Abstract
There is an urgent need for active immunization strategies that, if administered shortly after birth, could protect infants in developing countries from acquiring human immunodeficiency virus (HIV) infection through breast-feeding. Better knowledge of the immunogenic properties of vaccine candidates in infants and of the effect of maternal antibodies on vaccine efficacy will aid in the development of such a neonatal HIV vaccine. Simian immunodeficiency virus (SIV) infection of infant macaques is a useful animal model of pediatric HIV infection with which to address these questions. Groups of infant macaques were immunized at birth and 3 weeks of age with either modified vaccinia virus Ankara (MVA) expressing SIV Gag, Pol, and Env (MVA-SIVgpe) or live-attenuated SIVmac1A11. One MVA-SIVgpe-immunized group had maternally derived anti-SIV antibodies prior to immunization. Animals were challenged orally at 4 weeks of age with a genetically heterogeneous stock of virulent SIVmac251. Although all animals became infected, the immunized animals mounted better antiviral antibody responses, controlled virus levels more effectively, and had a longer disease-free survival than the unvaccinated infected monkeys. Maternal antibodies did not significantly reduce the efficacy of the MVA-SIVgpe vaccine. In conclusion, although the tested vaccines delayed the onset of AIDS, further studies are warranted to determine whether a vaccine that elicits stronger early immune responses at the time of virus exposure may be able to prevent viral infection or AIDS in infants.
The recent discovery of simplified zidovudine and nevirapine regimens to reduce peripartum human immunodeficiency virus type 1 (HIV-1) transmission is very promising (9, 16, 38, 50). However, the need for breast-feeding in developing countries continues to be a considerable risk for postnatal mother-to-child transmission of HIV, since breast-feeding is estimated to account for 33 to 50% of new infant HIV infections worldwide (2, 11, 20, 21, 31, 41). The efficacy and safety of prolonged administration of zidovudine or nevirapine to nursing infants to reduce infection through breast-feeding has not been determined. In addition, the high cost and complexity of such drug regimens would preclude their implementation in most of the developing world. These problems underscore the need for a vaccine that, when administered to the infant shortly after birth, could protect against HIV transmission via breast-feeding. However, there are several challenges to develop such a neonatal HIV vaccine. Although breast milk transmission of HIV can still occur at later stages, data suggest that most transmission occurs during the first 6 months of age (10, 27, 31). This emphasizes the need for an anti-HIV vaccine that rapidly elicits protective immune responses. In addition, the presence of maternally derived anti-HIV antibodies may interfere with the efficacy of active immunization in infants.
Advances in the understanding of the mechanisms of oral HIV transmission, the ontogeny of infant immune responses, and the effect of maternal antibodies will aid the development of an effective infant HIV-1 vaccine. These questions, however, are difficult to address in human studies. In addition, the logistical and ethical constraints associated with conducting clinical trials of HIV vaccines in infants necessarily delay progress.
Simian immunodeficiency virus (SIV) infection of infant macaques is a highly relevant animal model of pediatric HIV infection with which to rapidly evaluate the efficacy of pediatric HIV vaccine and drug interventions (25, 34, 42-45, 48, 49). We used this model to evaluate the efficacy of two vaccines: (i) modified vaccinia virus Ankara (MVA) expressing SIV Gag, Pol, and Env (MVA-SIVgpe) and (ii) live-attenuated SIVmac1A11. The safety and immunogenicity of MVA vaccines in animals and humans is well documented (22), and the molecular clone SIVmac1A11 is immunogenic and nonpathogenic for rhesus macaques of all ages (23, 25, 40). We demonstrate that, although both vaccines were immunogenic for newborn macaques, they did not prevent infection after oral challenge with SIVmac251 at 4 weeks of age, but the immunized animals mounted better antiviral antibody responses, had lower levels of virus replication, and had better survival than unimmunized animals.
MATERIALS AND METHODS
Infant immunizations, virus inoculations, and sample collection.
All newborn rhesus macaques (Macaca mulatta) were from the HIV-2, SIV, type D retrovirus, and simian T-cell lymphotropic virus type 1-free colony at the California National Primate Research Center. Newborn monkeys were hand-reared in a primate nursery, and all animals were housed in accordance with American Association for Accreditation of Laboratory Animal Care standards. We adhered to the Guide for Care and Use of Laboratory Animals (30). When necessary, animals were immobilized with 10 mg of ketamine hydrochloride (Parke-Davis, Morris Plains, N.J.)/kg, injected intramuscularly (i.m.).
One of two SIV vaccines was administered to newborn monkeys: (i) modified vaccinia virus Ankara expressing SIVmac239 Gag, Pol, and Env (MVA-SIVgpe) was given to 10 newborn monkeys or (ii) SIVmac1A11 (given to four newborn monkeys). For construction of MVA-SIVgpe, chicken embryo fibroblast cells were incubated simultaneously with five infectious units each of MVA/SIV239gagpol (14) and MVA/SH4wt. The latter virus expresses the SIVmac239 env gene, truncated after amino acid 733, under the control of the moderate-strength vaccinia virus promoter p7.5. A virus isolate expressing all three genes was clonally purified and amplified. Stocks of virus used for immunizations were grown in chicken embryo fibroblasts and shown to express Env and Gag proteins (not shown). Within 3 days of age, 10 newborn monkeys were vaccinated i.m. with 108 PFU of MVA-SIVgpe (250 μl in each of four limbs from a stock of 108 PFU/ml) and intranasally with 108 PFU of MVA-SIVgpe (100 μl per nostril from a stock of 5 × 108 PFU/ml); an identical booster immunization was given 3 weeks later. The SIVmac1A11 virus stock was grown on stimulated CD4-enriched rhesus macaque peripheral blood mononuclear cells (PBMC) and had a titer of 105 50% tissue culture infectious doses (TCID50)/ml. SIVmac1A11 was administered intravenously (0.5 ml), intranasally (50 μl per nostril), and orally (0.9 ml) to four newborn monkeys within 3 days of birth and again 3 weeks later.
To monitor the development of infant immune responses to nonviral, nonreplicating antigens, all newborns were immunized subcutaneously with 0.1 mg of cholera toxin B subunit (List Biological Laboratories, Campbell, Calif.) at 2 and 10 weeks of age and i.m. with 0.5 ml of tetanus toxoid in alum (Lederle Laboratories, Pearl River, N.Y.) at 6 and 14 weeks of age.
At 4 weeks of age, 17 newborn monkeys were inoculated orally with two doses (24 h apart) of virulent SIVmac251. Each dose consisted of 1 ml of undiluted SIVmac251 (stock no. -5/98) and was administered atraumatically by dispensing virus slowly into the mouth with a syringe. The SIVmac251-5/98 virus stock used in the present study was derived from a previous stock SIVmac251-8/95 that was serially passaged intravenously in rhesus macaques as described previously (15); virus isolated from plasma of animal 26108 2 weeks after infection was briefly expanded in rhesus PBMC. This SIVmac251-5/98 stock contained 105 TCID50 (determined by limiting dilution culture assay in 24-well plates [42]) and 1.4 × 109 copies of RNA per ml (as determined by branched DNA [bDNA] assay). SIVmac251-5/98 has been demonstrated to be pathogenic in adult rhesus macaques (24).
EDTA-anticoagulated blood samples were collected regularly for monitoring virologic and immunologic parameters. Complete blood cell counts were measured by using an automated electronic cell counter (Baker 9000; Serono Baker Diagnostics); differential counts were determined manually.
Immunization of pregnant rhesus macques.
Four adult female rhesus macaques were immunized and boosted during three or four consecutive pregnancies with whole-inactivated SIVmac251 plus Montanide ISA 51 adjuvant (Seppic, Fairfield, N.J.), administered i.m. as previously described (49). During each pregnancy the first immunization was administered between gestational days 137 to 139, whereas the booster immunization was given between gestational days 150 to 152. Infant macaques born to these females comprised group 4 (see below), the MVA-SIVgpe-vaccinated newborns with maternally derived anti-SIV antibodies.
Quantitative cell-associated virus isolation.
Levels of infectious virus in PBMC were determined regularly by a limiting dilution assay (four replicates per dilution) of PBMC in cultures of CEMx174 cells in 24-well plates and subsequent p27 core antigen measurement, according to methods previously described (42).
Quantitation of viral RNA in plasma.
Viral RNA in plasma was quantified by using a bDNA signal amplification assay specific for SIV (P. J. Dailey, M. Zamroud, R. Kelso, J. Kolberg, and M. Urdea, Abstr. 13th Annu. Symp. Nonhum. Primate Models of AIDS, Monterey, Calif., abstr. 99, 1995). This assay is similar to the Quantiplex HIV RNA assay except that target probes were designed to hybridize with the pol region of the SIVmac group of strains, including SIVmac251 and SIVmac239. SIV pol RNA in plasma samples was quantified by comparison with a standard curve produced with serial dilutions of cell-free SIV-infected tissue culture supernatant. The quantitation of this standard curve was done in comparison with purified, quantified, in vitro-transcribed SIVmac239 pol RNA. The lower quantitation limit of this assay was 1,500 copies of SIV RNA per ml of plasma. Due to the limited blood volume that can be collected from newborn macaques, plasma volumes of ≤50 μl were available during the early time points, which limited the sensitivity of this assay to ≥30,000 copies of SIV RNA per ml of plasma.
Detection of IgG antibodies to SIV, cholera toxin, and tetanus toxoid.
The enzyme-linked immunosorbent assays (ELISAs) to detect SIV-specific immunoglobulin G (IgG), cholera toxin-specific IgG, and tetanus toxoid-specific IgG have been described previously (33, 47, 49).
Measurement of SIV envelope-specific antibody endpoint titer, avidity, and conformational dependence in a ConA ELISA.
