Abstract
A hamster viscerotropic strain of yellow fever (YF) virus has been derived after serial passage of strain Asibi through hamsters. The parental Asibi/hamster p0 virus causes a mild and transient viremia in hamsters with no outward, clinical signs of illness. In contrast, the viscerotropic Asibi/hamster p7 virus causes a robust viremia, severe illness, and death in subadult hamsters. The genome of the hamster viscerotropic Asibi/hamster p7 virus has been sequenced and compared with the parental nonviscerotropic Asibi/hamster p0 virus identifying 14 nucleotide changes encoding only seven amino acid substitutions. The majority of these substitutions (five of seven) fall within the envelope (E) protein at positions Q27H, D28G, D155A, K323R, and K331R. These results support an important role for the E protein in determining YF virus viscerotropism.
Yellow fever (YF) virus is the causative agent of YF, a viral hemorrhagic fever. In addition to the significant morbidity and mortality caused by YF in regions of Africa and South America where it is endemic, YF virus poses a risk as a potential bioterrorism agent. Although an effective vaccine (17D) is available, there have been increasing numbers of YF cases in the past 15 years (28).
YF virus is a member of the family Flaviviridae, genus Flavivirus. Flaviviruses are small, enveloped viruses with a single-stranded, positive-sense RNA genome ca. 11 kb in length. The genome encodes a 5′ noncoding region (5′NCR), followed by a single open reading frame and a 3′NCR. The open reading frame codes for a polyprotein 3,411 amino acids in length that is co- and posttranslationally cleaved to generate three structural proteins (core [C], premembrane [prM], and envelope [E]) and eight nonstructural proteins (NS1, NS2A, NS2B, NS3, NS4A, 2K, NS4B, and NS5).
Although the disease caused by YF virus has been described extensively in the literature, there is a limited understanding of the molecular basis of attenuation and virulence of YF virus. The mechanism of 17D attenuation is still unknown and, in light of recent reports of reversion to virulence (4, 9, 22, 33), further investigation into the mechanisms of viscerotropism and attenuation are warranted.
The genomes of several attenuated YF viruses have been sequenced, including the vaccine strains 17D-204 (27), 17DD (7), and French neurotropic vaccine (FNV) (34), as well as the attenuated Asibi/HeLa p6 virus (8). These attenuated strains are characterized by loss of viscerotropism in monkeys and loss of vector competence. Comparison of these attenuated viruses with their respective parental viruses has identified a number of mutations that may be important in YF virus attenuation. Wild-type Asibi was passaged 176 times in mouse and chicken tissues to derive the 17D vaccine strain, and this subsequently led to derivation of two vaccine substrains, 17D-204 and 17DD, used today (for a review, see Barrett [2]). A comparison of wild-type Asibi virus with the vaccine substrains 17D-204 by Hahn et al. (11) resulted in the identification of 67 nucleotide changes encoding 31 amino acid substitutions. Inclusion of sequences from other isolates of 17D-204 and the 17DD substrain reduced the number of amino acid substitutions that separate the attenuated 17D viruses from the parental Asibi virus to 20 (2, 7, 11, 27). Similarly, the FNV strain was found to differ from its wild-type parent French viscerotropic virus by 77 nucleotides encoding 37 amino acids (34). In addition, six passages of wild-type strain Asibi in human HeLa cells resulted in an attenuated variant, Asibi/HeLa p6, that was attenuated for viscerotropism in monkeys, neurovirulence in mice, and vector competence in Aedes aegypti (1, 6, 13). Asibi/HeLa p6 differs from the parental Asibi by only 29 nucleotides encoding 10 amino acids (8). Due to the large number of mutations, elucidation of the precise determinants of attenuation and viscerotropism has not been possible. However, despite their varied passage histories, all of these attenuated strains show a disproportionate number of mutations within the E protein gene.
The E protein is the major surface protein of the flaviviruses and is thought to be involved in receptor binding and membrane fusion (14, 15, 16). The E protein forms a homodimer that is oriented parallel to the viral envelope. It is characterized by three distinct domains: domain I, the central domain; domain II, the dimerization domain; and domain III, the putative receptor-binding domain (26). Mutations in the flavivirus E protein have been implicated in alterations of viral tropism and virulence (3, 10, 12, 17, 18, 19, 20, 21, 23, 29-31).
Characterization of the molecular determinants of YF virus viscerotropism has been hindered by the lack of a small animal model. Previous studies were limited to the use of nonhuman primates (typically macaques or cynomolgus monkeys). Tesh et al. (32) and Xiao et al. (35) recently described the pathology of a viscerotropic YF virus infection in hamsters. These studies used a previously uncharacterized South American strain of YF virus, Jimenez. The wild-type Jimenez strain was found to cause illness and death in a small number of hamsters. However, after 10 serial passages through hamster liver, a more hamster-virulent YF virus was derived. The Jimenez/hamster passage 10 (p10) virus caused increased and prolonged viremia in hamsters but only a moderate increase in morbidity and mortality. In order to investigate the molecular determinants of YF virus viscerotropism in the hamster model, a hamster viscerotropic strain of the well-characterized Asibi virus was generated. In contrast to the model of Tesh et al. (32), the parental Asibi/hamster p0 virus causes only a transient viremia with no outward signs of clinical illness in subadult (3- to 4-week-old) hamsters, whereas the hamster viscerotropic, Asibi/hamster p7 virus causes severe illness and death in 100% of subadult hamsters. Generation of a hamster viscerotropic strain of YF virus from the well-characterized Asibi strain has allowed identification of key regions of the YF virus genome likely to be important in the viscerotropic phenotype. These regions may serve as targets for improved vaccine development and antiviral therapies.
