Abstract
Background
Studies investigating adverse events have traditionally been principally undertaken from a medical perspective. The impact that experience of an adverse event has on consumer confidence in health care is largely unknown. The objectives of the study were to seek public opinion on 1) the rate and severity of adverse events experienced in hospitals; and 2) the perception of safety in hospitals, so that predictors of lack of safety could be identified.
Methods
A multistage, clustered survey of persons residing in South Australia (2001), using household interviews (weighted n = 2,884).
Results
A total of 67% of respondents aged over forty years reported having at least one member of their household hospitalised in the past five years; with the average being two hospital admissions in five years. Respondents stated that 7.0% (95%CI: 6.2% to 7.9%) of those hospital admissions were associated with an adverse event; 59.7% of respondents (95% CI: 51.4% to 67.5%) rated the adverse event as really serious and 48.5% (95% CI: 40.4% to 56.8%) stated prolonged hospitalisation was required as a consequence of the adverse event. Perception of safety in hospitals was largely affected by the experience of an adverse event; really serious events were the most significant predictor of lack of safety in those aged 40 years and over (RR 2.38; p<0.001).
Conclusion
The experience of adverse events negatively impacted on public confidence in hospitals. The consumer-reported adverse event rate in hospitals (7.0%) is similar to that identified using medical record review. Based on estimates from other studies, self-reported claims of adverse events in hospital by consumers appear credible, and should be considered when developing appropriate treatment regimes.
Background
An adverse event is defined as an unintended injury or complication which results in death, disability or prolonged hospitalisation, and is caused by healthcare management [1]. Studies over the previous two decades have used various strategies to investigate the epidemiology of adverse events; most relate to hospitalised patients and are undertaken from a medical perspective [2].
Traditionally, the patient perspective on adverse events is obtained through complaints and litigation, which provide a somewhat biased picture, and likely underestimates the number of people dissatisfied with medical care [3]. For example, the elderly who are most at risk of adverse events [4] are also the least likely to complain [5]. Although patient surveys are increasingly being developed as valid tools to assess many facets of care provision [6], they are rarely used in investigating adverse events in hospitals.
Consumer surveys undertaken in the US and Australia have canvassed the opinions of adults regarding patient safety issues in health care and experiences of medical error [7-10]. However limitations in survey design have prevented comparison with rates determined from medical record review, the method most often cited to determine adverse event rates. We do not know whether the adverse event rate determined by consumers is congruent with that identified through medical record review undertaken by medical and nursing staff.
The aims of this study were to seek public opinion on:
1. the rate and severity of adverse events experienced in hospitals, using a lay definition, and
2. the perception of safety in hospitals
Methods
Data source
The data for this study were collected by household-based personal interview between September and November, 2001 [11]. The survey consisted of a multistage, systematic, clustered area sample (based on collector districts used by the Australian Bureau of Statistics in the 1996 Census [12]) of people aged 18 years or older living in metropolitan Adelaide, South Australia and country centres with a population exceeding 1000 (unweighted n = 2,945, weighted n = 2,884). The person in each household who had most recently had a birthday was interviewed. The survey was designed to have sufficient numbers to achieve a minimum of ± 1.75% accuracy with 95% confidence for any questionnaire item. Consent to participate in the survey was voluntary; no financial incentives were offered and interviewers obtained verbal consent prior to asking any questions of respondents.
Survey design
To determine the rate and severity of adverse events experienced in hospitals, respondents were asked, 'In the last five years, how many times have you and members of your current household been admitted to hospital?'. If there had been a hospitalisation they were then asked, 'With regard to those hospitals stays, did anything ever go wrong that you thought might have been due to the way the health care was carried out?'. If the respondent answered in the affirmative, they were then directed to rate the severity of the adverse event(s) on a three-point Likert scale of (1) not serious, (2) a little serious and (3) really serious, and whether or not they thought it required extra time in hospital. Details of the total household size were collected from respondents to calculate a household hospital admission rate.
To ascertain public confidence in hospitals, respondents were asked, 'With regard to mistakes made in medical treatment, how safe would you feel being admitted to a public hospital?'. Responses were rated on a four-point Likert scale of (1) very safe, (2) pretty safe, (3) a little unsafe and (4) very unsafe. Respondent demographic details obtained included age, gender, metropolitan/country residence, annual household income, country of birth and Indigenous status (Aboriginal and/or Torres Strait Islander origin).
