Abstract
Ebola virus causes lethal hemorrhagic fever in humans, but currently there are no effective vaccines or antiviral compounds for this infectious disease. Passive transfer of monoclonal antibodies (MAbs) protects mice from lethal Ebola virus infection (J. A. Wilson, M. Hevey, R. Bakken, S. Guest, M. Bray, A. L. Schmaljohn, and M. K. Hart, Science 287:1664-1666, 2000). However, the epitopes responsible for neutralization have been only partially characterized because some of the MAbs do not recognize the short synthetic peptides used for epitope mapping. To identify the amino acids recognized by neutralizing and protective antibodies, we generated a recombinant vesicular stomatitis virus (VSV) containing the Ebola virus glycoprotein-encoding gene instead of the VSV G protein-encoding gene and used it to select escape variants by growing it in the presence of a MAb (133/3.16 or 226/8.1) that neutralizes the infectivity of the virus. All three variants selected by MAb 133/3.16 contained a single amino acid substitution at amino acid position 549 in the GP2 subunit. By contrast, MAb 226/8.1 selected three different variants containing substitutions at positions 134, 194, and 199 in the GP1 subunit, suggesting that this antibody recognized a conformational epitope. Passive transfer of each of these MAbs completely protected mice from a lethal Ebola virus infection. These data indicate that neutralizing antibody cocktails for passive prophylaxis and therapy of Ebola hemorrhagic fever can reduce the possibility of the emergence of antigenic variants in infected individuals.
Ebola virus, a filamentous, enveloped, nonsegmented negative-strand RNA virus in the family Filoviridae, has caused sporadic outbreaks of lethal hemorrhagic disease for which no effective vaccine or antiviral treatment is available. The virus contains at least seven structural proteins, all of which are translated from monocistronic polyadenylated mRNA transcripts (2, 11). The fourth gene from the 3′ end of the Ebola virus genome encodes two glycoproteins: the envelope glycoprotein (GP), which is responsible for receptor binding and fusion of the virus with the host cell membrane (16, 22), and the nonstructural secretory glycoprotein (sGP), which is released from infected cells (12, 18).
Since GP is the only viral surface protein responsible for virus entry (16, 22), it must be an important target of neutralizing antibodies. However, DNA immunization of mice with the GP of the Zaire species of Ebola virus produced infectivity-enhancing antibodies, as well as neutralizing antibodies, raising issues about the development of passive prophylaxis or treatment with Ebola virus GP antibodies (17). The passive transfer of hyperimmune animal sera has been evaluated in mice, guinea pigs, and monkeys (5, 6, 8, 10) with inconsistent results. Although whole-blood transfusion from convalescent patients was also tested in patients during the Kikwit outbreak of Ebola hemorrhagic fever in 1995 (9), reliable conclusions could not be drawn from these studies owing to the inevitable lack of controls. Serum from mice subcutaneously infected with live Ebola virus protected recipient mice from a lethal challenge (3). However, it is unclear whether virus-induced immune factors other than antibodies (e.g., cytokines) may have affected the efficacy of such treatment. Although the protective efficacy of immune sera varies, as described above, passive transfer of neutralizing MAbs completely protected mice from a lethal Ebola virus infection (21).
B-cell epitopes are not well defined on Ebola virus GP. Thus, it is important not only to analyze the antigenic structure of the proteins but also to understand the mechanisms by which the antibodies interfere with the protein's function (e.g., inhibition of viral receptor binding and fusion). By using synthetic peptides derived from amino acid sequences of Ebola virus species Zaire GP, Wilson et al. (21) identified three epitopes recognized by neutralizing antibodies. However, it is generally believed that the use of synthetic peptides provides limited information about the B-cell epitopes of heavily glycosylated proteins such as Ebola virus GP (11). Since sugar chains are often important in the tertiary structure of these proteins, small synthetic peptides are not usually identical to those of the corresponding regions in the actual glycoprotein. Finally, synthetic peptides do not provide an optimal means of identifying conformational epitopes.
An alternative approach to the identification of B-cell epitopes, including conformational epitopes, is to determine the amino acid changes in antigenic variants that escape antibody neutralization. Thus, we generated a recombinant vesicular stomatitis virus (VSV) containing the GP-encoding gene instead of the VSV G protein-encoding gene and used it to select mutants that escape from neutralization by MAbs. This system allowed us to identify four different amino acid residues involved in the neutralizing activity of the antibodies that protected mice from a lethal Ebola virus infection.
