Things are seldom what they seem,
Skim milk masquerades as cream.
W.S. Gilbert, H.M.S. Pinafore
What would your diagnosis be in someone who had a focal sensory or motor impairment that came on abruptly, reached maximal intensity within 1 to 5 minutes, resolved in 24 hours or less, and left no residua? If your answer is TIA—transient ischemic attack—it could be wrong in up to 30% of such cases. 1 And if the diagnosis is wrong, the patient's management could be wrong, and the outcome could be costly—physically, emotionally, and financially.
Think of it this way. The diagnosis of TIA is difficult at best and is frequently made from the patient's history, rather than from clinical observation. 2 Patients, however, vary widely in their ability to communicate effectively. Physicians, in turn, vary not only in their ability to elicit and interpret the patient's history, but also in their semantic and operational concepts of TIA. 3 Not surprisingly, therefore, interobserver differences in the diagnosis of TIA are common, even among neurologists. 1,3,4 To complicate matters, tests to confirm TIA do not exist. 1,4 The reason should be obvious: these episodes are so brief and unpredictable that demonstrating focal cerebral hypoperfusion during an actual attack is virtually impossible. 5
Clearly, then, the diagnosis of TIA is always presumptive. Failure to appreciate this fact stifles consideration of causative mechanisms other than ischemia and may explain why so many articles on TIA pay little or no attention to differential diagnosis.
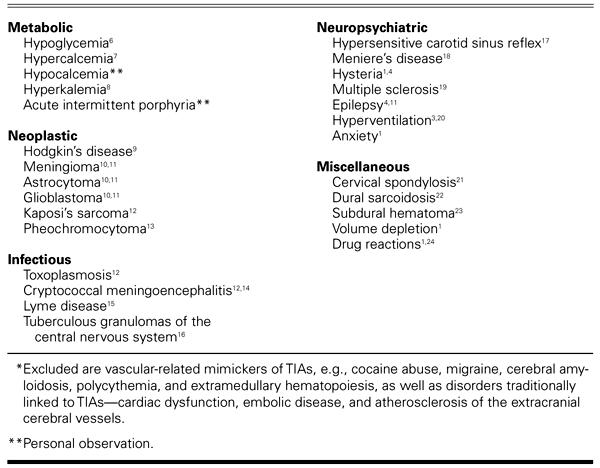
Over the years, I have learned that numerous nonvascular disorders can mimic TIAs. The more I search for these disorders—at the bedside and in the medical literature—the more of them I find (Table I 6–24). And the more of them I find, the more misleading I consider the term TIA to be.
TABLE I. Nonvascular Disorders Mimicking Transient Ischemic Attacks*
I believe that patients would be better off if we stopped using abbreviations and acronyms altogether and started spending time honing our diagnostic and communication skills. Meanwhile, if we insist on acronyms in the setting discussed here, I suggest TNA—transient neurologic abnormality. Others have used TNA to mean transient neurologic attack. 2 Either way, TNA, in contrast to TIA, defines the problem better, carries no misguiding implications, thwarts premature and presumptive conclusions, and prompts a more thoughtful diagnostic approach.
There should be no doubt that TIA is a TIA—treacherously inaccurate acronym.