Statistical analysis
A descriptive analysis was used to determine the adverse event rate and severity of the adverse event, with categorical variables reported as counts (percentages). To identify those most likely to have experienced an adverse event in their household and predictors of perceived lack of healthcare safety, univariate analyses were undertaken using weighted log binomial generalized linear modelling, followed by multivariate analysis aimed at determining the best joint predictors of safety. The conventional level of p ≤ 0.05 was taken to represent statistical significance.
Respondents who did not know how safe they felt being admitted to hospital were excluded from the analysis (representing 2.6% [n = 76] of all responses respectively). Analyses were weighted by age, sex and geographic region to be representative of the South Australian population (Table 1) [13]. The survey procedures of the Stata statistical software package were used [14].
Table 1.
Demographic profile of the respondent sample (weighted n = 2884), which was weighted by age, sex and geographical region to be comparable with the total population of South Australia in 2000 (n = 1,497,600) [13].
| Variable | Males | Females | Total | |||
| N | % | N | % | N | % | |
| Age (yrs) | ||||||
| 18–39 | 585 | 41.8 | 586 | 39.6 | 1171 | 40.6 |
| 40–59 | 499 | 35.6 | 505 | 34.1 | 1004 | 34.8 |
| 60+ | 318 | 22.7 | 391 | 26.4 | 709 | 24.6 |
| Total | 1402 | 100.0 | 1482 | 100.0 | 2884 | 100.0 |
| Residence | ||||||
| Country | 428 | 30.5 | 433 | 29.2 | 861 | 29.9 |
| Metropolitan | 974 | 69.5 | 1049 | 70.8 | 2023 | 70.1 |
| Total | 1402 | 100.0 | 1482 | 100.0 | 2884 | 100.0 |
| Annual Household Income (AUD) | ||||||
| ≤20,000 | 288 | 22.6 | 393 | 30.5 | 681 | 26.6 |
| 20,001–80,000 | 738 | 57.9 | 727 | 56.5 | 1465 | 57.2 |
| 80,001+ | 248 | 19.5 | 168 | 13.0 | 416 | 16.2 |
| Total | 1274 | 100.0 | 1288 | 100.0 | 2562 | 100.0 |
| Country of birth | ||||||
| Australia | ||||||
| ▪ Non-Indigenous | 1011 | 72.2 | 1091 | 73.6 | 2102 | 72.9 |
| ▪ Indigenous | 20 | 1.4 | 20 | 1.3 | 40 | 1.4 |
| Europe | ||||||
| ▪ UK/Ireland | 171 | 12.2 | 183 | 12.4 | 354 | 12.3 |
| ▪ Other | 97 | 6.9 | 92 | 6.2 | 189 | 6.5 |
| Asia | 30 | 2.1 | 28 | 1.9 | 58 | 2.0 |
| Other | 72 | 5.1 | 68 | 4.6 | 140 | 4.9 |
| Total | 1401 | 100.0 | 1482 | 100.0 | 2883 | 100.0 |
Results
From the initial 4,308 households selected randomly, 552 households were not contactable, 590 refused to be surveyed, 158 were either not available/too sick and 63 spoke no English. A total of 2,945 interviews were conducted (weighted n = 2,884), a participation rate of 78.4%. Table 1 shows the demographic profile of the respondents.
1. Consumer-reported adverse event rate and severity
With regard to the consumer-reported adverse event rate, we chose to analyse only the findings for households in which the individual surveyed was aged 40 years and over. It was considered that respondents aged less than 40 years might be less likely to provide reliable information about the experience of an adverse event in their household, particularly when asked to recall events occurring five years prior to the survey. As questions asked were in relation to the entire household, the sample pool consisted of 4,244 people (Figure 1).
Figure 1.
