Abstract
Background: Sedative-hypnotic drugs impair memory, but details regarding the nature of this effect are unknown. The influences of propofol, thiopental, and dexmedetomidine on the performance of a task that isolates specific components of episodic memory function were measured.
Methods: Working (1 intervening item, 6 s) and long-term memory (10 intervening items, 33 s) were tested using auditory words in a continuous recognition task before and during drug administration. Eighty-three volunteer participants were randomly assigned to receive a constant target concentration of drug or placebo, producing sedative effects from imperceptible to unresponsiveness. Responsive participants were categorized as high or low performers, using a median split of long-term memory performance during drug administration. Recognition of words at the end of the study day was assessed.
Results: High performers had acquisition of material into long-term memory when drug was present at the same level as placebo. Retention of this material at 225 min was significantly less for propofol (39 ± 23% loss of material) than for other drugs (17-23% loss; P < 0.01). Greater sedation in low performers was evident in multiple measures. Memory for words presented before drug was no different from that associated with placebo for all groups.
Conclusions: Lack of retention of material acquired into long-term memory during propofol administration, associated with minimal sedation, seems to define drug-induced amnesia. Sedation seems to impair the acquisition or encoding of material into long-term memory. Therefore, the putative targets of drug-induced amnesia by propofol are processes associated with retention of material in long-term memory.
MEMORY has been classified into two broad categories, working memory (i.e., short-term memory) and long-term memory. Information held in working memory has a limited capacity and lasts for only a few seconds without rehearsal, 1 whereas essentially unlimited amounts of information may be stored indefinitely in long-term memory. Long-term memory can been subclassified into two broad categories, explicit and implicit, with explicit memories being dependent on hippocampal function and implicit memories being independent of the hippocampus. 2 Explicit memories have frequently been further classified into semantic memory (i.e., general knowledge about the world) and episodic memory (i.e., personal memories). Episodic memories differ from semantic memories because they consist of a memory for both the particular item and the spatiotemporal context in which that item occurred.
Sedative-hypnotic drugs affect attention. It is well known that unattended stimuli do not enter working or explicit memory systems and processes. Therefore, all sedative-hypnotic drugs impair episodic memory for stimuli presented during drug administration because all of these drugs produce sedation. At maximal drug effect, no episodic memory exists for the presented stimuli because the drug has caused unresponsiveness. The degree of memory impairment is measured by the lack of recall or recognition of material presented during drug administration.
However, sedation is not the only factor that can impair episodic memory of material presented during drug administration. There are many suggestive data to support the idea that a different form of drug-induced memory impairment can be separated from the sedative effects of the drug.3-5 The term drug-induced amnesia will be used to describe this property of certain sedative-hypnotic drugs. Mechanisms underlying episodic memory impairment by drugs are not well understood. A previous study of regional cerebral blood flow (rCBF) changes when propofol was given to produce significant memory impairment, but low sedation effect, revealed depressed rCBF in regions associated with working memory.6 Therefore, working memory may be a target of the effect of propofol on episodic memory. Given that memory processes can be disrupted in a variety of ways, it is necessary to measure the drug effect on each component process.
One memory paradigm that permits the simultaneous assessment of attention and working memory influences on encoding and the retrieval of long-term memory is the continuous recognition memory task (CRT; fig. 1). Participants are presented with a continuous stream of stimuli, some of which are being experienced for the first time (i.e., new) and some of which are repeated (i.e., old). The participant's task is simply to make one response if the item is new and a different response if the item is old. By manipulating the number of intervening items (i.e., lag) between the first and second presentation of a particular item, one can control which memory system, working memory or long-term memory, is used to make the decision. That is, very short lags require the use of working memory, whereas lags involving delays of more than a few seconds require the use of long-term memory. Importantly, the fact that every stimulus requires a decision, whether new or old, means that the participant's level of attention can be assessed. That is, sedation will result in a longer reaction time for these decisions, or lack of response when items are unattended. Finally, longer-term retention of material can be assessed by administering a recognition test of previously presented items after the drug effect has worn off.
Fig. 1.
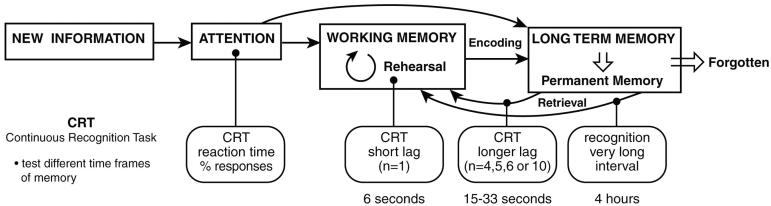
A model of episodic memory relevant to drug effect. Material must be attended to before it can enter into memory. New information can be present initially in working memory. To retain information for longer periods, it must be either rehearsed (e.g., remembering a new phone number) or incorporated into long-term memory (remembering a phone number given to you yesterday). The continuous recognition task (CRT) not only allows different temporal aspects of memory to be tested, but also can measure the attention to new material.
In this study, propofol is contrasted with thiopental, a primarily sedative drug administered as an active control. Although it is difficult to do, the different memory effects of propofol can be separated from those of thiopental.3 Dexmedetomidine is a new sedative-hypnotic agent with a unique mechanism of action that also impairs episodic memory.7-9 On approval for clinical use, participants in the current study were also randomized to receive this drug after data collection had started with propofol/thiopental.
Drugs were given at low, medium, or high target concentrations.∥ These produced behavioral effects from barely discernible to unresponsiveness. Data were analyzed based on the behavioral state of the participant during drug administration rather than initial randomization because of overlap of drug effect between randomized groups. Of primary interest in this study was memory impairment evident at final recognition of material presented when the drug was given at minimal levels of sedation. The least effect of sedation was seen when stimuli were successfully encoded into long-term memory, an event that was measured by the longest lag interval in the CRT. Therefore, participants with evidence of successful acquisition of material into long-term memory (high performers) were analyzed separately from those who did not demonstrate this success during drug administration (low performers). Although they were exposed to stimuli, these still responsive subjects provided no corroboration that stimuli had been acquired from working memory into long-term memory.
Materials and Methods
Participants
Eighty-three healthy right-handed volunteers were recruited by newspaper advertisement and gave informed consent to participate in this Institutional Review Board (Memorial Sloan-Kettering Cancer Center, New York, New York)-approved protocol. Volunteers were required to have normal hearing, as assessed by a screening questionnaire,10 and were not taking any centrally acting medications. Exclusion criteria included body mass index greater than the 85th percentile (27.3 for females, 27.8 for males), history of drug or alcohol abuse, medical or psychiatric illness, a first-degree relative with schizophrenia, or allergy to medications used in this study. Fifty-four percent of the volunteers had a college degree or higher level of education; more than 10% had only a high school level education. Fluency in English was assessed with the Wechsler Adult Intelligence Scale-Revised vocabulary test. Age-normed percentile ranks were well above the median (mean, 77.8; SD, 22.9). Volunteers attended an orientation session in which the study procedures were explained in detail, a brief physical examination was performed, and practice was allowed on the experimental tasks. Volunteers were excluded if they could not perform at a level of 70% correct recognition (on lag10 items, see below) after two tries on a trial version of the CRT (all stimuli different from those used on the study day but similar duration of test). Volunteers were paid for their participation. Participants consisted of 51 males and 32 females with a mean age of 31.3± 8.2 yr and a mean weight of 73.4 ±18.7 kg.