MATERIALS AND METHODS
Viruses.
The parental Asibi virus used in these studies was obtained from the World Reference Center for Arboviruses. The parental Asibi virus was passaged seven times through hamster liver (as described below) to derive the Asibi/hamster p7 virus.
Animals.
The animals used in these studies were 3- to 4-week-old, female, Golden Syrian hamsters (Mesocricetus auratus) from Harlan Sprague-Dawley. All animals were handled according to federal and institutional guidelines.
Hamster passages.
A single hamster was inoculated intraperitoneally (i.p.) with Asibi virus. At 3 days postinfection (dpi), the liver was harvested and homogenized in phosphate-buffered saline. After being frozen at −70°C overnight, 100 μl of the liver homogenate was inoculated i.p. into a naive hamster. This process was repeated six times to generate the viscerotropic Asibi/hamster p7 virus. The phenotype of the passage prior to p7 was tested in hamsters, and the Asibi/hamster p7 virus was the first passage to cause 100% mortality in 3- to 4-week-old hamsters.
Titration of viruses.
Serum was obtained by saphenous vein bleed each day for 6 days after i.p. inoculation with either wild-type Asibi/hamster p0 or viscerotropic Asibi/hamster p7. The virus titer in the serum was determined as the 50% tissue culture infectious dose in Vero cells.
Morbidity and mortality.
Hamsters were inoculated i.p. with Asibi/hamster p0 or Asibi/hamster p7 virus and observed for signs of illness for 14 days. Signs of illness included ruffled fur, lethargy, hunched posture, and paralysis. Some animals found to be completely moribund were euthanized to collect organ samples. These animals are not included in the survival curve data.
Histopathology.
Livers and spleens were harvested 5 and 6 dpi for histological examination. The tissues were fixed in 10% buffered formalin for 48 h and then transferred to 70% ethanol for storage. The tissues were paraffin embedded, sectioned, and stained with hematoxylin and eosin by the University of Texas Medical Branch histopathology core facility.
Nucleotide sequence analysis.
Viral RNA was isolated by using the QIamp viral RNA Minikit (Qiagen). The genome was amplified by reverse transcription-PCR with YF virus-specific primers. Fragments were cloned into either pGEM-T (Promega) or pCR (Invitrogen) vector and amplified in DH5α competent cells. A consensus sequence was taken from three or more clones sequenced in both directions. Automated sequencing was performed in the University of Texas Medical Branch protein chemistry core laboratory. Sequence analysis was performed by using the vector NTI program (InforMax).
RESULTS
Passage of wild-type YF virus Asibi in hamsters.
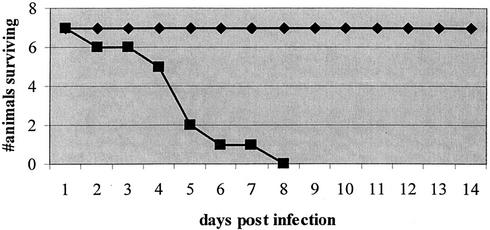
Wild-type, non-hamster-passaged Asibi (p0) virus caused a mild and transient viremia with no outward signs of illness in subadult hamsters, and all animals survived. In contrast, all seven hamsters inoculated with Asibi/hamster p7 developed outward signs of illness, including ruffled fur, lethargy, and hunched posture and died within 2 days of onset of clinical signs of disease. Signs of illness appeared by as early as 2 dpi, and all animals succumbed to illness by 8 dpi. The survival of these animals is summarized in Fig. 1.
FIG. 1.
Survival of 3- to 4-week-old Golden Syrian hamsters after inoculation with either parental Asibi p0 virus (♦) or viscerotropic Asibi p7 virus (▪).
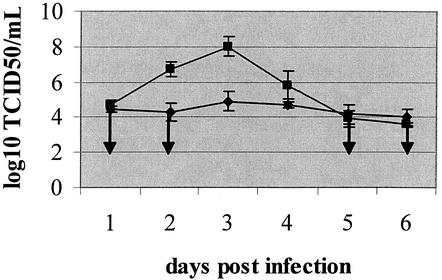
Viremia.
Hamsters inoculated with Asibi/hamster p7 virus developed a robust viremia that peaked at 3 dpi (Fig. 2), as shown with other strains of YF virus by Tesh et al. (32). Only a modest viremia was detected in hamsters inoculated with Asibi/hamster p0, and no viremia was detected in two of five animals (Fig. 2).
