Abstract
Objective:
The objective of this study was to analyze nearly 3 decades of surgical residents from an established training program to carefully define individual outcomes on personal and professional health and practice satisfaction.
Summary Background Data:
A paucity of data exists regarding the health and related practice issues of surgeons postresidency training. Despite several studies examining surgeon burnout and alcohol dependency problems, there have been no detailed reports defining health problems in practicing surgeons or preventive health patterns in this physician population. Important practice factors, including family and practice stress, that may impact on surgical career longevity and satisfaction have similarly received minimal focused examination.
Methods:
All former surgery residents at the University of Wisconsin from 1978 to 2002 were contacted. Detailed direct interview or phone contact was made to ensure confidentiality and to obtain reliable data. Interviews concentrated on serious health and practice issues since residency completion.
Results:
One hundred ten of 114 (97%) former residents were contacted. There were 100 males and 14 females with 2 deaths (accident, suicide). Including deaths and those lost to follow up, 15 (13.2%) were nonpracticing; 5 voluntarily (3 planned, 1 accident, 1 arthritis) and 4 involuntarily (alcohol/substance dependency). Eighty-nine percent were married or remarried with a 21.4% divorce rate postresidency. Major health issues occurred in 32% of all surveyed and in 50% of those ages ≥50. Only 10% reported complete lack of weekly exercise activity with 62% exercising at least 3 times per week. Body mass index increased from 23.9 ± 1.5 kg/m2 (age <40) to 26.6 ± 3.0 kg/m2 (P = 0.009) by age ≥50. Alcohol dependency was confirmed in 7.3%. Overall, 75% of surgeons surveyed were satisfied with their practice/career.
Conclusion:
Despite a high job satisfaction rate, surgeon health may be compromised in up to 50% by age ≥50, with a 20% voluntary or involuntary retirement rate. Alcohol dependency occurred in up to 7.3% of surgeons, which contributed to the practice attrition rate. The success and length of a career in surgery is defined by postresidency factors rarely examined during training and include major and minor health issues, preventive health patterns/exercise, alcohol use or dependency, family life, and practice satisfaction. Surgeons mentoring during the course of surgical training should be improved to inform of important health and practice issues and consequences.
The outcome of surgeons in terms of quality of life and personal health issues after residency training has had limited examination. An assessment of 110 of 114 (97%) surgeons revealed an overall job satisfaction rate of 75% with personal health issues affecting 50% of respondents over age 50. The success and length of surgical careers is determined by a variety of factors examined in this cohort of surgeons.
The surgical training process that extends through completion of medical school plus an established training program and additional specialization is a highly selective, lengthy, and demanding experience that hopefully prepares individual surgeons to enter the surgical community at the highest level. As evidenced by the remarkable lack of information regarding life as a surgeon, it would appear that many in the academic community may not feel compelled or informed enough to advise residents on aspects of personal health, quality of life, divorce rates, alcohol or substance abuse, and so on. Consequentially, the longevity and satisfaction with a career in surgery is defined by these and other postresidency training factors that may include major and minor health issues, preventive health habits, and work- or family-related stress that impact on quality of life. Although academic surgical programs have focused on the development of technically competent and well-rounded surgeons, there is surprisingly little information on career attrition rates and factors that essentially define the life of a surgeon in and outside of medicine.1
Physician health issues may be key determinants in length of surgical careers along with work-related stress as examined by Campbell et al.2 Their report identified over one third of practicing surgeons who were at risk for burnout. Such practice-related stress may be a major contributing factor to individual health status, although the spectrum of medical problems in surgeons over time has not been examined. Furthermore, stress-related practice issues contributing to retirement or burnout might contribute to other impairment problems such as alcohol use and abuse, of which the prevalence for surgeons is unknown.2,3 In reports by Krizek, it was estimated that up to 8% of surgeons have alcohol dependency.3,4 However, reports on physician dependency postresidency are not specific and defined for the surgical community.5
The present study is the first report to our knowledge that examines outcomes including major, minor, and preventive health issues (including exercise trends), alcohol use and dependency, and divorce rates in a direct follow up of surgeons after completion of residency training at a single institution over the last 25 years. The secondary goal of this comprehensive analysis was to gain insight into practice patterns and satisfaction, practice changes, and trends in medical legal issues that determines the level of work-related stress and impacts on personal–professional health.
METHODS
A direct follow-up examination of practicing surgeons trained at the University of Wisconsin over the last 25 years (l978–2002) was conducted to elicit important health-, family-, and practice-related issues. Recent graduates were excluded, because many were still in or completing fellowship training. Direct telephone (n = 101) or personal (n = 7) interviews were conducted to achieve the highest level of follow up of very specific and confidential health and quality-of-life, practice, and important feedback issues. Confidentially was ensured and the project was approved by the University of Wisconsin internal review board.
All interviews focused on 4 main areas of follow-up questioning to examine demographics, health, surgical practice (including practice satisfaction and attrition rates), and major sources of stress. A more specific summary of areas of analysis follows.
Demographics
Demographic data included age, gender, marital status (including divorce and percent remarried), number of children, and practice locale.
Health Issues
Pertinent health-related issues included queries on major and minor health problems, including any major surgery. Major health problems were classified as any significant cardiac problems (coronary artery disease, arrhythmias, and so on), alcohol/substance dependency, malignancies, severe depression, major surgery requiring rehabilitation or impacting on surgical practice or early retirement, and other problems as reported. Minor health issues included hypertension, hypercholesterolemia, renal calculi, and minor surgery among other conditions as listed. Alcohol or other substance use or dependency (requiring recovery or impacting on surgical practice) was also a major focus. Alcohol use in nondependent surgeons was recorded by age and classified by use as daily, every other day, weekly, monthly, or rarely/never. Surveyed surgeons were queried to describe their individual health status as excellent, good, fair, or poor and data was examined across age groups. Body mass index (BMI) was calculated for all responders. Additionally, exercise patterns (frequency of regular exercise per week) were determined. For surgeons 50 and over, the frequency of obtaining basic preventive health care, including cardiac evaluation, screening colonoscopy, and prostate evaluation in males or gynecologic/mammography examinations in females, was addressed.