MATERIALS AND METHODS
Viruses and cells.
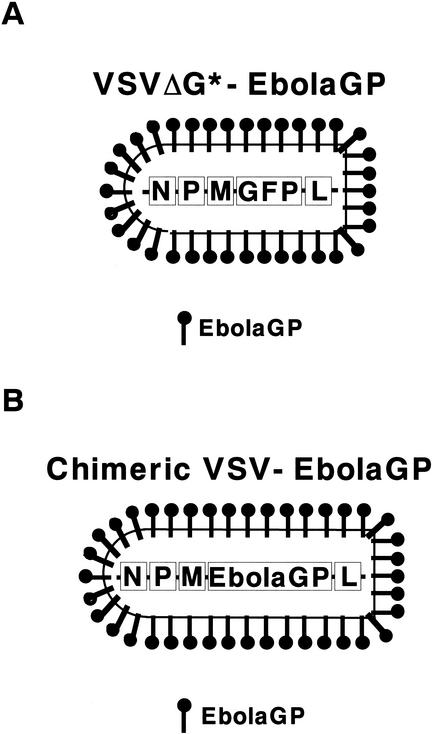
Ebola virus species Zaire, strain Mayinga (wild type), and a mouse-adapted Ebola virus strain (1) were propagated in Vero E6 cells and stored at −80°C until use. VSV pseudotyped with Ebola virus GP (VSVΔG*-EbolaGP) expressing green fluorescent protein (GFP) was generated as previously described (16) (Fig. 1A). Human embryonic kidney 293 cells were grown in Dulbecco modified Eagle medium complemented with 10% fetal bovine serum, l-glutamine, and antibiotics. VSV genomic plasmid pVSV-XN2 and plasmids for nucleoprotein, polymerase, and phosphoprotein expression were kindly provided by J. Rose, Yale University, New Haven, Conn. A recombinant VSV containing the Ebola virus GP-encoding gene instead of the VSV G protein-encoding gene (chimeric VSV-EbolaGP) (Fig. 1B) was generated as follows. The open reading frame of the Ebola virus GP-encoding gene was cloned into plasmid pVSV-XN2 lacking the VSV G protein-encoding gene (VSV-ΔG) at the site where the VSV G protein-encoding gene was deleted. The recombinant VSV expressing Ebola virus GP instead of VSV G protein (chimeric VSV-EbolaGP) was then generated as previously described (14). The virus was propagated in Vero E6 cells, and its titer was determined by plaque assay (107 PFU/ml). A characterization of the recombinant virus will be published elsewhere. All infectious materials involving chimeric VSV-EbolaGP were handled in a biosafety level 4 facility at the Canadian Science Centre for Human and Animal Health.
FIG. 1.
Schematic diagram of the two recombinant VSVs used in this study. (A) VSVΔG*-EbolaGP is a VSV pseudotyped with Ebola virus GP that contains the GFP-encoding gene instead of the VSV G protein-encoding gene and thus is not infectious unless a receptor binding/fusion protein (e.g., Ebola virus GP) is provided in trans. (B) Chimeric VSV-EbolaGP contains the Ebola virus GP-encoding gene in place of the VSV G protein-encoding gene and therefore can undergo multiple cycles of replication without complementation.
MAbs.
MAbs were produced as described previously (17). The hybridomas producing MAbs 133/3.16 (immunoglobulin G1 [IgG1]), 226/8.1 (IgG1), and 42/3.7 (IgG1) were grown in PFHM II (GIBCO BRL), and the antibodies were purified from the supernatants with protein A agarose columns (Bio-Rad). Mouse ascites was obtained by a standard procedure, and the concentration of GP-specific antibodies in the ascites was determined by enzyme-linked immunosorbent assay (ELISA) by using the purified antibodies as standards.
Virus neutralization tests of VSV pseudotyped with Ebola virus GP and Ebola virus.
VSVΔG*-EbolaGP or Ebola virus species Zaire was incubated with MAbs for 1 h at room temperature and inoculated onto monolayers of 293 cells. Infectivities of the viruses were determined by counting the fluorescent cells as described previously (16). The relative percentage of infected cells was determined by setting the number of infected cells in the presence of normal mouse IgG or ascites (approximately 50 to 100 fluorescent cells per microscopic field) to 100.
