Abstract
The Kansas strain of bovine parainfluenza virus type 3 (BPIV3) is 100- to 1,000-fold restricted in replication in the respiratory tracts of nonhuman primates compared to human PIV3 (HPIV3), an important pathogen of infants and young children. BPIV3 is also restricted in replication in human infants and children, yet it is immunogenic and is currently being evaluated in clinical trials as a vaccine candidate to protect against illness caused by HPIV3. We have examined the genetic basis for the host range attenuation phenotype of BPIV3 by exchanging each open reading frame (ORF) of a recombinant wild-type HPIV3 with the analogous ORF from BPIV3, with the caveats that the multiple ORFs of the P gene were exchanged as a single unit and that the HN and F genes were exchanged as a single unit. Recombinant chimeric bovine-human PIV3s were recovered from cDNA, and the levels of viral replication in vitro and in the respiratory tract of rhesus monkeys were determined. Recombinant chimeric HPIV3s bearing the BPIV3 N or P ORF were highly attenuated in the upper and lower respiratory tracts of monkeys, whereas those bearing the BPIV3 M or L ORF or the F and HN genes were only moderately attenuated. This indicates that the genetic determinants of the host range restriction of replication of BPIV3 for primates are polygenic, with the major determinants being the N and P ORFs. Monkeys immunized with these bovine-human chimeric viruses, including the more highly attenuated ones, developed higher levels of HPIV3 hemagglutination-inhibiting serum antibodies than did monkeys immunized with BPIV3 and were protected from challenge with wild-type HPIV3. Furthermore, host range determinants could be combined with attenuating point mutations to achieve an increased level of attenuation. Thus, chimeric recombinant bovine-human PIV3 viruses that manifest different levels of attenuation in rhesus monkeys are available for evaluation as vaccine candidates to protect infants from the severe lower respiratory tract disease caused by HPIV3.
Human parainfluenza virus type 3 (HPIV3) and its animal counterpart, bovine PIV3 (BPIV3), are enveloped, nonsegmented negative-strand RNA viruses of the genus Respirovirus in the family Paramyxoviridae (4, 26). HPIV3 is a common cause of respiratory disease in infants (8, 28), and presently a licensed vaccine is not available. HPIV3 and BPIV3 share a moderate to high level of nucleotide and amino acid sequence identity (2) and are 25% antigenically related by cross-neutralization studies (6). The Kansas strain of BPIV3 is restricted in replication in the respiratory tracts of humans and nonhuman primates (6, 23) and is being evaluated as a candidate vaccine to prevent the severe lower respiratory tract disease caused by infection of infants and young children with HPIV3 (22-24, 27).
BPIV3 and HPIV3 have the same genome organization (4), encoding nine proteins from six contiguous genes. These nine proteins include the three nucleocapsid-associated proteins, the nucleoprotein (N), the phosphoprotein (P) and the large polymerase protein (L), which form the nucleocapsid complex and the associated polymerase; an internal matrix protein (M); and the fusion (F) and hemagglutinin-neuraminidase (HN) envelope glycoproteins. The P gene also encodes three additional polypeptides by use of an alternative reading frame for the accessory protein C or by pseudotemplated nucleotide insertion (RNA editing) for the generation of the accessory V and D polypeptides. By analogy to other parainfluenza viruses, one or more of the HPIV3 accessory proteins might be involved in regulation of viral RNA synthesis and function as antagonists of the host antiviral interferon response (15).
While the cis-acting transcription and replication control regions are highly conserved between the two viruses, the amino acid sequence identities between homologous proteins of the two viruses range from approximately 59% for the P protein to 90% for the M protein (2). Thus, the host range determinants of the attenuation phenotype of BPIV3 for primates are likely encoded by one or more of the BPIV3 open reading frames (ORFs) rather than the highly conserved cis-acting regulatory sequences. Previously, the N ORF of BPIV3 was shown to confer a high level of attenuation when substituted for the analogous ORF in HPIV3 (1), and the BPIV3 F and HN genes were shown to confer a moderate level of attenuation when substituted for their F and HN counterparts in HPIV3 (34). In the present study, we have extended these observations to show that the P and, to a lesser extent, the M and L ORFs can also confer attenuation when substituted for the homologous HPIV3 ORF in the HPIV3 genome, demonstrating that the host range attenuation phenotype of BPIV3 is polygenic.
MATERIALS AND METHODS
Cell lines and viruses.
Human HEp-2 (ATCC CCL 23) and simian LLC-MK2 (ATCC CCL 7.1) cells were maintained in OptiMEM I (Life Technologies, Gaithersburg, Md.) supplemented with 5% fetal bovine serum and gentamicin sulfate (50 μg/ml). The generation and characterization of the recombinant JS strain (GenBank accession no. Z11575) of wild-type HPIV3 (rHPIV3), its attenuated derivative containing the temperature-sensitive (ts) and attenuating mutations of the cold-passaged HPIV3cp45 candidate vaccine virus (rHPIV3cp45), and the Kansas strain of BPIV3 were described previously (12, 34, 35). The PIV3s were propagated, and their titers were determined in LLC-MK2 cells as described previously (12, 20, 35); titers are expressed as 50% tissue culture infectious doses (TCID50) per milliliter. The biologically derived RSV A2 strain was grown in HEp-2 cells and was quantified by plaque assay as described previously (10).
Construction of infectious cDNAs of HPIV3 bearing ORF substitutions.
Unique restriction sites were introduced by PCR or site-directed mutagenesis at the translation initiation and termination codons of the cDNAs for the BPIV3 and HPIV3 N, P, M, or L ORFs. The ORF of each construct was exchanged via the introduced unique restriction sites by using standard molecular cloning techniques. Where necessary, the position of the unique restriction site following the stop codon of the ORF was adjusted so that the number of nucleotides (nt) following the stop codon that were transferred along with the ORF maintained each chimeric genome length as a multiple of six (25). Following the ORF substitution, the nucleotide sequence around the start of each ORF was further modified such that the substituted ORF sequence and the sequence upstream of the ORF was changed back to be that of each respective wild-type parent. The introduced unique restriction site following the end of the ORF was not further modified. The N ORF exchange had been previously described (1). The F and HN genes were substituted as a single restriction fragment by using unique restriction sites that had been introduced into the M and HN downstream noncoding regions, respectively (34).
Recovery of viruses from cDNA and sequencing of viral RNA (vRNA).
rHPIV3 was recovered from each full-length HPIV3 antigenomic cDNA bearing a BPIV3 ORF substitution (Fig. 1) from HEp-2 cells by cotransfection with PIV3 support plasmids and by coinfection with the MVA-T7 vaccinia virus recombinant (the generous gift of Linda Wyatt and Bernie Moss), as described previously (12, 34). rHPIV3s were biologically cloned by plaque purification on LLC-MK2 monolayers and were further propagated on LLC-MK2 cells, as previously described (36).