Antibody reactivity to detergent-disrupted SIVsmB7 envelope proteins (19) were determined in a conconavalin A (ConA) ELISA as previously described (8). Briefly, SIVsmB7 viral envelope proteins (gp120 and gp41) were captured onto Immulon 2HB microtiter plates (Dynex Corp.) by using 5 μg of ConA/well for 1 h at room temperature. After a washing step with phosphate-buffered saline (PBS), all wells were blocked by the addition of 5% dry milk in PBS (blocking solution) for 1 h at room temperature. Heat-inactivated plasma samples were serially diluted in blocking solution and incubated in the SIVsmB7 envelope-coated wells for 1 h at room temperature. After an extensive washing, peroxidase-conjugated anti-monkey IgG (Nordic Immunology Laboratories) was diluted in blocking solution, added to each well, and incubated for 1 h at room temperature. After a final washing step, all wells were incubated with TM Blue substrate (Intergen, Inc., Milford, Mass.) for 20 min at room temperature, color was developed by the addition of 1N sulfuric acid, and the wells were read at an optical density of 450 nm (OD450) by using an automated ELISA plate reader (Dynex Corp.). Antibody endpoint titers were calculated to be the last serial twofold dilution whose OD was twice that of normal monkey plasma. The avidity of plasma antibodies to native viral envelope proteins was determined by measuring the resistance of plasma antibody-envelope glycoprotein complexes to 8 M urea in a ConA ELISA as previously described (8). The avidity index values were obtained from the following calculation: (OD450 of PBS-washed wells/OD450 of urea-washed wells) × 100%. The conformational dependence of plasma antibodies was determined by comparing reactivities to native and denatured viral envelope glycoproteins in a ConA ELISA as previously described (8). The conformation ratio is a direct measure of the conformational dependence of a particular antibody sample, where conformation ratios of >1 reflect a predominant reactivity with native envelope glycoproteins and conformation ratios of <1 reflect a predominant antibody reactivity with denatured envelope glycoproteins.
Measurement of SIVmac251 PR55 Gag-specific antibody responses.
SIVmac251 PR55 Gag protein (kindly provided by the National Institutes of Health [NIH] AIDS Research and Reference Reagent Program) was diluted in 0.05 M bicarbonate buffer (pH 9.6) and allowed to adhere directly to Immulon 1B microtiter plates (Dynex Corp.) by an overnight incubation at room temperature. The ELISA was completed, and the endpoint titers were determined as described above for the ConA ELISA.
ELISPOT assay for SIV-specific IFN-γ-secreting cells.
To estimate the number of antigen-specific gamma interferon (IFN-γ)-producing cells in rhesus monkeys, an enzyme-linked immunospot (ELISPOT) assay was developed. According to manufacturer's instructions, anti-IFN-γ antibody was used to coat flat-bottom 96-well ELISPOT plates (U-Cytech, Amsterdam, The Netherlands) at 4°C overnight and then washed ca. 10 times with 0.05% Tween 20 in PBS (PBST) before 200 μl of 1% bovine serum albumin in PBS was added to each well for 1 h at 37°C to block nonspecific binding. Cryopreserved PBMC were thawed and washed, resuspended in AIM-V media (Gibco-BRL) with 10% fetal bovine serum. After an overnight rest, viable cells were counted, transferred in 96-well flat-bottom tissue culture plates to a final concentration of 2 million cells per ml, and stimulated with a pool of 20-mer peptides with a 10-amino-acid overlap of the entire p24 Gag region of SIVmac239 (provided by the NIH AIDS Research and Reference Reagent Program [www.aidsreagent.org]). Peptides were added to the cultures at a final concentration of 1 μg/ml. After incubation of 18 h in humidified atmosphere at 37°C with 5% CO2, 100 μl (2 × 105 cells) was transferred to the anti-IFN-γ antibody-coated ELISPOT plate and then incubated for another 5 h. The wells were then decanted and treated with 200 μl of ice-cold deionized water and washed 10 times with PBST. The ELISPOT plate was further incubated with biotinylated detector antibody, as well as φ-labeled anti-biotin antibody solution (GABA) as recommended by the manufacturer. After incubation, the plates were washed 10 times with PBST and finally developed with activator solution (U-Cytech) at room temperature. The reaction was stopped by rinsing the wells with distilled water. Negative control wells consisted of PBMC in AIM-V medium (withouth peptides); positive control wells consisted of PBMC stimulated with phorbol myristate acetate (50 ng/ml) and ionomycin (1 μg/ml). The spots were counted by using the KS ELISPOT system with version 4.3 software (Zeiss, Hallbergmoos, Germany). Results were considered positive if the number of spot-forming cells (SFC) for 2 × 105 cells was >10 per well and greater than the average of the negative control (medium only) wells plus two standard deviations. The results are presented as SFC per million cells. This assay was validated and quality controlled by using cryopreserved PBMC from juvenile and adult macaques: six healthy SIV-negative animals (mean, 13 SFC per million PBMC; range, 0 to 20 SFC) and four SIV-infected animals (mean, 249 SFC per million PBMC; range, 170 to 265 SFC). To ensure that the assay was performing as expected, PBMC samples from such SIV-positive and -negative rhesus monkeys were included in every assay.
Lymphocyte phenotyping by three-color flow cytometry.
T-lymphocyte antigens were detected by direct labeling of whole blood with peridinin chlorophyll protein (PerCP)-conjugated anti-human CD8 (clone SK1; Becton Dickinson Immunocytometry, Inc., San Jose, Calif.), phycoerythrin-conjugated anti-human CD4 (clone M-T477; Pharmingen), and fluorescein-conjugated anti-human CD3 (clone SP34; Pharmingen). A separate aliquot of blood was labeled with fluorescein-conjugated anti-human CD3 and PerCP-conjugated anti-human CD20 (clone L27; Becton Dickinson). Red blood cells were lysed, and the samples were fixed in paraformaldehyde by using the Coulter Q-Prep system (Coulter Corp., Hialeah, Fla.). Lymphocytes were gated by forward and side light scatter and were then analyzed with a FACSCalibur flow cytometer (Becton Dickinson). CD4+ T lymphocytes and CD8+ T lymphocytes were defined as CD3+ CD4+ and CD3+ CD8+ lymphocyte populations, respectively. B lymphocytes were defined as CD3− CD20+ lymphocytes.
Criteria for euthanasia and animal necropsies.
Euthanasia of animals with simian AIDS was indicated by three or more of the following clinical observations: weight loss of >10% in 2 weeks or of >30% in 2 months; chronic diarrhea unresponsive to treatment; infections unresponsive to treatment; inability to maintain body heat or fluids without supplementation; persistent, marked hematologic abnormalities, including lymphopenia, anemia, thrombocytopenia, or neutropenia; and persistent, marked splenomegaly or hepatomegaly (25). Animals which did not develop simian AIDS were euthanized at 28 weeks of age. A complete necropsy examination was performed on all animals, and a routine histopathologic examination was done on tissues collected at necropsy.
Statistical analysis.
Viral levels in plasma over time among groups were compared by a mixed model repeated measures analysis of variance and Dunnet's test with the SAS software package (version 8.0; SAS, Cary, N.C.). Growth rates of infants from 28 to 74 days of age were calculated by using linear regression analyses performed with Microsoft Excel (v. 5.0) software (Microsoft Corp., Redmond, Wash.). Statistical analysis of disease-free survival was done by using a log-rank test (Prism version 3.0 for Mac; GraphPad Software, Inc., San Diego, Calif.). For all statistical analyses, results were considered significant if the probability was <0.05 (i.e., P < 0.05).
RESULTS
Experimental design of animal experiments and summary of outcome.
Nineteen newborn rhesus macaques were divided into five experimental vaccine groups (Table 1). Group 1 (n = 5) consisted of nonimmunized control animals. One group 1 infant (animal 31608) was born to a pregnant female infected with SIVmac251, and therefore had maternal anti-SIV antibodies, but no virus was detected in this infant at 4 weeks of age. Animals in groups 2 to 5 were immunized at 0 and 3 weeks of age. Group 2 (n = 2), group 3 (n = 4), and group 4 (n = 4) animals were vaccinated with MVA-SIVgpe; group 4 (n = 4) animals had maternally derived SIV antibodies (due to immunization of their mothers with inactived SIV). Group 5 (n = 4) animals were immunized with live-attenuated SIVmac1A11 at 0 and 3 weeks. Except for group 2 (MVA-SIVgpe immunized, but unchallenged infants), all groups were inoculated orally with SIVmac251 at 4 weeks of age. All infants were immunized with cholera toxin subunit B (at 2 and 10 weeks of age) and tetanus toxoid (at 6 and 14 weeks of age) to determine immune responses to nonviral antigens. As described below, the animal groups were compared with regard to a number of parameters (survival, viremia, immune responses, etc.).
TABLE 1.