Footnotes
Address for reprints: Herbert L. Fred, MD, 8181 Fannin, #316, Houston, TX 77054
References
- 1.Calanchini PR, Swanson PD, Gotshall RA, Haerer AF, Poskanzer DC, Price TR, et al. Cooperative study of hospital frequency and character of transient ischemic attacks. IV. The reliability of diagnosis. JAMA 1977;238:2029–33. [PubMed]
- 2.Bots ML, van der Wilk EC, Koudstaal PJ, Hofman A, Grobbee DE. Transient neurological attacks in the general population. Prevalence, risk factors, and clinical relevance. Stroke 1997;28:768–73. [DOI] [PubMed]
- 3.Ferro JM, Falcao I, Rodrigues G, Canhao P, Melo TP, Oliveira V, et al. Diagnosis of transient ischemic attack by the nonneurologist. A validation study. Stroke 1996;27:2225–9. [DOI] [PubMed]
- 4.Landi G. Clinical diagnosis of transient ischaemic attacks. Lancet 1992;339:402–5. [DOI] [PubMed]
- 5.Dennis MS, Bamford JM, Sandercock PA, Warlow CP. Lone bilateral blindness: a transient ischaemic attack. Lancet 1989;1:185–8. [DOI] [PubMed]
- 6.Montgomery BM, Pinner CA. Transient hypoglycemic hemiplegia. Arch Intern Med 1964;114:680–4. [DOI] [PubMed]
- 7.Longo DL, Witherspoon JM. Focal neurologic symptoms in hypercalcemia. Neurology 1980;30:200–1. [DOI] [PubMed]
- 8.Lee KS, Powell BL, Adams PL. Focal neurologic signs associated with hyperkalemia. South Med J 1984;77:792–3. [DOI] [PubMed]
- 9.Feldmann E, Posner JB. Episodic neurologic dysfunction in patients with Hodgkin's disease. Arch Neurol 1986;43:1227–33. [DOI] [PubMed]
- 10.Ross RT. Transient tumor attacks. Arch Neurol 1983;40:633–6. [DOI] [PubMed]
- 11.Fisher CM. Transient paralytic attacks of obscure nature: the question of non-convulsive seizure paralysis. Can J Neurol Sci 1978;5:267–73. [DOI] [PubMed]
- 12.Engstrom JW, Lowenstein DH, Bredesen DE. Cerebral infarctions and transient neurologic deficits associated with acquired immunodeficiency syndrome. Am J Med 1989;86:528–32. [DOI] [PubMed]
- 13.Thomas JE, Rooke ED, Kvale WF. The neurologist's experience with pheochromocytoma. A review of 100 cases. JAMA 1966;197:754–8. [PubMed]
- 14.Nowack WJ, Bradsher RW. Cryptococcal meningoencephalitis presenting transient focal cerebral symptoms. South Med J 1989;82:395–6. [DOI] [PubMed]
- 15.Veenendaal-Hilbers JA, Perquin WV, Hoogland PH, Doornbos L. Basal meningovasculitis and occlusion of the basilar artery in two cases of Borrelia burgdorferi infection. Neurology 1988;38:1317–9. [DOI] [PubMed]
- 16.Chari CR, Rao NS. Transient neurologic deficit as a presentation of tuberculosis of the central nervous system. Neurology 1987;37:1884–5. [DOI] [PubMed]
- 17.Uesu CT, Eisenman JI, Stemmer EA. The problem of dizziness and syncope in old age: transient ischemic attacks versus hypersensitive carotid sinus reflex. J Am Geriatr Soc 1976;24:126–35. [DOI] [PubMed]
- 18.Brust JC. Transient ischemic attacks: natural history and anticoagulation. Neurology 1977;27:701–7. [DOI] [PubMed]
- 19.Osterman PO, Westerberg CE. Paroxysmal attacks in multiple sclerosis. Brain 1975;98:189–202. [DOI] [PubMed]
- 20.Blau JN, Wiles CM, Solomon FS. Unilateral somatic symptoms due to hyperventilation. Br Med J (Clin Res Ed) 1983;286:1108. [DOI] [PMC free article] [PubMed]
- 21.Sheehan S. Syndromes of basilar and carotid artery insufficiency: diagnosis and medical therapy. South Med J 1961;54:465–70.
- 22.Sethi KD, el Gammal T, Patel BR, Swift TR. Dural sarcoidosis presenting with transient neurologic symptoms. Arch Neurol 1986;43:595–7. [DOI] [PubMed]
- 23.Russell NA, Goumnerova L, Atack EA, Atack DM, Benoit BG. Chronic subdural hematoma mimicking transient ischemic attacks. J Trauma 1985;25:1113–4. [PubMed]
- 24.Purvin VA, Dunn DW. Nitrate-induced transient ischemic attacks. South Med J 1981;74:1130–1. [DOI] [PubMed]


