Abstract
Objective:
To evaluate the outcome of an aggressive surgical approach for duodenopancreatic neuroendocrine tumors (PETs) associated with multiple endocrine neoplasia type 1 (MEN1).
Summary Background Data:
The management of PETs is still controversial in the setting of the autosomal dominant inherited MEN1 syndrome.
Methods:
MEN1 patients that had either biochemical evidence of functioning PETs or visualized nonfunctioning PETs larger than 1 cm in size on imaging were operated. Since 1997, patients were followed annually by biochemical testing and imaging studies.
Results:
Twenty-six genetically confirmed MEN1 patients underwent duodenopancreatic resection for functioning (n = 17) or nonfunctioning (n = 9) PETs. Ten (38%) patients had malignant PETs as characterized by the presence of lymph node (10 patients) and/or distant metastases (2 patients). The surgical approach was selected based on the type, location, and size of PETs. Four Zollinger-Ellison syndrome (ZES) patients required pylorus preserving pancreaticoduodenectomy (PPPD) as initial or redo procedure, 20 patients underwent other duodenopancreatic resections, and 2 patients had simple enucleations of PETs. After median 83 months (range, 5–241 months), 24 patients were alive and 2 patients died of an unrelated cause. All patients with insulinoma or vipoma and 7 of 11 patients with ZES were biochemically cured, including the ZES patients who underwent PPPD. However, 19 of 26 (73%) patients developed new small PETs (<1 cm) in the pancreatic remnant, but no patient had yet detectable metastases on imaging.
Conclusions:
Early and aggressive surgery of PETs in MEN1 patients prevents the development of liver metastases, which are the most life-threatening determinant. PPPD might be the procedure of choice for MEN1–ZES, which has to be proven in large scale studies.
An early aggressive surgical approach for MEN1-associated pancreaticoduodenal endocrine tumors prevents the development of liver metastases, which are the major life-threatening determinant in patients with MEN1 syndrome.
Multiple endocrine neoplasia type 1 (MEN1) is an autosomal dominant inherited syndrome caused by mutations of the MEN1 tumor suppressor gene on chromosome 11q13.1 MEN1 is characterized by the combined occurrence of primary hyperparathyroidism (>90%), duodenopancreatic endocrine neoplasms (65%–75%), and tumors of the anterior pituitary gland (30%–65%).2 Adrenal tumors and neuroendocrine tumors of the thymus, bronchus, or stomach are associated less frequently.2,3 The pancreaticoduodenal endocrine tumors (PETs) are of outstanding interest because malignant PETs represent the most common cause of death in the MEN1 syndrome.4,5 PETs can consist of single or multiple benign or malignant neoplasms, some of which are functional, eg, gastrinoma, causing specific hormonal syndromes. Nonfunctional PETs occur in more than 50% of MEN1 patients with PETs followed by functional PETs, such as gastrinomas and insulinomas that account for about 30% and 10% of MEN1-associated PETs, respectively.6 PETs in MEN1 most frequently become symptomatic in the fourth or fifth life decade, although the biochemical abnormalities and tumor formation often develop much earlier.7 Indeed, it has been shown that syndromes based on hormonal excess may be late features of the endocrinopathy and, when developed, indicate the presence of distant metastases in more than one third of patients.8
The management of MEN1-PETs, especially of gastrinomas, is a highly controversial issue.9 Some groups have advocated a nonoperative approach for the Zollinger-Ellison syndrome (ZES) and use proton pump inhibitors to control the effects of hypergastrinemia.10,11 Other groups recommend an operative approach if the tumor reaches 3 cm in size, since the risk for liver metastases then increases significantly.12,13 Conversely, we and other groups recommend surgery if the biochemical diagnosis is unequivocal, even without other signs or symptoms.7,14 There is not only disagreement about the indication of surgical exploration but also about the type of operation, with differences primarily whether distal pancreatectomy or pylorus-preserving pancreaticoduodenectomy (PPPD) should be done. The management of hypoglycemia and other syndromes (eg, vipoma) is less controversial. Surgical treatment is generally recommended, although a standardized technique has not been generally adopted. There are only very few data on the management on imaged nonfunctional PETs in MEN1. Since it has been shown that there is no correlation between primary tumor size and the presence of metastases,15 some groups advocate pancreatic resection, even for small asymptomatic imageable nonfunctional PETs.7,14 The rationale for an aggressive approach is based on the fact that PETs have significant malignant potential and that the functional manifestations can actually be eliminated with an appropriate procedure.16 We prospectively analyzed our strategy of an aggressive surgical approach in MEN1-associated PETs and reevaluated a genotype/phenotype relation for MEN1 PETs that might facilitate the therapeutic approach for these lesions in the future.