Overview of Study Day Procedures
Participants had no food or drink from midnight the night before the study. All experimental procedures were completed within a single session, approximately 9 AM to 6 PM. An intravenous catheter and an arterial line for blood samples were placed, and participants were fitted with headphones (foam ear plug inserts; EarLink Auditory Systems, Indianapolis, IN) for presentation of auditory stimuli. Saline solution containing 5% dextrose was administered throughout the study, at a rate of approximately 125 ml/h. The electroencephalogram was recorded using a 64-channel QuickCap (NeuroScan, El Paso, TX). These electroencephalographic data are reported separately. The Bispectral Index (BIS) was recorded using Ziprep electrodes and an Aspect 1050 monitor (Aspect Medical Systems, Natick, MA). Various experimental tasks were performed before (baseline) and during infusion (drug condition), approximately 1 h later. A bathroom break was provided before starting the drug infusion. Instructions for each experimental task were read to the subject from a prepared script, so that all subjects received the same instructions. Before the task was started, subjects were asked whether the instructions were understood, and further explanation was provided if needed. This report focuses on the CRT. After equilibration of predicted effect site and serum concentrations, initial measures of sedation were obtained, and the CRT was performed. After collection of this and other data, drug infusion was discontinued, and the arterial line was removed. Lunch was served after the volunteer recovered from sedation. While waiting for the delayed recognition test at the end of the day, volunteers could watch movies or read. Participants were discharged using standard criteria for ambulatory surgery.
Study Drugs
Participants were randomly assigned to receive propofol (n = 30), thiopental (n = 31), dexmedetomidine (n = 10), or placebo (n = 12) in one of three doses via STANPUMP# to provide steady state concentrations throughout the infusion over approximately 90 min. Target concentrations were as follows: 0.3, 1.2, or 2.5μg/ml propofol; 2, 5, or 7 μg/ml thiopental; 0.25 or 0.5-0.8 ng/ml dexmedetomidine.**
Measurement of Sedation Performed Immediately before and during CRT
Various measures of sedation were obtained and include the Maddox Wing test of binocular coordination, subjective ratings of sedation using the Norris Visual Analog Scale (VAS), BIS values, reaction time to correctly identified word stimuli, and the standard Observer's Assessment of Alertness/Sedation scale measure.
Maddox Wing
The Maddox Wing test measures deviation, in prism diopters, of the ocular muscles from the fusion point in binocular vision, which increases with central drug effect. The Maddox Wing test is sensitive to the effects of sedation with inhalational anesthetics,11 propofol,12 and alcohol.13 In the current study, these measurements were made before, during, and after drug infusion. Although this test was performed twice during drug infusion, the data used from the drug condition are those obtained just before the CRT test commenced.
Visual Analog Scale
We used the same VAS task as in previous studies from our laboratory3,14 implemented for computer presentation. VAS was measured using 16 pairs of adjectives, with the subject asked to make a mark on a computer display (anywhere on a 10-cm line) to indicate his or her current state. VAS measurements were taken twice during drug administration; the data used here are from the measurement just before the CRT test. VAS scores on 8 of the adjective pairs were combined into measures of Physical Sedation (weak, clumsy, lazy, incompetent) and Mental Sedation (drowsy, fuzzy, slow, dreamy), which were then averaged for statistical analysis (Average Sedation, maximum score = 40). This reduction of VAS data has been previously shown to represent sedation effect accurately.3
Reaction Time
Reaction time on the CRT task was automatically recorded as the delay between stimulus onset and response. Reaction times reported here are only for correct responses to previously heard words.
Bispectral Index
The BIS, an index of depth of hypnosis in volunteers receiving sedative-hypnotic drugs,15 was measured continuously and automatically recorded using Datalogger software (Aspect Medical Systems) using a standard clinical electrode montage (Ziprep electrodes). Recording was commenced just before drug infusion and continued until drug infusion was discontinued. Data reported are those obtained during the CRT.
Observer's Assessment of Alertness/Sedation
Two experimenters made independent ratings of sedative effect using this scale while the participant was performing the CRT.16 This instrument uses a five-point scale to evaluate responsiveness, quality of speech (e.g., slowness or slurring), facial expression (e.g., slack jaw), and eyelid ptosis (drooping). Observers were blinded to group assignments while they made their ratings. Scores used for analysis were the mean of both raters' ratings on a summary or composite score, ranging from 1 (deep sleep) to 5 (alert).
Continuous Recognition Task
All stimuli in this task were presented as auditory stimuli through foam earphones. The auditory CRT as used here consists of 220 words (one word presented every 3 s; list length, 11 min) with a majority but not all of the words being repeated once at varying, unpredictable intervals. This single repetition occurred after 1 intervening word (lag1); after 4, 5, or 6 intervening words (lag5); or after 10 intervening words (lag10). Volunteer participants were required to push one of two buttons to indicate whether they had heard the word before. They were instructed as follows: “For every single word you hear, you have to make a decision, whether it's a new word or an old word. Try to make your decision as quickly as you can, because you only have about 2 s before the next word is presented. If you respond too late, your response won't count. So try to be quick— but accurate.” Lag5 words were staggered with 4, 5, or 6 intervening words to reduce expectation bias. Given that one item was presented every 3 s, these lags represent memory that occurred 6 s (lag1, working memory only), 15-21 s (lag5, probably long-term memory), and 33 s (lag10, clearly long-term memory; fig. 1) after first presentation of the item. The button press response allowed calculation of reaction time and detection accuracy. Separate word lists were used in the orientation (124 words), baseline (124 words), and drug (220 words) conditions. Two-syllable words from the Toronto Word Pool17 (word frequency in English language < 100; mean auditory length, 766 ms) were digitized for computer presentation and were presented every 3 s over 11 min. All stimuli were balanced for frequency in the English language, concreteness, and auditory word length. Pilot tests in volunteer participants showed that 11 min was the maximal duration of time a subject could perform the task and maintain adequate attention. Therefore, the CRT lists were designed with a parsimonious selection of stimulus categories and number of repetitions. The list presented in the baseline condition had 124 words (lag1, lag5: n = 0; lag10 repeated: n = 40; distractors: n = 44), and the list presented in the drug condition had 220 words (lag1 repeated: n = 35; lag5 repeated: n = 20; lag10 repeated: n = 50; distractors: n = 10). Lag1 and lag5 words were omitted during the baseline condition to shorten the test duration of an already long list of words.
