Abstract
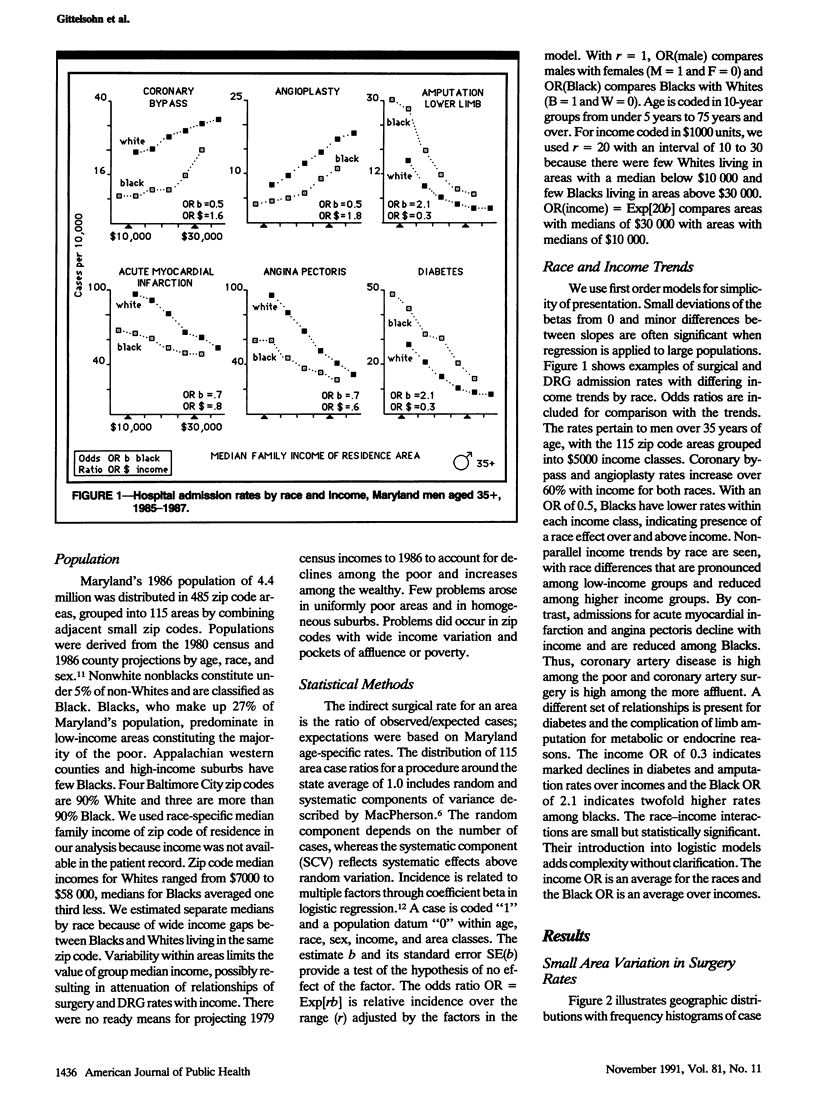
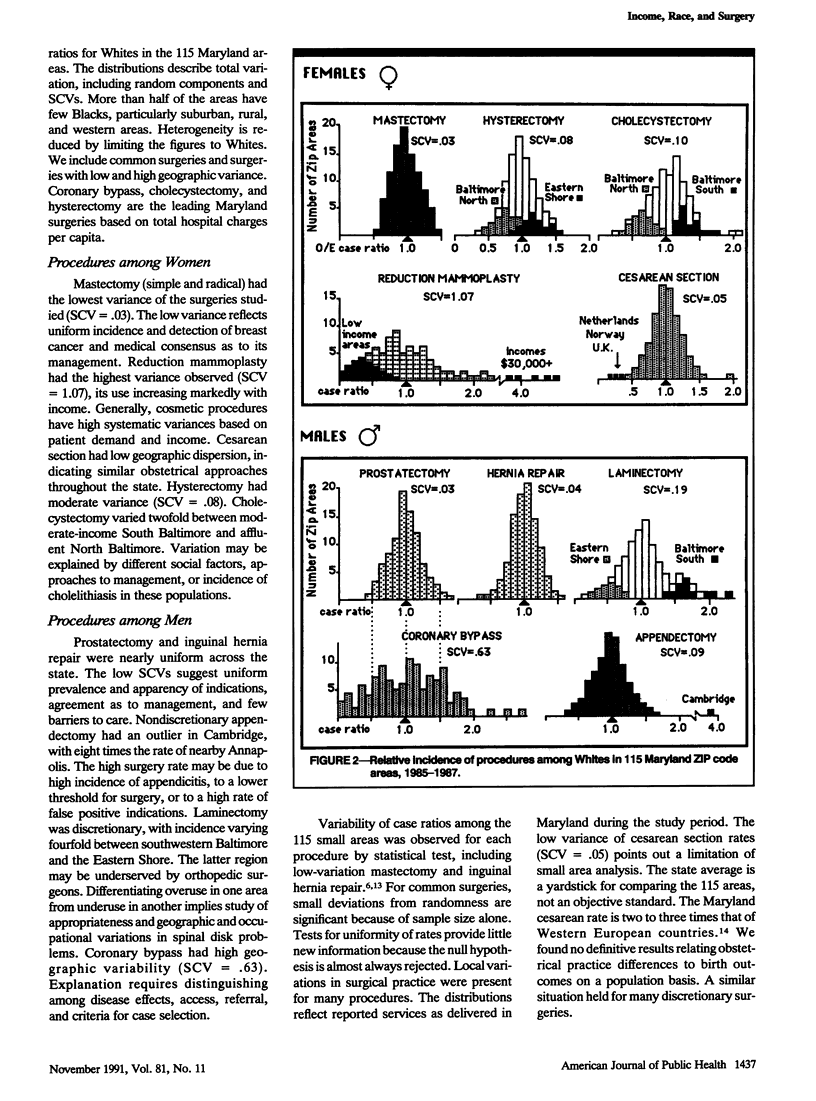
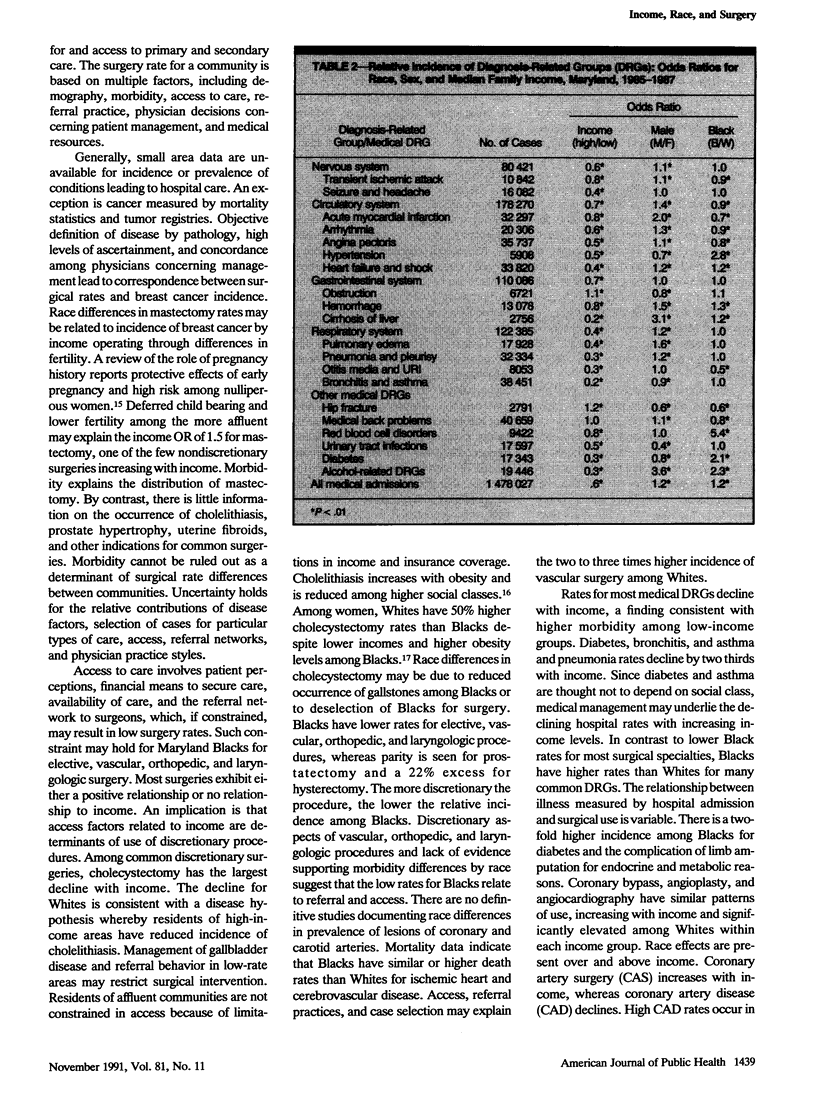
BACKGROUND. We describe common surgical and medical hospital admission rates for Maryland residents, exploring systematic effects of race and income. METHODS. The data comprise Maryland hospital discharges and population estimates for 1985 to 1987. Patient income is the race-specific median family income of residence zip code. Logistic regression is used to measure incidence by race, income, and residence for surgical and medical reasons for admission. RESULTS. Population rates for discretionary orthopedic, vascular, and laryngologic surgery tend to increase with community income levels. Coronary and carotid artery surgery rates are two to three times higher among Whites. The more discretionary the procedure, the lower is the relative incidence among Blacks. By contrast, admission rates for most medical reasons decline with increasing income levels and are elevated among Blacks. The affluent receive coronary artery procedures whereas the poor are hospitalized for coronary artery disease. CONCLUSIONS. Blacks and the poor appear to have higher illness burdens requiring hospital care. Discretionary