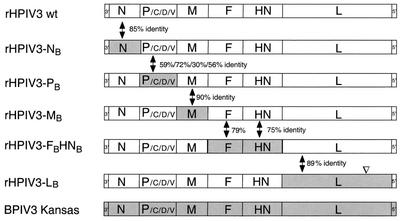
FIG. 1.
Schematic diagram (not to scale) of the genome structures of recombinant HPIV3s with BPIV3 ORF substitutions and of their parental HPIV3 wild-type and BPIV3 Kansas viruses. BPIV3 sequences are indicated by the shaded areas (░⃞), and HPIV3 sequences are indicated by the clear areas (□). The percent amino acid identity for the D and V proteins is provided for the portion of the D and V protein sequence that is present downstream of the P gene editing site and is represented in both viruses (2). ▿, relative position of the T1711I point mutation in rHPIV3-LBT1711I.
To confirm the identity and structure of each chimeric recombinant, vRNA was isolated from each biologically cloned virus as described previously (36) and was used as the template for reverse transcription-PCR (RT-PCR) to amplify the region of interest. Thus, an RT-PCR fragment containing the substituted ORF flanked by the backbone HPIV3 sequence was generated, and the amplified product was analyzed by restriction endonuclease digestion and DNA sequencing to confirm its structure (36).
Replication of rHPIV3s in vitro.
Multicycle growth kinetics of wild-type and chimeric rHPIV3s were determined in LLC-MK2 cells. Each virus tested was inoculated in triplicate into LLC-MK2 monolayers in six-well plates at a multiplicity of infection (MOI) of 0.01, and the cultures were incubated at 32°C. Medium (0.5 ml) from each well was harvested and replaced with 0.5 ml of fresh medium at 0 h and at 24-h intervals thereafter for 5 days postinfection. For determination of temperature sensitivity of replication in vitro, the virus titers (TCID50/ml) at 32°C and at graded temperatures from 35 to 40°C were determined by titration on LLC-MK2 monolayer cultures as described above.
Primate studies.
Rhesus monkeys (Macaca mulatta) that were negative for serum hemagglutination-inhibiting (HAI) antibody to HPIV3 were inoculated simultaneously by the intranasal (i.n.) and intratracheal (i.t.) routes with 1 ml per site of L15 medium containing 105 TCID50 of virus, as described previously (1, 34). Nasopharyngeal (NP) swab samples were collected on days 1 through 10 postinfection, and tracheal lavage (TL) samples were collected on days 2, 4, 6, 8, and 10 postinfection. Virus present in the NP and TL specimens was quantified by titration on LLC-MK2 cell monolayers at 32°C, as previously described (1, 34), and the mean peak virus titer obtained was expressed as log10 TCID50/ml. Rhesus monkeys were challenged i.n. and i.t. at 1 ml per site with medium containing 106 TCID50 of the wild-type JS strain of HPIV3 at 28 or 31 days after immunization, and NP and TL samples were collected on days 2, 4, 6, and 8 postchallenge. HPIV3 present in the samples was quantified as described above. Serum samples were taken preimmunization (day 0), postimmunization (day 28 or 31) and postchallenge (day 56 or 59) and assayed to determine the HAI antibody titer to HPIV3, as described previously (11, 39). For some groups, the data presented includes data collected from two previous studies (1, 34). Groups of animals in the present and previous studies were infected with identical virus preparations, and the samples were collected and quantitated by using similar procedures.
RESULTS
Recovery of rHPIV3s with BPIV3 ORF substitutions.
The Kansas strain of BPIV3 is restricted in replication in the respiratory tracts of humans and other primates. To identify the genetic determinants of the host range attenuation phenotype of BPIV3 in primates, the antigenomic cDNA of HPIV3 was modified to contain the N, P, M, or L ORF of BPIV3 in place of the analogous HPIV3 ORF (Fig. 1). In addition, the F and HN genes were transferred together as a pair to replace their HPIV3 counterparts, as described previously (34).
Each of the chimeric bovine-human PIV3s containing the N, P, M, F and HN, or L ORFs (Fig. 1) was recovered from cDNA. Two of these were previously described, namely, rHPIV3-FBHNB (34) and cKa-N (referred to here as rHPIV3-NB) (1). The recombinant chimeric viruses were biologically cloned by plaque isolation, and vRNA was isolated from the cloned virus and was used as a template to generate RT-PCR products. The structure of the genome flanking the substituted ORF was confirmed for each recombinant virus by sequencing and restriction enzyme analysis.
Two recombinant viruses, rHPIV3-LBT1711I and rHPIV3-LB (Fig. 1), bearing the BPIV3 L ORF were generated. rHPIV3-LBT1711I was generated first, but after it was found to be highly temperature sensitive in its replication in vitro (see below), it was sequenced and was found to contain two point mutations in the L ORF that resulted in an Ala-425-to-Val (A425V) and a Thr-1711-to-Ile substitution (T1711I). The latter mutation was present in the antigenomic cDNA, but the former was a spontaneous mutation occurring following transfection of this cDNA. Another recombinant was generated (rHPIV3-LB) that had the authentic BPIV3 L ORF sequence.
The ability to recover each of the chimeric recombinant bovine-human viruses indicates a substantial degree of compatibility of the substituted BPIV3 proteins with the HPIV3 proteins as well as with the cis-acting sequences of the HPIV3 genome.
Replication of chimeric rHPIV3s in vitro.
For each chimeric virus, the possibility existed that the substituted BPIV3 protein might not be fully compatible with the encoded proteins and cis-acting sequences of the HPIV3 backbone. If such a partial incompatibility exists, it should be manifested by a decrease in the replication of the chimeric virus in a cell line such as LLC-MK2, which is permissive for both parent viruses.
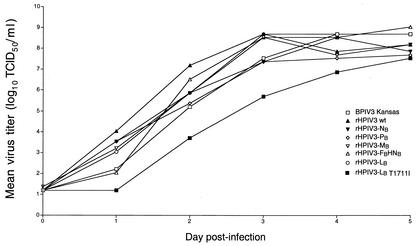
Therefore, the kinetics of replication of each chimeric rHPIV3 in vitro was compared to that of their wild-type rHPIV3 and BPIV3 parent viruses by infecting LLC-MK2 cells at an MOI of 0.01 and measuring virus yield at 24-h intervals. Except for rHPIV3-LBT1711I, all of the chimeric rHPIV3s bearing BPIV3 ORF substitutions grew at a rate similar to that of their parent viruses (Fig. 2), and all of the chimeric viruses grew to over 107 TCID50/ml by day 5 postinfection. This confirmed that each of the substituted wild-type BPIV3 proteins exhibited a high degree of compatibility with the proteins and cis-acting signals of the HPIV3 backbone. In contrast, the restricted replication of rHPIV3-LB T1711I in vitro indicates that one or both of the amino acid substitutions in its BPIV3 L polymerase protein are attenuating in vitro.