Immunofluorescence assay.
293 cells infected with Ebola virus were fixed with 2% paraformaldehyde 1 day after infection and treated with 0.1% Triton X-100 in phosphate-buffered saline. To detect virus-infected cells, we used rabbit antiserum to VP40 of Ebola virus (7) as the primary antibody. Goat anti-rabbit IgG conjugated with fluorescein isothiocyanate was purchased from Sigma (St. Louis, Mo.).
Selection of escape mutants.
Tenfold dilutions of chimeric VSV-EbolaGP were incubated with appropriately diluted mouse ascites (250 to 500 μg of specific antibodies/ml) at room temperature for 1 h, and the mixtures were inoculated onto Vero E6 cells. Mutant viruses that grew in the presence of the MAbs were harvested from the highest dilution of the virus. This procedure was repeated. After confirming the growth of the virus in the presence of the antibodies, we extracted the viral RNA and determined the nucleotide sequences of the GP-encoding genes by standard procedures.
Passive immunization and protection tests with mice.
Five-week-old female BALB/c mice (Charles River) were given 100 μl of appropriately diluted ascites (250 μg of specific antibodies/mouse) intraperitoneally on days −1 and 2. On day 0, all mice were intraperitoneally infected with 30 50% lethal doses of the mouse-adapted Ebola virus strain. The mice were monitored for clinical signs of infection for 24 days after the challenge.
RESULTS
Specificity of MAbs.
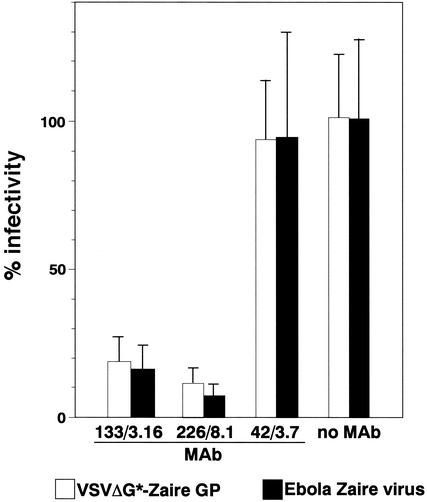
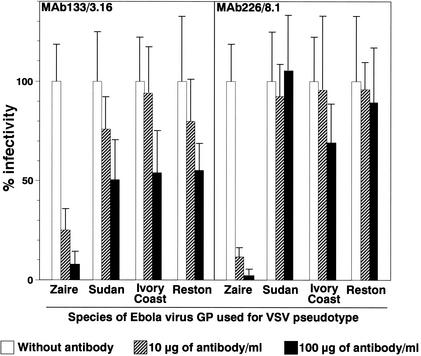
We first used VSV pseudotyped with GP from species Zaire (Fig. 1A) for virus neutralization tests and found that of the 10 clones we generated, two MAbs, 133/3.16 (IgG1) and 226/8.1 (IgG1), neutralized the infectivity of the virus (Fig. 2). We then confirmed that authentic Ebola virus species Zaire infectivity was also neutralized by these antibodies (Fig. 2). MAb 42/3.7 recognized GPs from all of the Ebola virus species in an ELISA (data not shown) but did not neutralize virus infectivity. While both MAbs 133/3.16 and 226/8.1 efficiently neutralized the infectivity of VSV pseudotyped with GP from species Zaire, neither of these MAbs appreciably neutralized the infectivity of the virus pseudotyped with GPs from the other Ebola virus species, Sudan, Ivory Coast, and Reston (Fig. 3). Limited cross-neutralizing activity was found with MAb 133/3.16 when the viruses were treated with the antibody at a higher concentration (100 μg/ml). The species specificity of these MAbs was also confirmed by ELISA with cells transfected with plasmids expressing these GPs (data not shown).
FIG. 2.
Neutralizing activity of MAbs to Zaire GP. VSV pseudotyped with GP of Ebola virus species Zaire or authentic Ebola virus species Zaire was incubated with purified antibodies (10 μg/ml) and inoculated onto 293 cells. Infectivity was determined by counting fluorescent cells. The relative percentage of infectivity was determined by setting the number of infected cells in the presence of normal mouse ascites (approximately 50 to 100 GFP-positive cells per microscopic field) at 100.