Surgical Practice
Surgical practice information included type of practice (solo, group, multispecialty, academic) and area of specialization. General surgery practices were examined for either a nonspecific general surgery focus versus practices including areas of focus or fellowship training (ie, vascular, trauma, colorectal, surgical oncology, breast, and so on). Additional areas of specialization postgeneral surgery residency training, including cardiac/thoracic and plastic surgery, were included. Practice satisfaction was addressed along with retirement or age of expected retirement. Impact of regional medical legal climates was graded by each surgeon as falling into one of 4 categories: minor issue, major, severe, or crisis level. Frequencies of claims, settlements, and pending or completed legal outcomes were surveyed. Additionally, practicing and nonpracticing surgeons were queried as to what (if anything) they would change with respect to: type of practice or area of specialization, practice locale, devotion to more family or personal health issues, or changes in financial or retirement plans.
Stress Factors
To identify major sources of stress that may impact on length of surgical practice and health, surgeon responders were asked to identify which factors impacted on practice, quality of life, or personal health. Stress was classified as major, moderate, or light for surgical practice/work and health/family. Major stress for work/surgery included excess workload, practice changes, burnout and early retirement, and major legal issues. Major stress for health/family included major medical or surgical problems, divorce, or personal and/or family alcohol dependency issues.
Data was examined across age groups as follows: <40 (early career), 40 to 49 (midcareer), and ≥50 (late career) for all health- and surgical practice-related issues.
Statistical Analysis
Statistical summaries (minimum, maximum, mean, standard deviation, and so on) were obtained for all the numerical variables. Calculations across age groups were classified as follows: less than 40, 41 to 49, and 50 and older. Crosstabulations of age group against other categorical variables were calculated. Association was tested with Fisher exact test. If a P value for Fisher exact test could not be found as a result of computational complexity, Pearson’s chi-squared test was used instead. A one-way analysis of variance between BMI and age groups was fitted. All pairwise contrasts between groups were obtained.
All computations and figures were done in R for Windows, version 2.0.1 patched (R Development Core Team, 2004).6
RESULTS
One hundred fourteen surgeons finished general surgical residency training during the time period examined. Four were lost to follow up despite an exhaustive search, including state licensing agencies. It was concluded that they were no longer practicing. Therefore, 110 (97%) of 114 practicing and nonpracticing surgeons were contacted. Two deaths have occurred from among this group of 114 surgeons, one death from suicide and an additional death from an airplane accident. For this analysis, known demographics of the 2 deceased surgeons were included. Data summary of University of Wisconsin trained residents included 100 males (including the 4 lost to follow up and excluded from statistical analysis) and 14 females. Statistical computations were made for early career <40 years (n = 29), mid career 40 to 49 years (n = 57), and late career ≥50 years (n = 24). Assessment of marital status confirmed 98 of 110 surgeons married and 12 single. Twenty-one surgeons, (21.4%) were divorced postresidency with 16 (76%) remarried at the time of interviews. Eighty-five percent were parents with a mean number of 2.6 (range, 1–7) children.
Follow up of surgeons, including questioning of major/minor health issues, is shown in Table 1. For surgeons in the ≥50-year age group, 50% reported major health issues in contrast to 6.9% and 17.5% in the <40 year and 40- to 49-year age groups, respectively (Fig. 1). There was a strong correlation (P = 0.0004) between increasing age and the likelihood of developing major health problems. Two surgeons reported significant coronary artery disease requiring stent placement and 2 with thoracic root dilation/aneurysmal disease presumed secondary to hypertension. Besides one severe depression leading to suicide, there were 2 malignancies and a surprising 7 surgeons requiring spine surgery or management of fractures with one career ending secondary to a skiing accident. Another career-ending, rapidly progressing arthritis was reported. Minor health issues (Fig. 1) occurred in 66.7% of the ≥50-year age group with 20.7% and 38.6%, respectively, in the <40-year and 40- to 49-year age group. Self-assessment of overall health status was surveyed and summarized in Figure 2. A total of 96.3% of the <40-year age group recorded excellent health with 78.7% in the 40- to 49-year age group and only 36.4% in the ≥50-year age group (P = 0.0001). Fifty percent of respondents in the ≥50-year age group reported their health as good, with 9% and 4.5% reporting fair and poor overall health, respectively.
TABLE 1. Summary of Major and Minor Health Problems in 110 Surveyed Surgeons
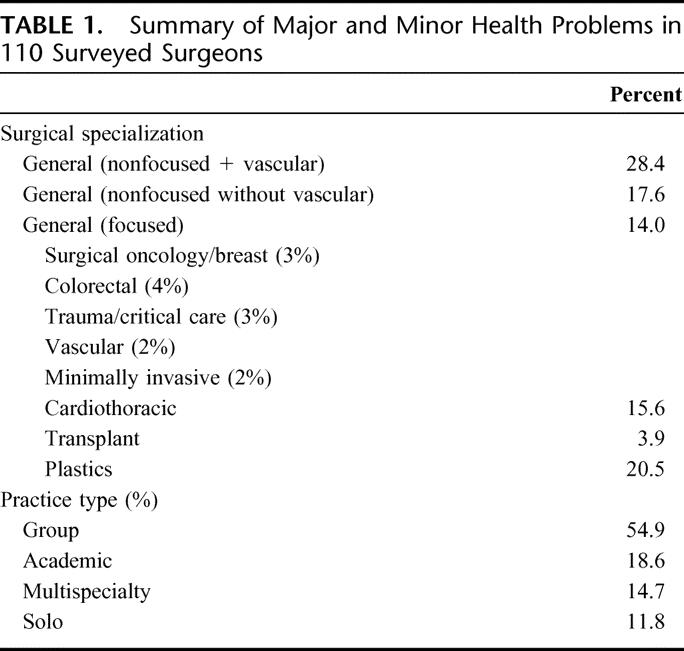
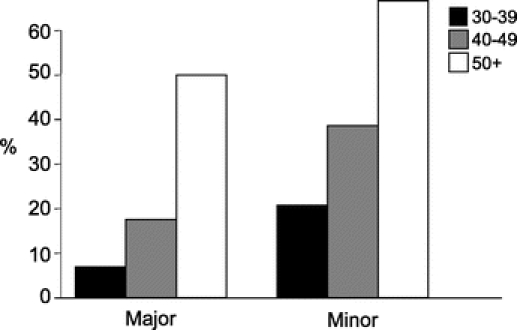
FIGURE 1. Percent of major and minor health issue by age groups 30–39, 40–49, and 50+. Association between age and major/minor health status. P < 0.003.