MATERIALS AND METHODS
Forty-two patients with genetically confirmed MEN1 were treated at the Department of Surgery, Philipps-University Marburg, Marburg, Germany between 1981 and December 2004. The clinical records of the patients were prospectively collected and analyzed with special regard to patient demographics, clinical features, preoperative and postoperative imaging, operative procedures, pathologic findings, and follow-up. Thirty-six (86%) MEN1 patients had PETs, of whom 26 patients underwent surgery and the other 10 patients with PETs are still under close surveillance. Since 1997, the majority of patients were followed annually by biochemical testing, abdominal computed tomography, endoscopic ultrasonography, and somatostatin-receptor-scintigraphy at our hospital, and the follow-up resulted from the most recent examination. In this study, we focused on the outcome of duodenopancreatic surgery in the 26 operated patients.
The diagnosis of ZES was established by clinical symptoms, an elevated fasting serum gastrin level (>125 pg/mL), a positive secretin stimulation test defined as an increase of serum gastrin concentration to >200 pg/mL together with low pH in the stomach, and a positive immunohistochemistry for gastrin of the tumor. The diagnosis of insulinoma required a symptomatic hypoglycemia (<40 mg/dL) with concomitant endogenous hyperinsulinism (>20 μU/mL) during a supervised fasting test and a positive immunohistochemistry for insulin of the tumor. The diagnosis of vipoma was confirmed by watery diarrhea (>6 L/day) and a fasting vasoactive intestinal polypeptide serum concentration >130 pg/mL. Lesions were considered as nonfunctioning PETs if there were no clinical symptoms of hormonal excess present and plasma hormone levels despite those of pancreatic polypeptide were within normal limits. Malignancy was determined on the basis of strict criteria of infiltrating growth, lymph node, or distant metastases.
MEN1 patients who fulfilled the criteria of ZES or hyperinsulinism underwent laparotomy after diffuse liver metastases were excluded by preoperative imaging. Patients with nonfunctional PETs were scheduled for exploration if the tumor size was >1 cm in diameter and diffuse liver metastases were excluded by imaging. Preoperative imaging routinely comprised thin-sectioned abdominal computed tomography, somatostatin receptor scintigraphy, and endoscopic ultrasonography. Bidigital palpation of the pancreas and intraoperative ultrasonography was performed in all patients. For ZES, a distal pancreatic resection to the level of the portal vein with enucleation of any tumors in the pancreatic head, a duodenotomy with excision of any tumors in the first to fourth portion of the duodenum and a peripancreatic lymph node dissection as suggested by Thompson17 was routinely performed until 1997. Since then, we prefer a PPPD with lymphadenectomy when the source of gastrin secretion could be regionalized to the pancreatic head region by preoperative selective arterial secretin injection angiography.18 Singular benign insulinomas or nonfunctional PETs were enucleated. In case of multiple tumors, a distal pancreatic resection to the level of the portal vein with enucleation of tumors out of the pancreatic head was performed. Malignant tumors were treated by pancreatic resection with regional lymph node dissection. In all types of PETs, synchronous liver metastases were resected simultaneously.
Abdominal reoperations were necessary for new developed PETs or metastases in 8 (31%) patients in this series. The specific reoperation performed was dependent on pattern of disease recurrence, as identified by imaging studies. Reoperative cases involved enucleation of the tumor(s) in pancreatic head or neck, distal pancreatic resection, duodenotomy with tumor excision, PPPD, or resection of metastases alone.