Recognition Memory Testing
Recognition testing was performed several hours after the drug condition, at a time when serum concentrations of drug according to STANPUMP software were below those previously demonstrated to have no measurable memory or sedative effect. During recognition testing, participants gave an old/new response to previously presented words and novel distractors, with the same instructions as detailed above. The recognition test was constructed from the same word pool as the CRT lists, using the same considerations previously described. Because of the long lists of words needed for testing, only lag10 words from baseline and drug conditions were included in a counterbalanced design with an equal number of distractors. Because of excessive list length and probable inattention of the subject at the end of the day for very long word lists, only a subset of old words (n = 35 each for baseline and drug lists) were presented in this 9-min-long task. Because we wanted the subject to have ample time to recognize words from the beginning of the study day, words were presented every 4 s for this test. Subjects were asked to press a button for each word, either “old” if the word had been previously heard at any time during the study day or “new” if not. Because all stimuli were counterbalanced and randomized, recognition testing was reported as a proportional rate, rather than being derived from an absolute value of testing for all stimuli presented.
Statistical Analysis
Participants included in this report responded to at least 10% of all stimuli presented during infusion, irrespective of correctness of response.
Group Assignment
Although assignment to drug dose was randomized, participants' reactions to different doses of drug were variable and overlapping between assignment groups. Therefore, analysis was performed on the basis of the subject's memory responses during drug infusion. To study effects of drug on long-term memory performance, participants in each drug group were divided at the median score for percent correct responses to lag10 words during drug administration (median for propofol: 38%, thiopental: 41%, dexmedetomidine: 45%; differences not significant), forming groups of high and low performers for each drug. High performers represented a group of participants that provided evidence of initial encoding of material into long-term memory.
Data for 9 participants were not included (placebo: n = 3; propofol: n = 4; thiopental: n = 2) for any of the following reasons: less than 50% correct score on lag10 words at baseline (< 2 SDs below mean), missing data at recognition, interruptions in the infusion, or absence of detectable drug effect, if the subject had received active drug. Data were analyzed by independent t tests and analysis of variance (ANOVA), with significance set at P < 0.05. One-way ANOVAs were performed using SPSS version 11.5 (Chicago, IL). A priori contrasts compared each group to placebo.
Results
Results on the behavioral measures of sedation and memory are presented in tables 1 and 2. Significant a priori comparisons against placebo are so indicated.
Table 1.
Measures of Sedation
| Variable | Placebo (n = 8) | Propofol High (n = 8) | Thiopental High (n = 8) | Dexmedetomidine High (n = 4) | Propofol Low (n = 9) | Thiopental Low (n = 9) | Dexmedetomidine Low (n = 4) |
|---|---|---|---|---|---|---|---|
| Responses to all stimuli, % Baseline | 92.5 (10.4) | 94.3 (7.6) | 97.3 (5.8) | 98.6 (1.9) | 95.0 (7.1) | 94.5 (6.6) | 88.9 (12.8) |
| Drug | 90.2 (8.9) | 85.8 (12.1) | 89.4 (12.3) | 83.8 (10.5) | 63.3 (11.6) | 45.6 (26.4) | 52.4 (32.0) |
| Maddox Wing, diopters Baseline | 4.34 (3.61) | 4.54 (2.96) | 3.84 (4.38) | 2.38 (1.31) | 3.81 (4.05) | 3.19 (2.06) | 9.00 (7.78) |
| Drug | 5.69 (4.61) | 7.89 (2.02) | 6.09 (5.27) | 3.56 (2.97) | 9.61 (3.12)* | 8.56 (3.78) | 16.38 (4.19)‡ |
| Visual analog scale average sedation, mm Baseline | 9.80 (8.14) | 8.14 (4.12) | 6.83 (6.29) | 13.50 (6.10) | 11.93 (7.70) | 12.39 (4.69) | 13.83 (8.85) |
| Drug | 13.36 (11.21) | 11.43 (7.14) | 18.38 (9.40) | 25.31 (2.37)* | 19.25 (8.48) | 28.09 (5.02)† | 25.86 (5.47)† |
| Reaction time to correct lag10 words, ms Baseline | 1,217 (111) | 1,035 (160)* | 1,064 (125) | 891 (66) | 1,161 (162) | 1,159 (181) | 1,231 (100) |
| Drug | 1,213 (148) | 1,232 (217) | 1,274 (139) | 1,109 (73) | 1,417 (131)‡ | 1,486 (208)‡ | 1,460 (114)‡ |
| Bispectral Index, Hz Baseline | — | — | — | — | — | — | — |
| Drug | 93.79 (3.27) | 93.52 (4.14) | 94.25 (4.63) | 92.98 (3.69) | 87.97 (5.79)* | 91.56 (2.91) | 85.09 (6.07)* |
| Observer's Assessment of Alertness/Sedation Baseline | 4.81 (0.37) | 4.94 (0.18) | 4.44 (1.40) | 4.88 (0.25) | 4.11 (1.76) | 4.75 (0.38) | 5.00 (0.0) |
| Drug | 4.56 (0.50) | 4.50 (0.46) | 3.69 (1.10) | 4.00 (0.41) | 3.56 (0.88)* | 3.31 (0.75)† | 3.00 (0.71)* |
Mean (SD) values on measures of sedation at baseline and during drug. Participants are classified by level of performance during drug infusion (high = above or low = below median for percent correct responses to repeated stimuli on continuous recognition task). Median for propofol = 38%, thiopental = 41%, dexmedetomidine = 45%. A priori contrast vs. placebo:
P ≤ 0.05
P ≤ 0.01
P ≤ 0.001
Table 2.
Measures of Memory Performance
| Variable | Placebo (n = 8) | Propofol High (n = 8) | Thiopental High (n = 8) | Dexmedetomidine High (n = 4) | Propofol Low (n = 9) | Thiopental Low (n = 9) | Dexmedetomidine Low (n = 4) |
|---|---|---|---|---|---|---|---|
| Lag1 words, % correct Baseline | — | — | — | — | — | — | — |
| Drug | 95.3 (3.7) | 90.0 (10.5) | 89.6 (10.7) | 90.0 (7.5) | 50.5‡(24.5) | 41.4‡(29.1) | 47.1*(27.4) |
| Lag5 words, % correct Baseline | — | — | — | — | — | — | — |
| Drug | 81.3 (10.3) | 81.9 (14.4) | 80.0 (8.5) | 72.5 (20.2) | 22.8‡ (17.0) | 21.3‡ (16.9) | 40.0 (29.4) |
| Lag10 words, % correct Baseline | 78.4 (12.2) | 90.6* (8.1) | 80.0 (11.7) | 87.5 (7.4) | 85.3 (12.1) | 76.3 (12.0) | 85.6 (13.8) |
| Drug | 73.3 (13.0) | 70.3 (21.8) | 62.2 (14.2) | 56.5 (12.4) | 23.1‡ (12.2) | 21.0‡ (15.5) | 25.0‡ (17.2) |
| Recognition lag10 words, % correct Baseline | 56.8 (14.8) | 42.5 (23.2) | 43.6 (21.4) | 57.9 (21.6) | 56.2 (25.6) | 55.0 (18.7) | 40.0 (27.1) |
| Drug | 61.4 (14.1) | 31.4† (21.9) | 39.3* (18.6) | 33.6* (20.0) | 29.5† (19.5) | 26.5‡ (18.8) | 17.9‡ (28.2) |
| Decrement, % Baseline to recog test | -21.7 (14.4) | -48.1† (21.2) | -31.7 (22.7) | -29.6 (23.2) | -29.1 (18.9) | -23.5 (13.2) | -45.7* (17.6) |
| Decrement, % Drug to recog test | -11.9 (8.4) | -38.8† (23.0) | -17.2 (18.8) | -22.9 (8.0) | +6.4 (24.1) | +2.1 (21.2) | -7.2 (19.2) |
| False alarms to new words During drug | 4.7 (3.8) | 8.4 (4.7) | 5.5 (6.6) | 4.3 (1.2) | 9.2 (11.0) | 4.8 (3.6) | 15.9 (15.1) |
| At recog test | 23.8 (13.7) | 12.9 (9.4) | 21.2 (16.7) | 19.6 (13.4) | 16.4 (9.7) | 22.0 (14.1) | 14.3 (13.8) |
| Time, min CRT drug to recog test | 217 (32) | 223 (9) | 235 (23) | 236 (28) | 210 (23) | 228 (14) | 246 (15) |
Mean (SD) scores (% correct responses) to continuous recognition task (CRT) test given at baseline, during drug, and delayed recognition (Recog test). Participants are classified by level of performance during drug infusion (high = above or low = below median for percent correct responses to repeated stimuli on CRT memory task). Median for propofol = 38%, thiopental = 41%, dexmedetomidine = 45%. A priori contrast vs. placebo:
P ≤ 0.05
P ≤ 0.01
P ≤ 0.001.