FIG. 2.
Multistep growth curves of chimeric rHPIV3s. LLC-MK2 monolayers were infected in triplicate with the indicated PIV3 at an MOI of 0.01 and incubated at 32°C. Aliquots of the medium supernatants were harvested at 24-h intervals, and the virus titer was quantified on LLC-MK2 monolayers at 32°C.
Replication of chimeric viruses at permissive and restrictive temperatures.
It was possible that one or more of the substituted BPIV3 proteins might have a marginal incompatibility with a protein in the HPIV3 backbone that was not detectable at 32°C but that might become evident at elevated temperatures. It also was of interest to further characterize the restricted replication exhibited by the mutant rHPIV3-LB T1711I virus (Fig. 2). To determine if the ORF substitutions in each rHPIV3 altered the ability of these viruses to grow at elevated temperatures, the level of temperature sensitivity of replication of each chimeric rHPIV3 was compared to that of the parent viruses and to that of rHPIV3cp45, which is a well characterized ts and attenuated candidate HPIV3 vaccine that was previously shown to be appropriately attenuated and immunogenic in humans and nonhuman primates (19, 20, 24). The wild-type and chimeric rHPIV3s were evaluated for their abilities to grow on LLC-MK2 cells at the permissive temperature of 32°C and at a range of higher temperatures (Table 1). Surprisingly, both rHPIV3-LB and rHPIV3-LB T1711I were highly ts, with rHPIV3-LB T1711I being more ts than either rHPIV3-LB or rHPIV3cp45. As noted above, the BPIV3 L ORF present in the rHPIV3-LB T1711I virus contained two amino acid coding changes relative to wild-type BPIV3, and it was of interest to determine which one, or both, was responsible for the increased ts phenotype of rHPIV3-LB T1711I compared to rHPIV3-LB. An alternative viral clone of rHPIV3-LB T1711I was identified that contained the T1711I substitution but not the A425V mutation. This virus had the same shutoff temperature as rHPIV3-LB T1711I (data not shown), indicating that the T1711I mutation alone is responsible for the increased level of temperature sensitivity of rHPIV3-LB T1711I.
TABLE 1.
Replication of chimeric bovine-human PIV3s at permissive and restrictive temperaturesa
| Virus | Mean titer (log10TCID50/ml) at 32°C | Mean log10 reduction in virus titer at the indicated temperature (°C) |
|||||
|---|---|---|---|---|---|---|---|
| 35 | 36 | 37 | 38 | 39 | 40 | ||
| BPIV3 Kansas | 8.7 | 0.0 | 0.1 | 0.2 | 0.8 | 1.1 | 1.3 |
| rHPIV3 wt | 8.6 | 0.3 | −0.2 | 0.1 | 0.3 | 0.4 | 0.5 |
| rHPIV3-NB | 8.5 | —b | — | — | 0.5 | 0.5 | 0.4 |
| rHPIV3-PB | 7.8 | — | — | — | 1.0 | 1.2 | 1.3 |
| rHPIV3-MB | 8.0 | — | — | — | 0.4 | 1.5 | 2.1 |
| rHPIV3-FBHNB | 8.2 | — | — | — | 0.5 | 0.6 | 0.7 |
| rHPIV3-LB | 8.0 | 0.0 | 0.4 | 1.5 | 3.7 | 4.6 | 4.1 |
| rHPIV3-LB(T1711I) | 7.0 | 1.6 | 1.4 | 4.2 | ≥5.3 | ≥5.6 | ≥5.7 |
| rHPIV3 cp45 | 7.8 | 0.9 | 1.3 | 2.2 | 3.0 | ≥6.4 | ≥6.4 |
Data are the means of results of two or more titrations. Values in bold type are at or above the shutoff temperature, which is defined as a 100-fold or greater reduction in titer compared to the titer at 32°C after adjusting for the reduction in replication of the rHPIV3 wild-type control virus. rHPIV3cp45 is included as a well-characterized ts control virus.
—, Data not gathered.
Introduction of a BPIV3 ORF into wild-type HPIV3 can attenuate rHPIV3 for rhesus monkeys.
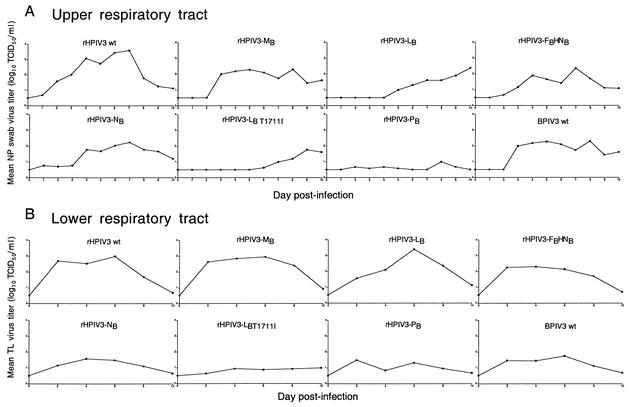
To determine the effect of each ORF or gene substitution on the ability of the chimeric rHPIV3 to replicate in the upper and lower respiratory tracts of rhesus monkeys, each chimeric virus was administered i.n. and i.t. to rhesus monkeys at a dose of 105 TCID50 per site. The levels of replication of the chimeric viruses was compared to those of the wild-type rHPIV3 and BPIV3 parental viruses. The kinetics of replication for each virus was determined in the upper and lower respiratory tracts of rhesus monkeys over a 10-day period (Fig. 3). This was expressed as the mean peak titer, which gives an indication of the peak titer of virus shedding, and as the mean of the sum of the daily titers, which gives a comparison of the virus load over the 10-day period (Table 2). The mean sums of the titers are generally higher in the NP specimens than in the TL specimens, since the NP specimens were collected daily whereas the TL specimens were collected only every other day.
FIG. 3.
Mean daily virus titers for chimeric rHPIV3s with BPIV3 ORF substitutions. Mean daily NP swab (A) and TL (B) virus titers for each group of monkeys infected with a parental or a chimeric HPIV3 are shown for the course of the infection. The number of monkeys per group is shown in Table 2. Mean virus titers were calculated for each group for each day. Some data are from previous animal studies (1, 34) (Table 2).
TABLE 2.