Cure of ZES was defined as a normal fasting gastrin concentration (<125 pg/mL) and a negative secretin stimulation test postoperatively and at annual follow-up investigations. Insulinoma was considered to be cured when fasting serum glucose levels were >40 mg/dL and concomitant insulin levels were <20 μU/mL. Nonfunctional PETs were considered to be cured if there was no evidence of tumor upon imaging studies.
MEN1 gene mutation analysis was performed by Taq cycle sequencing using an automated sequencer (ABI 310 Genetic Analyzer, Perkin Elmer) as described previously by our group.14 Patients’ genotype (type and localization of MEN1 mutation) and PETs phenotype, including age at initial diagnosis, number and type of tumors, rate of histologically verified malignancy, and disease-free interval, were compared using the χ2 test and Mann-Whitney U test. A value of P < 0.05 was considered to indicate statistical significance.
RESULTS
Clinical Characteristics and Pathology
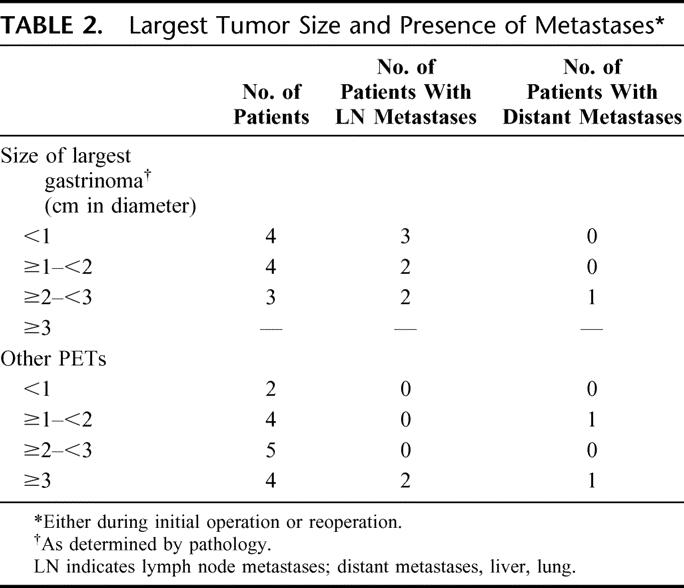
Among the 26 MEN1 patients who underwent surgery for PETs were 15 men and 11 women with a median age of 38 years (range, 13–68 years) at the time of initial operation in our institution. Initially, 11 patients (42%) had ZES, 5 patients (19%) had organic hyperinsulinism, whereas 1 additional patient developed hyperinsulinism 149 months after ZES, 1 patient (4%) had a vipoma, and 9 (35%) patients had only nonfunctioning PETs, respectively (Table 1). Twenty patients (77%) had multiple PETs (up to 11) and in 6 patients (23%) a single tumor was found (Table 1; Fig. 1). At the time of initial surgery, 1 of 11 (9%) ZES patients had duodenal gastrinomas alone, 2 of 11 (19%) had only pancreatic gastrinomas, whereas 8 of 11 (72%) ZES patients had synchronous duodenal gastrinomas and additional nonfunctioning endocrine pancreatic tumors. All other patients had only pancreatic tumors. Ten (38%) patients had histologically verified malignant tumors as characterized by the presence of lymph node (10 patients) and/or distant metastases (2 patients) (Table 2). The median largest tumor size of all patients was 29 mm (range, 3–250 mm). In ZES, the median tumor size was 12 mm, ranging from 3 mm to 25 mm. Lymph node metastases were present in 7 of the 11 ZES patients regardless the tumor size, whereas a liver metastasis was present in only 1 ZES patient with a 25-mm-sized pancreatic gastrinoma. In the 6 patients with other functioning PETs, the median tumor size was 57 mm, ranging from 5 mm to 250 mm. All 5 patients with insulinomas had benign tumors. The patient with a 250-mm-sized malignant vipoma developed 3 local recurrences and a metachronous liver metastasis. Seven of 9 patients with nonfunctional PETs had benign tumors with a median largest tumor diameter of 31 mm (range, 8–110 mm). Altogether, in this series no correlation between tumor size and metastatic potential was evident (P > 0.5), neither for ZES nor the nonfunctioning PETs.