FIG. 2.
Viremia in subadult hamsters inoculated with either Asibi p7 (▪) or Asibi p0 (♦) virus. The values shown are an average of results from five to six animals. Downward arrows indicate values that are at or below the limit of sensitivity for this assay.
Histopathology.
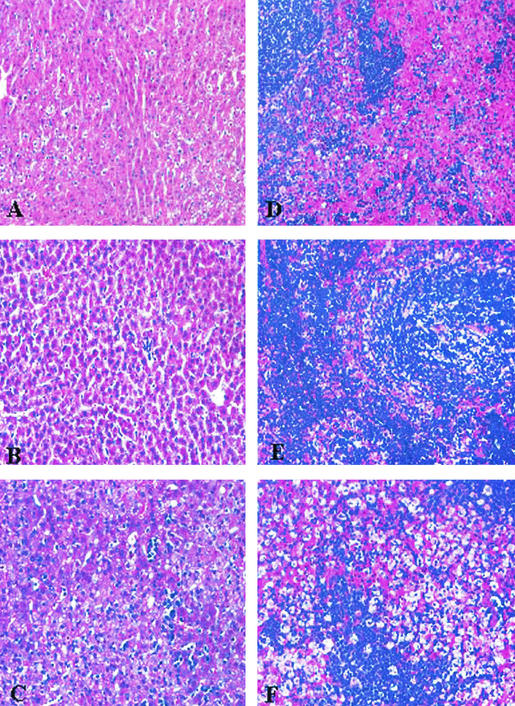
Spleen and liver were harvested at 5 to 6 dpi (at a time determined by Xiao et al. [35] to be the peak of histopathologic changes). Samples from five animals inoculated with Asibi/hamster p0 and five animals inoculated with Asibi/hamster p7 were paraffin embedded and stained with hematoxylin and eosin for microscopic evaluation. The microscopic examination was conducted with the pathologist having no previous knowledge as to the infectious status of each animal.
(i) Liver.
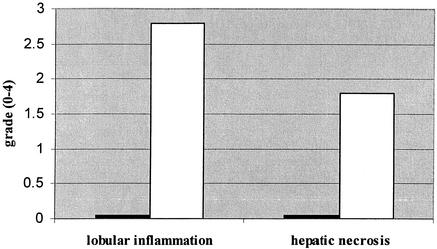
The livers of hamsters inoculated with Asibi/hamster p0 showed no significant changes on either day 5 or 6 pi when compared with those of mock-infected animals (Fig. 3A and B). However, the livers of hamsters inoculated with Asibi/hamster p7 showed significant pathological changes, including microvesicular steatosis (accumulation of fatty acids in small vesicles within hepatocytes), moderate to severe inflammation, and mild to moderate hepatic necrosis (Fig. 3C). Animals were sacrificed when they began showing clinical signs of illness (5 to 6 dpi). Hepatic pathology varied slightly among the animals with steatosis involving 50 to 98% of the liver, with an average of 77% (Fig. 4A). The results of these studies are summarized in Fig. 4.
FIG. 3.
Hematoxylin-and-eosin-stained sections of hamster liver and spleen 6 dpi. (A) Liver from mock-infected hamster; (B) liver from hamster infected with Asibi/hamster p0; (C) liver from hamster infected with Asibi/hamster p7; (D) spleen from mock-infected hamster; (E) spleen from hamster infected with Asibi/hamster p0; (F) spleen from hamster infected with Asibi/hamster p7.
FIG. 4.
Liver pathology in hamsters inoculated with viscerotropic Asibi p7. Hepatic necrosis and lobular inflammation are presented as a grade from 0 to 4, with 0 being none and 4 being severe. The data are shown as the average from five experimental animals. Columns: ▪, Asibi p0; □, Asibi p7.
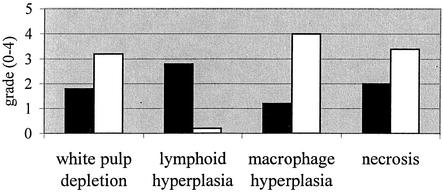
(ii) Spleen.
The spleens of four of five hamsters inoculated with Asibi/hamster p0 were characterized by marked lymphoid hyperplasia and moderate to severe white pulp depletion, necrosis, and splenic macrophage hyperplasia (Fig. 3E and 5). The spleen from the fifth hamster showed no abnormalities. There was no lymphoid hyperplasia in any of the spleens from hamsters inoculated with Asibi/hamster p7; however, there was severe splenic macrophage hyperplasia and necrosis. There was also moderate to severe white pulp depletion (Fig. 3F and 5).
FIG. 5.
Summary of the splenic abnormalities identified in 3- to 4-week-old hamsters inoculated with Asibi p0 and Asibi p7 viruses. Columns: ▪, Asibi p0; □, Asibi p7.
Nucleotide and deduced amino acid changes of Asibi/hamster p7 virus.
