Abstract
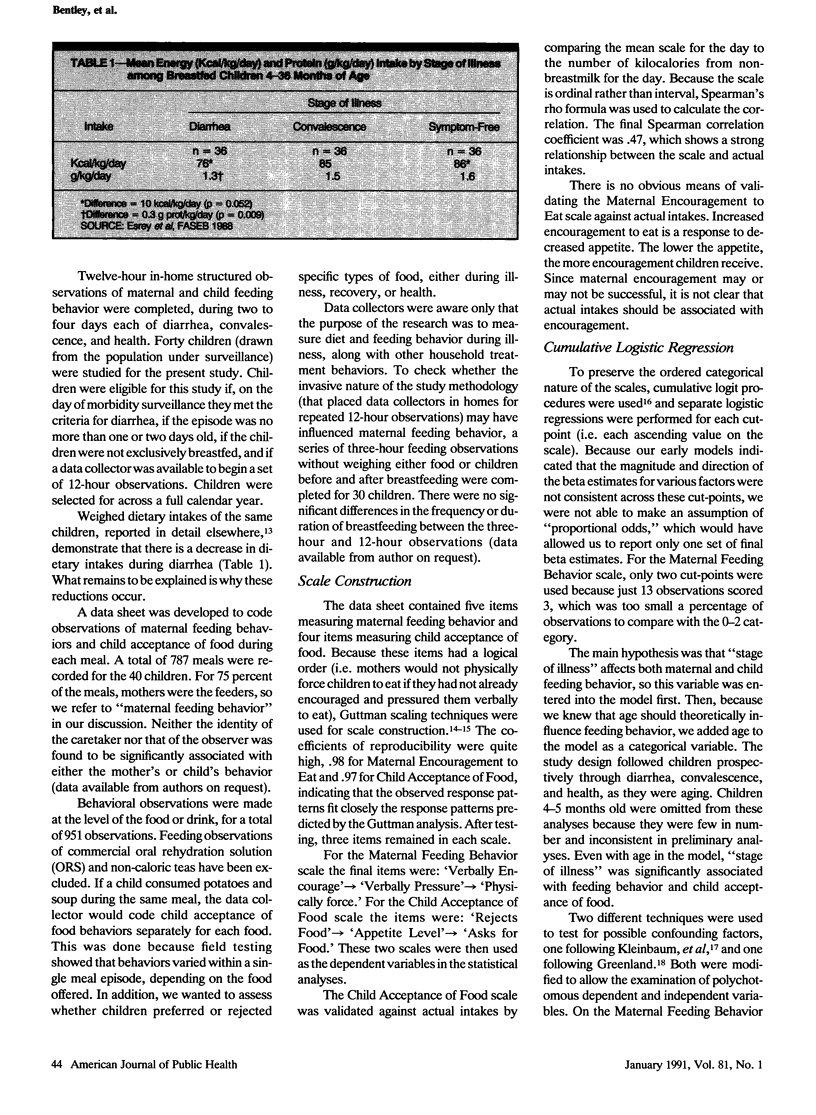
Feeding patterns by mothers and child acceptance of food were measured in a Peruvian village to determine changes on days when children had diarrhea as compared to days of convalescence and health. Morbidity surveillance identified 40 children, aged 4-36 months, with diarrhea. Children were followed using twelve-hour in-home structured observations during two to four days each of diarrhea, convalescence, and health. Using scales of maternal encouragement to eat and child acceptance of food and cumulative logistic regression analyses, maternal encouragement to eat decreased significantly during convalescence compared to diarrheal days (OR: 0.54, 90% CI: 0.35, 0.82) and health compared to diarrhea (OR: 0.65, 90% CI: 0.46, 0.93). In contrast, child acceptance of food increased during health compared to diarrhea (OR: 1.55, 90% CI: 1.02, 2.35). Results illustrate the importance of carefully examining the behavioral aspects of nutritional intake. Decreases in intake during diarrhea are due to anorexia and not withdrawal of food by mothers. In response to reductions in child appetite during illness, mothers are more likely to encourage children to eat, while they tend to become more passive feeders after the diarrhea has stopped. Program efforts should focus on messages to feed children more actively especially after diarrhea episodes, when appetite levels increase.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bentley M. E., Pelto G. H., Straus W. L., Schumann D. A., Adegbola C., de la Pena E., Oni G. A., Brown K. H., Huffman S. L. Rapid ethnographic assessment: applications in a diarrhea management program. Soc Sci Med. 1988;27(1):107–116. doi: 10.1016/0277-9536(88)90168-2. [DOI] [PubMed] [Google Scholar]
- Bentley M. E. The household management of childhood diarrhea in rural north India. Soc Sci Med. 1988;27(1):75–85. doi: 10.1016/0277-9536(88)90165-7. [DOI] [PubMed] [Google Scholar]
- Bentley M. E. The household management of childhood diarrhea in rural north India. Soc Sci Med. 1988;27(1):75–85. doi: 10.1016/0277-9536(88)90165-7. [DOI] [PubMed] [Google Scholar]
- Black R. E., Brown K. H., Becker S. Malnutrition is a determining factor in diarrheal duration, but not incidence, among young children in a longitudinal study in rural Bangladesh. Am J Clin Nutr. 1984 Jan;39(1):87–94. doi: 10.1093/ajcn/39.1.87. [DOI] [PubMed] [Google Scholar]
- Greenland S. Modeling and variable selection in epidemiologic analysis. Am J Public Health. 1989 Mar;79(3):340–349. doi: 10.2105/ajph.79.3.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyle B., Yunus M., Chen L. C. Breast-feeding and food intake among children with acute diarrheal disease. Am J Clin Nutr. 1980 Nov;33(11):2365–2371. doi: 10.1093/ajcn/33.11.2365. [DOI] [PubMed] [Google Scholar]
- Khan M. U., Ahmad K. Withdrawal of food during diarrhoea: major mechanism of malnutrition following diarrhoea in Bangladesh children. J Trop Pediatr. 1986 Apr;32(2):57–61. doi: 10.1093/tropej/32.2.57. [DOI] [PubMed] [Google Scholar]
- Kumar V., Clements C., Marwah K., Diwedi P. Beliefs and therapeutic preferences of mothers in management of acute diarrhoeal disease in children. J Trop Pediatr. 1985 Apr;31(2):109–112. doi: 10.1093/tropej/31.2.109. [DOI] [PubMed] [Google Scholar]
- Lopez de Romaña G., Brown K. H., Black R. E., Kanashiro H. C. Longitudinal studies of infectious diseases and physical growth of infants in Huascar, an underprivileged peri-urban community in Lima, Peru. Am J Epidemiol. 1989 Apr;129(4):769–784. doi: 10.1093/oxfordjournals.aje.a115192. [DOI] [PubMed] [Google Scholar]
- Martorell R., Habicht J. P., Yarbrough C., Lechtig A., Klein R. E., Western K. A. Acute morbidity and physical growth in rural Guatemalan children. Am J Dis Child. 1975 Nov;129(11):1296–1301. doi: 10.1001/archpedi.1975.02120480022007. [DOI] [PubMed] [Google Scholar]
- Zeger S. L., Liang K. Y., Albert P. S. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988 Dec;44(4):1049–1060. [PubMed] [Google Scholar]


