Abstract
The eustachian valve is an embryologic remnant of the valve of the inferior vena cava. It may be prominent in some individuals, but the echocardiographic appearance of a divided right atrium, as the consequence of a large eustachian valve, is extremely rare. Herein we describe an unusual giant eustachian valve with an echocardiographic appearance of a septal structure dividing the right atrium into 2 separate chambers. This abnormality should be differentiated from cor triatriatum dexter, a very rare cardiac malformation for which it could be mistaken. (Tex Heart Inst J 2002;29:336–8)
Key words: Cor triatriatum, echocardiography, heart atrium
During fetal life, the eustachian valve directs oxygen-rich blood from the inferior vena cava (IVC) toward the foramen ovale and away from the tricuspid valve. After the closure of the foramen ovale, it does not have a specific function. In echocardiographic examinations, the eustachian valve may appear as a thin flap originating from the orifice of the IVC, or it may be totally absent. Sometimes it may appear as a rigid, elongated structure in the inferior portion of the right atrium or as a membranous, undulating, echogenic mass within the right atrial cavity. Here we describe a giant eustachian valve that extended from the orifice of the IVC to the interatrial septum, which appeared as a septal structure dividing the right atrium into 2 chambers. To the best of our knowledge, this type of eustachian valve has never before been reported. Such a giant eustachian valve should be differentiated from cor triatriatum dexter, since the latter requires surgical correction.
Case Report
In January 2000, a 51-year-old woman was admitted to our hospital because of dyspnea on exertion, fatigue, and swelling in the legs. Her medical history revealed acute rheumatic fever during childhood, mitral balloon valvuloplasty at age 18, and a closed mitral commissurotomy 11 years after the balloon valvuloplasty.
On physical examination, she had bilateral edema in the lower limbs, and the liver was palpable up to 4 to 5 cm below the right substernal border. A rumbling diastolic murmur and a pansystolic murmur could be heard at the apex and at the 4th left intercostal space, respectively. A loud, ejection-type systolic murmur was heard at the 2nd left intercostal space.
A transthoracic echocardiogram demonstrated mitral stenosis, mild mitral regurgitation, moderate aortic regurgitation, aortic stenosis, severe tricuspid regurgitation, and tricuspid stenosis. The inferior vena cava and hepatic veins were dilated. A rigid, membranous structure was observed within the right atrial cavity (Fig. 1). This structure originated from the atrial wall just above the orifice of the IVC and extended into the middle of the interatrial septum, giving an echocardiographic appearance of a divided right atrium.
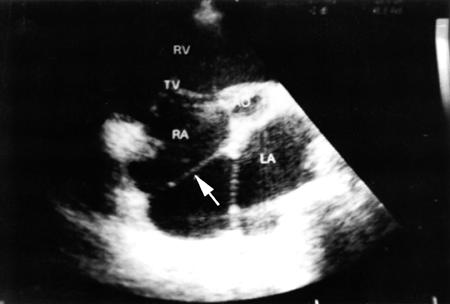
Fig. 1 Transthoracic echocardiogram appears to show a rigid membranous structure (arrow) dividing the right atrium.
AO = aorta; LA = left atrium; RA = right atrium; RV = right ventricle; TV = tricuspid valve
A coronary angiogram revealed normal coronary arteries. Cardiac catheterization indicated a mean pressure of 14 mmHg within the right atrial cavity, with no pressure rise within different portions. The patient was referred for mitral, aortic, and tricuspid valve surgery.
Surgical Technique
After median sternotomy, the patient was cannulated by means of the standard technique, and extracorporeal circulation was initiated. The mitral and aortic valves were replaced with mechanical prostheses. After a right atriotomy, a giant eustachian valve was observed within the right atrial cavity. The medial extension of the eustachian valve encroached on the atrial septum as far as the limbus of the fossa ovalis. The upper endocardial surface of the eustachian valve was covered with a thin layer of partially organized thrombus that had not been apparent in the echocardiographic examination. There were no interatrial septal defects. The eustachian valve was excised, and a tricuspid commissurotomy was performed, together with De Vega annuloplasty. The patient was discharged with no postoperative problems.