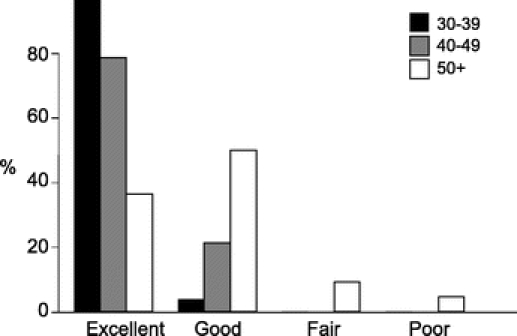
FIGURE 2. Percent of surveyed surgeons rating personal health as excellent, good, fair, and poor. Data expressed for ages 30–39, 40–49, and 50+. P = 0.001.
Basic preventive medical care questioned of the ≥50-year age group included cardiac assessment for males and a screening colonoscopy. For males, a prostate evaluation was included, and a gynecologic and mammographic examination in the single female surgeon over age 50. Not all surveyed surgeons were in compliance with basic preventive healthcare standards with 73% reporting having obtained a basic cardiac evaluation, 81% of males receiving a prostate evaluation, and 73% reported having a screening colonoscopy.
A summary of exercise patterns is shown in Figure 3, with 6% to 13% of all age groups reporting no exercise activity. There was no correlation between age and level of exercise. However, there was a statistically significant increase in BMI over time (24.3 for age <40 versus 26.6 for the ≥50 age group) (P = 0.01). The majority (62%) reported exercising at least 3 times per week and 26% reporting 5 or more times per week.
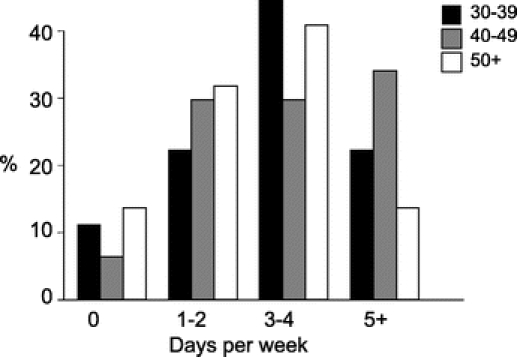
FIGURE 3. Exercise patterns and frequency are shown for age groups 30–39, 40–49, and 50+.
Alcohol and Substance Use
Of the 110 surgeons evaluated, 8 were recorded as having a significant dependency history. Six were primarily alcohol related with 2 additional having narcotic dependency. This calculated 7.3% dependency rate is in line with estimated alcohol dependency rates reported in the literature. Three surgeons have completed a successful recovery program and are currently practicing with the remainder not in practice. Smoking was rare with only 3% reporting occasional smoking habits.
A detailed assessment of routine alcohol consumption was recorded by age group and is reported in Figure 4. There was a significant rate of rarely and never alcohol use (includes surgeons completing successful recovery) in the ≥50-year age group (40%) versus that reported in the <40-year age group (P < 0.05). Seven percent to 10% of surgeons in all age groups reported daily alcohol consumption.
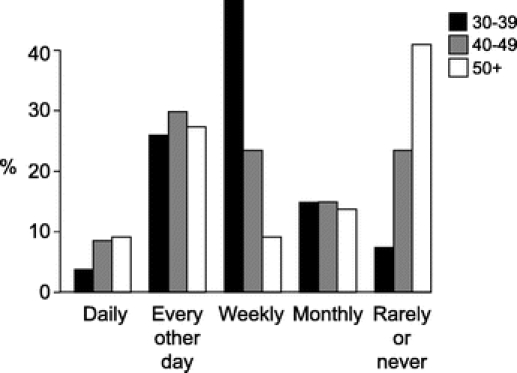
FIGURE 4. Alcohol consumption patterns by age groups 30–39, 40–49, and 50+. P = 0.0812.
