Abstract
Objective:
To investigate specialist physicians' practice decisions in response to liability concerns and their perceptions of the impact of the malpractice environment on patient access to care.
Summary Background Data:
A perennial concern during “malpractice crises” is that liability costs will drive physicians in high-risk specialties out of practice, creating specialist shortages and access-to-care problems.
Methods:
Mail survey of 824 Pennsylvania physicians in general surgery, neurosurgery, orthopedic surgery, obstetrics/gynecology, emergency medicine, and radiology eliciting information on practice decisions made in response to rising liability costs.
Results:
Strong majorities of specialists reported increases over the last 3 years in patients' driving distances (58%) and waiting times (83%) for specialist care or surgery, waiting times for emergency department care (82%), and the number of patients forced to switch physicians (89%). Professional liability costs and managed care were both considered important contributing factors. Small proportions of specialists reported that they would definitely retire (7%) or relocate their practice out of state (4%) within the next 2 years; another third (32% and 29%, respectively) said they would likely do so. Forty-two percent of specialists have reduced or eliminated high-risk aspects of their practice, and 50% are likely to do so over the next 2 years.
Conclusions:
Our data suggest that claims of a “physician exodus” from Pennsylvania due to rising liability costs are overstated, but the malpractice situation is having demonstrable effects on the supply of specialist physicians in affected areas and their scope of practice, which likely impinges upon patients' access to care.
During “malpractice crises,” concerns are expressed that liability costs drive high-risk specialist physicians from practice, creating access-to-care problems. A mail survey of 824 surgical and other specialists in Pennsylvania found that the liability environment is having demonstrable effects on the supply of specialists and their willingness to perform high-risk procedures.
A recurrent theme in policy debates over medical malpractice “crises”1,2 is the effect of rising liability costs on patient access to care. Providers argue that the liability environment is not just a professional problem for doctors and hospitals, but also a grave public health problem, because liability costs drive physician specialists to leave practice or stop providing high-risk services.3 The Bush Administration has recently taken up this theme, reporting a “growing access crisis” in which “increasingly, Americans are at risk for not being able to find a doctor when they most need one.”4 Surgeons are at the leading edge of this debate because they are among those at highest risk for malpractice claims and most affected by rising insurance premiums.
In the current crisis as well as previous crises, empirical evidence offered in support of the “physician exodus” hypothesis has been scarce. The policy debate has been dominated by anecdotes and claims by medical professional societies.4,5 The General Accounting Office (GAO) recently investigated these reports in 5 “crisis” states and was unable to corroborate some of the claimed physician withdrawals and access problems.6
To obtain additional data, we conducted a survey of Pennsylvania surgeons and other specialists in which we inquired about the extent to which liability pressures were causing respondents to exit the state, stop practicing, restrict the services they offer, or limit the types of patients they see. We also examined specialists' perceptions of changes in patient access to specialist care. We hypothesized that most specialists would report being heavily burdened by liability costs, but few would be committed to specific measures to reduce their costs or legal exposure; and to the extent that measures were taken, they would be concentrated among physicians in solo practice and physicians in the 5-county area around Philadelphia, where liability costs were highest.
METHODS
Study Design
Researchers at the Harvard School of Public Health and Columbia Law School partnered with a professional survey organization, Harris Interactive, Inc., to design and conduct the survey. The design of the sample and survey questionnaire were informed by findings from a series of 41 in-depth key informant interviews conducted with representatives from medical specialty societies, county medical societies, hospitals, insurers, and government agencies in Pennsylvania in the fall of 2002.
Sample
Key informants identified 6 specialties (general surgery, neurosurgery, orthopedic surgery, obstetrics/gynecology, emergency medicine, and radiology) as being especially affected by the current liability crisis. A stratified random sample of 1333 physicians in these specialties was drawn from the American Medical Association Physician Masterfile; 1 primary stratum consisted of 5 counties in southeast Pennsylvania which key informants identified as most affected by the crisis and the other consisted of all other counties. Within each stratum, specialists who were active in direct patient care at least 50% time according to Physician Masterfile data were sampled. Sampling was proportionate by specialty except that neurosurgeons were oversampled to ensure adequate representation.