The complete genomic sequence of the Asibi/hamster p7 virus was determined and compared with that of the published Asibi sequence (11) identifying 23 nucleotide changes. Regions that contained nucleotide changes were amplified from the parental Asibi/hamster p0 virus and sequenced for confirmation. The parental Asibi strain used in these studies was obtained from the World Reference Center for Arboviruses and had five passages through suckling mouse brain. This virus differed from the published sequence for Asibi (11) at genomic nucleotide positions 2193, 2355, 2704, 3817, 3925, 5926, 6013, 6829, and 7319 reducing the number of nucleotide changes between the parental and hamster-passaged viruses from 23 to 14. These 14 nucleotide changes encoded seven amino acid substitutions (Table 1). Three clones were sequenced for each fragment to determine a consensus sequence. The majority of the nucleotide changes were identified in all three clones. However, there was heterogeneity at nucleotide positions 802 and 1056 (amino acid Q28 in the E protein), where only two of three clones contained mutations.
TABLE 1.
Summary of the nucleotide and deduced amino acid changes between Asibi/hamster p0 virus and Asibi/hamster p7 virus
| Nucleotide no.a | Original nucleotide
|
Deduced amino acid change | Nucleotide substitution
|
||
|---|---|---|---|---|---|
| Asibi p0 | Asibi p7 | Asibi p0 | Asibi p7 | ||
| 802 | A | G | |||
| 887 | C | U | |||
| 1000* | G | A | |||
| 1054* | A | C | E27 | Q | H |
| 1056 | A | G | E28 | D | G |
| 1437* | A | C | E155 | D | A |
| 1941 | A | G | E323 | K | R |
| 1965*† | A | G | E331 | K | R |
| 2779 | U | C | |||
| 3274*† | G | A | |||
| 3821*‡ | A | G | NS2A48 | T | A |
| 4864*† | G | A | |||
| 7178*‡ | G | A | NS4B98 | V | I |
| 8917 | C | U | |||
*, Nucleotide substitutions shared with Asibi/HeLa p6 virus; †, nucleotide substitutions shared with 17D virus; ‡, nucleotide substitutions shared with FNV.
The nucleotide and amino acid substitutions in the Asibi/hamster p7 virus were not evenly distributed throughout the genome (Table 2). There were eight nucleotide substitutions found within the structural protein genes (two in the M protein gene and six in the E protein gene), and the remaining six nucleotide changes were located within the nonstructural protein genes (two in NS1 and one each in NS2A, NS3, NS4B, and NS5). No nucleotide changes were identified within the C, prM, NS2B, NS4A, and 2K protein genes or within the 5′NCR or 3′NCR. Two amino acid substitutions were located in the nonstructural proteins at positions NS2A T48A and NS4B V98I; however, the majority of the amino acid changes were located in the E protein: Q27H, D28G, D155A, K323R, and K331R. Many of the nucleotide and amino acid changes identified in the Asibi/hamster p7 virus were common to other derivatives of Asibi (17D and Asibi/HeLa p6), the vaccine strain FNV, and/or wild-type YF viruses. This may suggest that only certain regions of the genome can tolerate mutation; therefore, viable viruses accumulate mutations only within these regions despite strong selective pressures. Comparison of the Asibi/hamster p7 genome with other YF virus sequences in GenBank indicates that only four nucleotide changes appear to be unique to the Asibi/hamster p7 virus (Table 1), and these encode one amino acid substitution at E323 (K to R). All YF virus sequences in GenBank had K323, whereas Asibi/hamster p7 had K323R. In addition, a GenBank search revealed only three YF isolates, from the East and Central African genotype, with the mutation D28G (Ethiopia 60A and 60B and CAR 80) (24); however, the phenotype of these viruses in hamsters is unknown.
TABLE 2.
Distribution of nucleotide and amino acid changes throughout the genome of the Asibi/hamster p7 virus as compared with the Asibi/hamster p0 virusa
| Region | Length (no. of nt) | Total no. of nt changes | % nt changes | Total no. of aa changes | % aa changes |
|---|---|---|---|---|---|
| 5′NCR | 119 | 0 | NC | 0 | NC |
| C | 362 | 0 | NC | 0 | NC |
| prM | 267 | 0 | NC | 0 | NC |
| M | 225 | 2 | 0.8 | 0 | NC |
| E | 1,479 | 6 | 0.4 | 5 | 1.0 |
| NS1 | 1,227 | 2 | 0.2 | 0 | NC |
| NS2A | 501 | 1 | 0.2 | 1 | 0.6 |
| NS2B | 390 | 0 | NC | 0 | NC |
| NS3 | 1,869 | 1 | 0.1 | 0 | NC |
| NS4A | 378 | 0 | NC | 0 | NC |
| 2K | 66 | 0 | NC | 0 | NC |
| NS4B | 750 | 1 | 0.1 | 1 | 0.4 |
| NS5 | 2,715 | 1 | 0.04 | 0 | NC |
| 3′NCR | 511 | 0 | NC | 0 | NC |
nt, nucleotide(s); aa, amino acid(s); NC, no change(s).