Surgical Practice
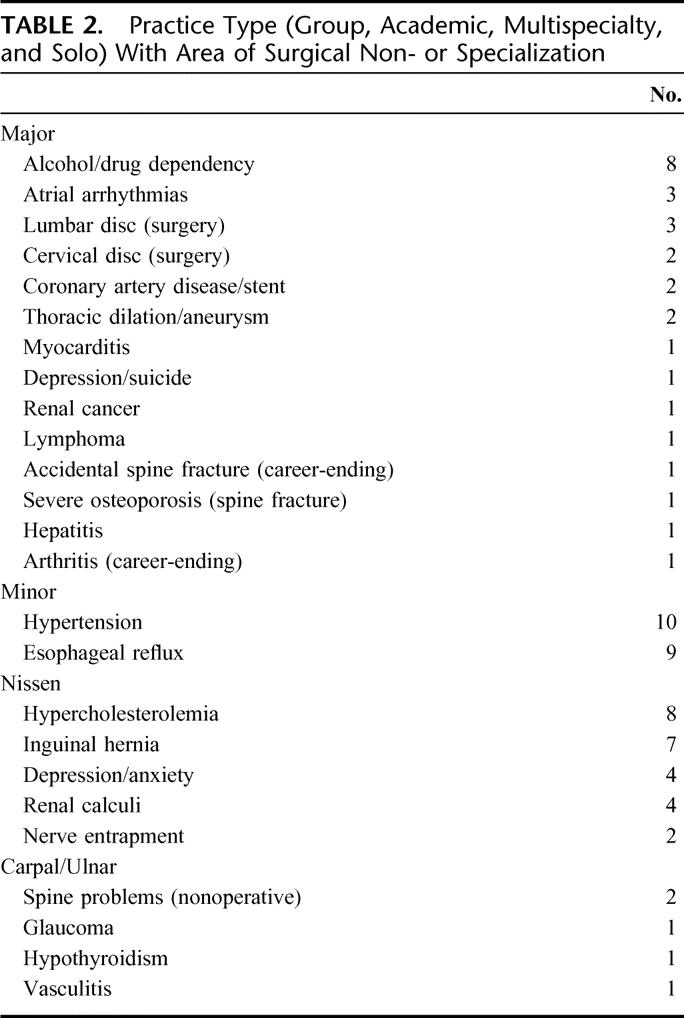
Including deaths and those lost to follow up in which there is no record of active license or practice, 15 (13.2%) were nonpracticing, 5 voluntarily (3 planned, one accident, one arthritis) and 4 involuntarily (alcohol/substance dependency). At the time of survey, all respondents in the <40-year age group were actively practicing with 14% and 20.8% in the 40- to 49-year and ≥50-year age groups, respectively, no longer in active surgical practice (P = 0.05). The type of surgical practice is shown in Table 2 with 11.8% in solo, 14.7% multispecialty, 18.6% in academic, and the majority (54.9%) in a group nonmultispecialty setting. Of the respondents, 59.8% were in some aspect of general surgery with 13.8% having an area of specialization. A total of 28.4% reported a nonfocused general surgical practice with a vascular component. The remainder fell into other subcategories as listed. Sixty percent were actively practicing in states other than Wisconsin.
TABLE 2. Practice Type (Group, Academic, Multispecialty, and Solo) With Area of Surgical Non- or Specialization
Assessment of practice satisfaction revealed no statistical difference between age groups with an overall high practice satisfaction rate. In the 3 age groups evaluated, 74% (range, 68–84%) of respondents listed their practice satisfaction as excellent (Fig. 5). Fifty percent rated their practice as good with 7% and 2% rating fair and poor, respectively. A similarly high level of satisfaction was identified when questioned whether changes would have been made in retrospect to their specialty or type of practice, practice locale, or health and family (Fig. 6). Overall, 60.1% of all respondents indicated no major retrospective changes would be considered with 41% in the ≥50-year age group reporting satisfaction with these areas of personal and professional life. The most common retrospective changes reported in 19.6% would have been to change type of practice (ie, group vs solo). Only 15% in the ≥50-year age group stated that they would have considered a different specialty. Finally, only 10.9% reported they would have devoted more time to personal health issues and family time. The majority were happy with geographic location as confirmed by only 4.3% reporting they would have preferred a different practice locale. Of the surveyed surgeons, 80% plan to retire by age 65 years, with 17% undecided.
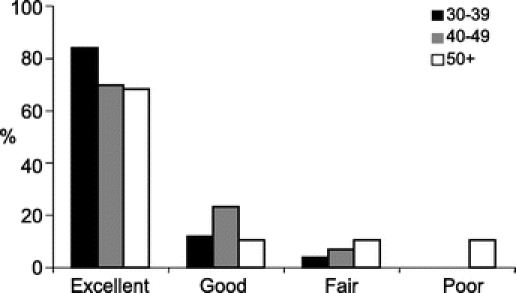
FIGURE 5. Practice satisfaction as rated for individual age groups 30–39, 40–49, and 50+.
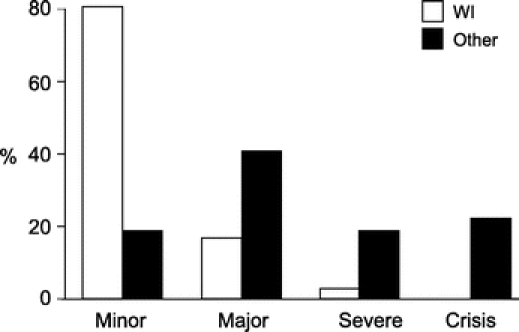
FIGURE 6. Trends in retrospective health/professional assessment when queried whether they would have changed specialty, health and family time, financial/retirement plans, or practice location.
Medical Legal Issues
Assessment of the legal climate was gauged from a minor issue to crisis level. There was a significant difference in regional medical–legal climates and effects on liability rates as demonstrated in Figure 7 comparing Wisconsin with other states where 60% of actively practicing surgeons are located. Overall, 71% of surgeons surveyed reported no legal claims have been filed against their individual practice with late career surgeons (age ≥50–60) reporting 54% with no filed legal claims. Of the 78 total claims, 42 were dropped, 19 were settled out of court, 6 were won, and 11 are pending.
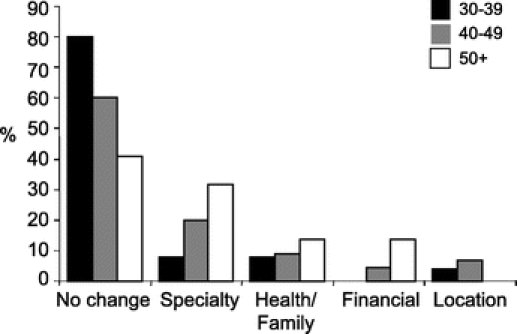
FIGURE 7. A significant difference in assessment of medical–legal climates and liability coverage is shown comparing those practicing in Wisconsin with other states. P < 0.001.