TABLE 1. Clinical Characteristics of 26 MEN1 Patients Undergoing Surgery for PETs
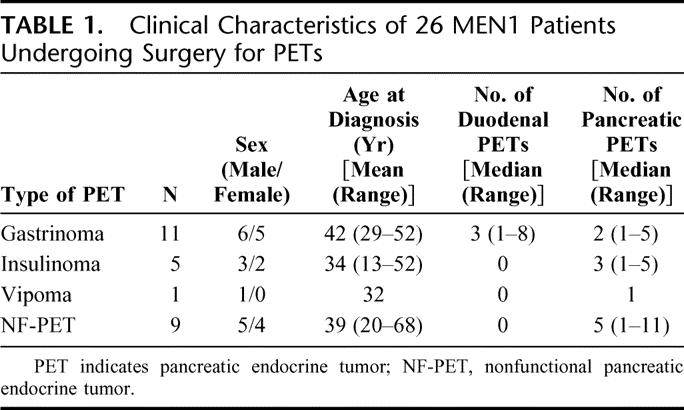

FIGURE 1. Specimen of distal spleen-preserving pancreatectomy from an MEN1 patient with multiple NPTs. Eleven PETs were identified by histopathology, the largest measuring 11 mm in size.
TABLE 2. Largest Tumor Size and Presence of Metastases
Initial Operative Procedures, Reoperations, and Complications
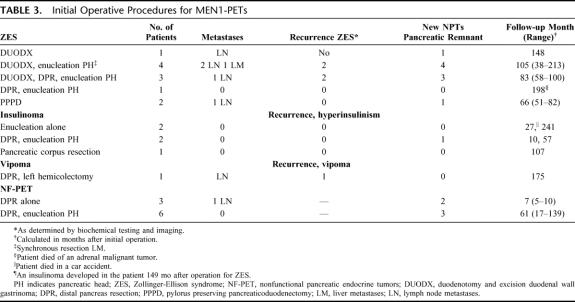
In 26 patients, 36 operations were performed: 26 initial operations and 10 reoperations. Two of 11 patients with ZES had their first duodenopancreatic resection, distal pancreatic resection, or partial duodenal resection at another institution. In addition, another 3 ZES patients had previous laparotomies at other institutions, including gastric acid-reducing surgery or surgery for duodenal ulcer perforations. ZES patients underwent duodenotomy with excision of duodenal gastrinomas as initial procedure alone, duodenotomy together with enucleation of pancreatic tumors, and/or distal pancreatic resection. PPPD was performed in 2 patients as the initial procedure (Table 3).
TABLE 3. Initial Operative Procedures for MEN1-PETs
The 5 patients with insulinoma were treated by tumor enucleation, pancreatic corpus resection, or distal pancreatic resection together with enucleation of nonfunctioning pancreatic head tumors (Table 3). The patient with the large malignant vipoma had a splenopancreatectomy with left colectomy as the initial procedure. All 9 patients with nonfunctioning PETs (Table 3) were treated with distal pancreatic resections, 6 of those with the spleen-preserving variant. Six patients also underwent enucleation of PETs out of the pancreatic head.
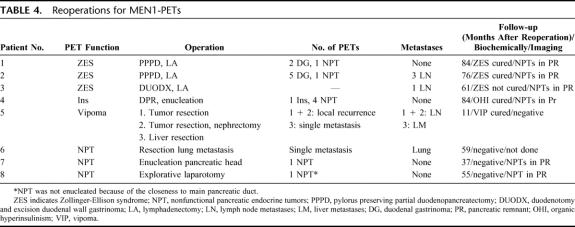
In 8 patients, reoperations were performed. Three ZES patients underwent reoperations because of recurrence of ZES 35, 39, and 41 months after initial operation, respectively (Table 4). In 2 patients, a PPPD was performed; in the third patient, a lymph node metastasis was resected. One patient developed an insulinoma after her operation for ZES. During reoperation, a distal pancreatic resection together with enucleation of 2 pancreatic head tumors had been performed. The patient with the malignant vipoma underwent 3 reoperations for local recurrences and a liver metastasis 90, 144, and 164 months after initial operation, respectively. Three patients with nonfunctional PETs underwent reoperations because of metastases or new developed nonfunctional PETs 1, 12, and 21 months after their initial operation (Table 4).