Levels of replication, immunogenicity, and efficacy of chimeric bovine-human PIV3s in rhesus monkeys
| Immunizing virusa | Group sizeb | Mean peak PIV3 titer (log10 TCID50/ml ± SE)c |
Mean of sum of daily titers (log10 TCID50/ml ± SE)d |
Postimmuni- zation serum HPIV3 HAI antibody titere | Mean peak challenge HPIV3 titer (log10 TCID50/ml) tof: |
Postchallenge serum HPIV3 HAI antibodyg |
||||
|---|---|---|---|---|---|---|---|---|---|---|
| NP | TL | NP | TL | NP | TL | Titer | Group size | |||
| rHPIV3 wt | 12 | 4.2 ± 0.4 | 3.5 ± 0.3 | 21.2 ± 1.7 A | 10.5 ± 1.1 | 8.6 ± 0.4 | 1.4 ± 0.3 | 1.1 ± 0.2 | 11.5 ± 0.3 | 6 |
| rHPIV3-LB | 4 | 3.0 ± 0.8 | 3.5 ± 0.2 | 11.8 ± 2.4 B, C, D | 10.5 ± 1.0 | 10.3 ± 0.5 | 0.9 ± 0.2 | 1.5 ± 0.1 | 10.8 ± 0.6 | 4 |
| rHPIV3-MB | 4 | 3.0 ± 0.6 | 3.4 ± 0.6 | 16.6 ± 3.7 A, B | 11.8 ± 2.3 | 7.8 ± 0.9 | 1.4 ± 0.9 | 1.2 ± 0.4 | 11.0 ± 0.4 | 4 |
| rHPIV3-FB HNB | 6 | 2.7 ± 0.2 | 2.7 ± 0.4 | 13.5 ± 0.9 B, C | 9.1 ± 2.1 | 4.7 ± 0.6 | 2.6 ± 0.2 | 1.8 ± 0.5 | 11.0 ± 0.0 | 4 |
| rHPIV3-NB | 8 | 2.6 ± 0.6 | 2.0 ± 0.4 | 14.5 ± 2.7 B | 6.0 ± 1.2 | 7.5 ± 0.4 | 2.1 ± 0.4 | 1.2 ± 0.2 | 10.0 ± 0.0 | 2 |
| rHPIV3-LBT1711I | 8 | 2.2 ± 0.2 | 1.4 ± 0.2 | 8.7 ± 0.3 C, D | 4.4 ± 0.6 | 9.8 ± 0.3 | 0.9 ± 0.1 | 1.6 ± 0.1 | 10.8 ± 0.5 | 4 |
| rHPIV3-PB | 6 | 1.2 ± 0.2 | 1.5 ± 0.3 | 6.2 ± 0.3 D | 5.3 ± 1.0 | 7.2 ± 0.6 | 2.4 ± 0.5 | 2.2 ± 0.6 | 10.4 ± 0.5 | 4 |
| BPIV3 Kansas | 12 | 2.5 ± 0.2 | 2.1 ± 0.2 | 14.2 ± 1.1 B | 6.4 ± 0.8 | 5.1 ± 0.5 | 2.9 ± 0.2 | 2.0 ± 0.5 | 11.0 ± 0.0 | 2 |
| RSV or none | 4 | NA | NA | NA | NA | <2.0 ± 0.0 | 5.0 ± 0.3 | 5.0 ± 0.3 | 11.5 ± 0.5 | 2 |
Animals were inoculated i.n. and i.t. on day 0 with 105 TCID50 of the indicated virus per site.
Includes data collected from similarly infected and sampled rhesus monkeys from two previous studies (1, 32). The published data included 6 of the 12 rHPIV3 wild-type animals, 2 of the 6 rHPIV3-FB HNB animals, 6 of the 8 rHPIV3-NB animals, and 6 of the 12 BPIV3 animals.
NP swab samples were collected on days 1 to 10 postinfection. TL samples were collected on days 2, 4, 6, 8, and 10 postinfection. Data are the means of the peak virus titer for each animal in its group irrespective of sampling day. The limit of detection of virus titer was 10 TCID50/ml. NA, not applicable.
The sum of the viral titers obtained for each animal on all sampling days was calculated, and a mean ± SE for each group was generated. Data are the means of sum (log10) daily titers for all animals in each group for NP (days 1 to 10) and TL (days 2, 4, 6, 8, and 10) samples. The lower limit of detection is 5.0 for NP swabs and 2.5 for TL samples. Means of sum titers were assigned to similar groups by the Fisher's PLSD test. Mean titers with different letters are statistically significantly different (P < 0.05). Titers indicated with two or three letters are not significantly different from those indicated with either letter.
Postinfection HAI data includes data from animals from the present study and from previous studies (1, 32). Sera were collected 28 to 31 days postinfection and titers were determined in the same assay, with the exception of the sera from groups that received rHPIV3LBT1711I and rHPIV3 LB, in which titers were determined in a second assay along with those in control sera from the first assay. The values obtained with the control sera in the second assay were similar to those obtained in the first assay.
Animals were challenged i.n. and i.t. on day 28 or 31 post-first immunization with 106 TCID50 of the JS strain of HPIV3 wild type per site. NP swab and TL samples were collected on days 2, 4, 6, 8, and 10 postinfection. Virus titrations were performed on LLC-MK2 cells at 32°C. Mean of the peak virus titers ± SE for each animal in its group irrespective of sampling day is shown. The limit of detection of virus titer was 10 TCID50/ml. Results include data from the present study and data from previous studies (1, 32).
Postchallenge antibody titers were obtained 28 days postchallenge for a subset of animals whose numbers are indicated in the last column. This does not include animals from references 1 and 32. The titers in sera from animals in this subset were determined in the same assay, with the exception of sera from the groups that received rHPIV3LB T1711I and rHPIV3 LB, in which titers were determined in a separate assay along with those in control sera from the first assay. The values obtained with the control sera in the second assay were similar to those obtained in the first assay.