Sedation
As measured by reaction time, BIS (fig. 2), VAS, or Maddox Wing (fig. 3), sedation levels were higher for low-performing participants than for high-performing participants but similar within group, regardless of drug administered (table 1). Low performers, however, were not deeply sedated (“out of it”), because they still responded to 54% of all stimuli presented, compared with high performers, who responded to 87%. The number of correct responses on lag1, lag5, and lag10 words and distractor stimuli in high performers did not differ from the number of correct responses from placebo participants. For low performers, the number of hits was much lower for lag1, lag5, and lag10 words than in the placebo group (P < 0.001 for these stimulus categories).
Fig. 2.
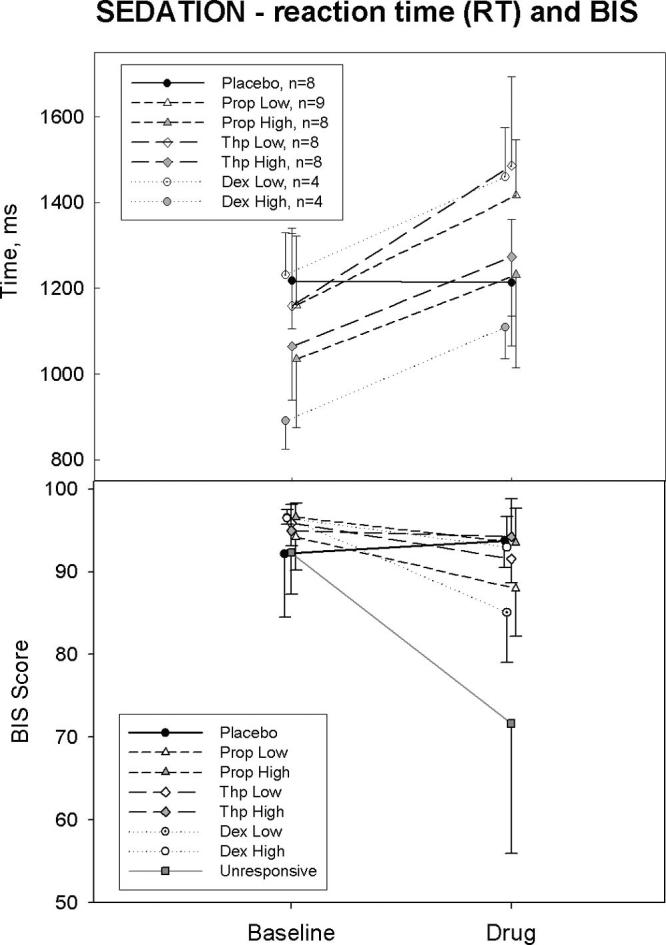
Sedation effect as measured by reaction time (RT, top) and Bispectral Index (BIS, bottom). Low-performing subjects (those with low lag10 performance scores during drug administration, gray symbols) demonstrated a greater sedative effect in comparison with high-performing subjects (open symbols) during drug administration. Unresponsive subjects had significantly lower BIS scores and are not included in data analyses. In this and other graphs, error bars represent SDs.
Fig. 3.
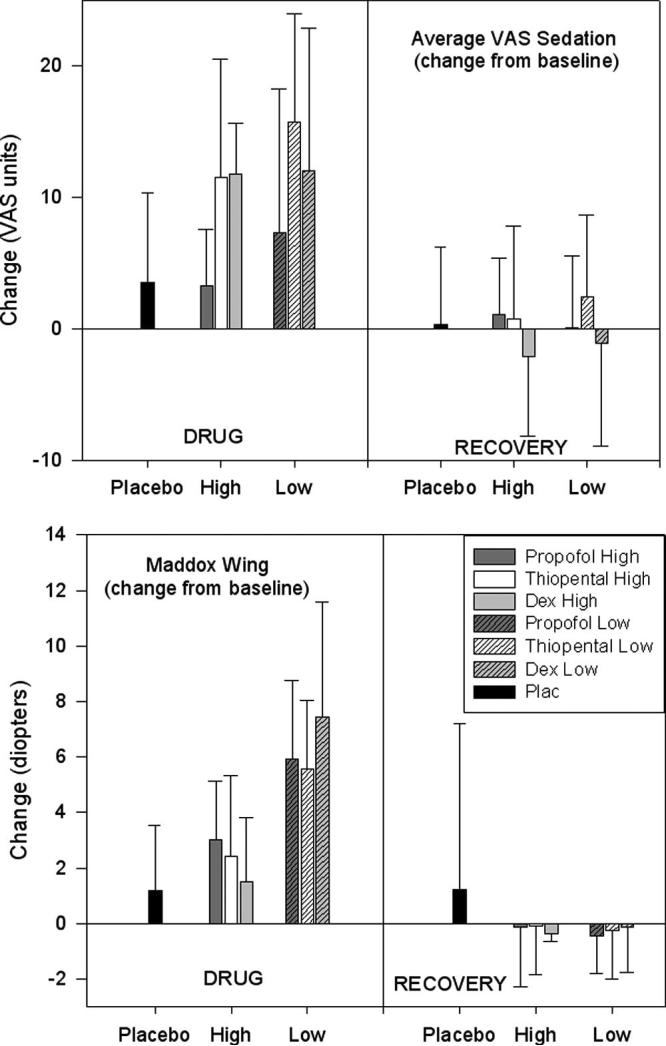
Sedation effect as measured by the Norris Visual Analog Scale (VAS; Physical and Mental Sedation combined, maximum score of 40; top) and the Maddox Wing (bottom), a test of exophoria, in prism diopters. During drug administration, low performing subjects (those with performance scores below the median during drug administration, striped bars) were more sedated than placebo subjects by self-ratings (VAS) and more sedated than high-performing subjects (solid bars) on the Maddox Wing test. Dex = dexmedetomidine; Plac = placebo.