TABLE 4. Reoperations for MEN1-PETs
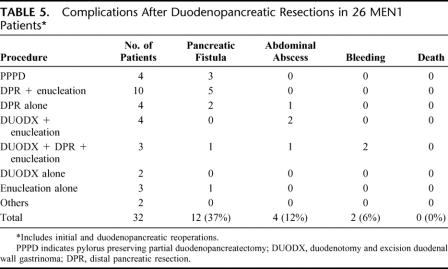
None of the 26 patients died during the perioperative period. Fifteen of 26 (58%) patients developed postoperative complications (Table 5). The most frequent complication was transient pancreatic fistula that occurred after 12 of 32 pancreatic (37%) procedures. All fistulas could be managed without reoperation. Three of the 26 patients (11%) had to undergo reoperation in the early postoperative period because of abdominal abscess (n = 2) or bleeding (n = 1). Only 1 of 26 (4%) patient developed pancreoprivic diabetes mellitus after his second operation.
TABLE 5. Complications After Duodenopancreatic Resections in 26 MEN1 Patients
Follow-up, Surveillance, and Outcome
Seven of 11 (77%) patients operated for ZES are biochemically cured after a median follow-up of 123 months (range, 38–213 months). Four of these 7 patients underwent PPPD either as initial or reoperative procedure. In contrast, all 4 patients with recurrent ZES underwent local excision of duodenal gastrinomas as the initial procedure. However, none of the 4 patients with biochemical recurrence of ZES has yet developed imageable metastases, especially no liver metastases.
All 5 patients with insulinoma have been rendered euglycemic and asymptomatic after a median follow-up of 88 months (range, 10–241 months). The patient with malignant vipoma has no evidence of disease 175 months after his initial operation and 11 months after his last of 3 reoperations. None of the 9 patients with nonfunctional PETs developed a functioning PET or imageable metastases after a median follow-up of 43 months (range, 5–139 months). However, 19 of 26 (73%) patients developed new small PETs (<1 cm) in the pancreatic remnant or duodenum during follow-up as determined by biochemical testing or visualized by endosonography. Newly developed PETs included ZES in 1 patient, insulinoma in 1 patient, and nonfunctional PETs in 17 patients, respectively. The size of visualized PETs ranged from 2 mm to 11 mm. So far, no patient with new NPTs has detectable lymph node or distant metastases on imaging. Altogether, after a median follow-up of 83 months (range, 5–241 months), no patient had died because of MEN1-related PETs. Twenty-four of 26 (96%) patients were alive; 2 patients were deceased for unrelated causes.
Genotype-Phenotype Comparisons
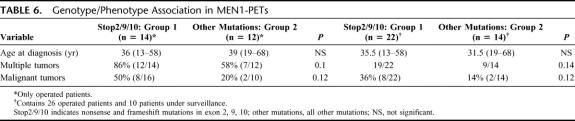
MEN1 gene mutation analysis identified the causative mutation in all 26 patients who underwent surgery and also in the 10 patients whose PETs are still under surveillance. Twenty-five different MEN1 gene mutations distributed throughout the gene could be identified, including 18 frame shift, 3 nonsense, 2 missense, and 2 splice-donor site mutations. Based on a previous report,14 we evaluated genotype/phenotype association between patients with truncating nonsense or frame shift mutations in the N- or C-terminal regions (exons 2, 9, 10 = group 1) of the MEN1 gene and patients with other mutations (group 2). Patients of group 1 tended to have a higher rate of malignant tumors (50% versus 20%, P = 0.12) and a higher rate of multiple tumors (86% versus 58%, P = 0.1) than patients of group 2 (Table 6). This tendency holds true, if one includes the 10 patients under surveillance with small NPTs without imageable signs of malignancy. There was no difference between both groups regarding the age at initial diagnosis, location and size of tumors, and survival. Notably, 7 of 8 gastrinomas of group 1 were malignant, whereas all 3 gastrinomas of group 2 were benign with yet no recurrence.