Experimental design and disease outcome
| Immunization groupa | Animal no. | Growth rateb | Time of euthanasia (wk)c | Histopathology and clinical pathology (level [g/dl]) |
|---|---|---|---|---|
| Group 1 (Unvaccinated + SIVmac251) | 31319 | 1.8 (0.9-2.6) | 13 | Thymus atrophy, lymphoid hyperplasia of bone marrow and spleen, colitis, hypoproteinemia (3.5) |
| 31321 | 2.1 (1.2-3.0) | 28 | Lymphoid hyperplasia, typhlocolitis, hepatitis, Pneumocystis carinii pneumonia, meningoencephalitis, hypoproteinemia (4.9) | |
| 31322 | 2.8 (2.2-3.4) | 14 | Lymphoid hyperplasia, colitis, dermatitis, hypoproteinemia (4.6) | |
| 31325 | 4.0 (3.4-4.7) | 12 | Lymphoid hyperplasia, thymus atrophy, hepatitis, necrotizing encephalitis, edema, hypoproteinemia (2.9) | |
| 31608d | 0.6 (0.0-1.2) | 11 | Mixed pattern of lymphoid hyperplasia and depletion, typhlocolitis | |
| Group 2 (MVA-SIVgpe only) | 31480 | 7.4 (6.9-7.9) | NAf | Healthy at 3 years |
| 31488 | 7.2 (6.8-7.7) | NA | Healthy at 3 years | |
| Group 3 (MVA-SIVgpe + SIVmac251) | 31378 | 6.5 (6.0-7.0) | 28e | Lymphoid hyperplasia, Cryptosporidium sp.-positive enteritis |
| 31533 | 5.2 (4.7-5.7) | 26 | Lymphoid hyperplasia, effacing Escherichia coli colitis, cytomegalovirus-positive hepatitis, nephritis, P. carinii pneumonia | |
| 31540 | 5.9 (4.4-7.5) | 28e | Lymphoid hyperplasia, mild enterocolitis | |
| 31542 | 7.8 (7.1-8.4) | 26 | Thymus atrophy, Cryptosporidium sp.- and E. coli-positive gastroenterocolitis, mild P. carinii pneumonia | |
| Group 4 (maternal antibodies + MVA-SIVgpe + SIVmac251) | 31526 | 2.5 (1.9-3.1) | 27 | Mixed pattern of lymphoid hyperplasia and depletion, thymus atrophy, Cryptosporidium sp.-positive enteritis, gastritis |
| 31732 | 4.7 (4.2-5.1) | 19 | Thymus atrophy, lymphoid depletion, necrotizing gastroenterocolitis, mild Candida albicans-positive esophagitis, hepatitis, hypoproteinemia (4.5) | |
| 31833 | 4.2 (3.5-4.8) | 28e | Lymphoid hyperplasia, splenomegaly, mild choledochocystitis and pancreatic ductitis, mild pneumonia | |
| 31856 | 6.3 (5.6-7.0) | 28e | Lymphoid hyperplasia, severe choledochocystitis, cholangiohepatitis, mild pneumonia | |
| Group 5 (SIVmac1A11 + SIVmac251) | 31777 | 4.5 (3.9-5.1) | 28e | Lymphoid hyperplasia, moderate colitis and splenomegaly |
| 31778 | 5.2 (4.7-5.8) | 28e | Lymphoid hyperplasia, mild Cryptosporidium sp.-positive enterocolitis, and pancreatic ductitis | |
| 31779 | 3.0 (2.2-3.8) | 28e | Lymphoid hyperplasia, mild to moderate Cryptosporidium sp.-positive pancreatic ductitis and bronchitis | |
| 31780 | 4.1 (3.6-4.6) | 28e | Lymphoid hyperplasia, mild Cryptosporidium sp.-positive pancreatic ductitis and enterocolitis, mild C. albicans-positive glossitis and esophagitis, mild pneumonia |
Vaccine was administered in two doses; at birth and 3 weeks later. Animals of groups 1, 3, 4, and 5 were challenged orally at 4 weeks of age with SIVmac251-5/98.
Average weight gain in grams/day (with 95% confidence interval in parentheses) between 28 and 74 days of age, as determined by regression analysis.
Age (weeks) at time of euthanasia.
Group 1 animal 31608 was born with maternally derived anti-SIV antibodies.
Animal was clinically stable at time of euthanasia; all other animals were euthanized due to life-threatening disease prior to or at 28 weeks of age.
NA, not applicable.
SIV infection and disease outcome in infants challenged orally with SIVmac251.
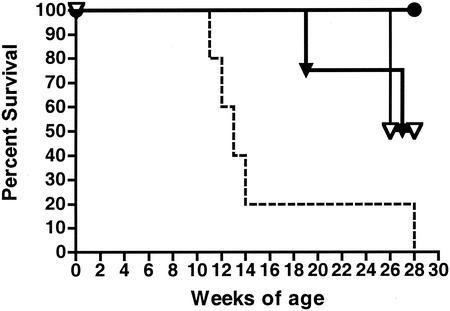
All 17 infants orally inoculated with SIVmac251 (Table 1, group 1 and groups 3 to 5) became infected 1 week after challenge as determined by virus isolation, bDNA analysis, and reverse transcription-PCR. All unvaccinated SIVmac251-infected animals (group 1) demonstrated a “failure to thrive” syndrome characterized by poor weight gain that was significantly lower than that of normal, uninfected nursery-reared rhesus infants (P < 0.05) (Table 1). Four of these five SIVmac251-infected control animals developed life-threatening immunodeficiency within 14 weeks of age, whereas the fifth animal needed euthanasia at 28 weeks of age (Table 1). Compared to group 1, the animals in the three immunized, SIVmac251-challenged groups (groups 3 to 5) had significantly longer disease-free survival (Fig. 1). Four MVA-SIVgpe-vaccinated animals developed AIDS by 19 weeks (animal 31732), 26 weeks (animals 31533 and 31542) or 27 weeks of age (animal 31526). The remaining eight vaccinated infants, including all four SIVmac1A11-vaccinated animals, were still clinically stable at the time of experimental necropsy (28 weeks of age). The two animals that were vaccinated with MVA-SIVgpe but not challenged with SIVmac251 (group 2) had normal weight gain and remained healthy throughout the observation period (>2 years).
FIG. 1.
Comparison of survival for vaccinated and unvaccinated infant rhesus macaques. The survival of unvaccinated (dashed line) and vaccinated (solid lines) animals by age (weeks) is shown. The comparison of survival curves was performed by using the log-rank test. The median survival time for unvaccinated animals was 13 weeks of age. The survival curves for unvaccinated animals were statistically different from animals vaccinated with SIVmac1A11 (P < 0.0049 [•]) and all eight animals vaccinated with MVA-SIVgpe (P < 0.0093 [triangles]). There was no statistically significant difference in the survival curves among the different groups of vaccinated animals (MVA-SIVgpe immunized, median survival = 27 weeks [▿]; MVA-SIVgpe plus maternal SIV antibodies, median survival = 27.5 weeks [▾]; SIVmac1A11-immunized, all animals healthy at 28 weeks).
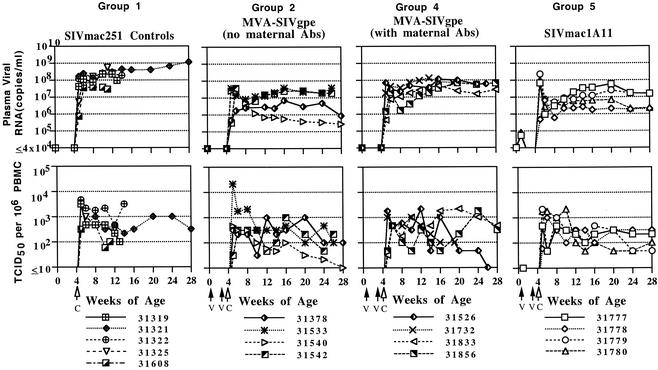
Comparison of viremia in SIVmac251-infected infant macaques.
There was a strong inverse correlation between SIV RNA levels in plasma and disease-free survival. After oral inoculation with SIVmac251 at 4 weeks of age (Table 1, groups 1 and 3 to 5), SIV RNA levels in plasma peaked 1 to 2 weeks later (Fig. 2). For the purpose of further discussions, viral RNA levels were classified as high (>108 RNA copies/ml), moderate (between 107 and 108 RNA copies/ml), or low (<107 RNA copies/ml). For the unimmunized control animals (Table 1, group 1), virus levels in plasma remained persistently high (four animals) or moderate (animal 31608) until the time of death (Fig. 2). In contrast, SIV RNA levels in the immunized infants were lower than in the controls. Although there was individual variation, SIV RNA levels in plasma for the group 3 animals (MVA-SIVgpe immunized) during initial peak viremia (1 to 3 weeks postchallenge) were ca. 10- to 100-fold lower than for the unvaccinated controls (group 1), and at 12 to 16 weeks of age, there were two animals with moderate viremia and two animals with low viremia. Viral RNA levels in group 4 (MVA-SIVgpe immunized with maternal antibodies) during the initial viremia and thereafter were ca. ≤10-fold lower than that observed in the unvaccinated controls, and at 12 to 16 weeks of age the animals had moderate viremia (n = 3) or moderate to high viremia (animal 31732; Fig. 3). For the group 5 animals (SIVmac1A11 immunized at 0 and 3 weeks of age), virus could be isolated from the PBMC of two of these infants (animals 31777 and 31780) at 1 and 2 weeks of age, and low levels of viral RNA (53,000 to 80,000 copies/ml) were detected in plasma of three of these infants (animals 31777, 31779, and 31780) at 1 week of age, indicating the presence of replicating SIVmac1A11. After oral inoculation of these animals with SIVmac251 at 4 weeks of age, SIV RNA levels in plasma in three of the group 5 animals initially spiked to levels as high as those observed in the unvaccinated controls (Fig. 2), but from 6 weeks of age (2 weeks after challenge) SIV RNA levels declined to 10- to 100-fold lower than those of unvaccinated controls. At 12 to 16 weeks of age, there were two animals of group 5 with moderate viremia and two animals with low viremia, and thus there was no difference in viremia with the group 3 animals.
FIG. 2.
Virus levels in blood. Levels of SIV RNA in plasma (top panel) were measured by bDNA assay, whereas cell-associated virus levels (bottom panel) were measured by limiting dilution assay. Vaccine (V) was administered within 3 days after birth and 3 weeks later. All monkeys were challenged (C) orally with SIVmac251 at 4 weeks of age.