Survey Questionnaire
We developed a 6-page questionnaire using topics and response categories suggested by the key informant interviews. The questionnaire was pretested on 10 Pennsylvania physicians in the targeted specialties who were debriefed in cognitive interviews focusing on comprehension and appropriateness of question topics, wording, response options, and layout. After revision, the questionnaire contained 41 questions, including queries regarding perceptions of specialist supply and patient access to specialist care; likelihood of deciding to relocate, leave, or restrict their practice in response to liability concerns; insurance and malpractice claims experience; and demographic information.
Survey Administration
Following institutional review board approval, the survey was mailed in May 2003 along with a $75 honorarium. Multiple follow-up contacts were made with nonrespondents by mail and telephone over the next 8 weeks. Respondents were also given the option of completing the survey online; 8% of respondents did so. A total of 824 physicians completed the survey. The adjusted response rate, after exclusion of 65 noneligible physicians (52 no longer in direct patient care, 11 relocated out of state, and 2 deceased) was 65%. The margin of error was ±4% points.
Statistical Analysis
Sampling weights were applied to ensure that survey responses reflected the distribution of Pennsylvania physicians in direct patient care in the selected specialties. Data were weighted first within each geographic stratum by specialty, gender, and length of time in practice; and then to make the data representative of all Pennsylvania physicians in each specialty. All results except for the sample characteristics are presented in weighted form, although the effect of weighting was minimal.
The data were analyzed in the SPSS 11.5 and STATA 7.0 statistical software packages using appropriate corrections for the complex survey design. Subgroup comparisons were performed using adjusted Wald Tests for trend (for ordered responses) and design-corrected Pearson χ2 analysis (for unordered responses).
RESULTS
Respondent Characteristics
The sample contained 155 general surgeons, 52 neurosurgeons, 127 orthopedic surgeons, 187 obstetrician/gynecologists, 148 emergency medicine physicians, and 155 radiologists (Table 1). Approximately two thirds of the sample practiced in the 5 “high-risk” counties around Philadelphia. One fifth of the specialists were solo practitioners, about 40% worked in a group practice, 28% were hospital based, and 14% worked in other settings. Eighty percent of the sample had a strong personal connection to Pennsylvania (either grew up, attended medical school, or did residency training in the state). Nearly half of the specialists had been named in a malpractice suit in the previous 3 years, and only 12% had never been sued.
TABLE 1. Physician Sample Characteristics (n = 824)

Specialists' Personal Decisions to Leave or Modify Practice
Only a small proportion (<4%) of specialists indicated that they would definitely relocate part or all of their practice time out of state within the next 2 years because of the cost of professional liability insurance; much larger proportions reported that they were very likely (12%) or somewhat likely (17%) to relocate (Table 2). Surgeons (general surgeons, neurosurgeons, and orthopedic surgeons) were significantly more likely than other specialists to report plans to relocate (F = 4.28, P = 0.002). Solo practitioners were most inclined to relocate, and hospital-based physicians were least inclined (F = 3.64, P = 0.0004).
TABLE 2. Physician Decisions to Leave or Modify Practice, by Practice Setting
One third of specialists were at least somewhat likely to retire early or cease direct patient care in response to liability costs within the next 2 years, with 7% indicating that they would definitely do so (Table 2). Surgeons were more inclined to retire early than other specialists (F = 3.72, P = 0.01). The “solo practitioner” effect was again significant (F = 7.01, P < 0.0001), perhaps owing to the higher mean age of solo practitioners (54 years) relative to specialists in other settings (49 years) (t = −5.72, P < 0.0001).