TABLE 6. Genotype/Phenotype Association in MEN1-PETs
DISCUSSION
Understanding the natural history and course of PETs associated with the MEN1 syndrome is of paramount importance to an effective clinical screening program and therapeutic intervention strategies aimed at improved patient outcome. Studies of resected specimens and autopsy studies in MEN1 patients have confirmed the presence of preneoplastic changes, such as diffuse islet cell hyperplasia and multiple microscopic foci of neuroendocrine tumors, in virtually all affected patients.19,20 We can confirm these data, since 86% of our MEN1 patients had imageable PETs. However, the PETs are clinically insignificant for a long, yet not determinable period of time in the majority of MEN1 patients. Thus, the issue of surgery for MEN1-related PETs is still highly controversial. This gets even more complicated, since the availability of predictive genetic testing,1,21 the routine use of systematic biochemical testing7 and endosonography22,23 results in the detection of PETs on average in patients in their mid 20s.
Since total pancreatectomy is not justified given the excellent 10-year survival for MEN1-PETs of over 85%,24 many experts recommend a more conservative surgical approach based on the notion that there is a relation between the size of tumors and the development of liver metastases, at least in gastrinomas. One study demonstrated that gastrinomas larger than 3 cm in size had a 10 times higher risk of liver metastases than smaller tumors (40% versus 4.8%).25 Based on these data, some groups suggest that an operation is only indicated if the tumor size of gastrinomas or nonfunctional PETs extends 3 cm. However, another retrospective study of 48 MEN1 patients could not confirm a correlation between tumor size and the presence of metastatic disease in MEN1-PETs.15 The present study also showed no obvious correlation, especially since 2 patients with small (15 mm and 25 mm) PETs developed distant metastases.
It has been shown that MEN1-ZES patients with liver metastases have a significantly shorter survival than those without (96 versus 30 months)26 and that liver metastases occur in only 3% of patients with ZES managed surgically compared with 23% of those managed conservatively.27 Thus, liver metastases are the unequivocal life-determining variant in MEN1-PETs, especially in gastrinoma. Therefore, we and others have advocated a more aggressive surgical strategy.7,14,17,28 We see an indication for duodenopancreatic resections in MEN1 patients that either have biochemical evidence of functioning PETs or visualized nonfunctioning PETs larger than 1 cm in size on imaging if diffuse distant metastases are excluded on imaging. The objective of this approach is to detect and remove potentially malignant tumors when patients are asymptomatic before malignant transformation and metastatic spread to local and distant sites occurs. Since the majority of MEN1 patients, 73% in our series, developed new PETs in the pancreatic remnant after surgery, it is not the goal to cure but to control pancreaticoduodenal disease by preventing the development of metastases. Data of the Uppsala group support this rationale, since it showed a tendency toward a reduced death rate in patients who undergo early surgery.7
This aggressive surgical approach based on predictive genetic testing and regular surveillance does not only prevent the development of liver metastases, it might also result in a higher cure rate of MEN1-ZES because the tumors and their lymph node metastases were resected at the earliest possible stage. None of our 11 ZES patients developed postoperative liver metastases, and 55% (7 of 11) had a negative secretin test after a median follow-up of 104 months. This is an extraordinary cure rate compared with the data in the literature ranging between 0% and 30%.16,24 Another reason for our results might be the introduction of PPPD as the first-line procedure if the gastrin source could be regionalized to the pancreatic head region preoperatively. The rationale for this approach is that more than 90% of gastrinomas occur in the duodenum29; thus, recurrence is impossible if the organ of origin is removed. In the present study, all 4 patients who underwent PPPD as initial or redo procedure are biochemically cured 4 to 7 years after surgery, compared with only 3 of 7 patients who underwent only local excision and/or distal pancreatic resections. The limited data on PPPD for MEN1-ZES reported in 11 small-scale studies29–39 seem to confirm our results, since 17 of 21 (80%) MEN1-patients with ZES were cured after a minimum follow-up of 1 year. On the other hand, partial duodenopancreatectomy is a more demanding procedure and expected to have a higher morbidity and mortality than duodenal excisions and/or distal pancreatectomy. Furthermore, reoperation, which is often required in MEN1 patients, might be more difficult after PPPD, especially when there has been a pancreatic leak. At present, before a routine use of PPPD can be recommended, 2 important issues need to be clarified in prospective controlled large-scale studies. First, it should be established that PPPD really leads to increased long-term cure in MEN1-ZES, established by complete biochemical assessment, including the secretin test. Second, long-term side effects (>10 years) of PPPD and their frequency need to be carefully assessed because these are largely unknown.