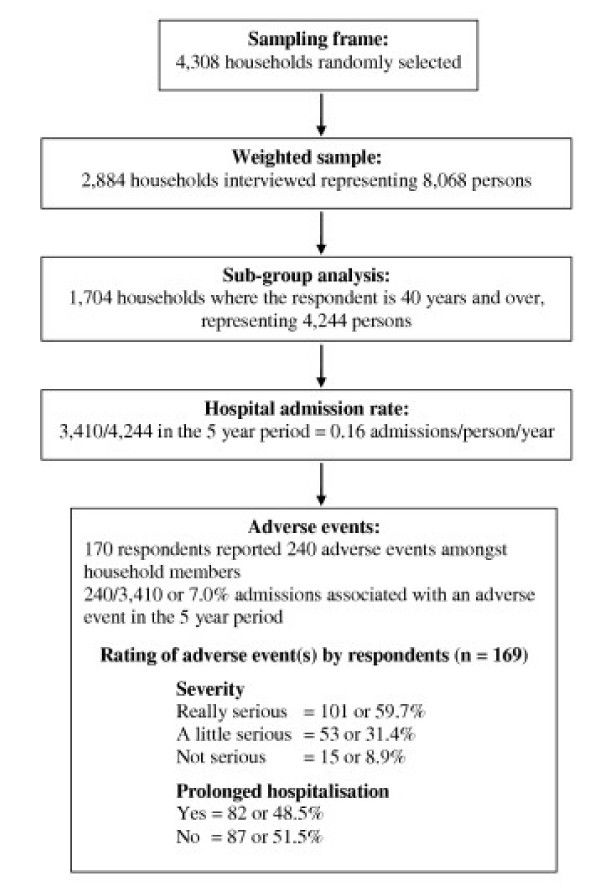
Flow diagram of adverse event rate and severity.
Of the 1,704 households surveyed where the respondent was aged 40 years or more, there were 1,137 (66.7%) where the respondent reported at least one hospital admission for any household member over the previous five years. This equated to 3,410 hospital admissions for all household members over the five year period. There were 11 respondents (6.5% of respondents aged 40 years and over) who did not know whether a household member had been admitted to hospital in the previous five years. Overall, 170 respondents (15.0%) reported that 240/3,410 or 7.0% (95%CI: 6.2% to 7.9%) of hospital admissions were associated with an adverse event over the five year period. When asked to rate the seriousness of the adverse event, 101 respondents (59.7%, 95% CI: 51.4% to 67.5%) rated the adverse event as really serious, and 82 (48.5%, 95% CI: 40.4% to 56.8%) indicated that extra time in hospital was required.
Tables 2 and 3 show the univariate and multivariate predictors of the likelihood of an adverse event occurring in the household of those aged 40 years and over. In Table 2, those more likely to have experienced one or more adverse events either to themselves or to a member of their household were aged less than 60 years or were an Indigenous Australian. In the multivariate model (Table 3), only being aged less than 60 years was a significant predictor.
Table 2.
Respondents aged 40 years and over who perceived that an adverse event had occurred to themselves or a household member – univariate analysis.
| Variable | Adverse event (%) | Total (N) | RR | 95% CI | Sig.* |
| Age (yr) | 1126 | ||||
| 40–59 | 17.3 | 648 | 1.00 | ||
| 60+ | 12.2 | 478 | 0.70 | 0.52 – 0.96 | 0.025 |
| Gender | 1126 | ||||
| Male | 13.7 | 542 | 1.00 | ||
| Female | 16.4 | 584 | 1.20 | 0.88 – 1.63 | 0.244 |
| Residence | 1126 | ||||
| Rural | 13.5 | 355 | 1.00 | ||
| Metropolitan | 15.8 | 771 | 1.17 | 0.80 – 1.69 | 0.417 |
| Country of birth | 1126 | ||||
| Australian: Non-Indigenous | 14.0 | 763 | 1.00 | ||
| Australian: Indigenous | 37.1 | 16 | 2.64 | 1.17 – 5.95 | 0.019 |
| Europe: UK/Ireland | 18.2 | 172 | 1.30 | 0.88 – 1.92 | 0.183 |
| Europe: Other | 15.8 | 113 | 1.12 | 0.67 – 1.88 | 0.654 |
| Asia | 8.4 | 15 | 0.60 | 0.09 – 3.91 | 0.595 |
| Other | 15.2 | 47 | 1.08 | 0.54 – 2.17 | 0.822 |
| Annual household income (AUD) | 1018 | ||||
| <$20,00 | 15.6 | 382 | 1.00 | ||
| $20,001–$80,000 | 15.8 | 489 | 1.02 | 0.73 – 1.41 | 0.928 |
| >$80,0001 | 15.6 | 147 | 1.00 | 0.59 – 1.69 | 0.996 |
* Weighted log binomial generalized linear model
Table 3.
