Abstract
Background
Socioeconomic status appears to be an important predictor of coronary angiography use after acute myocardial infarction. One potential explanation for this is that patients with lower socioeconomic status live in neighbourhoods near nonteaching hospitals that have no catheterization capacity, few specialists and lower volumes of patients with acute myocardial infarction. This study was conducted to determine whether the impact of socioeconomic status on angiography use would be lessened by considering variations in the supply of services.
Methods
We examined payment claims for physician services, hospital discharge abstracts and vital status data for 47 036 patients with acute myocardial infarction admitted to hospitals in Ontario between April 1994 and March 1997. Neighbourhood income of each patient was obtained from Canada's 1996 census. Using multivariate hierarchical logistic regression and adjusting for baseline patient and physician factors, we examined the interaction among hospital and regional characteristics, socioeconomic status and angiography use in the first 90 days after admission to hospital for acute myocardial infarction.
Results
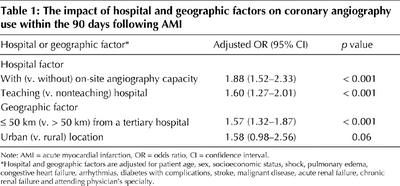
Within each hospital and geographic subgroup, crude rates of angiography rose progressively with increases in neighbourhood income. After adjusting for sociodemographic, clinical and physician characteristics, hospitals with on-site angiography capacity (adjusted odds ratio [OR] 1.88, 95% confidence interval [CI] 1.52–2.33), those with university affiliations (adjusted OR 1.60, 95% CI 1.27–2.01) and those closest to tertiary institutions (adjusted OR 1.57, 95% CI 1.32–1.87) were all associated with higher 90-day angiography use after acute myocardial infarction. However, the relative impact of socioeconomic status on 90-day angiography use was similar whether or not hospitals had on-site procedural capacity (interaction term p = 0.68), had university affiliations (interaction term p = 0.99), were near tertiary facilities (interaction term p = 0.67) or were in rural or urban regions (interaction term p = 0.90).
Interpretation
Socioeconomic status was as important a predictor of angiography use in hospitals with ready access to cardiac catheterization facilities as it was in those without. The socioeconomic gradient in the use of angiography after acute myocardial infarction cannot be explained by the distribution of specialists or tertiary hospitals.
Socioeconomic status is an important determinant of angiography use following acute myocardial infarction (AMI) in Canada.1,2 One possible explanation for the disparity in angiography use after AMI is that patients with lower socioeconomic status live in neighbourhoods near hospitals without university affiliations that have fewer specialists and less advanced technology and treat a lower volume of patients with AMI than hospitals with university affiliations. There are 3 reasons why this hypothesis seems plausible in Canada. First, after adjusting for patient case-mix differences, on-site procedural capacity at the admitting hospital, teaching status, and distance between the admitting hospital and the closest tertiary institution are all important determinants of angiography use in Canada (and elsewhere).1,2,3,4,5,6,7,8 Second, before the advent of universal health care, specialized medical services tended to be concentrated in affluent urban areas.9,10 Third, there is a general inverse correlation between rural areas and affluence, and between rural areas and hospital and provider characteristics.11,12 If the regional organization of specialty services in the Canadian hospital system provides access on the basis of socioeconomic status, then the system's equity would be improved with a broader diffusion of specialty services. Conversely, if socioeconomic disparities are similar across different types of institutions, then other policy initiatives are required to make the system fairer. The objective of this study was to examine the interactions among hospital and regional characteristics, socioeconomic status and coronary angiography use among patients admitted to hospital with AMI in Ontario.
Methods
We used the Ontario Myocardial Infarction Database (OMID), which links a variety of population-based administrative data sources in Ontario.13 The accuracy and validity of this database has been previously reported.13,14 As in other published studies,2,4,15 the median personal income of neighbourhoods (taken from 1996 Canadian census data) was selected as an indicator of socioeconomic status.2 Neighbourhoods were defined using postal code data (forward sortation area). This study received ethics approval from Sunnybrook & Women's College Health Sciences Centre, Toronto, Ont.