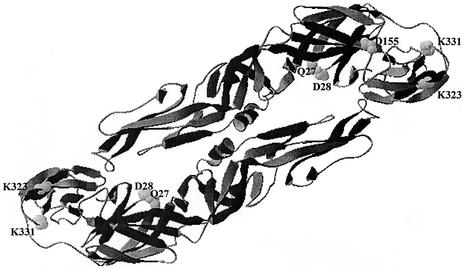
Spatial location of Asibi/hamster p7 residues on the model of the flavivirus E protein ectodomain.
Seven of the fourteen nucleotide changes encode amino acid substitutions, and five of these are located in the E protein at amino acid positions Q27H, D28G, D155A, K323R, and K331R. The locations of these amino acid changes have been modeled onto the tick-borne encephalitis (TBE) virus E protein crystal structure (26) (Fig. 6) to investigate the potential interactions of the amino acid substitutions. Q27, D28, and D155 are located in domain I, with Q27 and D28 adjacent to one another and D155 spatially distinct from the former residues. The other two changes, K323 and K331, are located relatively close together in domain III. There are no amino acid substitutions within domain II or the stem-anchor region.
FIG. 6.
Three-dimensional model of the YF virus E protein based on the crystallographic structure of TBE virus E protein (26). The five amino acid positions that differ between the Asibi/hamster p0 and Asibi/hamster p7—Q27, D28, D155, K323, and K331—are highlighted and labeled. The Swiss PDB program was used to model the YF virus E protein onto the crystallographic structure of the TBE virus E protein. The orientation of the monomers to form a dimer was approximated.
DISCUSSION
Until recently, studies on the mechanism of viscerotropic disease of YF were limited to using nonhuman primates. However, the recent descriptions of a hamster model for viscerotropic disease by Tesh et al. (32) and Xiao et al. (35) facilitates studies to characterize the molecular mechanism of viscerotropic YF disease. The well-characterized strain Asibi, the prototype strain of YF virus and parent to live attenuated vaccine strain 17D, was selected to investigate the molecular basis of viscerotropic disease in the hamster model. The genomes of wild-type Asibi (11) and attenuated derivatives 17D-204 (27), 17DD (7), and Asibi/HeLa p6 (8) have been published to elucidate molecular determinants of attenuation of Asibi. It is very likely that attenuation is multigenic and is encoded by mutations in both the structural and the nonstructural protein genes. However, due to a large number of mutations that separate these attenuated viruses from their parent viruses, only limited conclusions can be drawn.
Hamster-passaged Asibi virus serves as an excellent small-animal model to determine the molecular determinants of viscerotropic YF virus infection. Asibi/hamster p0 virus was only mildly hepatotropic in hamsters and caused a slight viremia with no outward clinical signs of illness or histologic changes in the liver. Asibi/hamster p0 virus caused only mild hepatic inflammation but substantial changes in the spleen, including marked lymphoid hyperplasia. Asibi/hamster p7 virus caused a robust viremia and a viscerotropic infection characterized by hepatic necrosis with severe microvesicular steatosis and death. The pathology of Asibi/hamster p7 infection in hamsters was consistent with that noted by Tesh et al. (32) and Xiao et al. (35), as well as with that of the established experimental model (macaques).
The selective pressure of serial passage through hamster liver resulted in a change of viral tropism between the parental Asibi/hamster p0 and the hamster viscerotropic Asibi/hamster p7. This was evidenced by the dramatic difference in peak viremia and the different histologic appearances of the livers and spleens of animals inoculated with these viruses.
The genomes of these phenotypically distinct viruses differed by only 14 nucleotides encoding seven amino acid substitutions (Table 1). Thus, there were relatively few nucleotide changes associated with passage in hamsters, and half of these nucleotide changes encoded amino acid substitutions. Heterogeneity was noted at some nucleotide positions (i.e., positions 802 and 1056), indicating a mixed population of viruses. YF virus has been shown by others to accumulate few mutations despite intense selective pressure, indicating that the virus can tolerate minimal sequence variation (8, 11, 34). The mutations that accumulated during virus passage were not evenly distributed throughout the genome (Table 2). Mutations tended to accumulate in specific regions of the genome (specifically the E, NS2A, and NS4B protein genes and the 3′NCR) regardless of the selective pressure applied. This is evidenced by the fact that vaccine strains 17D and FNV, as well as the attenuated strain Asibi-HeLa p6, share the same nucleotides and amino acid residues with the hamster viscerotropic Asibi/hamster p7 virus at a number of positions despite selection by passaging in different hosts, namely, chicken, mouse, and human HeLa cells, respectively (8, 11, 34) (Table 1). Many of these shared mutations fall within the E protein gene (7, 8, 11, 27, 34). The accumulation of mutations at the same positions despite varied selective pressures indicates that YF virus can tolerate mutation only at certain nucleotide or amino acid positions, and these positions are clustered in the E protein gene, NS2A, and NS4B.