Respondents aged 40 years and over who perceived that an adverse event had occurred to themselves or a household member – multivariate analysis.
| Variable | RR | 95% CI | Sig.* |
| Age (yr) | |||
| 40–59 | 1.00 | ||
| 60+ | 0.57 | 0.40 – 0.84 | 0.004 |
| Gender | |||
| Male | 1.00 | ||
| Female | 1.20 | 0.87 – 1.64 | 0.267 |
| Residence | |||
| Rural | 1.00 | ||
| Metropolitan | 1.16 | 0.79 – 1.71 | 0.454 |
| Country of birth | |||
| Australian: Non-Indigenous | 1.00 | ||
| Australian: Indigenous | 2.08 | 1.02 – 5.53 | 0.093 |
| Europe: UK/Ireland | 1.19 | 0.77 – 1.76 | 0.407 |
| Europe: Other | 1.06 | 0.60 – 1.78 | 0.844 |
| Asia | 0.58 | 0.09 – 3.64 | 0.553 |
| Other | 1.12 | 0.53 – 2.21 | 0.752 |
| Annual household income (AUD) | |||
| <$20,00 | 1.00 | ||
| $20,001–$80,000 | 0.83 | 0.57 – 1.20 | 0.322 |
| >$80,0001 | 0.73 | 0.42 – 1.29 | 0.280 |
* Weighted log binomial generalized linear model
2. Predictors of perceived lack of safety for respondents
To determine predictors of perceived lack of safety in hospitals, the total pool of 2,884 persons aged 18 years or older were interviewed. Of those interviewed, 5.2% (95% CI 4.4% – 6.1%) reported that they would feel very unsafe if admitted to hospital, 19.8% (95%CI 18.4% – 21.3%) stated that they would feel a little unsafe, 51.6% (95% CI 49.8% – 53.5%) stated that they would feel pretty safe and 23.3% (95% CI 21.8% – 24.9%) responded that they would feel very safe. Those who felt unsafe attending hospital were more likely to: be aged between 40 to 59 years, be female, reside in the metropolitan area, and have an annual household income greater than AUD $80,000 (Table 4). A strong predictor of feeling unsafe in hospital was having personally experienced an adverse event or knowing that a household member experienced an adverse event in the previous five years (Table 4). There was a gradient with the severity of the adverse event, i.e., the more severe the adverse event, the more the perception of lack of safety. In order to determine whether the experience of an adverse event affected respondents' perceptions of safety, multivariate analysis of those aged 40 years and over was undertaken. Multivariate analysis indicated that the best joint predictors for perceptions of lack of safety in public hospitals were being female, residing in a metropolitan area, having an income of between $20,000 and $80,000 and having either personally experienced a serious adverse event or being familiar with a household member who has (Table 5).
Table 4.
Public perceptions of lack of safety in public hospitals – univariate analysis.
