfunded time spent on research. These dollars increasingly are tied to productivity and vary significantly among departments. The department of surgery and the related surgical disciplines in any academic medical center, as well as in community hospitals, are responsible for the majority of any margin generated by the hospital. Depending on the overall financial performance of the hospital, which takes into account issues such as payer mix, location, costs associated with care of the uninsured, and general overhead, this margin may be severely eroded and may amount to little if any surplus at fiscal year's end.
The relationship between hospital margin and professional fees generated for RVUs performed is not straightforward. Because each clinical specialty requires a different amount of OR time, generates different numbers of RVUs per case, and performs different numbers of cases each year, it is the interaction of all of these relationships that determines how strongly a clinical service contributes to the overall hospital margin. As shown in Figure 6, the total number of cases performed in and of itself does not correlate with the overall relative hospital margin (P < 0.05), and the annual OR hours used by each service also has no significant relationship to relative hospital margin (P < 0.05) (Fig. 7). It becomes apparent that there are some services that use a lot of OR time and contribute substantially to hospital margin (neurosurgery, cardiac surgery, and gastrointestinal surgery) and a handful of services that neither take up a lot of OR time nor contribute much to overall hospital margin (oral maxillofacial surgery, trauma/surgical critical care, colorectal surgery, orthopedic surgery). However, there are services that use relatively little OR time but contribute greatly to overall hospital margin (thoracic surgery, transplant surgery) and others that occupy the OR a substantial amount of time but contribute little to hospital margin (otorhinolaryngology, urology, gynecologic surgery, urology, endocrine and oncologic surgery).

FIGURE 6. Relative hospital margin has no correlation with total number of cases performed per year by each service (P < 0.05). Neurosurg, neurosurgery department; TXP, liver, kidney, and pancreas transplant; CRS, colorectal surgery division; EOS, endocrine and oncologic surgery; ORL, otorhinolaryngology; TraumSC, trauma and surgical critical care; GYN, gynecologic surgery; Ortho, orthopedic surgery; OMFS, oral maxillofacial surgery.
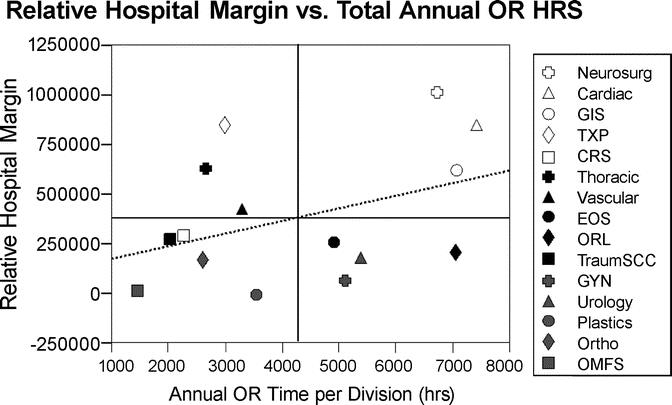
FIGURE 7. Relative hospital margin has no significant correlation with total annual OR hours used by each service (P < 0.05). Neurosurg, neurosurgery department; Cardiac, cardiac surgery division; GIS, gastrointestinal surgery division; TXP, liver, kidney, and pancreas transplant; CRS, colorectal surgery division; Thoracic, thoracic surgery division; Vascular, vascular surgery division; EOS, endocrine trauma and surgical critical care division; ORL, otorhinolaryngology; TraumSC, trauma and surgical critical care; GYN, gynecologic surgery; Urology, urology division; Plastics, plastic surgery division; Ortho, orthopedic surgery; OMFS, oral maxillofacial surgery department.
The question arises as to how generalizable these data are to other institutions and there are no easy answers. It is probably safe to say that surgeons, and OR activity, are the biggest contributors to hospital bottom line in any hospital setting, but numerous variables come into play at each institution. Obviously, the payer mix and efficient resource utilization are key to generating margin, but how contracts are negotiated also plays a major role. In many markets, surgeons are losing on the professional fee side, whereas hospitals are benefiting enormously from the RVUs generated in the OR.
Limitations of the study include the fact that outpatient procedures performed in the clinic, that do not use the operating room case log database, are not included in the operative data. However, there are very few cases that fall into this category. Another limitation is that only 1 primary procedure per case is logged into the OR case log. Therefore, cases that involve multiple CPT codes do not get credit for the RVUs corresponding to the secondary codes. However, the RVUs corresponding to the OR case log CPTs were highly correlated to the RVUs corresponding to the CPT codes for all procedures ultimately billed by the departments. Furthermore, this can also be seen as an advantage of the study, because differences in the ability of specialties to optimize coding strategies are excluded in the analysis. Also, the primary billing procedure carries most weight with many payers, so the exclusion of secondary procedures seems to be valid when looking at ultimate reimbursement.