A very substantial proportion of specialists reported restricting the scope of their clinical practice because of liability concerns. Forty-three percent had already personally reduced or eliminated high-risk aspects of their practice, and 50% said they would likely (continue to) do so over the next 2 years (12% definitely will, 19% very likely, and 19% somewhat likely). Surgeons were significantly more likely than other specialists to have already restricted their practice (56% versus 34%, P < 0.0001) and to be planning future restrictions (F = 6.27, P = 0.0003). Solo practitioners were significantly more likely (62%) than specialists based at hospitals (32%) or group practices (42%) to have already restricted their practice (F = 15.68, P < 0.0001), as well to be planning future restrictions (F = 5.59, P < 0.0001). Specialists who had been sued within the last 3 years were also more likely than those who had not been recently sued to be planning future restrictions (F = 3.18, P = 0.02).
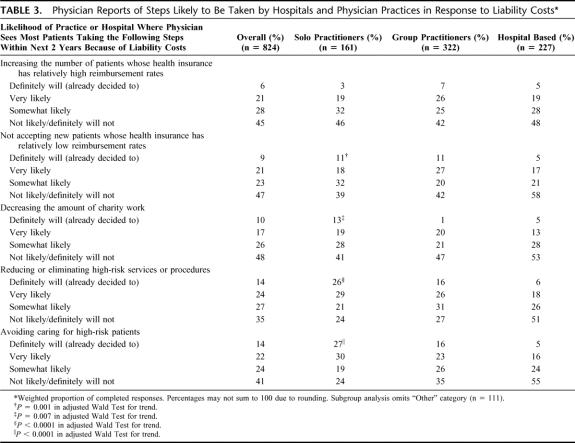
Physician Reports of Steps Likely to Be Taken by Hospitals and Physician Practices
We asked specialists to identify, if known to them, steps that their practice or hospital would likely take in response to liability costs. Nearly two thirds of respondents reported at least some likelihood that their practice or hospital would reduce or eliminate high-risk services, such as delivering babies and performing back surgery within the next 2 years (14% definitely will and 24% very likely) (Table 3). Thirty-six percent reported that their practice or hospital would definitely or very likely avoid “high-risk patients” such as obese persons and women with high-risk pregnancies, with another 24% reporting that they were somewhat likely to do so. The solo practitioner effect was again strong (F = 10.5, P < 0.0001 for high-risk services and F = 11.8, P < 0.0001 for high-risk patients). More than half of all solo practitioners indicated they definitely would or were very likely to reduce or eliminate both high-risk services and high-risk patients. In contrast, less than one fourth of hospital-based physicians reported that their hospitals planned to do so.
TABLE 3. Physician Reports of Steps Likely to Be Taken by Hospitals and Physician Practices in Response to Liability Costs
Many specialists also reported that their practices or hospitals would attempt to meet liability costs by making special efforts to increase revenue. Fifty-three percent of respondents said that their practice or hospital was at least somewhat likely to decline to treat new patients whose health insurance offered relatively low reimbursement rates (30% definitely will or very likely), and 55% said their practice would attempt to increase the number of patients with relatively generous insurance reimbursement (27% definitely will or very likely). Solo and group practitioners were significantly more likely than hospital-based physicians to report that their practices planned to turn away patients with undesirable insurance (F = 4.59, P < 0.0001). Fifty-two percent of specialists reported that their practice or hospital was at least somewhat likely to reduce the amount of charity work (10% definitely will and 17% very likely). Again, the proclivity was much stronger among physician practices than among hospitals (F = 2.96, P = 0.007).