FIG. 3.
Cross-neutralizing activities of MAbs. VSV pseudotyped with GP of Ebola virus species Zaire, Sudan, Ivory Coast, or Reston was incubated with the indicated concentrations of the purified antibodies and inoculated onto 293 cells. The other experimental conditions were the same as those described in the legend to Fig. 2.
Protective effects of passive immunization of mice with neutralizing antibodies.
We next tested the protective potential of the neutralizing antibodies in a mouse model (Table 1). Mice were treated with the antibodies twice, 1 day prior to and 2 days after a challenge with the mouse-adapted Ebola virus strain (1). All mice treated with either MAb 133/3.16 or 226/8.1 were protected from a lethal infection without disease signs, while untreated mice and those treated with MAb 42/3.7, which lacks virus-neutralizing activity, lost weight and died by day 8 postchallenge.
TABLE 1.
Protection conferred by passive immunization of mice with neutralizing antibodiesa
| Antibody | No. of survivors/total |
|---|---|
| 133/3.16 | 6/6 |
| 226/8.1 | 6/6 |
| 42/3.7b | 0/5 |
| None | 0/7 |
Each mouse was intraperitoneally inoculated with 250 μg of the indicated antibody 1 day before and 2 days after an intraperitoneal challenge with 30 50% lethal doses of Ebola virus.
This antibody reacts with the GPs of all Ebola virus species but does not neutralize virus infectivity in vitro.
Identification of neutralizing epitopes with chimeric GPs.
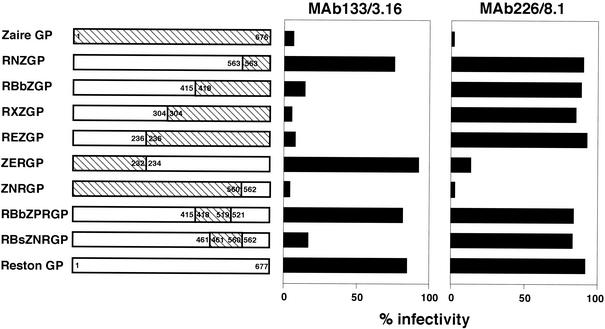
To identify GP regions involved in neutralization by these MAbs, we first generated a series of chimeric proteins with GPs from the Zaire and Reston species (Fig. 4). MAb 133/3.16 neutralized the infectivity of VSV pseudotyped with RBbZGP (Reston, positions 1 to 415; Zaire, positions 418 to 676), RXZGP (Reston, positions 1 to 304; Zaire, positions 304 to 676), REZGP (Reston, positions 1 to 236; Zaire, positions 236 to 676), ZNRGP (Zaire, positions 1 to 560; Reston, positions 562 to 677), and RBsZNRGP (Reston, positions 1 to 461 and 562 to 677; Zaire, positions 461 to 560) but not others, suggesting that this antibody recognizes a region in amino acid positions 521 to 560 of Zaire GP. By contrast, MAb 226/8.1 bound to a different region (positions 1 to 232) of Zaire GP, as indicated by the neutralization of infectivity of the virus with ZERGP (Zaire, positions 1 to 232; Reston, positions 234 to 677) or ZNRGP (Zaire, positions 1 to 560; Reston, positions 562 to 677), but not those with the other chimeric GPs. Since all three previously identified neutralizing epitopes are located in the region of amino acid positions 389 to 493 (21), these results suggested the existence of two other neutralizing epitopes on GP.
FIG. 4.
Identification of GP regions containing B-cell epitopes by use of VSV pseudotyped with chimeric GPs. The numbers inside the bars are the amino acid positions of GP of Ebola virus species Zaire and Reston. All of the chimeric GPs were functional and complemented infectivity of VSVΔG*. For neutralization tests, viruses were incubated with appropriately diluted mouse ascites (50 μg of specific antibodies/ml) and inoculated onto 293 cells. The relative percentage of infected cells was determined by setting the number of infected cells in the presence of normal mouse ascites (approximately 50 to 100 GFP-positive cells per microscopic field) at 100. Experiments were done three times, and representative data are shown.