Maddox Wing
There were no differences between high- and lowperforming groups at baseline. During drug infusion, horizontal changes (exophoria) were more marked than vertical changes, which did not differ from placebo in any group. Low-performing participants showed greater exophoria than high-performing participants did (across drugs: P = 0.001). The placebo group increased 1.3 ±2.5 diopters on average, but this was significantly less than the increases in the propofol (5.8 ± 3.2 diopters) and thiopental low performer groups (5.4 ± 2.6 diopters; P < 0.001 and P < 0.01, respectively, compared with placebo).
Visual Analog Scale
Self-ratings of sedation increased markedly in participants receiving drug, more so in the low performers (on a 40-point scale, an increase of 11.4 ± 10.2 over baseline levels) compared with the high performers (increase of 8.3 ± 7.5). The increase in self-rated sedation did not differ significantly between low and high performers (P = 0.258, not significant), probably due to high variability in this measure. Placebo participants showed only a 3.6 ± 6.8 increase in sedation ratings during the equivalent time period. All low-performing participants rated themselves as significantly more sedated than placebo participants (P = 0.035). High-performing participants did not differ from participants in the placebo group (P = 0.198, not significant).
Reaction Time
Low performers (thiopental: n = 8; propofol: n = 9; dexmedetomidine: n = 4) had a significantly greater reaction time of 225 ms or 18% more than high performers (P < 0.001). There was no change in reaction time for placebo participants. Interestingly, although the increase in reaction time with drug was the same for all groups, participants who were classified as high performers had significantly faster reaction times at baseline than the other two groups (P = 0.002 vs. placebo; P = 0.001 vs. low performers; fig. 2).
Bispectral Index
Before drug infusion, BIS levels were in the mid 90s and did not differ between high-and low-performing participants. During drug infusion, BIS values were lower (89 ± 5) for participants in the low performance group than those in the high performance group overall (94 ± 4; P = 0.001). Participants not responsive to verbal command or strong tactile stimulus (n = 23) had BIS values of 72 ± 16. Some pressed the button a few times before becoming unresponsive. These unresponsive participants (propofol: n = 8; thiopental: n = 13; dexmedetomidine: n = 2) are not included in this report.
Observer's Assessment of Alertness/Sedation
There were no differences between groups at baseline. Observer ratings of sedation showed no change in high-performing participants receiving any of the three drugs. Low-performing participants were rated as significantly more sedated than either placebo participants (P ≤ 0.001) or participants in the high-performing group (P ≤ 0.005).
Memory Performance on the CRT
At baseline, combining data from all participants, the percent correct performance on the lag10 words was82.9 ± 11.7%, with participants in the high-performing propofol group (90.6 ± 8.1) performing better than placebo (table 2, P < 0.04 vs. placebo; no other group different from placebo, ANOVA omnibus F test not significant for all groups combined). Distractors were correctly identified as new 88.6 ± 11.7% of the time. During drug infusion, high-performing participants, including propofol high performers, responded similarly to placebo on lag1, lag5, and lag10 words and false alarms (generally less than 10-15%; table 2). As expected by group assignment, low-performing participants demonstrated poor memory performance during drug compared with baseline (P < 0.001 for lag1, lag5, and lag10 words; figs. 4 and 5). The ability to correctly identify distractors decreased from 80-90% at baseline to 40-50% during drug.
Fig. 4.
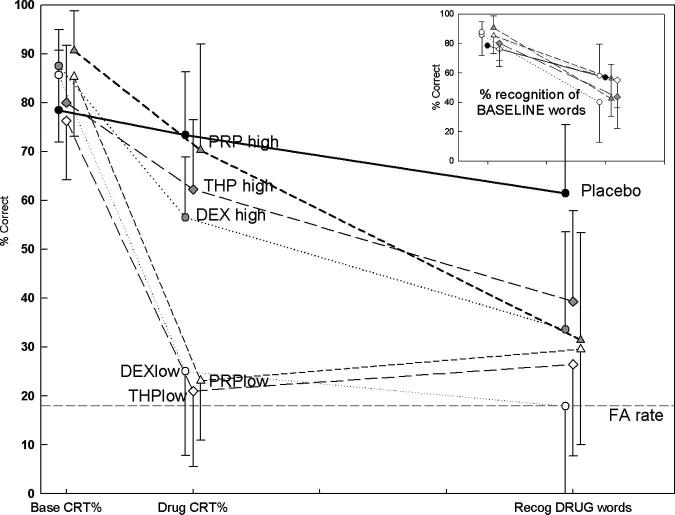
Memory performance for recognition of lag10 words on the continuous recognition task (CRT) at baseline and during drug administration and final recognition memory at the end of the study day. The first two points (Base CRT% and Drug CRT%) represent the percent correct recognition of lag10 words presented 33 s previously on the CRT. The final point, Recog DRUG words, is recognition of lag10 words presented during Drug CRT. Note that propofol (PRP) demonstrates a steeper slope, or greater information loss, of initially acquired material when compared with thiopental (THP) or dexmedetomidine (DEX). Propofol also demonstrates a sedative effect, as exemplified by low performers. Subjects in this category, regardless of drug, never acquired words during presentation and did not have any recognition of them, despite exposure to these stimuli during responsiveness. The small box in the upper right corner represents performance on CRT at baseline and recognition of these baseline words at the end of the day. There was no difference among groups overall by analysis of variance at baseline. FA = false alarm rate.
Fig. 5.
Comparison of performance on lag1, lag5, and lag10 words during drug administration. High performers (top lines) had a decrement in performance from lag1 through lag5 and lag10 words. Low performers (bottom lines), experiencing greater sedation, still had better performance on lag1 than lag5 or lag10 words. Interestingly, lag5 performance was no different from lag10 performance, indicating that the relation of performance with lag duration is different during sedation (there are only four subjects in the DEX low performer group). Sedation seems to interfere primarily with transfer of material from working memory, measured by lag1 performance, into long-term memory, measured by lag5 and lag10 performance. Dex = dexmedetomidine; Prop = propofol; Thp = thiopental.
Recognition at the End of the Day
As described above, results from the recognition test are for previously presented lag10 words. Delayed recognition testing for lag1 and lag5 words was not performed. Delayed recognition testing was started an average of 225 ± 23 min after drug infusion. There were no significant differences in this interval between groups (P < 0.09 by one-way ANOVA); the group with the longest delay was low-performing dexmedetomidine at 246 min (P = 0.054 vs. placebo). Selection of this time period was largely determined by predicted effect site concentrations as determined by STANPUMP, and recognition testing occurred at concentrations previously demonstrated to have no memory or sedative effects.3
All drugs produced memory impairment on the delayed recognition test (fig. 4). Placebo participants recognized a similar number of baseline (mean, 57%) and drug condition words (mean, 61%). Participants who received active drug recognized a mean of 49% of baseline words (range, 3-91%). For drug condition words, recognition in high-performing participants was significantly lower than that in placebo participants (propofol: 31%; thiopental: 39%; dexmedetomidine: 34%, as compared with placebo: 61%). Low-performing participants recognized few drug condition words (P < 0.002 vs. placebo). There were no differences between groups in the false-alarm rate during the recognition test (18.4 ±12.4% overall) or during drug infusion (7.3 ± 7.8% over-all, excluding placebo).