CONCLUSIONS
These data very clearly point out that there are advantages for hospitals to provide support for selected specialties and, in certain instances, even look toward a full-time employment model. This has been done in many hospitals with, among other specialties, cardiac surgery, in which the surgeons are hired by the hospital and become full-time employees, thus insuring the cardiac surgery volume and its contribution to the margin, and allowing the surgeons to benefit from some of the margin that they generate. It is certainly true that in general, whether in an employment model, a joint venture, or by working more closely in a traditional model, increased sharing of financial data between hospitals and physicians will allow both to more rationally develop overall strategies for the kind of care provided and thus optimize the overall value chain more effectively. Surgeons should recognize the significant and, depending on the specialty, sometimes minimal leverage they bring to the table when negotiating novel practice arrangements. Certain specialties generate substantial RVUs in the OR that contribute greatly to the hospital bottom line, whereas others may use significant OR time and contribute little in the way of margin. It remains the mission of the academic medical center to provide the full range of services, and we continue to support this mission, regardless of margin. Some services that are necessary for the function of the hospital's other service lines such as transplant medicine or medical intensive care may have negative margins when viewed in isolation. It is important to view these kinds of services as necessary costs to create positive margin elsewhere in the hospital. The use of readily available data may help to maximize some services while continuing to provide other services that may not contribute as much to the margin. Surgeons and hospitals alike will do well to look closely at cost and reimbursement data and budget accordingly in a cooperative fashion so as to maximize margins.
Discussions
Dr. Hiram C. Polk, Jr. (Louisville, Kentucky): Let me ask you just to clarify. Did you not include in your evaluation something I referred to yesterday, the enormous value of lab and x-rays ordered by your doctors? Is that correct?
Dr. Larry R. Kaiser (Philadelphia, Pennsylvania): That is correct. No downstream revenues were included. This was strictly from the OR. Those are mostly used, yes.
Dr. Hiram C. Polk, Jr. (Louisville, Kentucky): They are a very large component of what we do. The second thing I want to say just from our experience across our state is that you can rapidly turn a profitable operation into an unprofitable one by some simple surgeon choices in the OR. You take a standard general surgery procedure and put a harmonic scalpel in the set and you have abolished the profitability of the case. So this is an extraordinarily complicated field and Dr. Kaiser has done us a great service by getting us into this arena. We need to be here and we need to understand surgeon choices as being very important in the costs of many of these things.
Dr. Lazar J. Greenfield (Ann Arbor, Michigan): I would like to congratulate Dr. Kaiser on his presentation and the excellent manuscript. The codependent relationship between surgeon and hospital has always been assumed to be profitable to both, but quantitation of the hospital component has been shrouded in many creative ways. Breaking through the barriers to examine the actual figures requires time and persistence, and since there are no consistent standards for hospital accounting, each institution is unique. My colleague Paul Taheri had sufficient interest in this area to acquire an MBI, and his thoughts on this are included with mine.
Since the authors are comparing margins among the surgical specialties, the first question is whether all procedural billing was captured by reviewing the OR database. Did this include all outpatient and clinic procedures done by specialties such as plastic surgery, urology, and oral surgery? Similarly, since billing and coding have become an art form with frequent changes, are metrics in place for each specialty to assure that all cases are optimally coded?
On the hospital side, the first challenge is to determine how revenue is actually allocated among such diverse services as radiology, pathology, and the ER when the single DRG payment is received. Hospitals may or may not allocate the revenue as a percent of expense submitted.
Another important issue is how you define a service. For example, Transplant has a medical side that usually loses money, but is obviously essential. Therefore that service line requires a subsidy that has a major impact on profitability. From the hospital perspective, the apparent OR margin of a specialty service may well be consumed by supplements provided to other related specialties. But hospitals also benefit from end-of-year adjusted benefits from the Blues and other payers, and were these adjustments included?
The issue of costs is always a problem. You mention you included “direct clinical provider” costs for each service. Just how did you determine the provider costs for each procedure? And given the profitability of residents under the hospital's imputed costs, how were they factored in?
The bottom line is that surgery has always been the engine that drives the hospital, and if your assumption that hospitals will select services and surgeons to support based on margin is correct, then academic health centers will have abdicated their fundamental responsibility to education and research. That temptation is the reason that hospital administrators report to a higher authority. The practical limitation in clinical practice is the hospital's capacity and its success usually depends on its ability to limit the number of unprofitable admissions. But I doubt that a University hospital will push to eliminate or reduce one surgical service in favor of another.