Assessment of Practice and Home/Health Stress
Determinants of relative work or home/health stress factors are complex. Scoring from light to severe, 35% reported minimal or light work-related stress. Alternatively, 14% reported severe levels of work-related stress with the major issues being changes in practice or partners. Only 14% and 7.5% reported moderate or severe home- or health-related stress, respectively, with the majority being health- or divorce-related problems.
DISCUSSION
The technical and patient management demands of the surgical training process have evolved over decades and would ideally strike a balance between professional and personal life that would result in a well-rounded surgeon who is better adapted to meet the demands and frustrations of the present era. Because there is minimal data targeted at surgeons to draw conclusions on regarding their personal and professional fate after completing their training, it follows that many of our presumed best efforts to prepare them for the real world may be shortsighted and perhaps set the stage for future health, family, and professional problems. Ideally, mentoring during residency training should include information to avoid the traps both personally and professionally for the average practicing surgeon.
For a discipline that prides itself on investigation of individual disease and treatment management outcomes, little has been reported on eventual outcomes and lifestyle consequences after choosing a career in surgery. After the initial enthusiasm of heading into a surgical practice, the midcareer warning signs that may not be recognized or heeded may lead to major health problems and result in early retirement from health or burnout issues. The goal of this survey was to obtain detailed information on a well-defined population of practicing surgeons in various phases of their careers who could provide us with a snapshot of what may be expected in the life of the average surgeon.
The information presented in this report may be reflective of many other academic training programs; however, because there is no data or similar postresidency examination, we cannot definitively conclude that our findings mirror other institutions. However, a few targeted publications have tried to examine some aspects in the inherent practice of surgery. Campbell et al, in one of the most current examinations to date of burnout among American surgeons, reported that 32% demonstrated high levels of emotional exhaustion.2 There was also a significant inverse correlation between age, years in practice, and number of children with burnout. The highest at-risk group was younger (early career) practicing surgeons. Their conclusions were that as surgical educators, we might not be preparing our surgical trainees to survive in a mental health sense in today’s modern surgical community. However, the significance of this report, which examines factors that may determine practice longevity and personal/family satisfaction, can easily get lost in the evolution of surgical training programs or maintenance of the status quo.
The implications of practice stress on health and quality of life may be significant as evidenced by our current study. To our knowledge, this examination is the only investigation of its kind addressing individual health issues, which we were fortunate to discuss confidentially with our alumni. This clearly demonstrated a significant increase in major and minor health-related problems over time with 50% of surgeons 50 and over experiencing major and a significant number also demonstrating minor health-related problems. These problems included alcohol or substance abuse/dependency. The degree of significant health issues (excluding depression) that can be related to a career choice in surgery is difficult to quantify. Our single suicide likely resulted in part from practice factors, and although the incidence of our managed depression/anxiety problems as reported is small (n = 4), we may be underestimating the true rate of affected surgeons. However, practice stress and lifestyle choices likely contributed to the majority of cardiac-related problems. It is also interesting to note the number of spine-related problems. The 2 cervical and 3 lumbar spine surgeries may be in line with the 4% to 5% annual incidence of spine problems in the general population and the repetitive nature of surgical mechanical tasks.7
Little information is known about alcohol or substance dependency rates in practicing surgeons postresidency.8 In a survey of alcohol and drug use by surgery residents, Hyde et al estimated that approximately 10% could justifiably be placed in the category of regular or possibly problem drinkers.9 To more adequately examine these issues, it was recommended that more in-depth personal interviews be conducted rather than a voluntary questionnaire. This was exactly the focus of the current study. In an excellent review on alcohol and substance dependency issues, Krizek examined the role of surgery as an impairing profession.3 Just as other members of society are not immune to dependency issues nor are professional surgeons; both Clark et al and Vaillant have estimated that 9% to 10% of physicians are impaired.10,11 However, the data on the estimated dependency rate for physicians has not been specific for surgeons. Our dependency rate of 7.3% would go along with these reported estimations, although confirmatory evidence similar to our own is lacking. This, in part, contributed to the 13% and 20% involuntary retirement/attrition rate, respectively, in the 40- to 49-year and ≥50-year age ranges. Recovery programs are essential for successful treatment of alcohol dependency as have been described in a number of reports on treatment of impaired physicians.4,12 What stands out is the higher rate of successful recovery compared with the population as a whole.12 Three of our individuals surveyed with dependency problems have undergone successful treatment programs and have continued their careers as opposed to the remainder who are no longer actively practicing.
More striking is the drinking patterns of surveyed surgeons who are still actively practicing. It is interesting to note that between 7% and 10% of practicing surgeons drink daily in a profession that probably places them at-risk for dependency issues. The range of normal behavior in the surgical community is not known. Ahmad et al tried to examine perceptions of drinking while on call and found that although three fourths of surveyed physicians disagree with drinking when subject to call, over 25% encountered physicians who were covering call while impaired.13 Interestingly, in our survey, there was a significant dropoff in alcohol-related consumption over time with over 40% of respondents in the ≥50-year age group reporting drinking rarely or never. This may be counterintuitive to general assumptions of drinking habits with progressing age. An additional 4% of families (spouses or children) in our surveyed group had alcohol dependency issues. This number is probably underestimated and will likely grow as more siblings reach at-risk ages. Therefore, it can be estimated that the combined personal surgeon alcohol dependency of 7% to 8% plus the 4% to 5% or greater in the family will probably clearly exceed 11% to 13% based on our findings.