Each BPIV3 ORF conferred restriction of replication in the upper or lower respiratory tracts of rhesus monkeys when substituted for the analogous ORF in HPIV3 (Fig. 3), demonstrating that the host range attenuation phenotype of BPIV3 is polygenic. By comparison of the mean peak titers of virus replication in the upper respiratory tract (Table 2), the chimeric rHPIV3s fell into three groups: (i) viruses bearing the BPIV3 M or L ORF or the F and HN genes, whose replication was restricted approximately 16- to 32-fold, (ii) viruses bearing the BPIV3 N or LT1711I ORF, which exhibited 40- to 100-fold restrictions of replication, and (iii) the chimeric HPIV3 with the BPIV3 P ORF substitution, which exhibited a 1,000-fold restriction in replication, suggesting that the BPIV3 P ORF is the major contributor to the attenuation phenotype. The level of replication of rHPIV3-PB was even lower than that of its BPIV3 parent virus in the upper respiratory tract, suggesting that some of its restricted replication in vivo may also be due to a gene incompatibility effect that was not evident in vitro. The pattern was somewhat different in the lower respiratory tract, where the level of attenuation was generally lower. Virus bearing the BPIV3 L gene or the F and HN gene pair was attenuated sixfold or less, while viruses bearing the N, M, or LT1711I gene were attenuated 26- to 32-fold, and virus bearing the BPIV3 P gene was attenuated 100-fold, relative to wild-type rHPIV3 (Table 2). Because rHPIV3-LB T1711I was attenuated for replication in vitro and was highly ts, the level of attenuation of this virus observed in vivo likely is due to a combination of restricted replication specified by host range sequences and that specified by its high level of temperature sensitivity (the body temperature of rhesus monkeys is about 39°C). Interestingly, rHPIV3-MB, rHPIV3-FB HNB, and rHPIV3-LB, which were attenuated for replication in the upper respiratory tract, were not significantly restricted in the lower respiratory tract.
Chimeric rHPIV3s containing BPIV3 ORF substitutions are immunogenic and protect rhesus monkeys from challenge with wild-type HPIV3.
Protection against repeated infection with PIV3 is associated with high levels of antibodies against the major antigenic determinants, the F and HN glycoproteins (9, 29). Although the BPIV3 and HPIV3 F and HN proteins are 75 to 79% identical in amino acid sequence (2), they are only 25% antigenically related (6). To evaluate the immunogenicity of the rHPIV3s, serum samples were collected prior to infection and on day 28 or 31 following infection with the chimeric rHPIV3s or their parent viruses, and the levels of serum HAI antibodies to HPIV3 were determined. Each of the chimeric recombinants bearing the HPIV3 F and HN glycoproteins induced a high level of HAI antibodies to HPIV3, whereas rHPIV3-FBHNB and the BPIV3 parent virus bearing the BPIV3 glycoproteins induced 8- to 16-fold less HAI antibody reactive with the human virus. rHPIV3-LB T1711I, rHPIV3-NB, and rHPIV3-PB replicated approximately 2- to 10-fold less efficiently in the respiratory tracts of rhesus monkeys compared to BPIV3, yet they induced approximately 4- to 32-fold more HPIV3 HAI antibodies, likely because they bear the homologous HPIV3 glycoproteins.
To evaluate the protective efficacy of the chimeric rHPIV3s, monkeys were challenged i.n. and i.t. with 106 TCID50 of wild-type HPIV3 (Table 2). NP and TL samples were collected at 2-day intervals for 10 days postchallenge, and the virus present in the samples was quantified on LLC-MK2 cells. Each of the chimeric recombinants tested afforded a high level of protection against HPIV3 replication, including the highly attenuated rHPIV3-PB and rHPIV3-LB T1711I. Analysis of serum samples collected following the challenge showed that each of the groups developed a similar, high titer of HAI antibodies to HPIV3, indicating that all the monkeys had indeed been infected.
DISCUSSION
BPIV3 is highly restricted in replication in rhesus monkeys and in humans, providing an attenuation phenotype that is being used to develop live vaccines against HPIV3. The present study sought to determine the genetic basis of this attenuation by exchanging each of the HPIV3 ORFs with its corresponding BPIV3 counterpart and examining the effect of this exchange on the replication of each resulting chimeric virus in vitro and in rhesus monkeys. The findings indicated that each of the ORF substitutions attenuated rHPIV3 for rhesus monkeys and that there was a gradient of attenuation specified by the different ORFs. In general, chimeras containing a gene(s) in which the encoded protein is highly conserved between bovine and human PIV3 replicated to higher levels in vivo, whereas chimeras involving a gene(s) in which the encoded protein was less well conserved between bovine and human PIV3 replicated to lower titer.
The chimeric rHPIV3 bearing the BPIV3 P substitution, rHPIV3-PB, was highly attenuated in rhesus monkeys and, indeed, was somewhat more attenuated than the BPIV3 parent virus itself in the upper respiratory tract. Since rHPIV3-PB replicated in vitro as efficiently as its BPIV3 parent and was not ts, it is reasonable to suggest that its restriction of replication in vivo primarily reflects host range differences rather than an incompatibility of bovine and human PIV3 proteins. Thus, it is clear that one or more of the proteins encoded by this gene complex, namely, the P protein itself and the C, D, or V accessory proteins encoded by alternative ORFs, is a major contributor to the overall attenuation of BPIV3 for rhesus monkeys. The P proteins of BPIV3 and HPIV3 share approximately 59% amino acid identity and have the highest number of amino acid differences (247 amino acids) of all of the PIV3 polypeptides. The C, D, and V accessory proteins share approximately 72, 30 and 56% amino acid identity, respectively, which corresponds to 56, 92, and 35 amino acid differences, respectively (2).
One function of the accessory proteins of parainfluenza viruses is to counteract the antiviral effects of the host's interferon system (14, 16, 17). The loss of such anti-interferon genes in negative stranded viruses by functional deletion is often associated with attenuation of replication in vivo (14, 15, 18). The accessory proteins of BPIV3 and HPIV3 have not yet been directly demonstrated to have anti-interferon activities, but the deletion of these genes is attenuating (13), making it likely that one or more of these PIV3 accessory proteins functions as an antagonist of the interferon system. Furthermore, it is possible that one or more of the BPIV3 genes in the P/C/D/V complex has evolved to inhibit the bovine interferon response in a host-specific fashion such that this anti-interferon protein might not function efficiently in primates. Thus, part of the host range attenuation phenotype of the BPIV3 P gene complex might be a consequence of the host specificity of one or more encoded host defense antagonists.