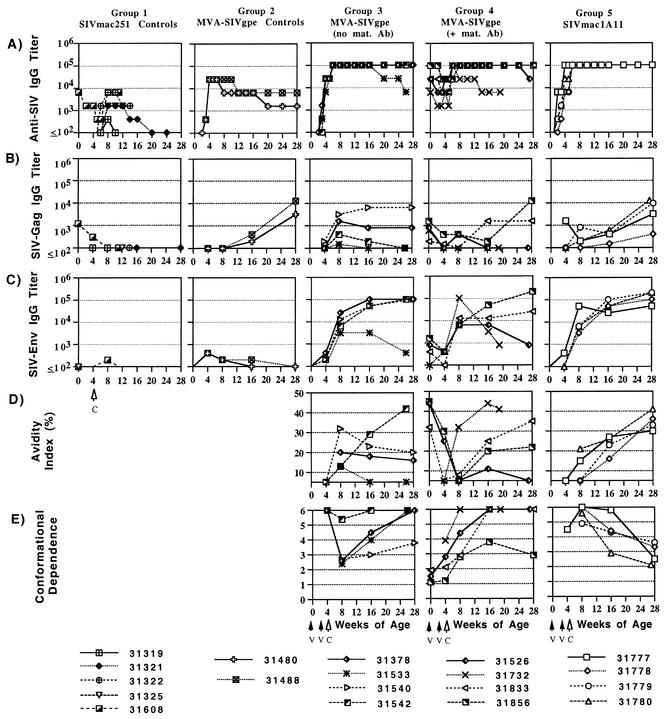
FIG. 3.
Measurements of quantitative and qualitative antibody responses in infant macaques orally inoculated with SIVmac251. Quantitative levels of SIV whole virus (A) and gag-specific (B) antibodies were determined in a standard ELISA. SIV Env-specific antibody endpoint titers (C), avidity (D), and conformational dependence (E) were determined in a ConA ELISA. All procedures are described in Materials and Methods.
During the first 10 weeks after oral challenge, each immunized group had significantly reduced mean SIV RNA levels in plasma after SIVmac251 infection compared to the mean SIV RNA levels in plasma in the unimmunized animals (group 3 versus group 1, P = 0.0011; group 4 versus group 1, P = 0.0291; and group 5 versus group 1, P = 0.0019). Due to the small number of animals per group and the larger variation in SIV RNA levels in plasma among vaccinated animals, no statistically significant differences in SIV RNA levels were detected among the three vaccine groups (groups 3, 4, and 5). However, from weeks 8 to 24 after challenge, only vaccinated groups 3 and 5 had mean SIV RNA levels in plasma that were significantly lower than those of the controls (group 3 versus group 1, P = 0.0005; group 4 versus group 1, P = 0.0941; and group 5 versus group 1, P = 0.0012).
Levels of infectious cell-associated SIV in blood of all 17 SIV-infected infants showed considerable variation among animals within each group and temporal variation for individual animals, and thus there were no significant differences among the experimental groups in cell-associated infectious virus levels at the time of peak viremia or thereafter (Fig. 2). Cell-associated SIV levels in blood peaked at 1 or 2 weeks after oral challenge (460 to 21,530 TCID50 per million PBMC) and thereafter ranged from 10 to 2,150 TCID50 per million PBMC.
Quantitative and qualitative comparison of antiviral antibody responses in infant macaques.
Total antiviral IgG antibody responses were quantified by whole-SIV ELISA. Gag- and Env-specific antibodies were measured by using protein-based ELISA assays. For those samples with detectable Env-specific antibodies, measurements of antibody avidity and conformational dependence were determined as described in Materials and Methods.
Except for maternally derived antibodies in animal 31608, all five SIVmac251-infected animals of group 1 had undetectable, or else low and transient de novo IgG responses, to whole SIV Gag and Env. The inability of these infants to mount or maintain antiviral antibody responses is a result of the rapid immunosuppression induced by the highly virulent SIVmac251 isolate.
The two animals of group 2, which were immunized with MVA-SIVgpe but were not challenged with SIVmac251, mounted a rapid anti-SIV IgG response by 4 weeks of age (titer of 1:25,600), and the antibodies persisted throughout the observation period (Fig. 3). This observation demonstrates the immunogenicity of this vaccine in infant macaques. However, SIV Env-specific endpoint titers were low at 4 weeks of age and became undetectable at 16 to 28 weeks of age. In contrast, SIV Gag-specific antibody responses continued to increase during the 28 weeks. Because MVA has been shown to have limited replication in human cells in vitro (3), the slow increase in SIV Gag-specific antibody responses in these infant macaques suggest that immunization with MVA-SIVgpe may result in a low level of residual replication with preferential expression of gag epitopes.
At birth, prior to the immunizations, the four infants of group 4 already had moderate to high levels of maternally derived whole SIV-specific antibodies, moderate levels of SIV Gag-specific antibodies, and except for animal 31732, detectable levels of anti-SIV Env antibodies (Fig. 3). At 4 weeks of age (i.e., after the two immunizations with MVA-SIVgpe or SIVmac1A11) all animals of groups 3, 4, and 5 had moderate to high antibody titers against whole SIV (titers of 6,400 to 102,400) but low levels of antibodies to SIV Gag and Env. After oral inoculation with SIVmac251 at 4 weeks of age, antibody titers followed a similar pattern: despite individual variation within each group, the immunized animals of groups 3, 4, and 5 mounted similar levels of whole SIV-, SIV Gag-, and SIV Env-specific antibodies during the first 4 weeks after SIV infection. Later, there was more variation in SIV-specific antibody levels. In general, antiviral antibody titers, in particular the Gag-specific antibody titers, declined for animals that developed AIDS within the 28 weeks of observation period (group 3, animals 31533 and 31542; group 4, animals 31526 and 31732) but remained stable or increased for animals that were clinically still asymptomatic at 28 weeks of age (including all of the group 5, SIVmac1A11-immunized animals). The maternal antibodies in group 4 animals did not have any detectable inhibitory effect on the levels of SIV-specific antibodies produced during the first 4 to 12 weeks of SIVmac251 infection. In summary, the immunizations with MVA-SIVgpe or SIVmac1A11 primed animals in groups 3, 4, and 5 to produce similar levels of SIV-specific antibodies early after SIVmac251 infection.
In contrast, there were marked differences among animals of groups 3, 4, and 5 in the quality of SIV-envelope specific antibodies as assessed by avidity and conformational dependence. In group 3 (MVA-SIVgpe immunized), SIV Env antibodies at the time of oral challenge had low or undetectable avidity but high conformation ratios (indicating reactivity to native envelope glycoprotein). For three of these four animals, avidity index values peaked by 4 weeks after SIV infection but remained low (≤32%) and declined afterward; the conformation ratio in these animals showed a pattern opposite to avidity, in that the conformation ratio dropped sharply 4 weeks after SIV infection but then increased again to higher levels, indicating preferential recognition of native envelope glycoprotein. Animal 31542 was the only animal for which the SIV envelope antibody avidity index increased gradually to intermediate levels (42%) by the onset of AIDS at 26 weeks of age and for which the conformational dependence remained remained high and showed little variation over time.
For the group 4 animals (MVA-SIVgpe-immunized infants with maternally derived SIV antibodies at birth) anti-SIV Env antibodies were detectable in only three of four animals at birth; the anti-env antibodies from these three animals had a moderate avidity index (32 to 45%) and a low conformational dependence (between 1 and 2; Fig. 3) that is consistent with a mature antibody response in their immunized mothers (6, 8, 29). For these three animals, there was a sharp decrease in avidity index after MVA-SIVgpe immunization (i.e., prior to SIVmac251 inoculation). After a further decrease for two animals during the first 4 weeks of SIV infection, there was a slower increase in avidity index compared to group 3 animals (which already had SIV Env antibodies with detectable avidity 4 weeks after oral SIVmac251 challenge; Fig. 3). This suggests that the de novo anti-SIV Env antibody response of these infants that was clearly detectable 4 weeks after SIV infection (Fig. 3C) consisted mainly of antibodies with very low avidity. In contrast, the fourth animal (i.e., animal 31732), which did not have detectable maternally derived anti-env antibodies at birth, mounted anti-env antibodies with moderate avidity within 4 weeks after SIV infection, a finding similar to the response of the group 3 animals that lacked maternal antibodies. For all four animals, the conformational dependence increased after SIV infection but then decreased again for animal 31856.
For the group 5 animals (SIVmac1A11 immunized), SIV-env antibody levels at 4 weeks of age were only detectable at sufficient levels in one animal (animal 31777) to allow measurements of antibody quality; the anti-env antibodies in this animal were found to have low avidity and high conformational dependence (Fig. 3). After SIVmac251 infection, SIV-env antibody avidity values for all four SIVmac1A11-immunized animals increased gradually to intermediate levels (30 to 41%) and were higher than those of most of the MVA-SIVgpe-immunized animals of groups 3 and 4. In contrast to the MVA-SIVgpe-immunized animals in groups 3 and 4, the conformational dependence of the anti-SIV Env antibodies of group 5 animals was high (>4) shortly after oral challenge with SIVmac251 but then decreased until 28 weeks of age, a finding consistent with previous reports of antibody maturation resulting from intravenous attenuated SIV infection (6, 8, 29).
In summary, there was a correlation between the development and maintenance of high antiviral antibody titers and lower viremia and delayed disease course. In contrast, the time course of the parameters of antibody quality was more complex, and there was no clear correlation of antibody quality with virus levels or survival. The initial mode of exposure to antigen (type of vaccine and the presence or absence of maternal antibodies) appeared to have modulated the parameters of SIV-specific antibody quality early during infection, and the subsequent changes in SIV envelope-specific antibody quality reflect most likely a complex process of antibody maturation in the presence of various degrees of immunosuppression.
Quantification of virus-specific IFN-γ-secreting lymphocytes.