We conducted multivariate analyses using hierarchical logistic models, after adjusting for baseline patient and physician characteristics, to examine the interaction among socioeconomic status, hospital and geographic factors, and angiography use post-MI. These models incorporated random effects in order to consider the clustering of patients within hospitals and regions and to account for the fact that variables were measured at the patient, physician and institution levels of the data hierarchy. In so doing, the effect of socioeconomic status was allowed to vary randomly across admitting hospital and regional characteristics. We examined 4 main hospital or regional factors: on-site angiography capacity at the admitting hospital; proximity of the admitting hospital to the closest tertiary cardiac institution (using latitude and longitude); university affiliation; and whether or not the admitting hospital was in a rural or urban location. All statistical models were adjusted for patient-level factors (i.e., the validated AMI mortality prediction rule variables16): age, sex, cardiogenic shock, congestive heart failure, pulmonary edema, arrhythmias, diabetes with complications, malignant disease, stroke, acute renal failure, chronic renal failure and physician characteristics (the specialty of the admitting physician). Statistical significance was defined as p < 0.05 for all analyses.
Results
The cohort consisted of 47 036 patients with AMI who were admitted to hospital between Apr. 1, 1994, and Mar. 31, 1997. The mean age was 67.1 years, and 36.3% of patients were female. The following were found to be independent predictors of higher angiography use post-MI: living in a higher-income neighbourhood (p = 0.001), being younger (p < 0.001), being male (p < 0.001), having low-risk clinical markers (i.e., the absence of shock, congestive heart failure, pulmonary edema, diabetes with complications, malignant disease, stroke and renal failure, p < 0.001 for each factor) and the specialty of the attending physician (p < 0.001). After adjusting for sociodemographic, clinical and physician characteristics, hospitals with on-site procedural capacity (p < 0.001) and university affiliations (p < 0.001), and those closest to tertiary institutions (p < 0.001), were each associated with higher rates of coronary angiography use after AMI. Urban hospitals had a nonsignificant trend toward higher angiography use post-MI (p = 0.06) (Table 1).
Table 1
Table 2 shows that the absolute rates of angiography per 100 patients with AMI rose progressively with increases in neighbourhood income across all hospital and geographic subgroups. However, as illustrated in Fig. 1, the relative effect of socioeconomic status (every $10 000 increase in neighbourhood income) on 90-day angiography use after AMI was similar for hospitals with or without on-site procedural capacity (interaction term p = 0.68) or university affiliation (interaction term p = 0.99), and regardless of distance from tertiary facilities (interaction term p = 0.67), or whether they were rural or urban (interaction term p = 0.90). In short, socioeconomic status was as important a predictor of angiography use in hospitals with ready access to cardiac catheterization facilities as it was in those with limited access.