Drug-induced Amnesia: Lack of Recognition for Successfully Acquired Stimuli
Drug-induced amnesia was measured by retention of material successfully acquired into long-term memory during drug administration. A measure of this retention was the change or decrement in correct responses to lag10 words on the drug CRT and recognition tested 3.5-4 h later (fig. 6). The decrement seen in the placebo group over this time interval was 11.9 ± 8.4%. This decrement was larger in participants receiving drug and was greatest in the high-performing participants receiving propofol (38.8 ± 23.0; P = 0.008 vs. placebo). This group had a significantly greater decrement than did the high-performing group receiving thiopental (17.2 ±18.8; P = 0.037 vs. high-performing propofol group). Low-performing participants, who experienced greater sedative effect, showed decrements of varying but small magnitude because their initial acquisition of the words was at a much lower level. The profile of memory impairment by dexmedetomidine was identical to that by thiopental, with a smaller decrement than propofol.
Fig. 6.
Time-related recognition performance. This graph demonstrates the lack of retention of successfully acquired material in the high performer groups over the time interval from encoding during drug administration to recognition testing, 3-4 h later at the end of the study day. Participants who were more deeply sedated during drug effect (low performers) never encoded the stimuli during drug effect and thus had little change in retention over time. D = dexmedetomidine; P = propofol; Plac = placebo; T = thiopental.
The decrement from baseline to delayed recognition testing was 21.7 ± 14.4% in the placebo group. There were no significant differences in this decrement between groups overall (omnibus significance F = 2.0, P = 0.085 by ANOVA), although the decrement in high-performing propofol participants was significantly greater than that in the placebo group (48.1 ± 21.2; P = 0.007, a priori comparison). However, this decrement may be related to the possibly better baseline memory performance of high-performing propofol subjects (a priori t test vs. placebo, P = 0.037, although the omnibus F test of ANOVA for all groups was not significant [F = 1.6, P = 0.17]). Similarly, low-performing dexmedetomidine participants had a higher decrement on baseline words compared with placebo participants (P = 0.043, a priori contrast).
Discussion
The current study demonstrates that material can be successfully encoded into long-term memory during drug administration, as represented by the high-performing groups. However, in the case of propofol, the retention of this material is particularly poor. The low-performing groups are characterized by the inability to encode material into long-term memory during drug administration and a greater degree of sedation than the high-performing groups. These findings point to multiple effects of these drugs on episodic memory.
Both drugs used in the current study produce sedation. In addition, propofol seems to have an effect on memory that is not the result of sedation. This type of memory impairment is typified by the results of the propofol high performance group, which demonstrates increased information loss over time in comparison with other drugs (fig. 6). Different forms of memory impairment have been demonstrated previously, although the distinction is made with some difficulty.4,18,19 If recognition or recall of previously presented material is only tested after a certain time after presentation of the material, much information regarding the effects of drug on memory processes is potentially lost. For example, working memory is active for only a few seconds, and acquisition of material into longterm memory starts in this time frame. The continuous recognition task provides information about memory processes during the presentation of stimuli using a randomized, concurrent design, as shown in figure 1. Although drug-induced amnesia, exemplified by the benzodiazepines, has been described as interference with acquisition of new information,20-22 data from this study reveal a defect of retention of successfully acquired material as a potential defining characteristic of sedation-independent memory impairment, or drug-induced amnesia.
Despite being exposed to the same stimuli as the high performers, recognition memory for material presented to low performers was no different than chance, regardless of drug administered. Low performers were still responsive but clearly more sedated than high performers. Working memory, although affected by sedation, was still functioning to a large extent to classify words as old or new most of time, as long as the lag interval was short. This is shown by the reliably better performance on lag1 than lag10 or lag5 words in this group (fig. 5). Interestingly, low performers had no better performance than chance on both lag5 and lag10 words. Therefore, performance at higher levels of sedation is not simply related to lag duration. This further supports the concept that the primary effect of sedation on episodic memory is to interfere with encoding of material into long-term memory. As far as a dose-response effect is concerned, likely the first discernible effect of drug-induced sedation on episodic memory is the inability to encode material into long-term memory during drug administration.
Aside from sedation, another form of drug impairment of episodic memory is revealed by the lack of retention of material successfully acquired into long-term memory during drug administration. To highlight its difference from sedation, we call this effect on episodic memory drug-induced amnesia. This effect would be measured by less and less recognition performance over time and would be greater than the normal rate of forgetting in a control group. This effect is apparent only on material encoded during drug administration, because there was no difference in delayed recognition of words presented at baseline compared with placebo (small box in fig. 4). Because the drugs were administered approximately 50 min after the baseline CRT task, this indicates that normal retention of material in long-term memory occurs after this time period regardless of subsequent drug administration.
The lack of retention of material acquired into long-term memory during propofol administration may not be a conclusive result, largely based on better baseline performance of high performers in the propofol group.†† It should be noted that these participants performed at the same level during drug administration as high performers receiving other drugs (including placebo), not only on lag10 material, but also on lag1 and lag5 material. Therefore, if there were some innately better memory performance in propofol high performers, it was not evident during the drug CRT. These are the critical data on which the main conclusions are based. Nevertheless, results from this study would be more conclusive if all participants performed at a higher level during drug (“training to criterion”). Likewise, final recognition scores of words presented during drug administration in active drug groups were all less than 40%, possibly representing a basement effect. Somewhat different constructions for the CRT list were used for baseline and drug conditions. The rate of “forgetting” may be related to the somewhat different structuring of memory tasks at different time points, including the recognition task. We believe that the influence of this confound is small, because the placebo group did not demonstrate significant differences between scores in baseline and drug CRT tasks. Because randomization to the dexmedetomidine group was started after the study was begun, this drug was administered to a small number of subjects, and results from this group should be interpreted with caution. Despite these limitations, the results of this study support previous indications from other testing paradigms that propofol and midazolam interfere with the retention of material acquired into long-term memory.
We have previously demonstrated the “fragility” of the memory formed in the presence of drug as assessed by a learning paradigm, the Rey Auditory-Verbal Learning Test. This task measures the memory for a repeatedly presented, 15-item word list.23 When one tries to learn these words during repeated presentations, words in this task are encoding into long-term memory. A notable characteristic of the drug-induced memory impairment on these recently learned words is the large effect of interference by subsequent material. When an interference list was presented during drug administration, recall of just-learned material was no better than on the first presentation. This is in marked contrast to the control condition, where little information loss occurred after presentation of this interfering material. Therefore, a potential mechanism for lack of retention of long-term memory is the interference of newly presented material. Delayed recognition of material presented on the Rey Auditory-Verbal Learning Test reveals remarkably similar effects of propofol, midazolam, and thiopental over this time period. However, differences among midazolam, propofol, and thiopental were evident in serial position effects of the first presentation of the word list. This well-described effect occurs in recall of a supraspan list, one that is larger than seven plus or minus two items.24,25 Normally items from the beginning and end of the list are remembered more successfully than the middle of the list, creating a U-shaped response. This effect is likely due to two processes: easier recall of recently presented information, the recency effect, and sequential rehearsal of material at the beginning more than the middle of the list, the primacy effect. Despite impairment of recognition memory similar to that caused by other drugs, thiopental had little influence on the serial position effect, whereas both propofol and midazolam interfered with the primacy but not the recency effect. Analysis of similar data obtained from a previous study where sedation effects were closely matched3 reveals a similar trend.‡‡ As evidenced by the recency effect, which was not affected by any of these drugs, relatively normal encoding of new material occurs. However, later recall of successfully acquired information is less for propofol and midazolam than for thiopental, possibly because of interference by intervening words.
