Abstract
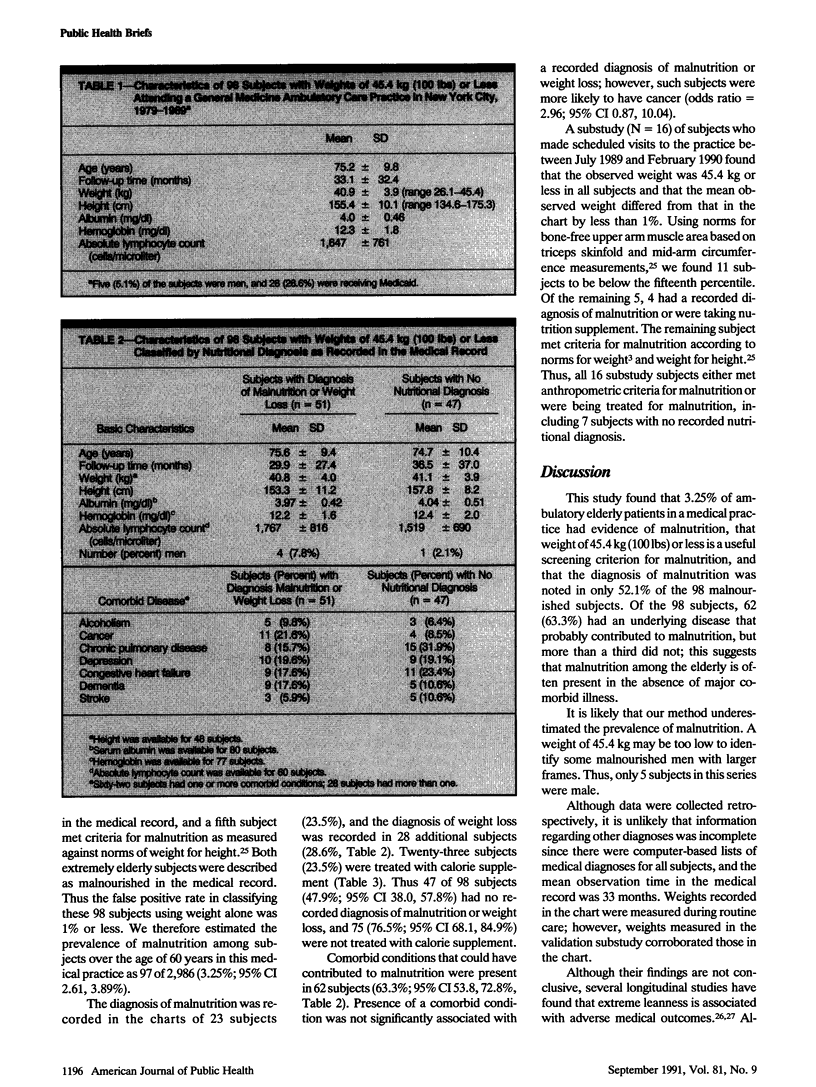
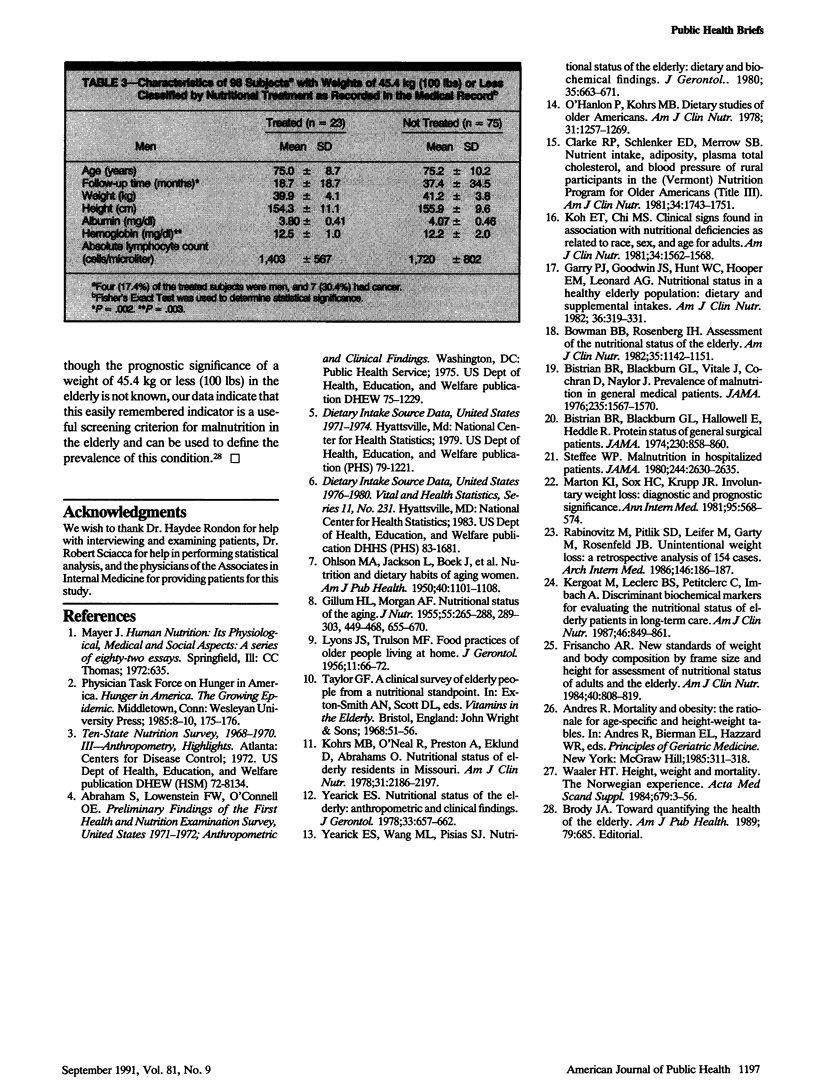
Elderly ambulatory persons may be especially susceptible to malnutrition, particularly those who are poor and socially isolated or have comorbid chronic medical diseases. We found that 98 of 2,986 persons aged 60 years or older attending a hospital-based medical practice between 1979 and 1989 weighed less than 45.4 kg (100 lbs). All but 1 of these subjects met criteria for malnutrition as judged against age-specific norms for weight. Thus the prevalence of malnutrition in this sample was 3.25% (95% CI 2.61, 3.89%). Interviews and physical examinations of a subsample (n = 16) revealed that all 16 subjects either met anthropometric-based criteria for malnutrition or were being treated for malnutrition. Of the 98 subjects who weighed less than 45.4 kg, 62 (63.3%; 95% CI 53.8, 72.8%) had comorbid conditions that could have contributed to malnutrition. Physicians did not record a diagnosis of malnutrition or weight loss in 47.9% of subjects (95% CI 38.0, 57.8%) and did not prescribe a nutrition supplement for 76.5% of subjects (95% CI 68.1, 84.9%). Subjects treated with nutrition supplement were more likely to have cancer. These findings suggest that malnutrition, both with and without concomitant major comorbid disease, is relatively frequent among elderly ambulatory patients and that a specific nutritional diagnosis is not made in many cases. We suggest that weight under 45.4 kg in an elderly person is a useful criterion for identifying elderly patients at nutritional risk.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bistrian B. R., Blackburn G. L., Hallowell E., Heddle R. Protein status of general surgical patients. JAMA. 1974 Nov 11;230(6):858–860. [PubMed] [Google Scholar]
- Bistrian B. R., Blackburn G. L., Vitale J., Cochran D., Naylor J. Prevalence of malnutrition in general medical patients. JAMA. 1976 Apr 12;235(15):1567–1570. [PubMed] [Google Scholar]