Table 2
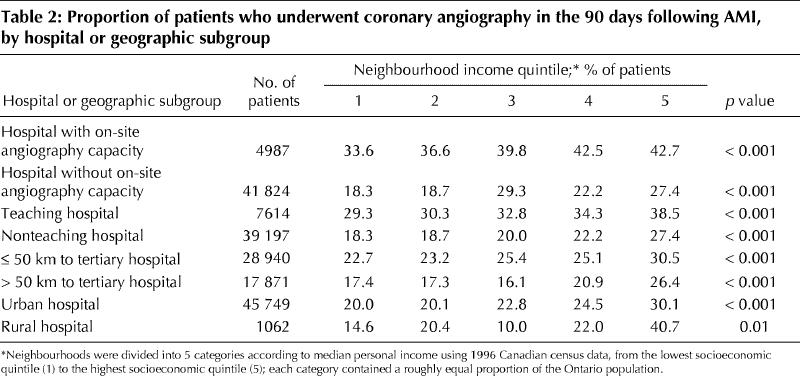
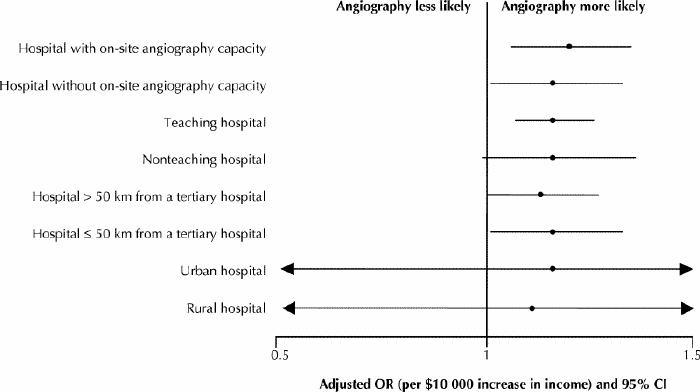
Fig. 1: The relation between neighbourhood income and angiography use within 90 days of acute myocardial infarction in hospitals and regions with different degrees of access to specialized cardiac services. The relative effects of socioeconomic status on angiography use post myocardial infarction are illustrated by the adjusted odds ratio (OR) and 95% confidence interval (CI) for each $10 000 increase in neighbourhood income (derived from 1996 census data), after adjusting for age, sex, cardiogenic shock, congestive heart failure, pulmonary edema, cardiac arrhythmias, diabetes with complications, stroke, malignant disease, acute renal failure, chronic renal failure and the attending physician's specialty. This figure shows, for example, that for 5 of the 8 hospital and geographic subgroups examined, people living in neighbourhoods with a median income of $10 000 more than that of adjacent neighbourhoods were 16% more likely than their poorer neighbours to receive angiography, after adjusting for baseline factors. (This percentage reflects the point estimates for these 5 odds ratios.) The 95% confidence intervals for urban and rural factors are truncated. Tertiary hospitals are defined as those institutions with on-site angiography and revascularization capacity.
Interpretation
We found no significant interaction among socioeconomic status, hospital and regional factors, and coronary angiography use after AMI. Instead, the effect of socioeconomic status was as important in tertiary hospitals as it was in community institutions, even after adjusting for variations in baseline patient-level and physician-level factors. Our findings therefore refute at least one widely held hypothesis: that socioeconomically related treatment inequalities can be attributed to variations in the supply and distribution of resources.17
Why do socioeconomic disparities in the post-MI use of angiography persist in a universal health care system? Like others,18 we have demonstrated an inverse relation between case-mix severity and angiography use after AMI. Given that less affluent patients are often sicker and have a higher incidence of coexisting conditions,19 variations in clinical severity and comorbidities may alter physicians' perceptions of the risk–benefit trade-offs associated with cardiac interventions post-MI.20 This hypothesis is consistent with evidence demonstrating that physicians generally select lower-risk patients for coronary angiography post-MI.4
Other effects of socioeconomic status may be more direct. For example, physicians may vary their responses to patients at either end of the socioeconomic spectrum.1,21,22 Further, socioeconomic status may affect the degree to which patients themselves seek care.1 However, these are merely speculations.
This study does have some limitations. First, we used geographic rather than individual indicators of socioeconomic status. However, several studies have demonstrated that such indicators are useful measures of socioeconomic status.23,24,25 Moreover, neighbourhood income of the patient is a determinant of both treatment and mortality in Ontario.1,2 Second, administrative databases lack detailed clinical information such as infarct location, initial heart rate, blood pressure and post-MI left ventricular function. Although it is possible that the inclusion of such clinical variables has altered our results, it would only have done so if the incidence of such variables systematically differed across socioeconomic status, hospital subgroups, and urban and rural regions.
In conclusion, the relative effect of neighbourhood income on the likelihood of receiving coronary angiography was similar in hospitals with and without on-site procedural capacity, and in regions with and without easy access to specialized cardiac services. These findings suggest that such disparities are unlikely to be remedied by an increase in the overall availability of angiography or by a redistribution of angiography resources to less affluent neighbourhoods. Future research should examine the extent to which intrinsic patient case-mix factors and physician or patient attitudes explain the socioeconomically related disparities in treatment after AMI.