These results taken together suggest plausible possibilities that point to potential avenues for further investigation. Having identified retention in long-term memory as the likely mode of drug-induced amnesia, one can consider potential mechanisms underlying this effect using a large body of animal and functional neuroimaging literature on long-term memory processes. Investigations of cellular mechanisms responsible for the formation of explicit memories in animals indicate that such memories are formed in the hippocampus by a process of long-term potentiation. At the molecular level, long-term potentiation seems to consist of an early process (roughly 0-30 min) dependent on protein kinases and a late process (> 30 min) involving gene mechanisms and subsequent neuronal structural changes.26,27 Early hippocampal processes are also identified by patterns of electrophysiologic activity, such as electroencephalographic synchrony between hippocampal and nearby brain regions28 These hippocampal processes, along with others (such as repetitive retrieval and reencoding29) help to consolidate new memories into permanent, long-term memory. Lack of retention of material in long-term memory may be due to effects on any number of short-term or long-term hippocampal processes. One such marker of long-term hippocampal processes, neuronal polysialylation, is inhibited by propofol in animals.30
Previous results from imaging rCBF changes with propofol may provide additional clues as to how propofol affects episodic memory. These studies have demonstrated that there is little effect of propofol on rCBF in medial temporal lobe structures which include the hippocampus.6 In marked contrast, rCBF decreases do occur in various neocortical regions, e.g., the parietal association cortex. Hippocampal and parietal regions are connected to each other via polysynaptic pathways.31More and more evidence points to the interaction of the hippocampal-complex structures with neocortical regions shortly after acquisition of new material.32-35 Interference with this interaction may explain decreased subsequent recognition of material, because normal retention of memory requires ongoing processing of recently acquired information.29,36
In conclusion, memory impairment during propofol administration in minimally sedated volunteers may involve mechanisms that come into play after the successful acquisition of material into long-term memory. We propose that drug-induced amnesia is characterized by successful encoding of material into long-term memory, which is subsequently not well retained. Contrasting with this effect is that of sedation, which seems to prevent initial encoding of material into long-term memory. The results of this study indicate that future investigations regarding drug-induced amnesia should focus on long-term memory processes, some of which start within a short time period of stimulus presentation.
Footnotes
Dexmedetomidine was randomized to only two concentrations: low and medium.
Shafer S: STANPUMP program. Available at: http://anesthesia.stanford.edu/pkpd. Accessed March 17, 2004.
Because randomization to dexmedetomidine was started after the study had begun, only doses affecting memory (low and medium) were targeted. The medium dose represents a range based on subject behavioral response (sedation) at the time of drug administration, before the CRT was administered. It is emphasized that data were analyzed based on memory performance, which was unknown at the time of data collection.
However, this difference is borderline; the omnibus value in the ANOVA test is not significant, although a priori comparison with placebo is significant.
Difference between propofol and thiopental on recall of the words for the beginning third of the list, P = 0.10.
Supported by grant No. R01 GM58782 from the National Institutes of Health, Bethesda, Maryland. Aspect Medical Systems, Natick, Massachusetts, loaned the equipment used to collect Bispectral Index data. Presented in part at the American Society of Anesthesiologists Annual Meeting, San Francisco, California, October 11-15, 2003, the 50th Annual Meeting of the Association of University Anesthesiologists, Milwaukee, Wisconsin, May 1-4, 2003, and the Cognitive Neuroscience Society, New York, New York, March 30-April 1, 2003.
References
- 1.Baddeley A. The episodic buffer: A new component of working memory? Trends Cogn Sci. 2000;4:417–23. doi: 10.1016/s1364-6613(00)01538-2. [DOI] [PubMed] [Google Scholar]
- 2.Cohen NJ, Squire LR. Preserved learning and retention of pattern-analyzing skill in amnesia: Dissociation of knowing how and knowing that. Science. 1980;210:207–10. doi: 10.1126/science.7414331. [DOI] [PubMed] [Google Scholar]
- 3.Veselis RA, Reinsel RA, Feshchenko VA, Wronski M. The comparative amnestic effects of midazolam, propofol, thiopental, and fentanyl at equisedative concentrations. Anesthesiology. 1997;87:749–64. doi: 10.1097/00000542-199710000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Curran HV, Pooviboonsuk P, Dalton JA, Lader MH. Differentiating the effects of centrally acting drugs on arousal and memory: An event-related potential study of scopolamine, lorazepam and diphenhydramine. Psychopharmacology (Berl) 1998;135:27–36. doi: 10.1007/s002130050482. [DOI] [PubMed] [Google Scholar]
- 5.Veselis RA, Reinsel RA, Feshchenko VA. Drug-induced amnesia is a separate phenomenon from sedation: Electrophysiologic evidence. Anesthesiology. 2001;95:896–907. doi: 10.1097/00000542-200110000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Veselis RA, Reinsel RA, Feshchenko VA, Dnistrian AM. A neuroanatomical construct for the amnesic effects of propofol. Anesthesiology. 2002;97:329–37. doi: 10.1097/00000542-200208000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Nelson LE, Lu J, Guo T, Saper CB, Franks NP, Maze M. The alpha2-adrenoceptor agonist dexmedetomidine converges on an endogenous sleeppromoting pathway to exert its sedative effects. Anesthesiology. 2003;98:428–36. doi: 10.1097/00000542-200302000-00024. [DOI] [PubMed] [Google Scholar]
- 8.Hall JE, Uhrich TD, Barney JA, Arain SR, Ebert TJ. Sedative, amnestic, and analgesic properties of small-dose dexmedetomidine infusions. Anesth Analg. 2000;90:699–705. doi: 10.1097/00000539-200003000-00035. [DOI] [PubMed] [Google Scholar]