- Bowman B. B., Rosenberg I. H. Assessment of the nutritional status of the elderly. Am J Clin Nutr. 1982 May;35(5 Suppl):1142–1151. doi: 10.1093/ajcn/35.5.1142. [DOI] [PubMed] [Google Scholar]
- Brody J. A. Toward quantifying the health of the elderly. Am J Public Health. 1989 Jun;79(6):685–686. doi: 10.2105/ajph.79.6.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke R. P., Schlenker E. D., Merrow S. B. Nutrient intake, adiposity, plasma total cholesterol, and blood pressure of rural participants in the (Vermont) Nutrition Program for Older Americans (Title III). Am J Clin Nutr. 1981 Sep;34(9):1743–1751. doi: 10.1093/ajcn/34.9.1743. [DOI] [PubMed] [Google Scholar]
- Frisancho A. R. New standards of weight and body composition by frame size and height for assessment of nutritional status of adults and the elderly. Am J Clin Nutr. 1984 Oct;40(4):808–819. doi: 10.1093/ajcn/40.4.808. [DOI] [PubMed] [Google Scholar]
- GILLUM H. L., MORGAN A. F. Nutritional status of the aging. I. Hemoglobin levels, packed cell volumes and sedimentation rates of 577 normal men and women over 50 years of age. J Nutr. 1955 Feb 10;55(2):265–288. doi: 10.1093/jn/55.2.265. [DOI] [PubMed] [Google Scholar]
- Garry P. J., Goodwin J. S., Hunt W. C., Hooper E. M., Leonard A. G. Nutritional status in a healthy elderly population: dietary and supplemental intakes. Am J Clin Nutr. 1982 Aug;36(2):319–331. doi: 10.1093/ajcn/36.2.319. [DOI] [PubMed] [Google Scholar]
- Kergoat M. J., Leclerc B. S., PetitClerc C., Imbach A. Discriminant biochemical markers for evaluating the nutritional status of elderly patients in long-term care. Am J Clin Nutr. 1987 Nov;46(5):849–861. doi: 10.1093/ajcn/46.5.849. [DOI] [PubMed] [Google Scholar]
- Koh E. T., Chi M. S. Clinical signs found in association with nutritional deficiencies as related to race, sex, and age for adults. Am J Clin Nutr. 1981 Aug;34(8):1562–1568. doi: 10.1093/ajcn/34.8.1562. [DOI] [PubMed] [Google Scholar]