The rHPIV3-NB, rHPIV3-MB, rHPIV3-FBHNB, and rHPIV3-LB chimeric viruses were each attenuated in the upper or lower respiratory tract, suggesting that the N and L genes, the F and HN pair of genes, and to a lesser extent the M gene each possesses host range determinants of attenuation. The observations that the rHPIV3-NB, rHPIV3-MB, rHPIV3-FBHNB, and rHPIV3-LB chimeric viruses are not significantly restricted in replication in vitro suggest that each of the substituted wild-type BPIV3 proteins functioned efficiently in the context of the HPIV3 proteins and cis-acting signals and that the attenuation observed in vivo for each substitution likely is not due to an incompatibility between the BPIV3 and HPIV3 components, but rather represents an authentic host range restriction. This is also suggested by the finding that some of these viruses were restricted for replication in the upper but not the lower respiratory tract. We do note that there was evidence of a possible small effect of incompatibility between the imported BPIV3 L ORF and the HPIV3 genetic background, since the rHPIV3-LB chimera was found to be ts at elevated temperatures in vitro. This likely reflects a reduction in the efficiency of interaction between the BPIV3 L protein and the HPIV3 components at increased, nonphysiologic temperature. Whether this contributes to the attenuation of this chimeric virus in vivo is unknown. The finding that rHPIV3-LB replicates to the same level as wild-type HPIV3 in the warmer lower respiratory tract but is restricted for replication in the cooler upper respiratory tract suggests that temperature sensitivity or viral protein incompatibility does not play a major role in its restriction of replication in primates. The lack of a significant level of attenuation conferred in the lower respiratory tract by the BPIV3 M, L, and F and HN ORFs indicates that the host range restriction specified by these genes may be tissue specific. Clearly, the host range restriction of replication of BPIV3 is polygenic, with the N, P, M, and L genes and the F and HN pair of genes each possessing host range determinants of attenuation. Since the host range restriction of replication of BPIV3 is specified by at least five genes, the attenuation phenotype of this virus should be highly stable phenotypically following replication in humans, and preliminary observations indicate that this is indeed the case (23).
Although the genetic stability of BPIV3 is a desirable characteristic for a live vaccine against HPIV3, the antigenic difference between BPIV3 and HPIV3 would reduce its protective efficacy against HPIV3. This was illustrated in the present study by the lower level of HPIV3-reactive HAI antibodies induced by rHPIV3-FBHNB versus wild-type rHPIV3. Thus, neither BPIV3 nor rHPIV3-FBHNB would be an optimal HPIV3 vaccine candidate, since they bear the major protective antigens of BPIV3 rather than HPIV3. In contrast, each of the other chimeric viruses described here bears the HPIV3 F and HN antigenic determinants combined with host range restriction determinants of BPIV3. Although several of these chimeric HPIV3s (rHPIV3-NB, rHPIV3-PB, and rHPIV3-LBT1711I) were moderately to highly attenuated in vivo, they induced a higher level of serum HAI antibodies than BPIV3 and thus may prove to be useful as candidate vaccines for HPIV3. A chimeric virus, rBPIV3-FHHNH, in which BPIV3 was used as the backbone and its F and HN genes were replaced by those of HPIV3, has also been generated and is being evaluated as a vaccine candidate (21, 34). This vaccine candidate should also be phenotypically stable, since it possesses four of the BPIV3 genes that individually specify restricted replication in primates.
The high level of attenuation of rHPIV3-LB T1711I in rhesus monkeys reflects the additivity of the restriction of replication specified by host range sequences of its L gene and one or both of the T1711I and A425V point mutations. The T1711I mutation was shown to confer the ts phenotype in vitro and thus likely also is responsible for the attenuation phenotype in vivo, although a contribution by the A425V mutation cannot be excluded at this time. Although the individual contributions of these two mutations to attenuation in vivo remain to be defined, the increased attenuation of rHPIV3-LBT1711I versus rHPIV3-LB illustrates that ts and host range determinants of attenuation can be combined to fine-tune the level of attenuation of a candidate vaccine virus.
Several other animal or avian viruses, such as the bovine and rhesus rotaviruses, avian influenza A viruses, bovine respiratory syncytial virus, and vaccinia virus (whose natural host is unknown), have a host range restriction of replication in humans or in nonhuman primates and are considered “Jennerian” vaccine candidates able to protect humans against the respective human pathogens (30). However, not all animal counterparts of a human viral pathogen exhibit a host range attenuation phenotype. For example, Sendai virus is a murine PIV1 that is approximately as similar in amino acid and nucleotide sequence to human PIV1 (HPIV1) as are the bovine and human PIV3s (33). However, Sendai virus replicates to the same level as wild-type HPIV1 in primates (37), indicating that it lacks the host range determinants of attenuation for primates manifested by BPIV3. Thus, a large number of amino acid differences between analogous viral polypeptides does not automatically confer a host range attenuation phenotype.
In the examples where host range attenuation in humans does occur, its genetic basis usually is not well understood and previously had been systematically evaluated only in a single case. An avian influenza A virus was evaluated as a live attenuated vaccine candidate for humans, since it was highly attenuated in nonhuman primates (32). Influenza A reassortant viruses bearing the hemagglutinin and neuraminidase genes of an H3N2 wild-type human virus and the set of six remaining RNA segments from the avian influenza A virus were found to be highly attenuated yet immunogenic in humans (31). Single-gene reassortant analysis showed that the avian influenza A virus NS, M, PB2, and PB1 gene segments each attenuated the wild-type H3N2 influenza A virus for humans (5). Interestingly, the NS1 protein encoded by the NS gene segment of the influenza A virus has been shown to be an interferon antagonist, and viruses lacking it are attenuated in vivo (38), raising the possibility that BPIV3 and the avian influenza A virus are each partially attenuated by functional loss of an interferon antagonist.
The attachment or fusion proteins can also play an important role in host range attenuation of respiratory viruses for primates. For example, receptor specificity has been shown to be a determinant for host range restriction of avian versus human influenza A viruses (7, 40). The host range attenuation phenotype of bovine respiratory syncytial virus, a virus that is highly restricted in replication in our closest animal relative, the chimpanzee, is partially mediated by its attachment G and/or fusion F protein (3). Therefore, it was not surprising to find that the BPIV3 attachment or fusion protein, i.e., the HN or F protein, could contribute to the host range attenuation phenotype of this virus for humans (34).
Thus, the genetic determinants of attenuation of two Jennerian vaccine candidates, BPIV3 in this study and a previously studied avian influenza A virus (5), have been defined for nonhuman primates or humans. In both cases, multiple genes contribute to the host range restriction of replication. This suggests that there may be multiple mechanisms by which this restriction of replication is achieved. This information provides a partial explanation for the safety and phenotypic stability of such viruses for use as vaccines, and sets groundwork for future studies that can specifically address the mechanism by which each of the BPIV3 proteins acts to restrict replication in the primate host.
Acknowledgments
We thank Paul Duprex for a helpful PCR suggestion and Tammy Tobery, Ernest Williams, and Fatimeh Davoodi for technical assistance.