Footnotes
This article has been peer reviewed.
Contributors: Dr. Alter was responsible for study conception, design and intellectual content; analysis and interpretation of data; and drafting and revising the manuscript. Dr. Naylor was responsible for study conception, design, intellectual content and article revision. Dr. Austin contributed to study conception, design and intellectual content; and acquisition, analysis and interpretation of data; and revisions of the manuscript. Dr. Chan contributed to intellectual content, acquisition of data and article revision. Dr. Tu was responsible for intellectual content, acquisition of data and article revision. All authors approved the final version.
Acknowledgements: We wish to thank Dr. Don Redelmeier for comments on an earlier draft of this article.
This project was supported by an operating grant from the Canadian Institutes of Health Research (CIHR). The Institute for Clinical Evaluative Sciences is supported in part by a grant from the Ontario Ministry of Health and Long-Term Care. The results, conclusions and opinions are those of the authors, and no endorsement by the Ministry, the Institute or the CIHR is intended or should be inferred. Dr. Tu is supported by a Canada Research Chair in Health Services Research. Dr. Alter is a New Investigator at the CIHR.
Competing interests: None declared.
Correspondence to: Dr. David A. Alter, Institute for Clinical Evaluative Sciences, Rm. G106, 2075 Bayview Ave., Toronto ON M4N 3M5; fax 416 480-6048; david.alter@ices.on.ca
References
- 1.Alter DA, Basinski AS, Naylor CD. A survey of provider experiences and perceptions of preferential access to cardiovascular care in Ontario, Canada. Ann Intern Med 1998;129:567-72. [DOI] [PubMed]
- 2.Alter DA, Naylor CD, Austin P, Tu JV. Effects of socioeconomic status on access to invasive cardiac procedures and on mortality after acute myocardial infarction. N Engl J Med 1999;341:1359-67. [DOI] [PubMed]
- 3.Alter DA, Austin P, Tu JV. Use of coronary angiography, angioplasty, and bypass surgery after acute myocardial infarction in Ontario. In: Naylor CD, Slaughter PM, editors. Cardiovascular health and services in Ontario: an ICES atlas. Toronto: Institute for Clinical Evaluative Sciences; 1999. p. 141-64.
- 4.Alter DA, Naylor CD, Austin PC, Tu JV. Long-term MI outcomes at hospitals with or without on-site revascularization. JAMA 2001;285:2101-8. [DOI] [PubMed]
- 5.Tu JV, Austin PC, Chan BT. Relationship between annual volume of patients treated by admitting physician and mortality after acute myocardial infarction. JAMA 2001;285:3116-22. [DOI] [PubMed]
- 6.Blustein J. High-technology cardiac procedures. The impact of service availability on service use in New York State. JAMA 1993;270:344-9. [DOI] [PubMed]
- 7.Di Salvo TT, Paul SD, Lloyd-Jones D, Smith AJ, Villarreal-Levy G, Bamezai V, et al. Care of acute myocardial infarction by noninvasive and invasive cardiologists: procedure use, cost and outcome. J Am Coll Cardiol 1996;27:262-9. [DOI] [PubMed]
- 8.Every NR, Fihn SD, Maynard C, Martin JS, Weaver WD. Resource utilization in treatment of acute myocardial infarction: staff-model health maintenance organization versus fee-for-service hospitals. The MITI Investigators. Myocardial infarction triage and intervention. J Am Coll Cardiol 1995;26:401-6. [DOI] [PubMed]
- 9.Badgley RF, Wolfe S. Equity and health care. In: Naylor CD, editor. Canadian health care and the state: a century of evolution. Montreal: McGill-Queen's University Press; 1992. p. 193-237.