5′NCR and 3′NCR are thought to play an important role in the viral life cycle. Mutations in 3′NCR are thought to affect viral replication and have been identified in attenuated strains of YF virus (7, 8, 11, 27, 34). However, there were no mutations within the 5′NCR or 3′NCR of the hamster viscerotropic Asibi/hamster p7 virus, indicating that these regions are not involved in the increased viscerotropism of the Asibi/hamster p7 virus.
The E protein is the major surface protein of YF virus and plays an important role in viral tropism. Based on the high proportion of changes identified in the E protein of the Asibi/hamster p7 virus (5/7) and the fact that the unique amino acid substitution falls within the E protein, this region is likely to play an important role in the viscerotropic phenotype of this virus in hamsters. No changes were identified in domain II or the stem-anchor region of the E protein, indicating that changes in domains I and/or III may be sufficient to alter viral tropism and increase virulence in hamsters.
The mutations in the E protein—Q27H, D28G, and D155A—fall within domain I, the central domain. Q27H and D155A are also found in the attenuated Asibi/HeLa p6 virus. All wild-type and attenuated YF virus strains sequenced to date have D28G except for three East and Central African strains (Ethiopia 61A, Ethiopia 61B, and CAR 80) (24). These three viruses share the D28G substitution like the Asibi/hamster p7 virus. The hamster virulence phenotype of these viruses is currently under investigation.
Domain III is hypothesized to be the receptor-binding domain and is likely to be important in the determination of viral tropism (14, 15, 16, 26). Mutation in this region has been associated with a neurovirulent 17D vaccine revertant (18), as well as with attenuation in other flaviviruses (3, 10, 12, 17, 19, 20, 21). The hamster viscerotropic Asibi/hamster p7 virus differs from the parental Asibi/hamster p0 at two amino acids within domain III: K323 and K331. The substitution K331R is also found in the attenuated Asibi/HeLa p6 and 17D viruses, as well as the wild-type French viscerotropic virus (7, 8, 11, 27, 34). However, the K323R substitution appears to be unique to the hamster viscerotropic virus. K323 is found in all wild-type and vaccine YF virus sequences in GenBank. Since this is the only truly unique change between Asibi/hamster p0 and Asibi/hamster p7, it is highly likely that domain III is a critical determinant for YF tropism to hamster hepatocytes. We speculate that the K323R mutation enables the virus to bind to cell receptor(s) on hamster hepatocytes and subsequently infect the hepatocytes.
Mutations in the nonstructural proteins may also affect the viscerotropic phenotype of the Asibi/hamster p7 virus. The small hydrophobic proteins (NS2A, NS2B, NS4A, and NS4B) have been implicated in membrane permeabilization and the cytopathic effects of Japanese encephalitis virus, a member of the Flavivirus genus (5, 25). The amino acid changes identified within NS2A and NS4B may be involved in the increased liver pathology found with the Asibi/hamster p7 virus. It is also possible that these mutations could lead to enhanced viral replication, causing increased viremia and tissue damage.
These studies support a multigenic model for YF virus viscerotropism. Mutations within the E protein (particularly domain III) are hypothesized to increase attachment and/or entry into hepatocytes, whereas changes in the small hydrophobic nonstructural proteins NS2A and NS4B may cause cellular damage and hepatic necrosis, leading to hamster illness and/or death.
Previous studies on the molecular mechanisms of viscerotropism and attenuation have identified large numbers of nucleotide and amino acid differences between virulent and attenuated strains (7, 8, 11, 27, 34). The small number of amino acid substitutions (only seven) identified between the nonviscerotropic virus (Asibi/hamster p0) and the viscerotropic virus (Asibi/hamster p7) allows a more specific determination of the critical regions of the YF virus genome involved in viscerotropic YF disease (and probably attenuation). No nucleotide changes were identified in the 5′NCR or 3′NCR, and the amino acid substitutions were clustered into three regions: the E protein (five of seven), NS2A (one of seven), and NS4B (one of seven). This information will aid in the improvement of YF virus vaccines with reduced potential for reversion to viscerotropism.
Acknowledgments
We thank R. Shope for providing the Asibi virus and R. Tesh for helpful discussions.
M.A.M. was funded by an institutional training grant from the NIH (T32 AI 7526).