| Variable | Feel unsafe (%) | Total (N) | RR | 95% CI | Sig.* |
| Age (yr) | 2819 | ||||
| 18–39 | 22.6 | 1157 | 1.00 | ||
| 40–59 | 29.2 | 988 | 1.29 | 1.09 – 1.52 | 0.002 |
| 60+ | 23.2 | 674 | 1.02 | 0.85 – 1.23 | 0.797 |
| Gender | 2819 | ||||
| Male | 22.7 | 1381 | 1.00 | ||
| Female | 27.3 | 1438 | 1.20 | 1.04 – 1.38 | 0.013 |
| Residence | 2820 | ||||
| Country | 18.2 | 844 | 1.00 | ||
| Metropolitan | 28.0 | 1976 | 1.54 | 1.2 6 – 1.87 | <0.001 |
| Country of birth | 2818 | ||||
| Australia: Non-Indigenous | 24.6 | 2067 | 1.00 | ||
| Australia: Indigenous | 25.6 | 39 | 1.00 | 0.52 – 1.94 | 0.991 |
| Europe: UK/Ireland | 24.5 | 343 | 0.99 | 0.81 – 1.22 | 0.954 |
| Europe: Other | 28.5 | 179 | 1.15 | 0.88 – 1.50 | 0.294 |
| Asia | 24.6 | 57 | 1.03 | 0.53 – 1.99 | 0.935 |
| Other | 28.6 | 133 | 1.16 | 0.86 – 1.57 | 0.331 |
| Annual household income | 2509 | ||||
| <$20,00 | 23.6 | 652 | 1.00 | ||
| $20,001–$80,000 | 24.5 | 1448 | 1.04 | 0.88 – 1.22 | 0.665 |
| >$80,0001 | 30.8 | 409 | 1.30 | 1.04 – 1.62 | 0.019 |
| Previous hospital-acquired adverse event † | 1091 | ||||
| No | 21.6 | 923 | 1.00 | ||
| Yes | 46.9 | 168 | 2.25 | 1.89 – 2.67 | <0.001 |
| Severity of that hospital-acquired adverse event † | 1091 | ||||
| No adverse event | 21.6 | 923 | 1.00 | ||
| Not serious | 29.2 | 15 | 1.06 | 0.49 – 2.23 | 0.898 |
| A little serious | 36.6 | 52 | 1.72 | .1.36 – 2.36 | 0.001 |
| Really serious | 54.6 | 101 | 2.72 | 2.27 – 3.25 | <0.001 |
* Weighted log binomial generalized linear model †respondents aged 40 years and over
Table 5.
Public perceptions of lack of safety in public hospitals (respondents aged 40 years and over) – multivariate analysis.
| Variable | RR | 95% CI | Sig.* |
| Age (yr) | |||
| 40–59 | 1.00 | ||
| 60+ | 0.80 | 0.61 – 1.03 | 0.085 |
| Gender | |||
| Male | 1.00 | ||
| Female | 1.28 | 1.02 – 1.60 | 0.032 |
| Residence | |||
| Rural | 1.00 | ||
| Metropolitan | 1.44 | 1.06 – 1.95 | 0.020 |
| Country of birth | |||
| Australian: Non-Indigenous | 1.00 | ||
| Australian: Indigenous | 0.50 | 0.18 – 1.40 | 0.187 |
| Europe: UK/Ireland | 0.83 | 0.60 – 1.14 | 0.251 |
| Europe: Other | 0.83 | 0.54 – 1.26 | 0.374 |
| Asia | 0.21 | 0.03 – 1.47 | 0.117 |
| Other | 1.07 | 0.63 – 1.80 | 0.806 |
| Annual household income (AUD) | |||
| <$20,00 | 1.00 | ||
| $20,001–$80,000 | 1.36 | 1.04 – 1.78 | 0.024 |
| >$80,0001 | 1.20 | 0.80 – 1.81 | 0.385 |
| Severity of that hospital-acquired adverse event | |||
| No adverse event | 1.00 | ||
| Not serious | 1.36 | 0.67 – 2.76 | 0.396 |
| A little serious | 1.68 | 1.12 – 2.51 | 0.011 |
| Really serious | 2.38 | 1.85 – 3.07 | <0.001 |
* Weighted log binomial generalized linear model
Discussion
When people were asked to comment on how safe they felt going to hospital, one in four respondents felt either a little or very unsafe. Respondents aged forty years and over were asked how many times they or household members had been hospitalised in the previous five years. In each household there were on average two hospital admissions over the previous five years. Seven percent of those hospitalisations were associated with an adverse event. People most likely to report an adverse event in the household were aged less than sixty years. Over half of respondents regarded the adverse event as being really serious, and a third indicated that the adverse event had delayed discharge from hospital.
Individual experience of an adverse event or knowledge of a household member who had suffered one while hospitalised had a deleterious impact on consumer confidence in hospitals. The severity of the adverse event was the key factor in determining the extent to which respondents felt unsafe, with serious adverse events leading to approximately a two-fold increase in the likelihood that a person would feel unsafe in public hospitals.