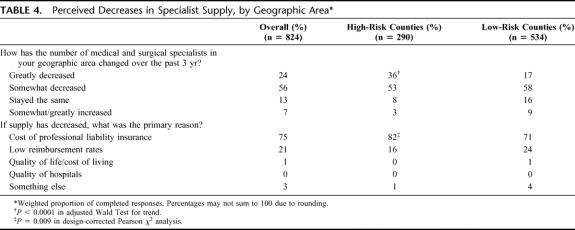
Supply of Specialists
Eighty percent of respondents reported that the supply of medical and surgical specialists in their area had greatly or somewhat decreased in the past 3 years (Table 4). Specialists in high-risk counties were significantly more likely than those in lower-risk areas to report a decrease (F = 16.71, P < 0.0001). Liability insurance costs were identified as the primary reason for the decrease (75%); low reimbursement was a distant second (21%). Surgeons were significantly more likely than other specialists to name liability costs as the primary reason (58% versus 47%, P = 0.04).
TABLE 4. Perceived Decreases in Specialist Supply, by Geographic Area
Patient Access-to-Care Problems
We inquired about 4 measures directly related to patient access to care: driving distances to see a specialist (in any specialty) or get a surgical procedure, waiting times for appointments with specialists or surgical procedures, waiting times in the emergency room, and patients having to switch physicians. A strong majority of specialists reported perceived increases across all 4 indicators over the past 3 years for patients whom they treated (Table 5). For the 2 waiting time measures and the physician switching measure, approximately one third of respondents reported great increases and more than 80% reported at least some increase. Increased waiting times for specialist and surgical appointments were a bigger perceived problem in high-risk counties than low-risk counties, despite the presumably higher baseline supply of specialists in the greater Philadelphia area. There were also notable differences by specialty, with neurosurgeons most likely to report large increases in driving distances and waiting times and obstetrician/gynecologists and orthopedists most likely to report more patients having to switch doctors.
TABLE 5. Perceived Decrements in Patient Access to Care
We probed the relative contributions of liability costs and other potential contributors to access problems by asking respondents to identify what they believe to be the primary reason for each type of reported access problem, from among the following choices: managed care restrictions/health insurance issues; reimbursement levels; professional liability insurance costs; or something else. Their responses indicate that causation is multifactorial, but for increased driving distances and waiting times for specialist and surgical care, professional liability costs are the strongest driver (Table 5). Managed care was reported to be the strongest driver for patients having to switch physicians (61%); but in high-risk counties, liability costs were more frequently cited (53%) as the primary cause than managed care (43%). Surgeons were significantly more likely than other specialists to indicate that liability costs were the primary reason for increased driving distances (P = 0.04), waiting times for specialist and surgical care (P = 0.002), and waiting times in the emergency room (P = 0.002).
DISCUSSION
The results of this survey suggest that the supply of surgical and other specialists in Pennsylvania is likely to decrease, perhaps substantially in some areas, over the next 2 years; that this decrease is attributable primarily to the cost of professional liability insurance; and that it may be contributing to decrements in some measures of patient access to care. Reimbursement and managed care arrangements are contributing to access restrictions, but liability is perceived to be the strongest driver.
Physicians' most prevalent response to liability concerns has been to restrict the scope of practice or decrease the number of practitioners in a group practice who provide high-risk services. A majority of specialists also believe that their practice or hospital will likely avoid caring for high-risk and lower-paying patients. On the basis of these reports, actual and potential access problems appear greatest for patients in need of high-risk services, uninsured patients, and patients whose insurance reimburses specialists relatively meagerly.
Our estimates of the proportions of specialists who have made or are planning to make changes to their practice are generally lower than those of several physician surveys conducted in Pennsylvania by medical professional societies. A national survey of obstetrician/gynecologists found that more than a third of respondents in Pennsylvania had retired, moved their practices out of state, or restricted their practice to exclude obstetric services.7 A survey of Pennsylvania orthopedic surgery practices reported that 17% of the state's orthopedic surgeons had left the state or reduced their surgical services in 2001 to 2002 (reasons for these decisions were not elicited).8 Surveys conducted by provider organizations have been called into question because some have very low response rates and suffer from limited scope, lack of specificity, and other problems.6
In its recent study of 5 “crisis” states, the GAO identified some evidence that the malpractice crisis was affecting access to care but concluded that overall the impact was less severe than provider groups had claimed. In Pennsylvania, the effects appeared to be largely limited to obstetrical and emergency surgical services in certain areas (suburban Philadelphia and some rural areas with preexisting physician shortages).6 The GAO's findings were based on an investigation of a limited number of specific claims of access problems; it did not conduct a statewide access study. It did examine utilization of high-risk services among Medicare patients and found that rates of orthopedic surgeries increased steadily over the past 5 years and mammography rates remained stable, although wait times increased.