The presence of virus-specific IFN-γ-secreting cells in PBMC was measured by an ELISPOT assay by using stimulation with overlapping peptides of the p24 Gag region. For all animals, cryopreserved PBMC samples that were collected at 4, 5, 6, and 8 weeks of age (i.e., the day of oral SIVmac251 challenge and 1, 2, and 4 weeks afterward) were tested. All PBMC samples collected at the time of the oral SIVmac251 challenge had levels of SIV-specific IFN-γ-secreting cells below the cutoff value (see Materials and Methods). After SIVmac251 infection, only two samples had detectable levels of virus-specific IFN-γ-secreting cells: group 4 animal 31833 (week 8 of age, 80 SFC/million PBMC; medium-control wells, 0 SFC/million PBMC), and group 5 animal 31777 (week 5 of age, 128 SFC/million PBMC; medium control wells, 43 SFC/million PBMC). Both of these animals developed moderate viremia (viral RNA levels at 12 to 16 weeks were between 107 and 108 copies per ml of plasma). None of the animals that developed low viremia (<107) had detectable virus-specific IFN-γ-secreting cells at these early time points after infection. For the two MVA-SIVgpe-immunized animals of group 2, which did not receive SIVmac251 challenge, no IFN-γ-secreting cells were detected at these same time points.
Immune response to cholera toxin and tetanus toxoid.
None of the 19 neonates in the study had any maternal antibodies against cholera toxin at birth. After the first cholera toxin subunit B immunization at 2 weeks of age (2 weeks prior to oral SIV inoculation), all 19 animals developed a strong primary antibody response (cholera toxin-specific IgG titer of ≥25,600 at 8 weeks of age), demonstrating competence of infant macaques to respond immunologically to this antigen. All animals also made an anamnestic response (≥4-fold increase in IgG titer; data not shown) after the second cholera toxin subunit B immunization at 10 weeks of age (6 weeks after oral challenge). These cholera toxin subunit B antibody responses show that even in the unimmunized, SIV-infected control animals (group 1), primary and secondary antibody responses to non-SIV antigens were not impaired at these stages of SIV infection.
Most animals had maternally derived antibodies to tetanus toxoid that declined after birth with a half-life of ca. 2 weeks. At the time of the first immunization (6 weeks of age), tetanus toxoid-specific IgG titers ranged from 1:100 to 1:6,400. For the animals with high anti-tetanus toxoid titers (1:1,600 to 1,601:6,400), an absence of a further decline of tetanus toxoid-specific IgG was therefore interpreted as evidence of a primary immune response. Except for animals 31319 (group 1) and 31526 (group 4), all animals made a primary tetanus toxoid-specific antibody response. Animals received a booster immunization with tetanus toxoid at 14 weeks of age (10 weeks pc). In group 1, only animal 31321 was still alive and made a weak (∼2-fold increase in titer) secondary tetanus toxoid response. For groups 2 to 5, there was a correlation between the degree of the booster response with clinical outcome; animals 31732 and 31533 (which both developed AIDS at 19 and 26 weeks of age, respectively) had a weak increase (2- to 4-fold), whereas all other animals had a ≥4-fold increase in tetanus toxoid-specific IgG titers.
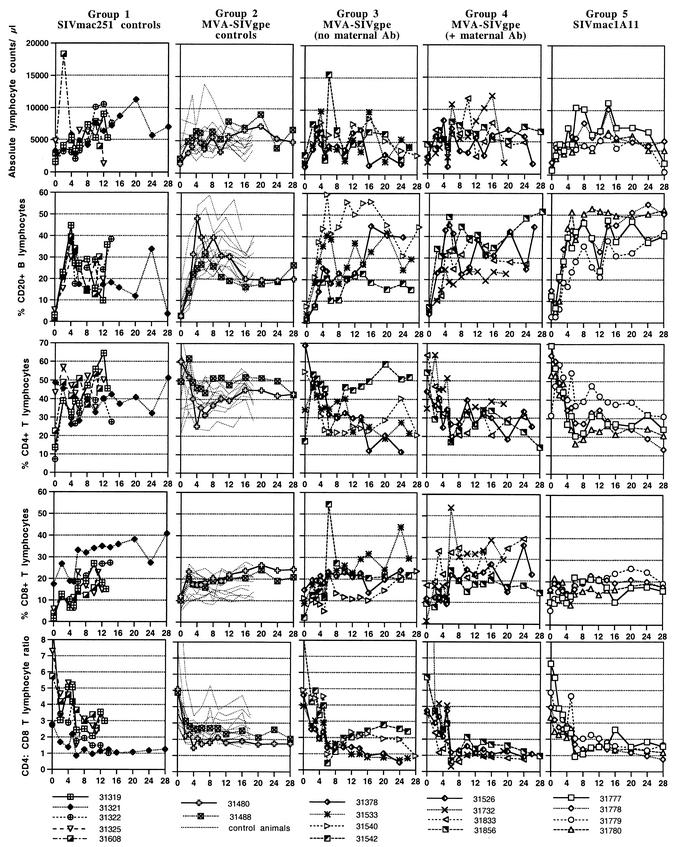
Lymphocyte subset populations.
Absolute lymphocyte counts were quite variable over time in all animals, even for animals that were not SIV infected (group 2), and absolute counts of the T- and B-lymphocyte subsets showed similar levels of variability (Fig. 4). The percentages of cell types were more reliable parameters for comparing the animal groups.
FIG. 4.
Lymphocyte subsets in peripheral blood as measured by flow cytometric analyses. The percentages are expressed as fractions of the total number of lymphocytes.
Similar to humans, infant macaques have age-related changes in their numbers of total lymphocytes and lymphocyte subsets (12). In particular, newborn animals have a high percentage of CD4+ T lymphocytes and a low percentage of CD8+ T lymphocytes, resulting in a high CD4/CD8 ratio (>3). During the first few months of age, there is a gradual decrease in CD4+ T lymphocytes and an increase in CD8+ T lymphocytes (Fig. 4), resulting in a decrease of the CD4/CD8 ratio to ca. 2 to 3. There is also an age-related increase in CD20+ B lymphocytes (Fig. 4). Lymphocyte subsets of the unchallenged MVA-SIVgpe-immunized animals (group 2) were indistinguishable from those of normal, age-matched control animals. For the other animals, all of which became infected after oral SIVmac251 inoculation at 4 weeks of age, some interesting observations were made. Except for the SIVmac1A11-immunized animals, the majority of the other animals had at least a 35% drop in absolute lymphocyte counts at 1 week postchallenge. Whereas the unimmunized SIVmac251-infected animals showed absolute counts and percentages of CD20+ B lymphocytes near or below the range for uninfected animals, most immunized animals (groups 3 to 5), in particular the SIVmac1A11-immunized infants (group 5), had B lymphocytes within the normal range.
Unexpectedly, the unimmunized SIV-infected animals (group 1) showed percentages and numbers of CD4+ T lymphocytes that were generally in the range of the uninfected animals (Fig. 4). In contrast, most animals of groups 3, 4, and 5 had a sudden decrease in percent CD4+ T lymphocytes 2 weeks after SIVmac251 inoculation, which slowly recovered but did not reach preinfection baseline values. Absolute CD4+-T-lymphocyte counts in groups 3 to 5 were within the normal range (>1,000/μl) during the first few months after SIV infection, but total lymphocyte counts were also often elevated (Fig. 4). The numbers of CD4+ T lymphocytes declined in seven animals of groups 3 to 5 by ≥16 weeks of age to <1,000/μl, concomitant with a decline in absolute total lymphocyte counts.
For the majority of animals, SIV infection was associated with increased and more variable percentages of CD8+ T lymphocytes. An exception were the SIVmac1A11-immunized animals (group 5) and the MVA-SIVgpe-immunized animals of groups 3 and 4 that had slower disease progression (e.g., animals 31540 and 31856), for which the percentage of CD8+ T lymphocytes showed a minor increase after SIVmac251 infection and remained more stable throughout the observation period (Fig. 4).
As a result of these opposite changes in the percentages of CD4+ and CD8+ T lymphocytes, the CD4/CD8 ratios were essentially unchanged in most of the unimmunized SIVmac251-infected animals (group 1) but were reduced in all immunized SIVmac251-infected groups (groups 3 to 5), especially in the MVA-SIVgpe-immunized animals (groups 3 to 4), with a nadir occurring 2 weeks after SIVmac251 infection (Fig. 4).
DISCUSSION
The primary goal of the present study was to determine whether SIV vaccines given as early as possible after birth could rapidly induce immunity against oral challenge with pathogenic SIVmac251. The second objective was to examine whether maternally acquired anti-SIV antibodies affected the generation of immune responses and the efficacy of active immunization of the infants.
Infant macaques were inoculated orally with SIVmac251 at 4 weeks of age. Four of the five unimmunized control animals exhibited persistently high virus levels and poor antiviral immune responses, and they developed fatal immunodeficiency within 11 to 14 weeks of age (i.e., 7 to 10 weeks after SIVmac251 infection). This rapid disease course in the majority of unimmunized animals is indistinguishable from our previous observations when animals were inoculated with SIVmac251 at birth (25, 46, 49). The observation that anti-SIV immune responses in these SIV-infected animals were very weak, whereas these animals were able to make immune responses to other non-SIV antigens, is in agreement with the recent observation that HIV preferentially infects HIV-specific CD4+ T lymphocytes, and thus antiviral immune responses are even suppressed prior to the development of generalized immunodeficiency (13).