REFERENCES
- 1.Bailly, J. E., J. M. McAuliffe, A. P. Durbin, W. R. Elkins, P. L. Collins, and B. R. Murphy. 2000. A recombinant human parainfluenza virus type 3 (PIV3) in which the nucleocapsid N protein has been replaced by that of bovine PIV3 is attenuated in primates. J. Virol. 74:3188-3195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bailly, J. E., J. M. McAuliffe, M. H. Skiadopoulos, P. L. Collins, and B. R. Murphy. 2000. Sequence determination and molecular analysis of two strains of bovine parainfluenza virus type 3 that are attenuated for primates. Virus Genes 20:173-182. [DOI] [PubMed] [Google Scholar]
- 3.Buchholz, U. J., H. Granzow, K. Schuldt, S. S. Whitehead, B. R. Murphy, and P. L. Collins. 2000. Chimeric bovine respiratory syncytial virus with glycoprotein gene substitutions from human respiratory syncytial virus (HRSV): effects on host range and evaluation as a live-attenuated HRSV vaccine. J. Virol. 74:1187-1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chanock, R. M., B. R. Murphy, and P. L. Collins. 2001. Parainfluenza viruses, p. 1341-1379. In D. M. Knipe, P. M. Howley, D. E. Griffin, R. A. Lamb, M. A. Martin, B. Roizman, and S. E. Straus (ed.), Fields virology, 4th ed., vol. 1. Lippincott Williams & Wilkins, Philadelphia, Pa.
- 5.Clements, M. L., E. K. Subbarao, L. F. Fries, R. A. Karron, W. T. London, and B. R. Murphy. 1992. Use of single-gene reassortant viruses to study the role of avian influenza A virus genes in attenuation of wild-type human influenza A virus for squirrel monkeys and adult human volunteers. J. Clin. Microbiol. 30:655-662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coelingh, K., C. C. Winter, E. L. Tierney, W. T. London, and B. R. Murphy. 1988. Attenuation of bovine parainfluenza virus type 3 in nonhuman primates and its ability to confer immunity to human parainfluenza virus type 3 challenge. J. Infect. Dis. 157:655-662. [DOI] [PubMed] [Google Scholar]
- 7.Connor, R. J., Y. Kawaoka, R. G. Webster, and J. C. Paulson. 1994. Receptor specificity in human, avian, and equine H2 and H3 influenza virus isolates. Virology 205:17-23. [DOI] [PubMed] [Google Scholar]
- 8.Crowe, J. E., Jr. 1995. Current approaches to the development of vaccines against disease caused by respiratory syncytial virus (RSV) and parainfluenza virus (PIV). A meeting report of the WHO Programme for Vaccine Development. Vaccine 13:415-421. [DOI] [PubMed] [Google Scholar]
- 9.Crowe, J. E., Jr. 1998. Immune responses of infants to infection with respiratory viruses and live attenuated respiratory virus candidate vaccines. Vaccine 16:1423-1432. [DOI] [PubMed] [Google Scholar]
- 10.Crowe, J. E., Jr., P. T. Bui, W. T. London, A. R. Davis, P. P. Hung, R. M. Chanock, and B. R. Murphy. 1994. Satisfactorily attenuated and protective mutants derived from a partially attenuated cold-passaged respiratory syncytial virus mutant by introduction of additional attenuating mutations during chemical mutagenesis. Vaccine 12:691-699. [DOI] [PubMed] [Google Scholar]
- 11.Durbin, A. P., W. R. Elkins, and B. R. Murphy. 2000. African green monkeys provide a useful nonhuman primate model for the study of human parainfluenza virus types-1, -2, and -3 infection. Vaccine 18:2462-2469. [DOI] [PubMed] [Google Scholar]
- 12.Durbin, A. P., S. L. Hall, J. W. Siew, S. S. Whitehead, P. L. Collins, and B. R. Murphy. 1997. Recovery of infectious human parainfluenza virus type 3 from cDNA. Virology 235:323-332. [DOI] [PubMed] [Google Scholar]
- 13.Durbin, A. P., J. M. McAuliffe, P. L. Collins, and B. R. Murphy. 1999. Mutations in the C, D, and V open reading frames of human parainfluenza virus type 3 attenuate replication in rodents and primates. Virology 261:319-330. [DOI] [PubMed] [Google Scholar]
- 14.Garcia-Sastre, A. 2001. Inhibition of interferon-mediated antiviral responses by influenza A viruses and other negative-strand RNA viruses. Virology 279:375-384. [DOI] [PubMed] [Google Scholar]
- 15.Garcin, D., J. B. Marq, L. Strahle, P. le Mercier, and D. Kolakofsky. 2002. All four Sendai virus C proteins bind Stat1, but only the larger forms also induce its mono-ubiquitination and degradation. Virology 295:256-265. [DOI] [PubMed] [Google Scholar]
- 16.Goodbourn, S., L. Didcock, and R. E. Randall. 2000. Interferons: cell signalling, immune modulation, antiviral response and virus countermeasures. J. Gen. Virol. 81:2341-2364. [DOI] [PubMed] [Google Scholar]
- 17.Gotoh, B., T. Komatsu, K. Takeuchi, and J. Yokoo. 2001. Paramyxovirus accessory proteins as interferon antagonists. Microbiol. Immunol. 45:787-800. [DOI] [PubMed] [Google Scholar]
- 18.Gotoh, B., K. Takeuchi, T. Komatsu, J. Yokoo, Y. Kimura, A. Kurotani, A. Kato, and Y. Nagai. 1999. Knockout of the Sendai virus C gene eliminates the viral ability to prevent the interferon-alpha/beta-mediated responses. FEBS Lett. 459:205-210. [DOI] [PubMed] [Google Scholar]
- 19.Hall, S. L., C. M. Sarris, E. L. Tierney, W. T. London, and B. R. Murphy. 1993. A cold-adapted mutant of parainfluenza virus type 3 is attenuated and protective in chimpanzees. J. Infect. Dis. 167:958-962. [DOI] [PubMed] [Google Scholar]
- 20.Hall, S. L., A. Stokes, E. L. Tierney, W. T. London, R. B. Belshe, F. C. Newman, and B. R. Murphy. 1992. Cold-passaged human parainfluenza type 3 viruses contain ts and non-ts mutations leading to attenuation in rhesus monkeys. Virus Res. 22:173-184. [DOI] [PubMed] [Google Scholar]
- 21.Haller, A. A., T. Miller, M. Mitiku, and K. Coelingh. 2000. Expression of the surface glycoproteins of human parainfluenza virus type 3 by bovine parainfluenza virus type 3, a novel attenuated virus vaccine vector. J. Virol. 74:11626-11635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karron, R. A., M. Makhene, K. Gay, M. H. Wilson, M. L. Clements, and B. R. Murphy. 1996. Evaluation of a live attenuated bovine parainfluenza type 3 vaccine in two- to six-month-old infants. Pediatr. Infect. Dis. J. 15:650-654. [DOI] [PubMed] [Google Scholar]
- 23.Karron, R. A., P. F. Wright, S. L. Hall, M. Makhene, J. Thompson, B. A. Burns, S. Tollefson, M. C. Steinhoff, M. H. Wilson, D. O. Harris, et al. 1995. A live attenuated bovine parainfluenza virus type 3 vaccine is safe, infectious, immunogenic, and phenotypically stable in infants and children. J. Infect. Dis. 171:1107-1114. [DOI] [PubMed] [Google Scholar]
- 24.Karron, R. A., P. F. Wright, F. K. Newman, M. Makhene, J. Thompson, R. Samorodin, M. H. Wilson, E. L. Anderson, M. L. Clements, B. R. Murphy, and R. B. Belshe. 1995. A live human parainfluenza type 3 virus vaccine is attenuated and immunogenic in healthy infants and children. J. Infect. Dis. 172:1445-1450. [DOI] [PubMed] [Google Scholar]
- 25.Kolakofsky, D., T. Pelet, D. Garcin, S. Hausmann, J. Curran, and L. Roux. 1998. Paramyxovirus RNA synthesis and the requirement for hexamer genome length: the rule of six revisited. J. Virol. 72:891-899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lamb, R. A., and D. Kolakofsky. 2001. Paramyxoviridae: the viruses and their replication, p. 1305-1340. In D. M. Knipe, P. M. Howley, D. E. Griffin, R. A. Lamb, M. A. Martin, B. Roizman, and S. E. Straus (ed.), Fields virology, 4th ed., vol. 1. Lippincott Williams & Wilkins, Philadelphia, Pa.