Gross et al reported that physicians as a group largely avoid regular medical care, which also can impact on how preventive health measures are conveyed in individual patient counseling.15 It was encouraging to note that the majority of our surveyed surgeons over 50 had received some of the basic recommendations for cardiac workup, colonoscopy, and so on, although there is room for improvement. Furthermore, because exercise patterns in the spectrum of preventive health patterns in the surgical community is largely unknown, it is noteworthy that over 62% of our respondents reported exercise routines of 3 or more times per week. This would be in line with the report by Frank et al on exercise patterns in women physicians that demonstrated a higher rate of regular exercise versus the general population.16
Does a failure to adequately balance health, family, and practice stress and issues result in frustration, loss of personal/professional satisfaction, and an inevitable reflection that certain changes should have been made during the course of individual careers?17 Campbell et al noted that although stress and the signs of surgical burnout are not uncommon, there appear to be individual personality traits that confer vulnerability or resistance to stress that ultimately may influence length of surgical career.2 Furthermore, it would appear from our own survey that most including all ages and phases of career (range, 68–86%), report a high job satisfaction rate. This is despite key indices of burnout, which was likely present but not fully examined, and frustration with some aspects such as the medical–legal climate as outlined in Figure 7. Although a significant proportion of our surveyed surgeon alumni have been unaffected by liability claims, the rising liability rates and assessment scores outside the state of Wisconsin are contributing to a negative environment and enhancing practice stress. A number of nonsurgical reports have attempted to address physician wellness and practice satisfaction issues.18–20 In our survey, a surprising number (61%), when queried whether they would have changed anything about their practice, specialty selection, practice locale, personal health, family, and financial issues, responded with no major changes in hindsight. Surprisingly few surgeons (4%) reported any desire to change practice locale despite severe or crisis-level regional legal climates (Fig. 6). Similarly, even with the majority of respondents reporting moderate or severe work- and practice-related stress, the resistance and coping skills to the surgical practice environment appear to translate into fairly good professional job satisfaction. However, as evidenced by health issues, dependency problems, and indicators of practice, health, and family stress, many have struggled to balance a healthy lifestyle outside the surgical practice.
In conclusion, this report serves to examine important health- and practice-related satisfaction and issues that contribute to individual and professional health that ultimately impact on length of career. It would appear that in the cohort of surgeons surveyed, there is a significant incidence of major and minor health problems by age 50 to 60 that may be unique from the general population. Much like other members of society, we encounter an 8% incidence of alcohol/substance dependency that is even greater when the family as a whole is included. Despite individual health-, family-, or practice-related stress, the overall job satisfaction rate is high at over 70%. However, when all factors such as health, practice stress, and family issues are examined, there is a combined voluntary and involuntary attrition rate of 20% from active practice by age 50 to 60. These findings may offset the limited historical data on the outcome of life as a surgeon and should be stressed to surgical trainees to make them more fully aware of potential future hurdles. Many in the academic training community who have not provided optimal mentoring in the past may be more aware of the consequences of not balancing personal health, family, surgical practice, and life postresidency training.
Discussions
Dr. E. Christopher Ellison (Columbus, Ohio): Dr. Harms and colleagues have used a survey tool administered by interview to assess health, practice patterns and retirement of surgeons trained at the University of Wisconsin between 1978 and 2002. The response rate of 97% is remarkable and the authors are to be congratulated. As Dr. Harms has pointed out, there is a paucity of health information on physicians and in particular surgeons. Therefore the findings of this study are important and interesting and provide many thoughts for consideration.
The study was well executed and I believe the conclusions are substantiated by the data. The only potential weakness is that associated with interview questions about sensitive healthcare issues. There might be underreporting if the interviewer knows the identity of the former trainee, and I wonder if you corrected for this or analyzed this in your study.
Next I would like to address the overall health of the study population. About three-quarters of the group over the age of 50 indeed had health surveys done. However, one-quarter of them did not. And this goes along and is consistent with other studies demonstrating that physicians in general do not like to go to the doctor. Therefore what, if any, recommendations do you have to encourage us as physicians to take an interest in our health?
The other significant finding was the extensive list of maladies that the study group had, and that list grew increasingly with age. I guess the point is no matter how much we would like to believe it, we as surgeons are not immune to the aging process and human disease. Given the predicted physician and surgeon shortages in the future, maintaining the health of our physician pool perhaps through more regular health screening may be more important than ever. In addition, the public expects physician health. Therefore, do you believe that documented maintenance of health should be part of institutional credentialing?
The second area of interest is that of depression, substance abuse, and suicide. The results of your study showed 8 trainees with documented substance abuse, an additional trainee with depression and suicide, and another 7–10% who used alcohol daily. This latter group could arguably be considered at risk for alcoholism and depression. If that is the case, then collectively 18–20% of physicians in your study had some element of potential stress-related substance abuse. If indeed this is the result of the stress of surgical practice, and surgical practice clearly interfaces with stress on a daily basis, what would you recommend in terms of incorporating stress management into our residencies or our postgraduate courses?
Finally, in your assessment of stress did you collect information on the work hours of the study population and was there any correlation between the number of hours worked, substance abuse, alcoholism, and practice satisfaction?
I enjoyed the paper very much. I think the message is loud and clear.
Dr. Bruce A. Harms (Madison, Wisconsin): To get the kind of information that we were going after, you have to do this yourself. I think the reports that have been out there have stated that you basically have to do direct interviews.
And you have to have a rapport with the people that you are interviewing. I have been around Wisconsin for a long time and I know these individuals. You have to open up to them to get the information that you need, and you have to be willing to share what is going on in your life as well. I am very comfortable in talking to these individuals, especially after losing a partner, especially after having somebody in the family involved with alcohol problems. You are able to deal with that. And I think we are getting as reliable data as we can.
However, I would agree with what you said. I think there is an underestimation. And I have a couple individuals that I can’t definitely confirm that I know are at risk that were not factored in.
The overall word in substance problem is “denial.” And to sort through that is tough. There is an old adage that absence of evidence is not evidence of absence. And that is probably true.
In the comments of what is going on in terms of preventive health, I didn’t comment on that. Twenty-five percent of our individuals over 50 haven’t had a screening colonoscopy, haven’t had a cardiac exam, and the males haven’t even had a prostate examination. And the comment I have on that is this, what can we do for our colleagues? Basically it is look in the mirror. You have to look around you and be smart enough to figure out that you are not immune. If our former chairman had had a screening colonoscopy, maybe he would be here.