The GAO also examined physician licensure data and determined that, notwithstanding the departure of a number of obstetrician/gynecologists from Pennsylvania, a decline in the number of women of childbearing age in the state resulted in stable per-capita supply of obstetrician/gynecologists in 2001 to 2002. Importantly, licensure data do not distinguish physicians who are active in patient care from those who are inactive, or physicians who practice obstetrics from those who practice only gynecology. Studies by the Pennsylvania Medical Society using more sensitive data found that the per-capita supply of general surgeons, obstetricians, orthopedic surgeons, and neurosurgeons has been declining in recent years,9,10 although some trends predate the onset of the current liability crisis and are also visible in states with less severe liability problems.
Studies from previous malpractice crises have generally found that rising liability costs were associated with decisions by obstetricians and family practitioners to stop practicing obstetrics,11–16 with 1 exception.17 More recent studies have demonstrated a significant association between state-level physician supply and caps on noneconomic damages in malpractice cases18,18a (Klick J, Stratmann T. Does medical malpractice reform help states retain physicians and does it matter? [unpublished manuscript, 2003]). Studies of the relationship between physician supply and malpractice insurance premiums have produced mixed findings.18b–19a
Our findings have several implications for healthcare delivery and health policy. First, our results suggest that liability pressures may be leading to greater consolidation of high-risk specialty care services in a smaller number of providers. This is likely to be particularly true for high-technology services that, prior to the onset of this malpractice crisis, had been dispersing out from the academic medical centers to community hospitals. Academic medical centers are relatively well positioned to absorb additional liability expenses and, because of higher prevalence of self-insurance, more secure than community hospitals and community-based physicians in the availability of insurance coverage.20 Whether it is desirable for teaching hospitals to reassume a greater volume of high-risk services is an interesting question. The well-established relationship between surgical volume and outcome21–23 is an argument in favor of this trend, but a key question is whether patients residing in areas distant from teaching hospitals will find services available in their community. The increase in driving distances for specialist services reported in our study suggests that this consolidation may already be resulting in decreased availability in some areas.
Second, we found that solo practitioners were especially likely to be taking steps to reduce their liability risk and change their patient mix to boost revenue. Solo practitioners perceive their liability insurance premiums to be a greater burden than do physicians in other settings, and may encounter more difficulty securing coverage than specialists whose policies are arranged by their hospital. As we have discussed elsewhere,20 the need to find lower-cost insurance may push physicians in solo and small-group practices toward closer relationships with hospitals.
Third, the link between liability insurance costs and supply of specialists points to the need for greater risk pooling across specialties. Pricing malpractice insurance according to the legal risk associated with particular specialties, but experience-rating physicians only minimally (if at all) within specialties, is a byproduct of combining an imprecise litigation system with a fragmented healthcare delivery system. When insurance markets tighten, high-risk specialists suffer disproportionately. Maintaining a socially optimal supply of such specialists may require greater cross-subsidization of premiums within institutions and insurers.
Fourth, our findings suggest that policy interventions may be needed to retain high-risk specialists in states that are experiencing large and rapid rises in malpractice premiums and are not oversupplied with such specialists. This need is particularly acute in markets in which the major healthcare payers are not likely to be amenable to upward adjustments in reimbursement to reflect physicians' increased overhead costs. Among the policy alternatives discussed to date are insurance subsidies, stricter insurance regulation, and reforms to the tort liability system.24–26
Our study has several limitations. First, we did not measure access-to-care problems directly by surveying patients or analyzing trends in utilization, but rather relied on physicians' reports of access problems encountered by patients whom they treated. Physicians may underreport access problems because they are not aware of them or may exaggerate them due to a political interest in casting the malpractice crisis as a public health problem.