surgeries have a White predominance and increase with income; medical admissions have a Black predominance and decline with income. Race and community income level are important factors in differential hospital utilization rates.
Full text
PDF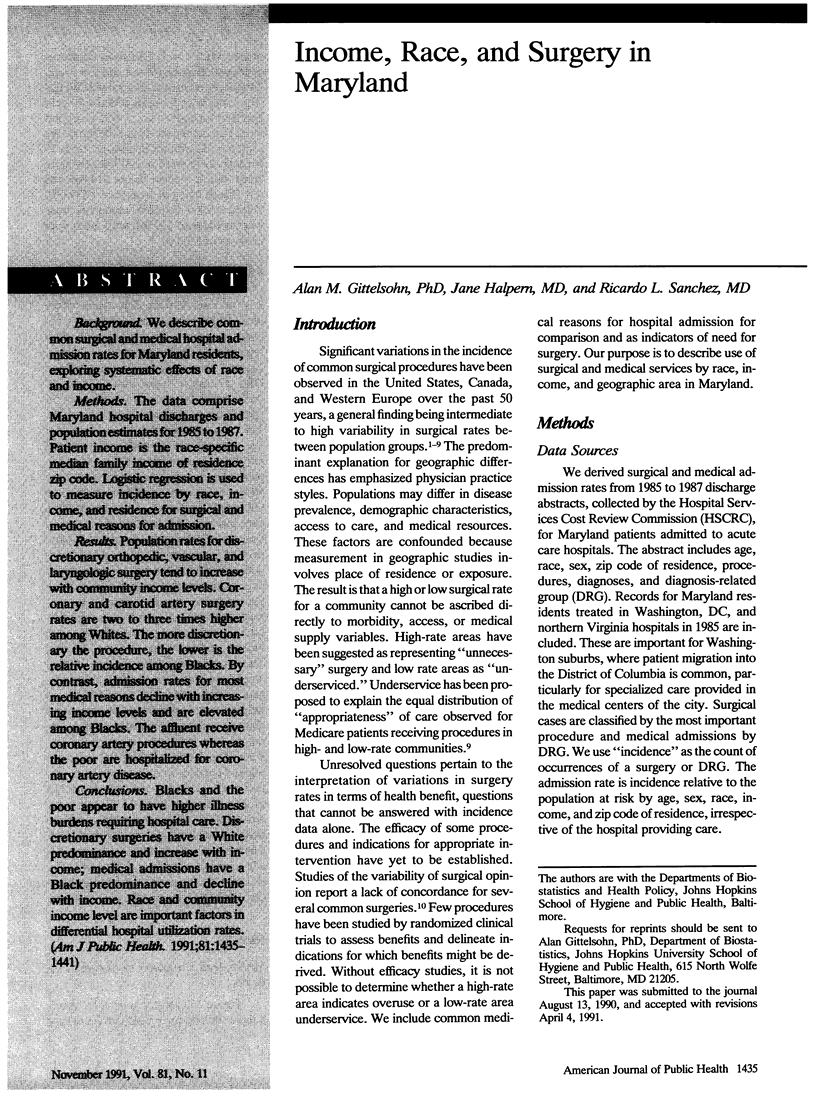

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barnes B. A., O'Brien E., Comstock C., D'Arpa D. G., Donahue C. L. Report on variation in rates of utilization of surgical services in the Commonwealth of Massachusetts. JAMA. 1985 Jul 19;254(3):371–375. [PubMed] [Google Scholar]
- Chassin M. R., Brook R. H., Park R. E., Keesey J., Fink A., Kosecoff J., Kahn K., Merrick N., Solomon D. H. Variations in the use of medical and surgical services by the Medicare population. N Engl J Med. 1986 Jan 30;314(5):285–290. doi: 10.1056/NEJM198601303140505. [DOI] [PubMed] [Google Scholar]
- Chassin M. R., Kosecoff J., Park R. E., Winslow C. M., Kahn K. L., Merrick N. J., Keesey J., Fink A., Solomon D. H., Brook R. H. Does inappropriate use explain geographic variations in the use of health care services? A study of three procedures. JAMA. 1987 Nov 13;258(18):2533–2537. [PubMed] [Google Scholar]