We demonstrated that both vaccines, MVA-SIVgpe and SIVmac1A11, elicited rapid immune responses in infant macaques. Thus, the immune system of newborn monkeys is competent to make immune responses, a finding in agreement with the results of HIV-1 vaccine trials in human neonates (4, 26). Neither of the two vaccines in our study prevented SIV-infection after oral challenge at 4 weeks of age. However, both vaccines primed the infant macaque immune system such that, after challenge with pathogenic SIVmac251, vaccinated animals (i) mounted rapid, high SIV-specific antibody responses; (ii) more effectively controlled virus replication; and (iii) had longer disease-free survival than the unvaccinated infants. Similar results were reported for juvenile macaques immunized with MVA expressing SIV antigens and challenged intravenously or intrarectally with pathogenic SIV (18, 32, 35, 37). The efficacy of the MVA-SIVgpe vaccine is due to the expression of SIV proteins and not simply to infection with MVA vector, since immunization of newborn macaques with MVA expressing measles antigens did not affect viremia or disease course after SIVmac251 challenge (unpublished observations). We previously reported that two of five macaques infected with SIVmac1A11 in utero or at birth were protected from oral SIVmac251 challenge (33). That study differed from the present one, however, in that monkeys were challenged 1 year after SIVmac1A11 infection, which allowed more time for immune responses to mature.
In the current study, both MVA-SIVgpe and SIVmac1A11 primed the immune system of the infant rhesus macaques to make more rapid antiviral immune responses after SIVmac251 infection. Both group 3 (MVA-SIVgpe) and group 5 (SIVmac1A11) animals had similar virus levels after SIV infection. However, the four SIVmac1A11-immunized animals remained healthy at 28 weeks of age, and they had minor histopathological evidence of opportunistic infections; in contrast, two of the four MVA-SIVgpe-immunized animals had developed simian AIDS by 28 weeks. The maturation of the antibody responses also differed among these two groups. Three of four MVA-SIVgpe-immunized animals (group 3) had, after an initial peak at 8 weeks of age, a gradual decrease in antibody avidity; all four animals had, after an initial decline early after SIV infection, a progressive increase in conformational dependence (indicating more recognition of conformational epitopes than of linear epitopes). This pattern displayed by the MVA-SIVgpe-immunized group 4 monkeys is similar to that previously observed for some HIV-infected people (6). In contrast, the development of a high anti-SIV Env antibody response with a gradual increase in avidity and decrease of the conformational dependence observed for all four SIVmac1A11-immunized animals is consistent with that reported previously for juvenile and adult macaques infected with other attenuated or pathogenic strains of SIV (6, 8) and indicates that antibody responses are broadening to also include fewer conformational epitopes (i.e., including linear epitopes) (7). Despite these different patterns, there was no detectable correlation between these changes in antibody quality and virus levels or disease progression, a finding that suggests that the role of antibody quality on virus replication and the disease course in infants is not clear. It is possible that these distinct temporal patterns of antibody quality between animals immunized with the two different SIV vaccines reflect a combination of initial differences in SIV vaccine epitopes or their expression level during the priming of the immune system, followed by differences in SIV-induced immunosuppression (8).
The second objective of this study was to determine the effect of maternally derived SIV antibodies on the efficacy of SIV vaccines. One group of newborn macaques (group 4) was born to SIV-immunized macaques and therefore had maternal antiviral antibodies. We immunized these newborns with MVA-SIVgpe and then challenged them orally with SIVmac251. Compared to the results of a similar challenge by using MVA-SIVgpe-vaccinated infant macaques born without maternal antibodies (group 3), both groups of MVA-SIVgpe-immunized infants had similar clinical outcomes (two of four animals in each group were healthy at 28 weeks of age). Both groups also developed similar levels of SIV-specific antibodies. This finding is consistent with the antibody responses observed in infants, born to HIV-infected women, who were given an HIV-1 recombinant gp120 vaccine (26). In a measles model in macaques, immunization of infant (51) or juvenile monkeys (39) with an MVA-based measles vaccine was effective in the presence of passively acquired neutralizing antibody. In addition, a trial in which human newborns with maternal antibodies received an accelerated immunization schedule with recombinant HIV-1 gp120 also found that the presence of maternal antibodies did not inhibit a de novo antibody response (26). In the present study in infant macaques, although no effect on vaccine efficacy was observed, our observations suggest that maternal antibodies caused differences in the antibody quality, in particular with respect to avidity, after MVA-SIVgpe immunization (Fig. 3). The data suggest that, in the presence of maternal antibodies, the expression of SIV antigens by MVA-SIVgpe may have induced the clearance of high-avidity antibodies from the circulation and that these maternal antibodies may have masked particular SIV epitopes needed to prime the induction of high-avidity SIV antibodies; thus, infants only started to make a primary immune response to these epitopes after SIVmac251 infection and when maternally derived SIV antibody levels were reduced. Although these measures of antibody quality did not show a detectable correlation with virus levels and survival in the SIV-infected infant macaques in the present study, these observations suggest that data regarding antibody quality derived from HIV vaccine trials in uninfected adults cannot necessarily be extrapolated to infants who have maternally derived HIV antibodies. This underscores the urgent need for HIV vaccine studies that are targeted specifically for infants born to HIV-infected women.
These results appear to contrast with those of our previous studies that indicated an important role for anti-SIV IgG in preventing SIV infection in neonatal macaques (44, 49). However, these studies are not directly comparable because of differences in the experimental design (transplacental transfer or passive immunization with pooled serum versus active immunization), differences in measures of antibody quality (avidity and conformational dependence), and different ages at the time of virus challenge (neonates versus 4-week-old infants).
In the present study, immunization with MVA-SIVgpe or SIVmac1A11 at birth and 3 weeks of age did not give any detectable levels of virus-specific IFN-γ-secreting PBMC by 4 weeks of age, when the animals were exposed orally to SIVmac251. The 4-week time period of immunizations in the present study may have been too short to induce detectable levels in peripheral blood, especially for newborn animals. Although immunization of human newborns with optimal dosage regimens of recombinant HIV-1 gp120 in adjuvant induced proliferative responses in PBMC at week 4, results from these different assays cannot be compared directly (4). In addition, peripheral blood samples are probably not representative of cell-mediated immune responses that occur in lymphoid tissues or mucosal sites (1, 17). It is unknown whether virus-specific IFN-γ-secreting cells were present in the mucosa and lymphoid tissues that drain the upper orogastrointestinal tract, where SIVmac251 infection was initiated. After infection with SIVmac251, only two animals had detectable levels of virus-specific IFN-γ-secreting PBMC at a single time point within the first 4 weeks of infection, and neither of these animals was able to control viremia to low levels. Although further research on the early development of cell-mediated immunity is needed, these findings are in agreement with observations of infrequent detection of HIV-specific effector CD8+-T-cell activity in HIV-infected infants under 3 years of age (36).
Flow cytometric determination of lymphocyte subsets revealed some interesting trends. The lymphopenia during acute infection and subsequent increase in CD8+ T lymphocytes were expected findings based on prior experiments. Surprising findings were that the unimmunized SIV-infected control animals (group 1) maintained a relatively normal percentage of CD4+ T lymphocytes compared to the immunized animals after oral SIV challenge. Several of these group 1 animals showed histopathological evidence of lymphoid hyperplasia at the time of necropsy (Table 1). Altogether, these findings suggest that the rapid immunosuppression and rapid disease course in the group 1 animals was more likely due to a functional defect in CD4+ T helper cells than to a direct effect of depletion. In contrast, most immunized animals had a reduction in the percentage of CD4+ T lymphocytes and an increase in the percentage of CD8+ T lymphocytes in peripheral blood early after SIVmac251 infection, which is probably due to a combination of changes in cell death or proliferation and redistribution among lymphoid compartments (5, 28).
In summary, the present study underscores the relevance of the SIV infant macaque model for evaluating strategies to prevent maternal transmission of HIV. In developing countries, there is a critical need for a vaccine that can protect babies born to HIV-infected women from infection acquired via breast-feeding. In the present study, immunization with MVA-SIVgpe or SIVmac1A11 did not protect infant macaques against oral infection with virulent SIVmac251 and did not modulate the specific SIV variants that established systemic infection (unpublished data). However, vaccinated infant macaques had lower viral levels, enhanced immune responses, and longer disease-free survival times than unvaccinated infants, demonstrating that both SIV vaccines substantially altered the disease course. A vaccine capable of inducing more effective immune responses rapidly, especially near the site of initial exposure to virus, is needed to prevent viral infection.
Acknowledgments
We thank N. Aguirre, S. Au, D. Bennet, D. Brandt, I. Bolton, K. Bost, L. Brignolo, K. Christe, L. Hirst, A. Spinner, K. Schmidt, W. von Morgenland, and the California National Primate Research Center Colony Services for expert technical assistance. We thank Shilpa Hattangadi and Lynn Frampton for construction of recombinant MVAs; the NIH AIDS Research and Reference Reagent Program, Division of AIDS, NIAID, NIH, for providing the SIV p55 Gag protein and the 20-mer peptides of the p24 Gag region; and R. Desrosiers (New England Regional Primate Research Center) for the plasmid containing the SIVmac239 env gene. Neil Willits, Statistical Laboratory, University of California at Davis, provided expert assistance for statistical analyses.
This work was supported by Public Health Science grant RR00169 from the National Center for Research Resources, NIH/NIAID grants AI39109 (M.L.M.), AI46320 (M.L.M.), and AI47758 (K.S.C., J.D.S., and R.C.M.), and Elizabeth Glaser Scientist award 8-97 (M.L.M.) from the Elizabeth Glaser Pediatric AIDS Foundation.