You have done an admirable job of analyzing real dollar income in your institution, but I don't think the answer to declining reimbursement is to become a closer employee of the hospital. Instead, I believe that joint venturing with the hospital into new clinical areas, getting paid for management services provided, and working with the institution to reduce costs will ultimately be more worthwhile, especially since gainsharing of money saved has now been approved by MEDPAC.
Thanks very much, and congratulations again on this important subject.
Dr. Larry R. Kaiser (Philadelphia, Pennsylvania): Thank you for your comments, Dr. Greenfield. And as you point out, you and Dr. Taheri certainly contributed to this area in the literature.
Your first question dealt with CPT codes and billing. And there is no question that the billing information is a little bit more difficult to get to than the CPT codes. We did look at billing information. There was a strong correlation between the billing information and the CPT codes, fairly consistent between services. It was much easier to use the CPT codes as the surrogate here and we think that that is fairly accurate.
In terms of end-of-year adjustments, those have been included in the overall data.
You also mentioned outpatient and clinic procedures. We don't have a free-standing outpatient surgical center, those cases are done in our so-called outpatient or day surgery ORs, so all of that is included. Procedures that are done in the clinic are not included; they would not be part of the operating room logs.
In terms of how provider costs are allocated, this is done consistently across the services. It is based on our cost-accounting system. And there are costs allocated for people in the operating room, et cetera, but it is consistent across the services.
You mentioned some of the medical components of some of these services. Clearly that is not what we are talking about today. This was strictly looking at margin data based on OR productivity.
Dr. Richard J. Shemin (Boston, Massachusetts): This is a very interesting study and a unique data set. Two specific questions:
In regards to variability of contractual adjustments among the various services, did cardiac surgery have more contractual adjustments compared to any other service?
The second question relates to using these data in a different way. Very often we look at the clinical volume of cardiac surgery in a hospital as a threshold for quality. Can we also look at these data to search for a threshold of profitability? Very often we see new community hospitals starting cardiac surgery programs, and these programs are highly subsidized by the hospital just to have the cardiac surgical service present.
Dr. Larry R. Kaiser (Philadelphia, Pennsylvania): I think there are a couple things. And as I mentioned, there are all sorts of assumptions and all sorts of variables built into any of these data.
But the Philadelphia market is somewhat unusual in that 80% of the people who we treat have 1 of 2 providers providing their health insurance. There is only Aetna and the independence Blue Cross entity. So 80% are covered by 1 of these 2 entities. So our contracts are fairly stringently negotiated.
We do have, for instance at the Hospital of the University of Pennsylvania, some more favorable rates than some of the other institutions in town, but there are negotiations that go on every few years. So there is no particular variability of contractual adjustments between services, with few exceptions. But we negotiate as an entire practice, the clinical practices at the University of Pennsylvania.
Dr. Carlos A. Pellegrini (Seattle, Washington): I am happy to see that you did not include downstream revenue calculated into this. And I would encourage if you are going to look into this to keep it just to the services. Because if we do that, then we open the door for those who claim that we, surgeons, are downstream – and then the support for medical specialties comes in.
My question is: Do you have an idea how in your hospital the margin that you just showed generated by surgical specialties compares to that of medical specialties, in particular oncology and others that are coming up as important factors in hospital margins?
Dr. Larry R. Kaiser (Philadelphia, Pennsylvania): Over 75% of the hospital margin is generated by the surgical services at our place, so that leaves 25% for everybody else. How that is distributed, I couldn't tell you exactly. But over 75% of the margin is generated by the surgical services.
Dr. Gregorio A. Sicard (St. Louis, Missouri): Vascular surgical procedures are being performed by different specialties or subspecialties within or across departments. Have you looked at the economics of similar procedures performed by cardiologists, vascular surgeons and radiologists? If you have done so, how does that empower you in negotiations with hospital administrators if the results of a procedure done by surgeons provide a bigger margin to the hospital?
Dr. Larry R. Kaiser (Philadelphia, Pennsylvania): That is a very good question. And it would apply to Bruce Gewertz as well, who is standing over there. I actually just had occasion the other day to look at some of those data. And as Dr. Sicard points out, interventional radiologists, cardiologists, and vascular surgeons are doing endovascular procedures. And it is very interesting to look at the margin among those various services as well as the costs.
I would tell you looking at aneurysms, peripheral vascular work and carotid work that it turns out, for instance, with peripheral vascular work, if you look at what vascular surgery generates in terms of the margin versus what the interventional radiologists generate, they lose money at our place where the vascular surgeons are making money on each case. So there is just one example. In every instance we looked at their costs were lower and the margin on the practice was significantly greater when vascular surgeons were doing these procedures than when either interventional radiologists or cardiologists were doing the procedure.