- 9.Ebert TJ, Hall JE, Barney JA, Uhrich TD, Colinco MD. The effects of increasing plasma concentrations of dexmedetomidine in humans. Anesthesiology. 2000;93:382–94. doi: 10.1097/00000542-200008000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Coren S, Hakstian AR. The development and cross-validation of a selfreport inventory to assess pure-tone threshold hearing sensitivity. J Speech Hear Res. 1992;35:921–8. doi: 10.1044/jshr.3504.921. [DOI] [PubMed] [Google Scholar]
- 11.Pollard BJ, Bryan A, Bennett D, Faragher EB, Un EN, Keegan M, Wilson A, Burkill M, Beatty PCW, Stollery BT, Snowdon AT, Healy TEJ. Recovery after oral surgery with halothane, enflurane, isoflurane or propofol anaesthesia. Br J Anaesth. 1994;72:559–66. doi: 10.1093/bja/72.5.559. [DOI] [PubMed] [Google Scholar]
- 12.Zuurmond WWA, Balk VA, van Dis H, van Leeuwen L, Paul EAA. Multidimensionality of psychological recovery from anaesthesia. Anaesthesia. 1987;44:889–92. doi: 10.1111/j.1365-2044.1989.tb09141.x. [DOI] [PubMed] [Google Scholar]
- 13.Thapar P, Zacny JP, Thompson W, Apfelbaum JL. Using alcohol as a standard to assess the degree of impairment induced by sedative and analgesic drugs used in ambulatory surgery. Anesthesiology. 1995;82:53–9. doi: 10.1097/00000542-199501000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Norris H. The action of sedatives on brain stem oculomotor systems in man. Neuropharmacology. 1971;10:181–91. doi: 10.1016/0028-3908(71)90039-6. [DOI] [PubMed] [Google Scholar]
- 15.Glass PS, Bloom M, Kearse L, Rosow C, Sebel P, Manberg P. Bispectral analysis measures sedation and memory effects of propofol, midazolam, isoflurane, and alfentanil in healthy volunteers. Anesthesiology. 1997;86:836–47. doi: 10.1097/00000542-199704000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Chernik DA, Gillings D, Laine H, Hendler J, Silver JM, Davidson AB, Schwam EM, Siegel JL. Validity and reliability of the Observer's Assessment of Alertness/Sedation Scale: Study with intravenous midazolam. J Clin Psychopharmacol. 1990;10:244–51. [PubMed] [Google Scholar]
- 17.Rubin DC, Friendly M. Predicting which words get recalled: Measures of free recall, availability, goodness, emotionality, and pronunciability for 925 nouns. Mem Cognit. 1986;14:79–94. doi: 10.3758/bf03209231. [DOI] [PubMed] [Google Scholar]
- 18.Ghoneim MM, Block RI. Learning and memory during general anesthesia. Anesthesiology. 1997;87:387–410. doi: 10.1097/00000542-199708000-00027. [DOI] [PubMed] [Google Scholar]
- 19.Curran HV, Birch B. Differentiating the sedative, psychomotor and amnesic effects of benzodiazepines: A study with midazolam and the benzodiazepine antagonist, flumazenil. Psychopharmacology. 1991;103:519–23. doi: 10.1007/BF02244252. [DOI] [PubMed] [Google Scholar]
- 20.Curran HV. Benzodiazepines, memory and mood: A review. Psychopharmacology. 1991;105:1–8. doi: 10.1007/BF02316856. [DOI] [PubMed] [Google Scholar]
- 21.Ghoneim MM, Mewaldt SP. Benzodiazepines and human memory: A review. Anesthesiology. 1990;72:926–38. [PubMed] [Google Scholar]
- 22.Hinrichs JV, Mewaldt SP, Ghoneim MM, Berie JL. Diazepam and learning: Assessment of acquisition deficits. Pharmacol Biochem Behav. 1982;17:165–70. doi: 10.1016/0091-3057(82)90280-5. [DOI] [PubMed] [Google Scholar]
- 23.Reinsel R, Veselis R, Wronski M, Marino P, Heino R, Alagesan R. Memory impairment during conscious sedation: A comparison of midazolam, propofol and thiopental, Memory and Awareness. In: Sebel PS, Bonke B, Winograd E, editors. Anesthesia. Englewood; New Jersey, Prentice-Hall: 1993. pp. 127–40. [Google Scholar]
- 24.Miller GA. The magical number seven, plus or minus two: Some limits on our capacity for processing information. Psychol Rev. 1956;63:81–97. [PubMed] [Google Scholar]
- 25.Brodie DA, Prytulak LS. Free recall curves: Nothing but rehearsing some items more or recalling them sooner? J Verbal Learning Verbal Behav. 1975;14:549–63. [Google Scholar]
- 26.Abel T, Lattal KM. Molecular mechanisms of memory acquisition, consolidation and retrieval. Curr Opin Neurobiol. 2001;11:180–7. doi: 10.1016/s0959-4388(00)00194-x. [DOI] [PubMed] [Google Scholar]
- 27.Steward O, Worley PF. A cellular mechanism for targeting newly synthesized mRNAs to synaptic sites on dendrites. Proc Natl Acad Sci U S A. 2001;98:7062–8. doi: 10.1073/pnas.131146398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fell J, Klaver P, Lehnertz K, Grunwald T, Schaller C, Elger CE, Fernandez G. Human memory formation is accompanied by rhinal-hippocampal coupling and decoupling. Nat Neurosci. 2001;4:1259–64. doi: 10.1038/nn759. [DOI] [PubMed] [Google Scholar]
- 29.Maguire EA, Vargha-Khadem F, Mishkin M. The effects of bilateral hippocampal damage on fMRI regional activations and interactions during memory retrieval. Brain. 2001;124:1156–70. doi: 10.1093/brain/124.6.1156. [DOI] [PubMed] [Google Scholar]
- 30.O'Gorman DA, O'Connell AW, Murphy KJ, Moriarty DC, Shiotani T, Regan CM. Nefiracetam prevents propofol-induced anterograde and retrograde amnesia in the rodent without compromising quality of anesthesia. Anesthesiology. 1998;89:699–706. doi: 10.1097/00000542-199809000-00021. [DOI] [PubMed] [Google Scholar]
- 31.Duvernoy HM, Bourgouin P. Vascularization and Serial Sections with MRI. 2nd Springer; Berlin and New York: 1998. The Human Hippocampus: Functional Anatomy; p. 29. [Google Scholar]
- 32.Johnson R., Jr . Event-related potential insights into the neurobiology of memory systems. In: Johnson RJ, Baron JC, editors. Handbook of Neuropsychology. Elsevier Science; Amsterdam and New York: 1995. pp. 135–63. [Google Scholar]
- 33.Fernandez G, Effern A, Grunwald T, Pezer N, Lehnert K, Duempelmann M, Van Roost D, Elger CE. Real-time tracking of memory formation in the human rhinal cortex and hippocampus. Science. 1999;285:1582–5. doi: 10.1126/science.285.5433.1582. [DOI] [PubMed] [Google Scholar]
- 34.Klimesch W, Doppelmayr M, Schwaiger J, Winkler T, Gruber W. Theta oscillations and the ERP old/new effect: independent phenomena? Clin Neurophysiol. 2000;111:781–93. doi: 10.1016/s1388-2457(00)00254-6. [DOI] [PubMed] [Google Scholar]
- 35.Hasselmo ME, Bodelon C, Wyble BP. A proposed function for hippocampal theta rhythm: Separate phases of encoding and retrieval enhance reversal of prior learning. Neural Comput. 2002;14:793–817. doi: 10.1162/089976602317318965. [DOI] [PubMed] [Google Scholar]
- 36.Stark CE, Squire LR. Functional magnetic resonance imaging (fMRI) activity in the hippocampal region during recognition memory. J Neurosci. 2000;20:7776–81. doi: 10.1523/JNEUROSCI.20-20-07776.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]