REFERENCES
- 1.Barrett, A. D., T. P. Monath, C. B. Cropp, J. A. Adkins, T. N. Ledger, E. A. Gould, J. J. Schlesinger, R. M. Kinney, and D. W. Trent. 1990. Attenuation of wild-type yellow fever virus by passage in HeLa cells. J. Gen. Virol. 71:2301-2306. [DOI] [PubMed] [Google Scholar]
- 2.Barrett, A. D. 1997. Yellow fever vaccines. Biologicals 25:17-25. [DOI] [PubMed] [Google Scholar]
- 3.Cecilia, D., and E. A. Gould. 1991. Nucleotide changes responsible for loss of neuroinvasiveness in Japanese encephalitis virus neutralization-resistant mutants. Virology 181:70-77. [DOI] [PubMed] [Google Scholar]
- 4.Chan, R. C., D. J. Penney, D. Little, I. W. Carter, J. A. Roberts, and W. D. Rawlinson. 2001. Hepatitis and death following vaccination with 17D-204 yellow fever vaccine. Lancet 358:121-122. [DOI] [PubMed] [Google Scholar]
- 5.Chang, Y. S., C. L. Liao, C. H. Tsao, M. C. Chen, C. I. Liu, L. K. Chen, and Y. L. Lin. 1999. Membrane permeabilization by small hydrophobic nonstructural proteins of Japanese encephalitis virus. J. Virol. 73:6257-6264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Converse, J. L., R. M. Kovatch, J. D. Pulliam, S. C. Nagle, Jr., and E. M. Snyder. 1971. Virulence and pathogenesis of yellow fever virus serially passaged in cell culture. Appl. Microbiol. 21:1053-1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.dos Santos, C. N., P. R. Post, R. Carvalho, I. I. Ferreira, C. M. Rice, and R. Galler. 1995. Complete nucleotide sequence of yellow fever virus vaccine strains 17DD and 17D-213. Virus Res. 35:35-41. [DOI] [PubMed] [Google Scholar]
- 8.Dunster, L. M., H. Wang, K. D. Ryman, B. R. Miller, S. J. Watowich, P. D. Minor, and A. D. Barrett. 1999. Molecular and biological changes associated with HeLa cell attenuation of wild-type yellow fever virus. Virology 261:309-318. [DOI] [PubMed] [Google Scholar]
- 9.Galler, R., K. V. Pugachev, C. L. Santos, S. W. Ocran, A. V. Jabor, S. G. Rodrigues, R. S. Marchevsky, M. S. Freire, L. F. Almeida, A. C. Cruz, A. M. Yamamura, I. M. Rocco, E. S. da Rosa, L. T. Souza, P. F. Vasconcelos, F. Guirakhoo, and T. P. Monath. 2001. Phenotypic and molecular analyses of yellow fever 17DD vaccine viruses associated with serious adverse events in Brazil. Virology 290:309-319. [DOI] [PubMed] [Google Scholar]
- 10.Gao, G. F., M. H. Hussain, H. W. Reid, and E. A. Gould. 1994. Identification of naturally occurring monoclonal antibody escape variants of louping ill virus. J. Gen. Virol. 75:609-614. [DOI] [PubMed] [Google Scholar]
- 11.Hahn, C. S., J. M. Dalrymple, J. H. Strauss, and C. M. Rice. 1987. Comparison of the virulent Asibi strain of yellow fever virus with the 17D vaccine strain derived from it. Proc. Natl. Acad. Sci. USA 84:2019-2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hasegawa, H., M. Yoshida, T. Shiosaka, S. Fujita, and Y. Kobayashi. 1992. Mutations in the envelope protein of Japanese encephalitis virus affect entry into cultured cells and virulence in mice. Virology 191:158-165. [DOI] [PubMed] [Google Scholar]
- 13.Hearn, H. J., Jr., W. A. Chappell, P. Demchak, and J. W. Kominik. 1966. Attenuation of aerosolized yellow fever virus after passage in cell culture. Bacteriol. Rev. 30:615-623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heinz, F. X. 1986. Epitope mapping of flavivirus glycoproteins. Adv. Virus Res. 31:103-168. [DOI] [PubMed] [Google Scholar]
- 15.Heinz, F. X., and S. L. Allison. 2000. Structures and mechanisms in flavivirus fusion. Adv. Virus Res. 55:231-269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heinz, F. X., and S. L. Allison. 2001. The machinery for flavivirus fusion with host cell membranes. Curr. Opin. Microbiol. 4:450-455. [DOI] [PubMed] [Google Scholar]
- 17.Holzmann, H., F. X. Heinz, C. W. Mandl, F. Guirakhoo, and C. Kunz. 1990. A single amino acid substitution in envelope protein E of tick-borne encephalitis virus leads to attenuation in the mouse model. J. Virol. 64:5156-5159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jennings, A. D., J. E. Whitby, P. D. Minor, and A. D. Barrett. 1993. Comparison of the nucleotide and deduced amino acid sequences of the structural protein genes of the yellow fever 17DD vaccine strain from Senegal with those of other yellow fever vaccine viruses. Vaccine 11:679-681. [DOI] [PubMed] [Google Scholar]
- 19.Jiang, W. R., A. Lowe, S. Higgs, H. Reid, and E. A. Gould. 1993. Single amino acid codon changes detected in louping ill virus antibody-resistant mutants with reduced neurovirulence. J. Gen. Virol. 74:931-935. [DOI] [PubMed] [Google Scholar]