Identification of neutralizing epitopes with a recombinant VSV containing the Ebola virus GP-encoding gene.
To conclusively determine the neutralizing epitopes for these antibodies, we sought to obtain antigenic variants that escape from neutralization by the antibodies. We generated a recombinant VSV containing the Ebola virus GP-encoding gene instead of the VSV G protein-encoding gene (chimeric VSV-EbolaGP) (Fig. 1B). The properties of this virus will be described in detail elsewhere. This virus expresses Ebola virus GP in the context of the VSV genome, utilizes Ebola virus GP for entry into cells, and grows rapidly in cell culture (107 to 108 PFU/ml in 2 to 3 days), as is the case with wild-type VSV. Thus, this VSV-EbolaGP chimera is useful for rapid selection of antigenic variants from GP-encoding gene pools in the VSV genome.
Chimeric VSV-EbolaGP was grown in the presence of either MAb 133/3.16 or 226/8.1, and antigenic variants that escaped from neutralization were isolated 3 days after infection. We biologically cloned three variants for each antibody as described in Materials and Methods. The frequencies of isolation of the antigenic variants from the parent virus were 10−5.25 and 10−4.75 with MAbs 133/16.3 and 226/8.1, respectively.
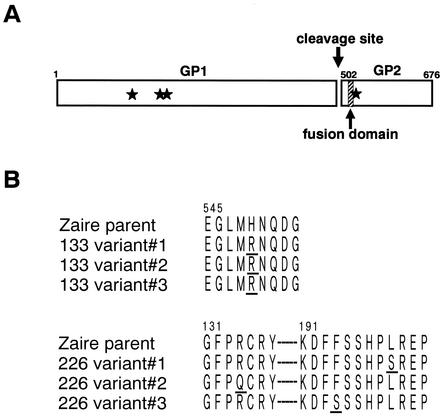
Sequence analysis of these variants' GPs revealed that each variant had a single amino acid change in the GP (Fig. 5). All three variants selected with MAb 133/3.16 had the same His-to-Arg substitution at position 549 in GP2, which is adjacent to the fusion domain (10 amino acids downstream) of GP2 (Fig. 5A). By contrast, MAb 226/8.1 selected three variants with different amino acid substitutions: Leu at position 199, Phe at position 194, or Arg at position 134 in GP1 was replaced with Ser, Ser, or Gln, respectively, suggesting that MAb 226/8.1 recognized a conformational epitope on the GP molecule. Consistent with this finding, this antibody did not react to GP in an immunoblot assay (data not shown). All amino acid substitutions were located in the regions predicted by the use of VSV pseudotyped with chimeric proteins (Fig. 4). However, neither antibody bound to synthetic peptides containing the GP regions identified by the neutralization assay.
FIG. 5.
(A) Schematic diagram of Ebola virus GP. Ebola virus GP is proteolytically cleaved into GP1 and GP2 subunits (20). The fusion domain, a highly conserved hydrophobic region (amino acids 524 to 539), is located 24 amino acids downstream of the N terminus of the GP2 subunit. Stars represent the positions of amino acid substitutions. (B) Amino acid substitutions found in escape mutants selected by MAbs 133/3.16 (133 variants 1 to 3) and 226/8.1 (226 variants 1 to 3). Substituted amino acids are underlined.
DISCUSSION
To identify B-cell epitopes for neutralization of Ebola virus, we used a recombinant VSV containing the Ebola virus GP-encoding gene in place of the VSV G protein-encoding gene. This chimeric virus utilizes Ebola virus GP for cell entry, relying on VSV genes and proteins for replication and transcription of its genome and for viral protein synthesis. It therefore grows rapidly in cell culture, comparably to wild-type VSV. Consequently, this virus can be used to select GP antigenic variants more efficiently than wild-type Ebola virus, which does not grow in cultured cells as rapidly as VSV (taking a week to develop complete cytopathic effects). Hence, this chimeric VSV system should be useful for selecting antigenic variants from glycoproteins of viruses incapable of being cultured satisfactorily in vitro.