- Diehl A. K., Rosenthal M., Hazuda H. P., Comeaux P. J., Stern M. P. Socioeconomic status and the prevalence of clinical gallbladder disease. J Chronic Dis. 1985;38(12):1019–1026. doi: 10.1016/0021-9681(85)90100-6. [DOI] [PubMed] [Google Scholar]
- Hadley J., Steinberg E. P., Feder J. Comparison of uninsured and privately insured hospital patients. Condition on admission, resource use, and outcome. JAMA. 1991 Jan 16;265(3):374–379. [PubMed] [Google Scholar]
- Kumanyika S. Obesity in black women. Epidemiol Rev. 1987;9:31–50. doi: 10.1093/oxfordjournals.epirev.a036307. [DOI] [PubMed] [Google Scholar]
- LEMBCKE P. A. Medical auditing by scientific methods; illustrated by major female pelvic surgery. J Am Med Assoc. 1956 Oct 13;162(7):646–655. doi: 10.1001/jama.1956.72970240010009. [DOI] [PubMed] [Google Scholar]
- Lewis C. E. Variations in the incidence of surgery. N Engl J Med. 1969 Oct 16;281(16):880–884. doi: 10.1056/NEJM196910162811606. [DOI] [PubMed] [Google Scholar]
- MacMahon B., Cole P., Lin T. M., Lowe C. R., Mirra A. P., Ravnihar B., Salber E. J., Valaoras V. G., Yuasa S. Age at first birth and breast cancer risk. Bull World Health Organ. 1970;43(2):209–221. [PMC free article] [PubMed] [Google Scholar]