The finding that a significant proportion of respondents felt unsafe attending hospitals may be attributable to a number of factors; people generally present to hospitals in the acute stage of their illness, are usually unfamiliar with the surroundings and personnel, and often receive complex and numerous procedures in a short period of time. People feeling less safe when aware of an adverse event having occurred in their household during a hospital admission is likely due to them having gained a greater understanding of the inherent risks associated with being hospitalised. The finding that people aged less than sixty years were more likely to report an adverse event compared to older respondents is contrary to findings in the literature [4]. It may be that older respondents were less aware of an adverse event occurring than younger people, or more accepting of adverse events as expected complications of their increasingly complex health problems or less likely to complain because they fear recrimination [5]. Results may be biased by the fact that young people are more likely than elderly people to have a larger household size.
Perceived or real past experience of an adverse event occurring to a household member may impact upon the patient-healthcare worker relationship, particularly in terms of patient confidence, and this may, in turn, negatively impact on attendance at follow-up appointments and treatment compliance. Recognising those people most likely to feel unsafe, particularly those who have experienced an adverse event, should assist healthcare providers in understanding human behaviour, thereby enabling management strategies to be developed and individually customised to address these concerns. This might include strategies such as providing hospital in the home services and focusing on early discharge with community support, where appropriate.
The adverse event rate of seven percent identified in this study is within the range of that identified by medical record review, which has estimated that between 2.9% [15] and 16.6% [1] of hospital admissions were associated with adverse events. Even the higher rate likely underestimates the true incidence, given that many adverse events are not recorded in medical records [16], and prospective studies have identified high incidences [17,18]. Although our survey was applied specifically to hospital-acquired adverse events, other consumer studies have found that adverse events in any setting leads to diminished perceived safety in the healthcare environment [7,9]
There were several limitations to the study. Firstly, the survey represents self-reported experiences by the public, using lay judgement of what constitutes an adverse event based on their interpretation of the definition provided. Respondents may not have construed this definition in the same way as medical reviewers, who used strict criteria. Secondly, there are inherent risks when using data based on a person's recall, namely limitation of the amount and type of information retained by people over time (recall bias). While respondents might have experienced more than one adverse event for the household, they were only asked to rate one of them. It may be the case that, for those who reported multiple adverse events, only the most severe adverse event was cited, resulting in an overestimate of severity and an underestimate of the adverse event rate. Thirdly, adverse event rates might be underestimated through respondents being unfamiliar with household members' medical history or because errors may have been concealed from them [19,20].
Conclusion
The findings of this survey are of interest to public health professionals. Given that our consumer estimates of adverse events rates are similar to medical record review, claims of past adverse events by consumers would appear to be credible. If those who feel unsafe attending hospitals are themselves required to be hospitalised, strategies such as pre-admission hospital orientation and early discharge with hospital-in-the home services may assist in allaying fear. These and other strategies need to be considered when developing treatment regimes which best meet consumers' needs.
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
Sue Evans has made substantial contribution to conception and design and interpretation of the data. She has written several drafts of the paper.
Jesia Berry has provided statistical analysis, has assisted in the conception and design and interpretation of the data, and has assisted with writing the manuscript.
Brian Smith has contributed to the conception and design, writing and interpretation of the data and has authorised funding for the study.
Adrian Esterman has provided statistical consultancy and has provided assistance in writing the manuscript including revising the draft in line with reviewers comments.
All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
The authors would like to acknowledge the work of Harrison Health Research and the South Australian Department of Human Services Centre for Population Studies in Epidemiology in conducting the SA Health Omnibus survey. We would also like to thank staff of the Clinical Epidemiology and Health Outcomes Unit, Mr Adrian Heard and Mr Colin McIver for their contribution to the project.
Contributor Information
Sue M Evans, Email: sue.evans@med.monash.edu.au.
Jesia G Berry, Email: jesia.berry@flinders.edu.au.
Brian J Smith, Email: brian.smith@nwahs.sa.gov.au.
Adrian J Esterman, Email: adrian.esterman@unisa.edu.au.