- 10.Enterline PE, Salter V, McDonald AD, McDonald JC. The distribution of medical services before and after “free” medical care — the Quebec experience. N Engl J Med 1973;289:1174-8. [DOI] [PubMed]
- 11.Bondy SJ, Jaglal SB, Slaughter PM. Area variation in heart disease mortality rates. In: Naylor CD, Slaughter PM, editors. Cardiovascular health and services in Ontario: an ICES atlas. Toronto: Institute for Clinical Evaluative Sciences; 1999. p. 51-62.
- 12.Jaglal SB, Bondy SJ, Slaughter PM. Risk factors for cardiovascular disease. In: Naylor CD, Slaughter PM, editors. Cardiovascular health and services in Ontario: an ICES atlas. Toronto: Institute for Clinical Evaluative Sciences; 1999. p. 63-82.
- 13.Tu JV, Naylor CD, Austin P. Temporal changes in the outcomes of acute myocardial infarction in Ontario, 1992–1996. CMAJ 1999;161(10):1257-61. [PMC free article] [PubMed]
- 14.Tu JV, Austin P, Naylor CD, Iron K, Zhang H. Acute myocardial infarction outcomes in Ontario. In: Naylor CD, Slaughter PM, editors. Cardiovascular health and services in Ontario: an ICES atlas. Toronto: Institute for Clinical Evaluative Sciences; 1999. p. 83-110.
- 15.Anderson GM, Grumbach K, Luft HS, Roos LL, Mustard C, Brook R. Use of coronary artery bypass surgery in the United States and Canada. Influence of age and income. JAMA 1993;269:1661-6. [PubMed]
- 16.Tu JV, Austin P, Walld R, Roos LL, Aguglia F, McDonough P. Development and validation of the Ontario acute myocardial infarction mortality prediction rules. J Am Coll Cardiol 2001;37:992-7. [DOI] [PubMed]
- 17.Williams RB, Barefoot JC, Califf RM, Haney TL, Saunders WB, Pryor DB, et al. Prognostic importance of social and economic resources among medically treated patients with angiographically documented coronary artery disease. JAMA 1992;267:520-4. [PubMed]
- 18.Yusuf S, Flather M, Pogue J, Hunt D, Varigos J, Piegas L, et al. Variations between countries in invasive cardiac procedures and outcomes in patients with suspected unstable angina or myocardial infarction without initial ST elevation. OASIS (Organisation to Assess Strategies for Ischaemic Syndromes) Registry Investigators. Lancet 1998;352:507-14. [DOI] [PubMed]
- 19.Evans RG. Introduction. In: Evans RG, Barer ML, Marmor TR, editors. Why are some people healthy and others not? The determinants of health of populations. New York: Aldine de Gruyter; 1994. p. 3-26.
- 20.Guadagnoli E, Landrum MB, Normand SL, Ayanian JZ, Garg P, Hauptman PJ, et al. Impact of underuse, overuse, and discretionary use on geographic variation in the use of coronary angiography after acute myocardial infarction. Med Care 2001;39:446-58. [DOI] [PubMed]
- 21.Ayanian JZ, Udvarhelyi IS, Gatsonis CA, Pashos CL, Epstein AM. Racial differences in the use of revascularization procedures after coronary angiography. JAMA 1993;269:2642-6. [PubMed]
- 22.Ayanian JZ, Landrum MB, Normand SL, Guadagnoli E, McNeil BJ. Rating the appropriateness of coronary angiography — do practicing physicians agree with an expert panel and with each other? N Engl J Med 1998;338:1896-904. [DOI] [PubMed]
- 23.Smith GD, Hart C, Watt G, Hole D, Hawthorne V. Individual social class, area-based deprivation, cardiovascular disease risk factors, and mortality: the Renfrew and Paisley Study. J Epidemiol Community Health 1998;52:399-405. [DOI] [PMC free article] [PubMed]
- 24.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health 1992;82:703-10. [DOI] [PMC free article] [PubMed]
- 25.Carr-Hill R, Rice N. Is enumeration district level an improvement on ward level analysis in studies of deprivation and health? J Epidemiol Community Health 1995;49:S28-9. [DOI] [PMC free article] [PubMed]