- 20.Lee, E., and M. Lobigs. 2002. Mechanism of virulence attenuation of glycosaminoglycan-binding variants of Japanese encephalitis virus and Murray Valley encephalitis virus. J. Virol. 76:4901-4911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lobigs, M., R. Usha, A. Nestorowicz, I. D. Marshall, R. C. Weir, and L. Dalgarno. 1990. Host cell selection of Murray Valley encephalitis virus variants altered at an RGD sequence in the envelope protein and in mouse virulence. Virology 176:587-595. [DOI] [PubMed] [Google Scholar]
- 22.Martin, M., T. F. Tsai, B. Cropp, G. J. Chang, D. A. Holmes, J. Tseng, W. Shieh, S. R. Zaki, I. Al Sanouri, A. F. Cutrona, G. Ray, L. H. Weld, and M. S. Cetron. 2001. Fever and multisystem organ failure associated with 17D-204 yellow fever vaccination: a report of four cases. Lancet 358:98-104. [DOI] [PubMed] [Google Scholar]
- 23.Monath, T. P., J. Arroyo, I. Levenbook, Z. X. Zhang, J. Catalan, K. Draper, and F. Guirakhoo. 2002. Single mutation in the flavivirus envelope protein hinge region increases neurovirulence for mice and monkeys but decreases viscerotropism for monkeys: relevance to development and safety testing of live, attenuated vaccines. J. Virol. 76:1932-1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mutebi, J. P., H. Wang, L. Li, J. E. Bryant, and A. D. Barrett. 2001. Phylogenetic and evolutionary relationships among yellow fever virus isolates in Africa. J. Virol. 75:6999-7008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qu, L., L. K. McMullan, and C. M. Rice. 2001. Isolation and characterization of noncytopathic pestivirus mutants reveals a role for nonstructural protein NS4B in viral cytopathogenicity. J. Virol. 75:10651-10662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rey, F. A., F. X. Heinz, C. Mandl, C. Kunz, and S. C. Harrison. 1995. The envelope glycoprotein from tick-borne encephalitis virus at 2 Å resolution. Nature 375:291-298. [DOI] [PubMed] [Google Scholar]
- 27.Rice, C. M., E. M. Lenches, S. R. Eddy, S. J. Shin, R. L. Sheets, and J. H. Strauss. 1985. Nucleotide sequence of yellow fever virus: implications for flavivirus gene expression and evolution. Science 229:726-733. [DOI] [PubMed] [Google Scholar]
- 28.Robertson, S. E., B. P. Hull, O. Tomori, J. W. LeDuc, and K. Esteves. 1996. Yellow fever: a decade of reemergence. JAMA 276:1157-1162. [PubMed] [Google Scholar]
- 29.Ryman, K. D., T. N. Ledger, R. C. Weir, J. J. Schlesinger, and A. D. Barrett. 1997. Yellow fever virus envelope protein has two discrete type-specific neutralizing epitopes. J. Gen. Virol. 78:1353-1356. [DOI] [PubMed] [Google Scholar]
- 30.Ryman, K. D., T. N. Ledger, G. A. Campbell, S. J. Watowich, and A. D. Barrett. 1998. Mutation in a 17D-204 vaccine substrain-specific envelope protein epitope alters the pathogenesis of yellow fever virus in mice. Virology 244:59-65. [DOI] [PubMed] [Google Scholar]
- 31.Sil, B. K., L. M. Dunster, T. N. Ledger, M. R. Wills, P. D. Minor, and A. D. Barrett. 1992. Identification of envelope protein epitopes that are important in the attenuation process of wild-type yellow fever virus. J. Virol. 66:4265-4270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tesh, R. B., H. Guzman, A. P. da Rosa, P. F. Vasconcelos, L. B. Dias, J. E. Bunnell, H. Zhang, and S. Y. Xiao. 2001. Experimental yellow fever virus infection in the golden hamster (Mesocricetus auratus). I. Virologic, biochemical, and immunologic studies. J. Infect. Dis. 183:1431-1436. [DOI] [PubMed] [Google Scholar]
- 33.Vasconcelos, P. F., E. J. Luna, R. Galler, L. J. Silva, T. L. Coimbra, V. L. Barros, T. P. Monath, S. G. Rodigues, C. Laval, Z. G. Costa, M. F. Vilela, C. L. Santos, P. M. Papaiordanou, V. A. Alves, L. D. Andrade, H. K. Sato, E. S. Rosa, G. B. Froguas, E. Lacava, L. M. Almeida, A. C. Cruz, I. M. Rocco, R. T. Santos, O. F. Oliva, and C. M. Papaiordanou. 2001. Serious adverse events associated with yellow fever 17DD vaccine in Brazil: a report of two cases. Lancet 358:91-97. [DOI] [PubMed] [Google Scholar]
- 34.Wang, E., K. D. Ryman, A. D. Jennings, D. J. Wood, F. Taffs, P. D. Minor, P. G. Sanders, and A. D. Barrett. 1995. Comparison of the genomes of the wild-type French viscerotropic strain of yellow fever virus with its vaccine derivative French neurotropic vaccine. J. Gen. Virol. 76:2749-2755. [DOI] [PubMed] [Google Scholar]
- 35.Xiao, S. Y., H. Zhang, H. Guzman, and R. B. Tesh. 2001. Experimental yellow fever virus infection in the golden hamster (Mesocricetus auratus). II. Pathology. J. Infect. Dis. 183:1437-1444. [DOI] [PubMed] [Google Scholar]