- McPherson K., Strong P. M., Epstein A., Jones L. Regional variations in the use of common surgical procedures: within and between England and Wales, Canada and the United States of America. Soc Sci Med A. 1981 May;15(3 Pt 1):273–288. doi: 10.1016/0271-7123(81)90011-0. [DOI] [PubMed] [Google Scholar]
- Rutkow I. M., Gittelsohn A. M., Zuidema G. D. Surgical decision making. The reliability of clinical judgment. Ann Surg. 1979 Sep;190(3):409–419. doi: 10.1097/00000658-197909000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wennberg J. E., Gittelsohn A. Health care delivery in Maine I: patterns of use of common surgical procedures. J Maine Med Assoc. 1975 May;66(5):123-30, 149. [PubMed] [Google Scholar]
- Wennberg J., Gittelsohn Small area variations in health care delivery. Science. 1973 Dec 14;182(4117):1102–1108. doi: 10.1126/science.182.4117.1102. [DOI] [PubMed] [Google Scholar]
- Wenneker M. B., Epstein A. M. Racial inequalities in the use of procedures for patients with ischemic heart disease in Massachusetts. JAMA. 1989 Jan 13;261(2):253–257. [PubMed] [Google Scholar]
- Wenneker M. B., Weissman J. S., Epstein A. M. The association of payer with utilization of cardiac procedures in Massachusetts. JAMA. 1990 Sep 12;264(10):1255–1260. [PubMed] [Google Scholar]