Dr. Bruce L. Gewertz (Chicago, Illinois): I want to thank you for bringing me back to reality. I hadn't thought about this for about 12 hours.
At the University of Chicago, we have looked at this data quite carefully as well. We see a slightly different pattern which is more of a skewing of profitability. That is, we have many more of our services that are close to a break-even sort of situation and few services that generate very high margins. In contrast, 4 years ago we saw all of surgical services make a 1 to 4 million dollar financial contribution very similar to the distribution seen at Penn. We found that one of the factors that fundamentally drives this is the use of prosthetic devices. Any surgical service that uses a prosthetic device is going to be challenged financially relative to a hospital margin, in contradistinction to general surgery and most cancer surgery that tends to be extirpative and highly compensated.
The second issue I would ask you to comment on is the wide variability professional fee income which is strongly payor specific as you briefly alluded to in the introduction. We, like you, have a number of physician services in which the AAMC-mandated compensation level and expenses are greater than their professional fee reimbursement. This effect is very adverse for the department.
To follow up on Dr. Greenfield's point, this data shows how critical economic credentialing is going to be to the development of academic surgery departments. This will be evident in terms of programmatic development where we are need investors to help seed our program development. It will also have very strong implications on how to incentivize activity that is not RVU accountable, whether it is educational or research activity. I think this is really a challenge for all of us.
Dr. Larry R. Kaiser (Philadelphia, Pennsylvania): Dr. Gerwertz, thank you for your comments. You raised a number of interesting points, especially as you just concluded.
Let me just say that the use of devices, of course, does figure into any margin data, and those services that don't tend to use devices will have significantly less in the way of cost. On the other hand, some of those device costs can be reduced by having some consistency in the operating room. And we have tremendous inventory management in our operating room, and consistency. For instance, in orthopedics, if every orthopedic surgeon is using a different knee implant – not even getting into some of the inspector general questions that have been raised with some of the manufacturers as to which knee implant or whatever they chose to use – if there is some consistency, one can drive down the costs of some of those by negotiating better contracts if you use lots of those devices. And that goes for cardiac valves as well.
In terms of professional fees, I didn't deal with the professional fee issues here. Professional fees, of course, differ among markets around the country. The Philadelphia market has among the lowest professional fee reimbursement in the country but much more favorable rates of reimbursement to the hospital. So this issue that you raise about funds flow between the hospital and the practice for our institution works very well because we are all one. The practice plan does not sit separate from the institution itself, so there can be funds flow between the entities. And that is a particularly important consideration. But we did not deal with professional fee revenue here.
As you mention, dealing with activities that don't generate RVUs is also particularly important. It gets into the issue of funds flow between the entity. How do you support education? How do you support medical student education? How do you support unfunded research, for that matter? Not all research can be funded for every percent of everyone's time.
Dr. Eric Munoz (Newark, New Jersey): This is just one of many, many economic aspects. I was happy to hear that one of your residents is going to the great Wharton School, because when I got an MBA years back people thought I was nuts, but 20 years later it is much more relevant.
May I remind the Association that $1.7 trillion this year is being spent on health costs. The great late Francis D. Moore published an article and showed about one-third of all that money is related to surgery. So we as surgeons and leaders in this field have to say to ourselves we can't turn our back on that. There are many aspects of this – doing research on hospital costs.
Dr. Larry R. Kaiser (Philadelphia, Pennsylvania): Dr. Munoz, thank you. And I would just mention that not only has Dr. Resnick gone to the Wharton School but he is at the top of his class at the Wharton School, and he graduates next month.
Footnotes
Reprints: Larry R. Kaiser, MD, John Rhea Barton Professor and Chairman of Surgery, 3400 Spruce Street, 4 Silverstein Pavilion, Philadelphia, PA 19104. E-mail: larry.kaiser@uphs.upenn.edu.
REFERENCES
- 1.Todd BA, Resnick AS, Stuhlemmer R, et al. Challenges of the 80-hour resident work rules: collaboration between surgeons and nonphysician practitioners. Surg Clin North Am. 2004;84:1573–1586. [DOI] [PubMed] [Google Scholar]
- 2.Huber TS, et al. Financial impact of tertiary care in an academic medical center. Ann Surg. 2000;231:860–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taheri PA, Butz DA, Dechert R, et al. How DRGs hurt academic medical centers. J Am Coll Surg. 2001;193:1–11. [DOI] [PubMed] [Google Scholar]
- 4.Taheri PA, Butz DA, Greenfield LJ. Paying a premium: how patient complexity affects costs and margin margins. Ann Surg. 1999;229:807–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.2004 National Physician Fee Schedule Relative Value File. Washington, DC: Centers for Medicare and Medicaid, Department of Health and Human Services; 2004. [Google Scholar]