REFERENCES
- 1.Abel, K., M. J. Alegria-Hartman, K. Zanotto, M. B. McChesney, M. L. Marthas, and C. J. Miller. 2001. Anatomic site and immune function correlate with relative cytokine mRNA expression levels in lymphoid tissues of normal rhesus macaques. Cytokine 16:191-204. [DOI] [PubMed] [Google Scholar]
- 2.Bertolli, J., M. E. St. Louis, R. J. Simonds, P. Nieburg, M. Kamenga, C. Brown, M. Tarande, T. Quinn, and C. Y. Ou. 1996. Estimating the timing of mother-to-child transmission of human immunodeficiency virus in a breast-feeding population in Kinshasa, Zaire. J. Infect. Dis. 174:722-726. [DOI] [PubMed] [Google Scholar]
- 3.Blanchard, T. J., A. Alcami, P. Andrea, and G. L. Smith. 1998. Modified vaccinia virus Ankara undergoes limited replication in human cells and lacks several immunomodulatory proteins: implications for use as a human vaccine. J. Gen. Virol. 79:1159-1167. [DOI] [PubMed] [Google Scholar]
- 4.Borkowsky, W., D. Wara, T. Fenton, J. McNamara, M. Kang, L. Mofenson, E. McFarland, C. Cunningham, A.-M. Duliege, D. Francis, Y. Bryson, S. Burchett, S. A. Spector, L. M. Frenkel, S. Starr, R. Van Dyke, E. Jiminez, et al. 2000. Lymphoproliferative responses to recombinant HIV-1 envelope antigens in neonates and infants receiving gp120 vaccines. J. Infect. Dis. 181:890-896. [DOI] [PubMed] [Google Scholar]
- 5.Bucy, R. P., R. D. Hockett, C. A. Derdeyn, M. S. Saag, K. Squires, M. Sillers, R. T. Mitsuyasu, and J. M. Kilby. 1999. Initial increase in blood CD4+ lymphocytes after HIV antiretroviral therapy reflects redistribution from lymphoid tissues. J. Clin. Investig. 103:1391-1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cole, K. S., M. Murphey-Corb, O. Narayan, S. Y. Joag, G. M. Shaw, and R. C. Montelaro. 1998. Common themes of antibody maturation to simian immunodeficiency virus, simian-human immunodeficiency virus, and human immunodeficiency virus type 1 infections. J. Virol. 72:7852-7859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cole, K. S., M. J. Paliotti, M. Murphey-Corb, and R. C. Montelaro. 2000. Maturation of envelope-specific antibody responses to linear determinants in monkeys inoculated with attenuated SIV. J. Med. Primatol. 29:220-230. [DOI] [PubMed] [Google Scholar]
- 8.Cole, K. S., J. L. Rowles, B. A. Jagerski, M. Murphey-Corb, T. Unangst, J. E. Clements, J. Robinson, M. S. Wyand, R. C. Desrosiers, and R. C. Montelaro. 1997. Evolution of envelope-specific antibody responses in monkeys experimentally infected or immunized with SIV and its association with the development of protective immunity. J. Virol. 71:5069-5079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dabis, F., P. Msellati, N. Meda, C. Welffens-Ekra, B. You, O. Manigart, V. Leroy, A. Simonon, M. Cartoux, P. Combe, A. Ouangré, R. Ramon, O. Ky-Zerbo, C. Montcho, R. Salamon, C. Rouzioux, P. Van de Perre, L. Mandelbrot, et al. 1999. Six-month efficacy, tolerance, and acceptability of a short regimen of oral zidovudine to reduce vertical transmission of HIV in breastfed children in Côte d'Ivoire and Burkina Faso: a double-blind placebo-controlled multicentre trial. Lancet 353:786-792. [DOI] [PubMed] [Google Scholar]
- 10.Datta, P., J. P. Embree, J. P. Kreiss, J. O. Ndinya-Achola, M. Braddick, M. Temmerman, N. J. D. Nagelkerke, G. Maitha, K. K. Holmes, P. Piot, H. O. Pamba, and F. A. Plummer. 1994. Mother-to-child transmission of human immunodeficiency virus type 1: report from the Nairobi study. J. Infect. Dis. 170:1134-1140. [DOI] [PubMed] [Google Scholar]
- 11.De Cock, K., M. G. Fowler, E. Mercier, I. de Vincenzi, J. Saba, E. Hoff, D. J. Alnwick, M. Rogers, and N. Shaffer. 2000. Prevention of mother-to-child HIV transmission in resource-poor countries: translating research into policy and practice. JAMA 283:1175-1182. [DOI] [PubMed] [Google Scholar]
- 12.DeMaria, M. A., M. Casto, M. O'Connell, R. P. Johnson, and M. Rosenzweig. 2000. Characterization of lymphocyte subsets in rhesus macaques during the first year of life. Eur. J. Haematol. 65:245-257. [DOI] [PubMed]
- 13.Douek, D. C., J. M. Brenchley, M. R. Betts, D. R. Ambrozak, B. J. Hill, Y. Okamoto, J. P. Casazza, J. Kuruppu, K. Kunstman, S. Wolinsky, Z. Grossman, M. Dybul, A. Oxenius, D. A. Price, and R. A. Koup. 2002. HIV preferentially infects HIV-specific CD4+ T cells. Nature 417:95-98. [DOI] [PubMed] [Google Scholar]
- 14.Earl, P. L., L. S. Wyatt, D. C. Montefiori, M. Bilska, R. Woodward, P. D. Markham, J. D. Malley, T. U. Vogel, T. M. Allen, D. I. Watkins, N. Miller, and B. Moss. 2002. Comparison of vaccine strategies using recombinant env-gag-pol MVA with or without an oligomeric Env protein boost in the SHIV rhesus macaque model. Virology 294:270-281. [DOI] [PubMed] [Google Scholar]
- 15.Greenier, J. L., C. J. Miller, D. Lu, P. J. Dailey, F. X. Lü, K. J. Kunstman, S. M. Wolinsky, and M. L. Marthas. 2001. Route of simian immunodeficiency virus inoculation determines the complexity but not the identity of viral variant populations that infect rhesus macaques. J. Virol. 75:3753-3765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guay, L. A., P. Musoke, T. Fleming, D. Bagenda, M. Allen, C. Nakabiito, J. Sherman, P. Bakaki, C. Ducar, M. Deseyve, L. Emel, M. Mirochnick, M. G. Fowler, L. Mofenson, P. Miotti, K. Dransfield, D. Bray, F. Mmiro, and J. B. Jackson. 1999. Intrapartum and neonatal single-dose nevirapine compared with zidovudine for prevention of mother-to-child transmission of HIV-1 in Kampala, Uganda: HIVNET 012 randomized trial. Lancet 354:795-802. [DOI] [PubMed] [Google Scholar]
- 17.Hel, Z., J. Nacsa, B. Kelsall, W.-P. Tsai, N. Letvin, R. Washington Parks, E. Tryniszewska, L. Picker, M. G. Lewis, Y. Edghill-Smith, M. Moniuszko, R. Pal, L. Stevceva, J. D. Altman, T. M. Allen, D. Watkins, J. V. Torres, J. A. Berzofsky, I. M. Belyakov, W. Strober, and G. Franchini. 2001. Impairment of gag-specific CD8+ T-cell function in mucosal and systemic compartments of simian immunodeficiency virus mac251- and simian-human immunodeficiency virus KU2-infected macaques. J. Virol. 75:11483-11495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hirsch, V. M., T. R. Fuerst, G. Sutter, M. W. Carroll, L. C. Yang, S. Goldstein, M. J. Piatak, W. R. Elkins, W. G. Alvord, D. C. Montefiori, B. Moss, and J. D. Lifson. 1996. Patterns of viral replication correlate with outcome in simian immunodeficiency virus (SIV)-infected macaques: effect of prior immunization with a trivalent SIV vaccine in modified vaccinia virus Ankara. J. Virol. 70:3741-3752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kraiselburd, E. N., and J. V. Torres. 1995. Properties of virus-like particles produced by SIV-chronically infected human cell clones. Cell. Mol. Biol. 41:S41-S52. [PubMed] [Google Scholar]
- 20.Kreiss, J. 1997. Breastfeeding and vertical transmission of HIV-1. Acta Paediatr. Suppl. 421:113-117. [DOI] [PubMed] [Google Scholar]
- 21.Leroy, V., M. L. Newell, F. Dabis, C. Peckham, P. Van de Perre, M. Bulterys, C. Kind, R. J. Simonds, S. Wiktor, P. Msellati, et al. 1998. International mulicentre pooled analysis of late postnatal mother-to-child transmission of HIV-1 infection. Lancet 352:597-600. [DOI] [PubMed] [Google Scholar]
- 22.Mahnel, H., and A. Mayr. 1994. Experiences with immunization against orthopox viruses of humans and animals using vaccine strain MVA. Berl. Munch. Tieraerztl. Wochenschrift. 107:253-256. [PubMed] [Google Scholar]
- 23.Marthas, M. L., B. Banapour, S. Sutjipto, M. E. Siegel, P. A. Marx, M. B. Gardner, N. C. Pedersen, and P. A. Luciw. 1989. Rhesus macaques inoculated with molecularly cloned simian immunodeficiency virus. J. Med. Primatol. 18:311-319. [PubMed] [Google Scholar]
- 24.Marthas, M. L., D. L. Lu, M. C. T. Penedo, A. G. Hendrickx, and C. J. Miller. 2001. Titration of an SIVmac251 stock by vaginal inoculation of Indian and Chinese origin rhesus macaques: transmission efficiency, viral loads, and antibody responses. AIDS Res. Hum. Retrovir. 17:1455-1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marthas, M. L., K. K. A. Van Rompay, M. Otsyula, C. J. Miller, D. Canfield, N. C. Pedersen, and M. B. McChesney. 1995. Viral factors determine progression to AIDS in SIV-infected newborn rhesus macaques. J. Virol. 69:4198-4205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McFarland, E. J., W. Borkowsky, T. Fenton, D. Wara, J. McNamara, P. Samson, M. Kang, L. Mofenson, C. Cunningham, A. M. Duliege, F. Sinangil, S. A. Spector, E. Jimenez, Y. Bryson, S. Burchett, L. M. Frenkel, R. Yogev, F. Gigliotti, K. Luzuriaga, and R. A. Livingston. 2001. Human immunodeficiency virus type 1 (HIV-1) gp120-specific antibodies in neonates receiving an HIV-1 recombinant gp120 vaccine. J. Infect. Dis. 184:1331-1335. [DOI] [PubMed] [Google Scholar]
- 27.Miotti, P. G., T. E. Taha, N. I. Kumwenda, R. Broadhead, L. A. Mtimavalye, L. Van der Hoeven, J. D. Chiphangwi, G. Liomba, and R. J. Biggar. 1999. HIV transmission through breastfeeding: a study in Malawi. JAMA 282:744-749. [DOI] [PubMed] [Google Scholar]
- 28.Mohri, H., S. Bonhoeffer, S. Monard, A. S. Perelson, and D. D. Ho. 1998. Rapid turnover of T lymphocytes in SIV-infected rhesus macaques. Science 279:1223-1227. [DOI] [PubMed] [Google Scholar]
- 29.Montelaro, R. C., K. S. Cole, and S. A. Hammond. 1998. Maturation of immune responses to lentivirus infection: implications for AIDS vaccine development. AIDS Res. Hum. Retrovir. 14:S255-S259. [PubMed] [Google Scholar]
- 30.National Research Council. 1996. Guide for the care and use of laboratory animals. National Academy Press, Washington, D.C.