Discussion
There is a large variability in size, shape, thickness, and texture of the persistent eustachian valve, and in the extent to which it encroaches on neighboring structures such as the atrial septum. At one end of the spectrum, the embryonic eustachian valve disappears completely or is represented only by a thin ridge. Most commonly, it is a crescentic fold of endocardium arising from the anterior rim of the IVC orifice. The lateral horn of the crescent tends to meet the lower end of the crista terminalis, while the medial horn joins the thebesian valve, a semicircular valvular fold at the orifice of the coronary sinus. At the other extreme, it persists as a mobile, elongated structure projecting several centimeters into the right atrial cavity. In this case, it may demonstrate an undulating motion in real time echocardiography; and when it is quite large, it may be confused with right atrial tumors, thrombi, or vegetations. 1 Occasionally, the eustachian valve crosses the floor of the right atrium from the orifice of the IVC and inserts into the lower portion of the interatrial septum adjacent to the atrioventricular valves. 2 However, higher insertion of a giant eustachian valve, which (as in the case of our patient) mimics the echocardiographic appearance of divided right atrium, is very rare. This type of abnormality may be confused with cor triatriatum dexter. 2 Very rarely, such a configuration of a large eustachian valve may mimic a right atrial cystic tumor. 3
Cor triatriatum dexter results from persistence of the entire right sinus venosus valve, which forms a large, obstructive flap or septum across the right atrium and divides it into 2 separate chambers. The upstream chamber receives superior and inferior vena caval flow, while the downstream chamber incorporates the right atrial appendage. In this situation, venous flow is directed to the upstream chamber and subsequently across an atrial septal defect to the left atrium, resulting in a right-to-left shunt. Because the membrane is usually perforated, there is also some flow across the membrane into the downstream chamber and through the tricuspid valve into the right ventricle. Echocardiographically, the membrane generally runs from the inferior vena cava to the superior vena cava, separating the right atrial appendage and tricuspid valve from the great veins. This cardiac malformation can be differentiated from the gianteustachian valve dividing the right atrium, by echocardiographic demonstration of the atrial septal defect and by the presence of cyanosis. 4
Patients with persistent eustachian valves and without other significant structural heart disease usually require no treatment. It has been shown that symptomatic infants with persistent eustachian valve improve with conservative management alone. 5
However, large eustachian valves have been reported to increase right-to-left shunting in patients with atrial septal defects by directing inferior vena caval flow through the defect into the left atrium. This abnormality may cause cyanosis during early infancy and should be corrected surgically. 6–8 These cases may be also be confused with cor triatriatum dexter, both clinically and echocardiographically.
Occasionally, a eustachian valve is large enough to produce obstruction to flow entering from the IVC. The IVC may be dilated, which suggests that the eustachian valve may be impeding blood flow from the IVC to the right atrium. More commonly, the patient is asymptomatic and no further intervention is required. 9 In our patient, hepatic congestion and peripheral edema were most probably due to tricuspid stenosis and regurgitation, rather than to the obstructing eustachian valve, because pressures at different sites within the right atrial cavity were not elevated.
Endocarditis and thrombus formation over the eustachian valve are extremely rare complications. 10–13 In addition, very distinct cases of right atrial myxoma or papillary fibroelastoma originating from the eustachian valve have been reported. 14,15 Endocarditis of the eustachian valve, usually seen in intravenous drug users, can be treated with antibiotic therapy or surgery, depending on the clinical course of the case. 10–12 Right atrial thrombus may be attached to the eustachian valve and may result in pulmonary thromboembolism. 13 These cases may be successfully treated with thrombolytic therapy. In this particular case of giant eustachian valve, we decided intraoperatively to excise the valve because of the relatively high risk of thrombosis and endocarditis. The patient was in atrial fibrillation and had a very dilated right atrium, so risk of further enlargement of the thrombus over the eustachian valve and subsequent pulmonary embolism was considered to be high. The risk of infective endocarditis was also regarded to be high, because of the coexisting tricuspid valve disease.