We have to learn by example. We have a retirement age at the University of Wisconsin of 68. Five of the 11 didn’t make it to retirement, with an overall mortality rate for retirement for the last 25 years of 45%. Our morbidity in the people that did retire was 40%, having coronary stents or bypasses within a year. So the message is out there.
In terms of credentialing, I don’t think that is going to happen. There is a correlation between physician health and what we tell our patients. And I will leave it at that.
About half of the individuals affected with alcohol and substance abuse are estimated to have some kind of mental problem, usually depression. So it doesn’t correlate 1 for 1, it is estimated at about a half.
Should we include stress management issues in residency programs? I am not a residency program director. There is enough on the table already. But it is clearly something we have to think about. When I surveyed our residents, the majority of these problems started in residency and they took off. The message I got was there was nobody they could talk to. They knew they were in trouble and they just continued to escalate after residency. There is no correlation that I know of of work hours and stress or alcohol correlation. That doesn’t seem to be a factor. It doesn’t seem to be a factor with practice satisfaction. Fifteen percent of our individuals out there would describe their practice as under severe or crisis level stress.
It is a good point on the practice type that you made. A majority of our people that have dissatisfaction are in solo practices, rural communities, individuals feel isolated, although their medical-legal climate offsets for that, they are doing well in that category.
Prof. J. Hans Jeekel (Rotterdam, Netherlands): We don’t have in Europe, I think, to my knowledge, data on this subject. I have a few questions. In the first place, the size of the group is not very large. When you conclude divide residents in 3 age groups you draw conclusions on the basis of small groups. How does it compare to other professions? What is another comparable profession, like other professional organizations, maybe lawyers? How does it compare to that?
I was surprised to see that the retirement plan looks different from what I see here in the audience. I see here many surgeons working beyond the age of 65. Is that perhaps different between the university academic surgeons and the nonacademic surgeons? At the age of 60-plus in Europe, a very small percentage of surgeons still work.
Another question is: How is the part-time activity? Is it different between the age groups? In Holland we see a lot of part-timers coming, especially among women. And what about working hours in the different age groups? For example, in Holland again, you see nonacademic surgeons in a large number of hospitals organize 1 day off a week to take care of family.
Dr. Bruce A. Harms (Madison, Wisconsin): I don’t have any information on other professions. What we have got in terms of the numbers is actually quite large considering the length of time. I don’t necessarily think we can extrapolate it to other professions. The information on lawyers is not out there. We don’t know what their alcohol rate is. But in most professions it is in the 8–10% range. And that is probably underestimated.
In terms of the type of work environment, what we see here at this meeting and what is going on over there, there is a real disconnect between the private world. They have more hobbies and their overall condition is better, they have more outside activities than the academic arena that I see. That is my bias. I think there is a different European lifestyle. I lived over in Europe for a year and so I am a little bit familiar with that. They go at a different pace; and that is not necessarily true here.
It depends upon what your goals are. My goal is to get to retirement with my health. And if I look at the data from my own institution, that doesn’t happen over half the time. So that is 1 of the concerns I have. I don’t know, it is a different social philosophy of how you want to practice and live your life.
Dr. Darrell A. Campbell, Jr. (Ann Arbor, Michigan): Dr. Harms, that was a wonderful paper. Thanks for letting me look at it ahead of time. I think you have opened up a new phase in outcomes research, only now the outcomes are us as opposed to our patients. And I think that is very appropriate.
I have a question that comes to me almost every week, and I am sure the members of the American Surgical have the same question posed to them. And that is, a third-year student comes into the office and says, “Dr. Campbell, I’m very interested in surgery, I like it more than I thought I was going to like it. But I’m concerned about the lifestyle and how demanding and stressful it is. What are your thoughts about this?”
I think you have given us some information on how to answer that question in a very simple and direct way, and that is simply to look at a cohort of surgeons to find out what happened to them. So I applaud you for that.
But it is always a question of comparability. My question to you is: based on your data, how would you answer that third-year student’s question? Is it more traumatic to be a surgeon than other types of lifestyles or is it not?
As a corollary to that, as you talked with all these individual – nobody is going to argue that surgery is not a stressful lifestyle, but they must give off some kind of coping mechanism – did you get a sense for how folks coped with the high stress that they find themselves with? You did mention exercise.
Finally, based on your data, are there any suggestions you could give to Dr. Rikkers about how he might want to change his residency training program, or is it fine the way it is?
Dr. Bruce A. Harms (Madison, Wisconsin): What I tell the students is, you know, we are in a profession where you look back over time, and 70% of our people at the latter portion of their career still love what they do. And that is a good marker. In spite of it all, that is the message that comes through. And that is higher than a lot of other specialties. Our divorce rate is no worse than anybody else, in fact, lower than psychiatrists. So I think in that category we are doing well.
What is our coping mechanism? Your work is much more refined in that area. You alluded to the fact that there is something inherent about the coping mechanism of surgeons, and I believe that. And that is something that you have to study in future outcomes.
In terms of what Dr. Rikkers can do, it would be nice if we had a health club attached to the hospital so we can go work out on a regular basis.
Dr. Richard J. Shemin (Boston, Massachusetts): These data are very interesting. My comments are from the perspective having had the opportunity to chair the Society of Thoracic Surgeons Workforce Study since 1999. There were 4 studies before that year.
I am particularly interested in the prediction of retirement age. When we have looked at this in the past we have been disappointed by the failure of survey data to accurately predict retirement. In thoracic surgery, we are experiencing deferred retirement possibly for economic reasons. In addition, there is a lot of early retirement and midcareer professional changes with people pursuing other degrees. In an attempt to attract more women into our workforce, there are changes in our practice to make the specialists more attractive. Do you have any similar data on retirement, and can you make any comments?