- 27.Lee, M. S., D. P. Greenberg, S. H. Yeh, R. Yogev, K. S. Reisinger, J. I. Ward, M. M. Blatter, I. Cho, S. J. Holmes, J. M. Cordova, M. J. August, W. Chen, H. B. Mehta, K. L. Coelingh, and P. M. Mendelman. 2001. Antibody responses to bovine parainfluenza virus type 3 (piv3) vaccination and human piv3 infection in young infants. J. Infect. Dis. 184:909-913. [DOI] [PubMed] [Google Scholar]
- 28.Marx, A., T. J. Torok, R. C. Holman, M. J. Clarke, and L. J. Anderson. 1997. Pediatric hospitalizations for croup (laryngotracheobronchitis): biennial increases associated with human parainfluenza virus 1 epidemics. J. Infect. Dis. 176:1423-1427. [DOI] [PubMed] [Google Scholar]
- 29.Murphy, B. R. 1999. Mucosal immunity to viruses, p. 695-707. In P. L. Ogra, J. Mestecky, M. E. Lamm, W. Strober, J. R. McGhee, and J. Bienstock (ed.), Mucosal immunology, 2nd ed. Academic Press, Inc., New York, N.Y.
- 30.Murphy, B. R., and R. M. Chanock. 2001. Immunization against viral diseases, p. 435-468. In D. M. Knipe, P. M. Howley, D. E. Griffin, R. A. Lamb, M. A. Martin, B. Roizman, and S. E. Straus (ed.), Fields virology, 4th ed., vol. 1. Lippincott Williams & Wilkins, Philadelphia, Pa.
- 31.Murphy, B. R., M. L. Clements, E. L. Tierney, R. E. Black, J. Stienberg, and R. M. Chanock. 1985. Dose response of influenza A/Washington/897/80 (H3N2) avian-human reassortant virus in adult volunteers. J. Infect. Dis 152:225-229. [DOI] [PubMed] [Google Scholar]
- 32.Murphy, B. R., D. L. Sly, E. L. Tierney, N. T. Hosier, J. G. Massicot, W. T. London, R. M. Chanock, R. G. Webster, and V. S. Hinshaw. 1982. Reassortant virus derived from avian and human influenza A viruses is attenuated and immunogenic in monkeys. Science 218:1330-1332. [DOI] [PubMed] [Google Scholar]
- 33.Newman, J. T., S. R. Surman, J. M. Riggs, C. T. Hansen, P. L. Collins, B. R. Murphy, and M. H. Skiadopoulos. 2002. Sequence analysis of the Washington/1964 strain of human parainfluenza virus type 1 (HPIV1) and recovery and characterization of wild type recombinant HPIV1 produced by reverse genetics. Virus Genes 24:77-92. [DOI] [PubMed] [Google Scholar]
- 34.Schmidt, A. C., J. M. McAuliffe, A. Huang, S. R. Surman, J. E. Bailly, W. R. Elkins, P. L. Collins, B. R. Murphy, and M. H. Skiadopoulos. 2000. Bovine parainfluenza virus type 3 (BPIV3) fusion and hemagglutinin-neuraminidase glycoproteins make an important contribution to the restricted replication of BPIV3 in primates. J. Virol. 74:8922-8929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Skiadopoulos, M. H., A. P. Durbin, J. M. Tatem, S. L. Wu, M. Paschalis, T. Tao, P. L. Collins, and B. R. Murphy. 1998. Three amino acid substitutions in the L protein of the human parainfluenza virus type 3 cp45 live attenuated vaccine candidate contribute to its temperature-sensitive and attenuation phenotypes. J. Virol. 72:1762-1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Skiadopoulos, M. H., S. Surman, J. M. Tatem, M. Paschalis, S. L. Wu, S. A. Udem, A. P. Durbin, P. L. Collins, and B. R. Murphy. 1999. Identification of mutations contributing to the temperature-sensitive, cold-adapted, and attenuation phenotypes of the live-attenuated cold-passage 45 (cp45) human parainfluenza virus 3 candidate vaccine. J. Virol. 73:1374-1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Skiadopoulos, M. H., S. R. Surman, J. M. Riggs, W. R. Elkins, M. St. Claire, M. Nishio, D. Garcin, D. Kolakofsky, P. L. Collins, and B. R. Murphy. 2002. Sendai virus, a murine parainfluenza virus type 1, replicates to a level similar to human PIV1 in the upper and lower respiratory tract of African green monkeys and chimpanzees. Virology 297:153-160. [DOI] [PubMed] [Google Scholar]
- 38.Talon, J., C. M. Horvath, R. Polley, C. F. Basler, T. Muster, P. Palese, and A. Garcia-Sastre. 2000. Activation of interferon regulatory factor 3 is inhibited by the influenza A virus NS1 protein. J. Virol. 74:7989-7996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.van Wyke Coelingh, K. L., C. Winter, and B. R. Murphy. 1985. Antigenic variation in the hemagglutinin-neuraminidase protein of human parainfluenza type 3 virus. Virology 143:569-582. [DOI] [PubMed] [Google Scholar]
- 40.Vines, A., K. Wells, M. Matrosovich, M. R. Castrucci, T. Ito, and Y. Kawaoka. 1998. The role of influenza A virus hemagglutinin residues 226 and 228 in receptor specificity and host range restriction. J. Virol. 72:7626-7631. [DOI] [PMC free article] [PubMed] [Google Scholar]