We took several steps to minimize over-reporting in this survey. We constructed a sample that would permit comparisons of physicians in high- and low-risk counties; the observed differences suggest that the responses reflect physicians' actual experiences rather than a uniform “party line.” We worded and ordered questions and response categories so as to avoid “leading” respondents to attribute various problems to liability costs. We forced respondents to be specific about the likelihood of and timeframes for making various practice decisions. We asked about behaviors that are not socially desirable, such as avoiding patients with low-paying insurance. Finally, we asked respondents to judge the contribution of liability costs compared with other possible drivers of access problems.
A second study limitation is that our survey was confined to 6 specialties in a single state. Pennsylvania is broadly representative of states in severe tort crisis, but our data are not generalizable to the national level. Finally, because we surveyed physicians listed by the AMA as actively practicing in Pennsylvania, our sample could not capture those who have already left the state.
Further study of the supply of providers in Pennsylvania and other crisis states is desirable to validate the access-to-care problems reported in this survey. If a state is initially oversupplied with medical and surgical specialists, then even substantial decreases in the number of providers may result in only small decrements in patients' ability to access services. Continued empirical study of the malpractice crisis is imperative given the very high political, economic, and public health stakes involved.
ACKNOWLEDGMENTS
The authors thank Carly Kelly, JD, for able research assistance.
Footnotes
Supported by the Project on Medical Liability in Pennsylvania funded by the Pew Charitable Trusts (Grant No. 2002-00279).
Reprints: Michelle M. Mello, JD, PhD, Department of Health Policy and Management, Harvard School of Public Health, 677 Huntington Ave., Boston, MA 02115. E-mail: mmello@hsph.harvard.edu.
REFERENCES
- 1.Sage WM. Understanding the first malpractice crisis of the 21st century. In: Gosfield AG, ed. Health Law Handbook. St. Paul, MN: West Group, 2003. [Google Scholar]
- 2.Mello MM, Studdert DM, Brennan TA. The new medical malpractice crisis. N Engl J Med. 2003;348:2281–2284. [DOI] [PubMed] [Google Scholar]
- 3.Palmisano DJ. The physician's perspective: medical liability reform is essential for access to medical care [speech]. <http://www.ama-assn.org/ama/pub/category/15300.html> (October 3, 2005).
- 4.U.S. Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation. Addressing the New Health Care Crisis: Reforming the Medical Litigation System to Improve the Quality of Health Care. March 3, 2003. <http://aspe.hhs.gov/daltcp/reports/medliab.htm> (October 3, 2005).
- 5.U.S. Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation. Confronting the New Health Care Crisis: Improving Health Care Quality and Lowering Costs by Fixing Our Medical Liability System. July 24, 2002. <http://aspe.hhs.gov/daltcp/reports/litrefm.htm> (October 3, 2005).
- 6.U.S. General Accounting Office. Medical Malpractice: Implications of Rising Premiums on Access to Health Care [GAO-03-836]. Washington, DC: General Accounting Office, 2003. [Google Scholar]
- 7.Hammond CB. Who Will Deliver America's Babies? Remarks on HR 5, the HEALTH Act of 2003. February 6, 2003. <http://www.acog.org/from_home/publications/press_releases/nr02-06-03.cfm> (October 3, 2005).
- 8.Pennsylvania Orthopedic Society. Physician Exodus and Malpractice Insurance Availability Survey. 2002. <http://www.paorthosociety.org/MalpracticeSurvey2PDF.pdf> (October 3, 2005).