Since GP and sGP share approximately 300 N-terminal amino acids, they possess several epitopes in common (12, 18). In fact, sGP adsorbs neutralizing antibodies in anti-Zaire GP serum (4). Since sGP is detected at a high concentration in the blood of acutely infected patients (11, 12), neutralizing antibodies that do not react to sGP would be more effective for treatment of Ebola virus infection than those reacting to this molecule. In accord with this concept, neutralizing antibodies reacting with GP but not with sGP were reported to protect mice from lethal Ebola virus infection (21). We have identified single amino acid residues in two other neutralizing epitopes, and neither of the antibodies used in this study bound to sGP in an ELISA (data not shown). Interestingly, MAb 226/8.1 did not bind to sGP even though Leu at position 199, Phe at position 194, and Arg at position 134 are shared by GP and sGP. Since Ebola virus GP and sGP are composed of trimers of GP1-GP2 and antiparallel-orientated homodimers, respectively (13, 19), different oligomerization forms likely affect the tertiary structure of the conformational epitope. It is also conceivable that this epitope is not present on sGP monomers or may reside inside sGP dimers.
Including the two identified in this study, five different neutralizing epitopes on GP of Ebola virus species Zaire have been reported so far. Neither of the MAbs used in this study neutralized the infectivity of VSV pseudotyped with GPs from the Sudan, Ivory Coast, and Reston species. It seems that there are few cross-neutralizing epitopes among Ebola virus species (15). This antigenic difference must be considered for both passive prophylaxis and vaccination for Ebola virus infection. The use of neutralizing antibody cocktails, ideally cross-reactive among different Ebola virus species, should increase the protective effects of the treatments and reduce the possibility of the emergence of antigenic variants in the infected individuals.
Acknowledgments
We thank Daryl Dick, Michael Garbutt, and Krisna Wells for excellent technical assistance and John Gilbert for editing the manuscript.
This work was supported by a Grant-in-Aid for Scientific Research on Priority Areas from the Ministries of Education, Culture, Sports, Science, and Technology, Japan, to A.T., in part by a Japan Health Sciences Foundation grant to A.T., by National Institute of Allergy and Infectious Diseases Public Health Service research grants to Y.K., by CREST (Japan Science and Technology Corporation) (A.T. and Y.K.), and by a research grant from the Canadian Institutes of Health Research to H.F. (MOP-43921).
REFERENCES
- 1.Bray, M., K. Davis, T. Geisbert, C. Schmaljohn, and J. Huggins. 1998. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J. Infect. Dis. 178:651-661. [DOI] [PubMed] [Google Scholar]
- 2.Feldmann, H., and M. P. Kiley. 1999. Classification, structure, and replication of filoviruses. Curr. Top. Microbiol. Immunol. 235:1-22. [DOI] [PubMed] [Google Scholar]
- 3.Gupta, M., S. Mahanty, M. Bray, R. Ahmed, and P. E. Rollin. 2001. Passive transfer of antibodies protects immunocompetent and immunodeficient mice against lethal Ebola virus infection without complete inhibition of viral replication. J. Virol. 75:4649-4654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ito, H., S. Watanabe, A. Takada, and Y. Kawaoka. 2001. Ebola virus glycoprotein: proteolytic processing, acylation, cell tropism, and detection of neutralizing antibodies. J. Virol. 75:1576-1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jahrling, P. B., T. W. Geisbert, J. B. Geisbert, J. R. Swearengen, M. Bray, N. K. Jaax, J. W. Huggins, J. W. LeDuc, and C. J. Peters. 1999. Evaluation of immune globulin and recombinant interferon-alpha2b for treatment of experimental Ebola virus infections. J. Infect. Dis. 179(Suppl. 1):S224-S234. [DOI] [PubMed] [Google Scholar]
- 6.Jahrling, P. B., J. Geisbert, J. R. Swearengen, G. P. Jaax, T. Lewis, J. W. Huggins, J. J. Schmidt, J. W. LeDuc, and C. J. Peters. 1996. Passive immunization of Ebola virus-infected cynomolgus monkeys with immunoglobulin from hyperimmune horses. Arch. Virol. Suppl. 11:135-140. [DOI] [PubMed] [Google Scholar]
- 7.Jasenosky, L. D., G. Neumann, I. Lukashevich, and Y. Kawaoka. 2001. Ebola virus VP40-induced particle formation and association with the lipid bilayer. J. Virol. 75:5205-5214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kudoyarova-Zubavichene, N. M., N. N. Sergeyev, A. A. Chepurnov, and S. V. Netesov. 1999. Preparation and use of hyperimmune serum for prophylaxis and therapy of Ebola virus infections. J. Infect. Dis. 179(Suppl. 1):S218-S223. [DOI] [PubMed] [Google Scholar]
- 9.Mupapa, K., M. Massamba, K. Kibadi, K. Kuvula, A. Bwaka, M. Kipasa, R. Colebunders, J. J. Muyembe-Tamfum, et al. 1999. Treatment of Ebola hemorrhagic fever with blood transfusions from convalescent patients. J. Infect. Dis. 179(Suppl. 1):S18-S23. [DOI] [PubMed] [Google Scholar]
- 10.Peters, C. J., and A. S. Khan. 1999. Filovirus diseases. Curr. Top. Microbiol. Immunol. 235:85-95. [DOI] [PubMed] [Google Scholar]
- 11.Sanchez, A., A. S. Khan, S. R. Zaki, G. J. Nabel, T. G. Ksiazek, and C. J. Peters. 2001. Filoviridae: Marburg and Ebola viruses, p. 1279-1304. In D. M. Knipe and P. M. Howley (ed.), Fields virology, 4th ed. Lippincott Williams & Wilkins, Philadelphia, Pa.