- 31.Nduati, R., G. John, D. Mbori-Ngacha, B. Richardson, J. Overbaugh, A. Mwatha, J. Ndinya-Achola, J. Bwayo, F. E. Onyango, J. Hughes, and J. Kreiss. 2000. Effect of breastfeeding and formula feeding on transmission of HIV-1. JAMA 283:1167-1174. [DOI] [PubMed] [Google Scholar]
- 32.Nilsson, C., G. Sutter, L. Walther-Jallow, P. ten Haaft, L. Åkerblom, J. Heeney, V. Erfle, P. Böttiger, G. Biberfeld, and R. Thorstensson. 2002. Immunization with recombinant modified vaccinia virus Ankara can modify mucosal simian immunodeficiency virus infection and delay disease progression in macaques. J. Gen. Virol. 83:807-818. [DOI] [PubMed] [Google Scholar]
- 33.Otsyula, M. G., C. J. Miller, M. L. Marthas, K. K. A. Van Rompay, J. R. Collins, N. C. Pedersen, and M. B. McChesney. 1996. Virus-induced immunosuppression is linked to rapidly fatal disease in infant rhesus macaques infected with simian immunodeficiency virus. Pediatr. Res. 39:630-635. [DOI] [PubMed] [Google Scholar]
- 34.Otsyula, M. G., C. J. Miller, A. F. Tarantal, M. L. Marthas, T. P. Greene, J. R. Collins, K. K. A. Van Rompay, and M. B. McChesney. 1996. Fetal or neonatal infection with attenuated simian immunodeficiency virus results in protective immunity against oral challenge with pathogenic SIVmac251. Virology 222:275-278. [DOI] [PubMed] [Google Scholar]
- 35.Ourmanov, I., C. R. Brown, B. Moss, M. Carroll, L. Wyatt, L. Pletneva, S. Goldstein, D. Venzon, and V. M. Hirsch. 2000. Comparative efficacy of recombinant modified vaccinia virus Ankara expressing simian immunodeficiency virus (SIV) gag-pol and/or env in macaques challenged with pathogenic SIV. J. Virol. 74:2740-2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Scott, Z. A., E. G. Chadwick, L. L. Gibson, M. D. Catalina, M. M. McManus, R. Yogev, P. Palumbo, J. L. Sullivan, P. Britto, H. Gay, and K. Luzuriaga. 2001. Infrequent detection of HIV-1-specific, but not cytomegalovirus-specific, CD8+ T cell responses in young HIV-1-infected infants. J. Immunol. 167:7134-7140. [DOI] [PubMed] [Google Scholar]
- 37.Seth, A., I. Ourmanov, J. E. Schmitz, M. J. Kuroda, M. A. Lifton, C. E. Nickerson, L. Wyatt, M. Carroll, B. Moss, D. Venzon, N. L. Letvin, and V. M. Hirsch. 2000. Immunization with a modified vaccinia virus expressing simian immunodeficiency virus (SIV) Gag-Pol primes for an anamnestic Gag-specific cytotoxic T-lymphocyte response and is associated with reduction of viremia after SIV challenge. J. Virol. 74:2502-2509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shaffer, N., R. Chuachoowong, P. A. Mock, C. Bhadrakom, W. Siriwasin, N. L. Young, T. Chotpitayasunondh, S. Chearskul, A. Roongpisuthipong, P. Chinayon, J. Karon, T. Mastro, R. J. Simonds, et al. 1999. Short-course zidovudine for perinatal HIV-1 transmission in Bangkok, Thailand: a randomized controlled trial. Lancet 353:773-780. [DOI] [PubMed] [Google Scholar]
- 39.Stittelaar, K. J., L. S. Wyatt, R. L. de Swart, H. W. Vos, J. Groen, G. van Amerongen, R. S. van Binnendijk, S. Rozenblatt, B. Moss, and A. D. M. E. Osterhaus. 2000. Protective immunity in macaques vaccinated with a modified vaccinia virus Ankara measles virus vaccine in the presence of passively acquired antibodies. J. Virol. 74:4236-4243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tarantal, A., M. Marthas, S. Gargosky, M. Otsyula, M. McChesney, C. Miller, and A. Hendrickx. 1995. Effects of viral virulence on intrauterine growth in SIV-infected fetal rhesus macaques (Macaca mulatta). J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 10:129-138. [DOI] [PubMed] [Google Scholar]
- 41.The Petra Study Team. 2002. Efficacy of three short-course regimens of zidovudine and lamivudine in preventing early and late transmission of HIV-1 from mother to child in Tanzania, South Africa, and Uganda (Petra Study): a randomized, double-blind, placebo-controlled trial. Lancet 359:1178-1186. [DOI] [PubMed] [Google Scholar]
- 42.Van Rompay, K., M. Marthas, R. Ramos, C. Mandell, E. McGowan, S. Joye, and N. Pedersen. 1992. Simian immunodeficiency virus (SIV) infection of infant rhesus macaques as a model to test antiretroviral drug prophylaxis and therapy: oral 3′-azido-3′-deoxythymidine prevents SIV infection. Antimicrob. Agents Chemother. 36:2381-2386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Van Rompay, K. K. A., C. J. Berardi, N. L. Aguirre, N. Bischofberger, P. S. Lietman, N. C. Pedersen, and M. L. Marthas. 1998. Two doses of PMPA protect newborn macaques against oral simian immunodeficiency virus infection. AIDS 12:F79-F83. [DOI] [PubMed] [Google Scholar]
- 44.Van Rompay, K. K. A., C. J. Berardi, S. Dillard-Telm, R. P. Tarara, D. R. Canfield, C. R. Valverde, D. C. Montefiori, K. Stefano Cole, R. C. Montelaro, C. J. Miller, and M. L. Marthas. 1998. Passive immunization of newborn rhesus macaques prevents oral simian immunodeficiency virus infection. J. Infect. Dis. 177:1247-1259. [DOI] [PubMed] [Google Scholar]
- 45.Van Rompay, K. K. A., J. M. Cherrington, M. L. Marthas, C. J. Berardi, A. S. Mulato, A. Spinner, R. P. Tarara, D. R. Canfield, S. Telm, N. Bischofberger, and N. C. Pedersen. 1996. 9-[2-(Phosphonomethoxy)propyl]adenine therapy of established simian immunodeficiency virus infection in infant rhesus macaques. Antimicrob. Agents Chemother. 40:2586-2591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Van Rompay, K. K. A., P. J. Dailey, R. P. Tarara, D. R. Canfield, N. L. Aguirre, J. M. Cherrington, P. D. Lamy, N. Bischofberger, N. C. Pedersen, and M. L. Marthas. 1999. Early short-term 9-[2-(phosphonomethoxy)propyl]adenine (PMPA) treatment favorably alters subsequent disease course in simian immunodeficiency virus-infected newborn rhesus macaques. J. Virol. 73:2947-2955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Van Rompay, K. K. A., M. L. Marthas, J. D. Lifson, C. J. Berardi, G. M. Vasquez, E. Agatep, Z. A. Dehqanzada, K. C. Cundy, N. Bischofberger, and N. C. Pedersen. 1998. Administration of 9-[2-(phosphonomethoxy)propyl]adenine (PMPA) for prevention of perinatal simian immunodeficiency virus infection in rhesus macaques. AIDS Res. Hum. Retrovir. 14:761-773. [DOI] [PubMed] [Google Scholar]
- 48.Van Rompay, K. K. A., M. B. McChesney, N. L. Aguirre, K. A. Schmidt, N. Bischofberger, and M. L. Marthas. 2001. Two low doses of tenofovir protect newborn macaques against oral simian immunodeficiency virus infection. J. Infect. Dis. 184:429-438. [DOI] [PubMed] [Google Scholar]
- 49.Van Rompay, K. K. A., M. G. Otsyula, R. P. Tarara, D. R. Canfield, C. J. Berardi, M. B. McChesney, and M. L. Marthas. 1996. Vaccination of pregnant macaques protects newborns against mucosal simian immunodeficiency virus infection. J. Infect. Dis. 173:1327-1335. [DOI] [PubMed] [Google Scholar]
- 50.Wiktor, S., E. Ekpini, and J. M. Karon. 1999. Short-course oral zidovudine for prevention of mother-to-child transmission of HIV-1 in Abidjan, Côte d'Ivoire: a randomised trial. Lancet 353:781-785. [DOI] [PubMed] [Google Scholar]
- 51.Zhu, Y., P. Rota, L. Wyatt, A. Tamin, S. Rozenblatt, N. Lerche, B. Moss, W. Bellini, and M. McChesney. 2000. Evaluation of recombinant vaccinia virus-measles vaccines in infant rhesus macaques with preexisting measles antibody. Virology 276:202-213. [DOI] [PubMed] [Google Scholar]