Footnotes
Address for reprints: Turhan Yavuz, MD, Süleyman Demirel Univesitesi Tip Fakultesi, Kalp ve Damar Cerrahisi Klinigi, Isparta, Turkey
References
- 1.D'Cruz IA. Echocardiographic anatomy: understanding normal and abnormal echocardiograms. 1st ed. Stamford (CT): Appleton & Lange; 1996. p. 114–5.
- 2.Otto CM, editor. The practice of clinical echocardiography. 1st ed. Philadelphia: WB Saunders; 1997. p. 668.
- 3.Malaterre HR, Kallee K, Perier Y. Eustachian valve mimicking a right atrial cystic tumor. Int J Card Imaging 2000;16(4):305–7. [DOI] [PubMed]
- 4.Weyman AE. Principles and practice of echocardiography. 2nd ed. Philadelphia: Lea & Febiger; 1994. p. 849–50.
- 5.Sehra R, Ensing G, Hurwitz R. Persistent eustachian valves in infants: course and management in symptomatic patients. Pediatr Cardiol 1998;19:221–4. [DOI] [PubMed]
- 6.Morishita Y, Yamashita M, Yamada K, Arikawa K, Taira A. Cyanosis in atrial septal defect due to persistent eustachian valve. Ann Thorac Surg 1985;40:614–6. [DOI] [PubMed]
- 7.Corno AF, Bron C, von Segesser LK. Divided right atrium. Diagnosis by echocardiography, and considerations on the functional role of the Eustachian valve. Cardiol Young 1999;9(4):427–9. [DOI] [PubMed]
- 8.Condoluci C, di Donato RM, Marcelletti C, Guccione P. Central cyanosis in a newborn infant due to a prominence of the eustachian valve [in Italian]. G Ital Cardiol 1994;24:151–4. [PubMed]
- 9.Leon M, Pechacek LW, Solana LG, Massumkhani A, Cooley DA. Identification of a prominent eustachian valve by means of contrast two-dimensional echocardiography. Tex Heart Inst J 1983;10:219–21. [PMC free article] [PubMed]
- 10.Bowers J, Krimsky W, Gradon JD. The pitfalls of transthoracic echocardiography. A case of eustachian valve endocarditis. Tex Heart Inst J 2001;28:57–9. [PMC free article] [PubMed]
- 11.Palakodeti V, Keen WD Jr, Rickman LS, Blanchard DG. Eustachian valve endocarditis: detection with multiplane transesophageal echocardiography. Clin Cardiol 1997;20(6):579–80. [DOI] [PMC free article] [PubMed]
- 12.Punzo F, Guarini P, De Michele M, Accadia M, Irace L, Caruso A, et al. Eustachian valve endocarditis in an elderly woman. Echocardiography 1999;16(3):259–61. [DOI] [PubMed]
- 13.Jolly N, Kaul UA, Khalilullah M. Right atrial thrombus over eustachian valve—successful lysis with streptokinase. Int J Cardiol 1991;30(3):354–6. [DOI] [PubMed]
- 14.Teoh KH, Mulji A, Tomlinson CW, Lobo FV. Right atrial myxoma originating from the eustachian valve. Can J Cardiol 1993;9:441–3. [PubMed]
- 15.Shigemitsu O, Hadama T, Mori Y, Miyamoto S, Sako H, Uchida Y. Surgical treatment of right atrial papillary fibroelastoma, originated from the eustachian valve—a case report [in Japanese]. Nippon Kyobu Geka Gakkai Zasshi 1995;43(3):403–6. [PubMed]