- 12.Sanchez, A., S. G. Trappier, B. W. Mahy, C. J. Peters, and S. T. Nichol. 1996. The virion glycoproteins of Ebola viruses are encoded in two reading frames and are expressed through transcriptional editing. Proc. Natl. Acad. Sci. USA 93:3602-3607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sanchez, A., Z. Y. Yang, L. Xu, G. J. Nabel, T. Crews, and C. J. Peters. 1998. Biochemical analysis of the secreted and virion glycoproteins of Ebola virus. J. Virol. 72:6442-6447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schnell, M. J., L. Buonocore, E. Kretzschmar, E. Johnson, and J. K. Rose. 1996. Foreign glycoproteins expressed from recombinant vesicular stomatitis viruses are incorporated efficiently into virus particles. Proc. Natl. Acad. Sci. USA 93:11359-11365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Takada, A., and Y. Kawaoka. 2001. The pathogenesis of Ebola hemorrhagic fever. Trends Microbiol. 9:506-511. [DOI] [PubMed] [Google Scholar]
- 16.Takada, A., C. Robison, H. Goto, A. Sanchez, K. G. Murti, M. A. Whitt, and Y. Kawaoka. 1997. A system for functional analysis of Ebola virus glycoprotein. Proc. Natl. Acad. Sci. USA 94:14764-14769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Takada, A., S. Watanabe, K. Okazaki, H. Kida, and Y. Kawaoka. 2001. Infectivity-enhancing antibodies to Ebola virus glycoprotein. J. Virol. 75:2324-2330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Volchkov, V. E., S. Becker, V. A. Volchkova, V. A. Ternovoj, A. N. Kotov, S. V. Netesov, and H.-D. Klenk. 1995. GP mRNA of Ebola virus is edited by the Ebola virus polymerase and by T7 and vaccinia virus polymerases. Virology 214:421-430. [DOI] [PubMed] [Google Scholar]
- 19.Volchkova, V. A., H. Feldmann, H.-D. Klenk, and V. E. Volchkov. 1998. The nonstructural small glycoprotein sGP of Ebola virus is secreted as an antiparallel-orientated homodimer. Virology 250:408-414. [DOI] [PubMed] [Google Scholar]
- 20.Volchkov, V. E., H. Feldmann, V. A. Volchkova, and H.-D. Klenk. 1998. Processing of the Ebola virus glycoprotein by the proprotein convertase furin. Proc. Natl. Acad. Sci. USA 95:5762-5767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilson, J. A., M. Hevey, R. Bakken, S. Guest, M. Bray, A. L. Schmaljohn, and M. K. Hart. 2000. Epitopes involved in antibody-mediated protection from Ebola virus. Science 287:1664-1666. [DOI] [PubMed] [Google Scholar]
- 22.Wool-Lewis, R. J., and P. Bates. 1998. Characterization of Ebola virus entry by using pseudotyped viruses: identification of receptor-deficient cell lines. J. Virol. 72:3155-3160. [DOI] [PMC free article] [PubMed] [Google Scholar]