References
- Wilson RM, Runciman WB, Gibberd RW, Harrison BT, Newby L, Hamilton JD. The Quality in Australian Health Care Study. Med J Aust. 1995;163:458–71. doi: 10.5694/j.1326-5377.1995.tb124691.x. [DOI] [PubMed] [Google Scholar]
- Karson AS, Bates DW. Screening for adverse events. J Eval Clin Pract. 1999;5:23–32. doi: 10.1046/j.1365-2753.1999.00158.x. [DOI] [PubMed] [Google Scholar]
- Allsop J, Mulcahy L. Doctors' responses to patient complaints. In: Rosenthal MM, Mulcahy L, Lloyd-Bostock S, editor. Medical Mishaps: Pieces of the Puzzle. Buckingham, UK: Open University Press; 1999. [Google Scholar]
- Thomas EJ, Brennan TA. Incidence and types of preventable adverse events in elderly patients: population based review of medical records. BMJ. 2000;320:741–4. doi: 10.1136/bmj.320.7237.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allsop J, Mulcahy L. Dealing with clinical complaints. In: Vincent CE, editor. Clinical Risk Management. London: BMJ Publishing Group; 2001. [Google Scholar]
- Cleary PD. The increasing importance of patient surveys. Now that sound methods exist, patient surveys can facilitate improvement. BMJ. 1999;319:720–1. doi: 10.1136/bmj.319.7212.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Patient Safety Foundation at the AMA . Public Opinion of Patient Safety Issues Research Findings. Louis Harris and Associates; 1997. http://www.npsf.org/download/1997survey.pdf: [Google Scholar]
- Kaiser Family Foundation/Agency for Healthcare Research and Quality . National Survey on Americans as Health Care Consumers: An update on the role of quality information. Rockville, MD: Henry J Kaiser Family Foundation; 2000. [Google Scholar]
- Clark R, Australian Patient Safety Survey . Final Report to the Commonwealth Department of Health and Aged Care. Canberra, Australia: Commonwealth of Australia; 2001. http://www.participateinhealth.org.au/clearinghouse [Google Scholar]
- Blendon RJ, DesRoches CM, Brodie M, Benson MA, Rosen AB, Schneider E, Altman DE, Zapert K, Herrmann MJ, Steffenson AE. Views of practicing physicians and the public on medical errors. N Engl J Med. 2002;347:1933–40. doi: 10.1056/NEJMsa022151. [DOI] [PubMed] [Google Scholar]
- Wilson D, Wakefield M, Taylor A. The South Australian Health Omnibus Survey. Health Promotional J Aust. 1992;2:47–9. [Google Scholar]
- Australian Bureau of Statistics . How Australia takes a census collection. (Catalogue no. 2903.0) . Canberra, Australia: ABS; 2001. [Google Scholar]
- Australian Bureau of Statistics . Estimated Resident Population by Age and Sex in Statistical Local Areas, South Australia. Canberra, Australia: ABS; 2001. (Catalogue no. 3235.4) [Google Scholar]
- Stata statistical software, Version Release 8.0. College Station, TX: Stata Corporation; 2001. [Google Scholar]
- Thomas EJ, Studdert DM, Burstin HR, Orav EJ, Zeena T, Williams EJ, Howard KM, Weiler PC, Brennan TA. Incidence and types of adverse events and negligent care in Utah and Colorado. Med Care. 2000;38:261–71. doi: 10.1097/00005650-200003000-00003. [DOI] [PubMed] [Google Scholar]
- O'Neil AC, Petersen LA, Cook EF, Bates DW, Lee TH, Brennan TA. Physician reporting compared with medical-record review to identify adverse medical events. Ann Intern Med. 1993;119:370–6. doi: 10.7326/0003-4819-119-5-199309010-00004. [DOI] [PubMed] [Google Scholar]
- Andrews LB, Stocking C, Krizek T, Gottlieb L, Krizek C, Vargish T, Siegler M. An alternative strategy for studying adverse events in medical care. Lancet. 1997;349:309–13. doi: 10.1016/S0140-6736(96)08268-2. [DOI] [PubMed] [Google Scholar]
- Bellomo R, Goldsmith D, Russell S, Uchino S. Postoperative serious adverse events in a teaching hospital: a prospective study. Med J Aust. 2002;176:216–8. doi: 10.5694/j.1326-5377.2002.tb04376.x. [DOI] [PubMed] [Google Scholar]
- Leape LL. Error in medicine. JAMA. 1994;272:1851–7. doi: 10.1001/jama.272.23.1851. [DOI] [PubMed] [Google Scholar]
- McIntyre N, Popper K. The critical attitude in medicine: the need for a new ethics. Br Med J (Clin Res Ed) 1983;287:1919–23. doi: 10.1136/bmj.287.6409.1919. [DOI] [PMC free article] [PubMed] [Google Scholar]