- Kohrs M. B., O'Neal R., Preston A., Eklund D., Abrahams O. Nutritional status of elderly residents in Missouri. Am J Clin Nutr. 1978 Dec;31(12):2186–2197. doi: 10.1093/ajcn/31.12.2186. [DOI] [PubMed] [Google Scholar]
- LYONS J. S., TRULSON M. F. Food practices of older people living at home. J Gerontol. 1956 Jan;11(1):66–72. doi: 10.1093/geronj/11.1.66. [DOI] [PubMed] [Google Scholar]
- Marton K. I., Sox H. C., Jr, Krupp J. R. Involuntary weight loss: diagnostic and prognostic significance. Ann Intern Med. 1981 Nov;95(5):568–574. doi: 10.7326/0003-4819-95-5-568. [DOI] [PubMed] [Google Scholar]
- O'Hanlon P., Kohrs M. B. Dietary studies of older Americans. Am J Clin Nutr. 1978 Jul;31(7):1257–1269. doi: 10.1093/ajcn/31.7.1257. [DOI] [PubMed] [Google Scholar]
- OHLSON M. A., JACKSON L., BOEK J., CEDERQUIST D. C., BREWER W. D., BROWN E. G., TRAVER J., LOTT M. M., MAYHEW M., DUNSING D. Nutrition and dietary habits of aging women. Am J Public Health Nations Health. 1950 Sep;40(9):1101–1108. doi: 10.2105/ajph.40.9.1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabinovitz M., Pitlik S. D., Leifer M., Garty M., Rosenfeld J. B. Unintentional weight loss. A retrospective analysis of 154 cases. Arch Intern Med. 1986 Jan;146(1):186–187. doi: 10.1001/archinte.146.1.186. [DOI] [PubMed] [Google Scholar]
- Steffee W. P. Malnutrition in hospitalized patients. JAMA. 1980 Dec 12;244(23):2630–2635. [PubMed] [Google Scholar]
- Waaler H. T. Height, weight and mortality. The Norwegian experience. Acta Med Scand Suppl. 1984;679:1–56. doi: 10.1111/j.0954-6820.1984.tb12901.x. [DOI] [PubMed] [Google Scholar]
- Yearick E. S. Nutritional status of the elderly: anthropometric and clinical findings. J Gerontol. 1978 Sep;33(5):657–662. doi: 10.1093/geronj/33.5.657. [DOI] [PubMed] [Google Scholar]