Dr. Bruce A. Harms (Madison, Wisconsin): No, I don’t have any data on it. I think we will have to look back over time. The individuals have told me their estimated plan of retirement, what are they going to actually do when it comes down to retiring will be something for somebody else to do a follow-up study down the line. I think right now we are losing 20% over 50 for the reasons I have outlined. Most people are trying to get out early while they still have their health. Some individuals, there are only about 6% have been caught financially and then have extended their careers. It is dependent upon how their retirement system is structured that allows them to transition. About 30% plan to transition into some kind of a lower workload schedule.
Dr. Thomas R. Russell (Chicago, Illinois): The point I take away from the presentation is the job satisfaction and how many surgeons are actually quite satisfied with their work. At the end of some days, I feel there is no surgeon in this country that is happy when I receive these phone calls. This paper makes me feel really good that there is this degree of job satisfaction.
The other issue you touched on is the impaired physician in your talk. I think as a profession we tolerated the impaired physician in the past. In the future, with this transparency we heard about yesterday, it is not going to be tolerated with more stringent needs of maintenance of certification and maintenance of licensure. So at the College I would simply say that we have a very active committee, the Central Judiciary Committee, where we actually reprimand and expel dozens of surgeons (unfortunately) every year because of transgressions of professionalism.
I think there is some good information in this paper that we need to take into the residency training curriculum in order to instill habits as residents which they can then carry into practice.
Dr. Anthony A. Meyer (Chapel Hill, North Carolina): We have recently published a survey of 4 different training programs looking at residents before and after the 80 hours. And although indeed after the 80 hours they describe less amount of time and a decreased feeling of being tired, the stress that they feel is actually greater. Which gets to the point that Dr. Polk made that the 80-hour workweek is not a panacea to make all these things get better.
Dr. Bruce A. Harms (Madison): The individuals I surveyed, including, surprisingly, the women, are really scratching their heads about this, as their new partners to be come through the system, how they are going to adapt from an 80-hour workweek to the reality of the real world. And there is a perception out there and there is a concern out there about what is really going to happen down the line.
Footnotes
Reprints: Bruce A. Harms, MD, FACS, Professor of Surgery, Department of Surgery, 600 Highland Avenue, Madison, WI 53792. E-mail: harms@surgery.wisc.edu.
REFERENCES
- 1.Debas HT, et al. American Surgical Association Blue Ribbon Committee Report on Surgical Education: 2004. Ann Surgery. 2005;241:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campbell DA, et al. Burnout among American surgeons. Surgery. 2001;130:696–705. [DOI] [PubMed] [Google Scholar]
- 3.Krizek TJ. Ethics and philosophy lecture: surgery … is it an impairing profession. J Am Coll Surg. 2002;194:352–366. [DOI] [PubMed] [Google Scholar]
- 4.Krizek TJ, et al. The impaired surgical resident. Surg Clin North Am. 2004;84:1587–1604. [DOI] [PubMed] [Google Scholar]
- 5.Talbott GD, Gallegos KV, Angres DH. Impairment and recovery in physicians and other health professionals. In: Graham AW, Schultz TK, eds. Principles of Addiction Medicine, 2nd ed. Chevy Chase, MD: American Society of Addiction Medicine, Inc; 1998:1263–1277. [Google Scholar]
- 6.R Development Core Team (2004). A language and environment for statistical computing. Foundation for Statistical Computing, Vienna, Austria. Available at: http://www.R-project.org.
- 7.Bigos SJ, Mueller G. Spinal disorders and the workplace. The Adult and Pediatric Spine, 3rd ed. 2004;1:27–33. [Google Scholar]
- 8.Flaherty JA, Richman JA. Substance use and addiction among medical students, residents, and physicians. Psychiatr Clin North Am. 1993;16:189–197. [PubMed] [Google Scholar]
- 9.Hyde GL, Wolf J. Alcohol and drug use by surgery residents. J Am Coll Surg. 1995;181:1–5. [PubMed] [Google Scholar]
- 10.Clarke DC, et al. Alcohol use patterns through medical school: a longitudinal study. JAMA. 1987;257:2921–2926. [PubMed] [Google Scholar]
- 11.Vaillant GE. The Natural History of Alcoholism: Revisited. Cambridge: Harvard University Press; 1995. [Google Scholar]
- 12.Galanter M, et al. Combined Alcoholics Anonymous and professional care for addicted physicians. Am J Psychiatry. 1990;147:64–68. [DOI] [PubMed] [Google Scholar]
- 13.Ahmad T, et al. Doctors’ perceptions of drinking alcohol while on call: questionnaire survey. BMJ. 2002;325:579–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gross CP, et al. Physician, heal thyself? Regular source of care and use of preventive health service among physicians. Arch Intern Med. 2000;160:3209–3214. [DOI] [PubMed] [Google Scholar]
- 15.Feller D, Hatch R. Do physicians take care of their health? Psychiatr Ann. 2004;34:763–768. [Google Scholar]
- 16.Frank E. Exercise Counseling and personal exercise habits of UW women physicians. J Am Med Womens Assoc. 2003;58:178–187. [PubMed] [Google Scholar]
- 17.Ferris L, Walters B, MacKinnon S, et al. The quality of life of practicing Canadian women surgeons: results of the population study. J Womens Health. 1995;4:87–96. [Google Scholar]
- 18.Rollman BL, et al. Medical specialty and the incidence of divorce. N Engl J Med. 1997;336:800–803. [DOI] [PubMed] [Google Scholar]
- 19.Firth-Cozens J. Doctors, their wellbeing, and their stress. BMJ. 2003;326:670–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Landon BE, Reschovsky J, Blumenthal D. Changes in career satisfaction among primary care and specialist physicians, 1997–2001. JAMA. 2003;289:442–449. [DOI] [PubMed] [Google Scholar]