- 9.Foreman SE. Physician Manpower in Pennsylvania. Harrisburg, PA: Pennsylvania Medical Society, 2003. [Google Scholar]
- 10.Pennsylvania Medical Society. Southeast Pennsylvania Physician Manpower 2003. Harrisburg, PA: Pennsylvania Medical Society, 2003. [Google Scholar]
- 11.Grumbach K, Peltzman-Rennie D, Luft HS. Charges for Obstetric Liability Insurance and Discontinuation of Obstetric Practice in New York: Report to the Office of Technology Assessment. Washington, DC: Office of Technology Assessment, 1993. [Google Scholar]
- 12.Begneaud WP. Obstetric and gynecologic malpractice in Louisiana: incidence and impact. J Louisiana State Med Soc. 1989;141:27–33. [PubMed] [Google Scholar]
- 13.American College of Obstetricians and Gynecologists. Professional Liability and Its Effects: Report of 1987 Survey of ACOG Membership. Washington, DC: American College of Obstetricians and Gynecologists, 1988. [Google Scholar]
- 14.Rosenblatt RA, Detering B. Changing patterns of obstetric practice in Washington State: the impact of tort reform. Fam Med. 1988;20:101–107. [PubMed] [Google Scholar]
- 15.Bredfeldt R, Colliver JA, Wesley RM. Present status of obstetrics in family practice and the effects of malpractice issues. J Fam Pract. 1989;28:294–297. [PubMed] [Google Scholar]
- 16.Smith MA, Green LA, Schwenk TL. Family practice obstetrics in Michigan: factors affecting physician participation. J Fam Pract. 1989;28:433–437. [PubMed] [Google Scholar]
- 17.Rosenblatt RA, Wright CL. Rising malpractice premiums and obstetric practice patterns: the impact on family physicians in Washington State. West J Med. 1987;146:246–248. [PMC free article] [PubMed] [Google Scholar]
- 18.Encinosa WE, Hellinger FJ. Have state caps on malpractice awards increased the supply of physicians? Health Aff (Millwood). May 31, 2005. [DOI] [PubMed]
- 18a.Kessler DP, Sage WM, Becker DJ. Impact of malpractice reforms on the supply of physician services. JAMA. 2005;293:2618–2625. [DOI] [PubMed] [Google Scholar]
- 18b.Gius MP. An examination of the determinants of physicians supply at the state level. J. Business and Economic Studies. 2000;6:73–79. [Google Scholar]
- 19.Baicker K, Chandra A. The effect of malpractice liability on the delivery of health care. In: Cutler DM, Garber AM, eds. Frontiers in Health Policy. Cambridge, MA: MIT Press; 2005. [Google Scholar]
- 19a.Erus BB. Malpractice liability crisis and physician location choice. 2004. Located at Northwestern University Working Paper, Evanston, IL.
- 20.Mello MM, Kelly CN, Studdert DM, et al. Hospital's behavior in a tort crisis: observations from Pennsylvania. Health Aff. 2003;22:225–233. [DOI] [PubMed] [Google Scholar]
- 21.Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–1137. [DOI] [PubMed] [Google Scholar]
- 22.Epstein AM. Volume and outcome: it is time to move ahead. N Engl J Med. 2002;346:1161–1164. [DOI] [PubMed] [Google Scholar]
- 23.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med. 2002;137:511–520. [DOI] [PubMed] [Google Scholar]
- 24.Bovbjerg RR, Bartow A. Understanding Pennsylvania's Medical Malpractice Crisis: Facts about Liability Insurance, the Legal System, and Health Care in Pennsylvania. Philadelphia: Pew Charitable Trusts, 2003. <http://medliabilitypa.org/research/report0603/UnderstandingReport.pdf> (October 3, 2005).
- 25.Studdert DM, Mello MM, Brennan TA. Medical malpractice. N Engl J Med. 2004;350:283–292. [DOI] [PubMed] [Google Scholar]
- 26.Struve CT. Expertise in Medical Malpractice Litigation: Special Courts, Screening Panels, and Other Options. Philadelphia: Pew Charitable Trusts, 2003. <http://medliabilitypa.org/research/struve1003/> (October 3, 2005).