The management of other functioning PETs such as insulinoma is less controversial, since there is no good medical option to adequately control the symptoms of hormonal excess. Surgical resection is generally recommended, even if no tumor is detectable by preoperative imaging, as long as diffuse metastatic disease is excluded. Most authors recommend distal pancreatic resection to the level of the portal vein with preservation of the spleen and enucleation of PETs of the pancreatic head in the case of multiple tumors or enucleation in the case of a single PET. Compared with MEN1-ZES, the reported cure rates of this approach for MEN1-associated organic hyperinsulinism are excellent, ranging from 83% to 100% after follow-up as long as 15 years.17,40,41 The present study confirms these data, since all 6 MEN1 patients with organic hyperinsulinism are cured after a median follow-up of 88 months.
There are very little data about the management of nonfunctional PETs in MEN1.7,17,42 There are several special facts and unresolved questions regarding this issue. Nonfunctional PETs are asymptomatic, are often multiple, and occur in up to 85% of MEN1 patients as in our cohort of patients (36 of 42). The growth rate of nonfunctional PET as well as their metastatic potential remain to be established. Metastatic spread even to distant sites has rarely been observed also in small tumors (<2 cm in size), as in 1 of 9 patients in our study.15,26,42 However, no distant metastases have yet described in nonfunctional PETs <10 mm in size, which is confirmed by our results. None of the 7 patients with nonfunctional PETs smaller than 10 mm had lymph node or distant metastases. Therefore, we and others recommend an aggressive surgical approach to prevent the development of metastases if the largest tumor size exceeds 10 mm on imaging.8,17,42 This includes distal pancreatic resection to the level of the portal vein and enucleation of PETs in the pancreatic head. We agree with others8 that the spleen can be preserved in patients with small PETs that are not suspicious for malignancy. In tumors more than 2 cm in size or tumors with suspected malignancy, splenectomy should be performed to excise the lymph nodes from the splenic hilum, which are a frequent location of metastases. However, one has to keep in mind that this strategy does only control but not cure pancreatic disease in MEN1, since in the present study 73% (19 of 26) of patients developed new nonfunctional PETs during follow-up.
Major duodenopancreatic resection or enucleation in this series was associated with a relatively high incidence of complications (55%) but no incidence of perioperative death. Patients with MEN1 generally have soft, normal pancreatic glands, making the performance of pancreaticoenteric anastomoses or suturing of the resection margin challenging. Thus, the incidence of pancreatic fistula (37%) in this series was 3 times higher compared with results in pancreatic surgery for exocrine pancreatic diseases, but in the range of that of other recent reports.43–45 Fortunately, no patient required reoperation for pancreaticobiliary fistula. Thus, it is fair to say that duodenopancreatic resection in MEN1 carries a significant risk of operative morbidity. The young age and overall excellent physiologic reserve of patients are definitely optimal preconditions to overcome complications after duodenopancreatic surgery, so that perioperative mortality is <2% in specialized centers.17,37,38,42
Initial studies revealed no evidence for a genotype-phenotype correlation in MEN1, but these analyses did not focus on the individual tumor types.1,46 Our group recently suggested a potential genotype-phenotype association in MEN1-related PETs.14 Patients with truncating nonsense or frameshift mutations in the N- or C-terminal region of the MEN1-gene (exons 2, 9, and 10) had a significantly higher rate of malignant tumors than patients with other mutations (P < 0.02). This association was underscored by the findings of Kouvaraki et al.47 We also realized this correlation in MEN1-associated adrenal tumors.3 The evaluation of this potential genotype-phenotype correlation in the extended number of patients in this series revealed not longer statistical significance, but patients with truncating mutations of exons 2, 9, and 10 still tended to have a higher rate of malignant PETs (P = 0.12) and a higher rate of multiple PETs (P = 0.1) than patients with other mutations. This was especially noted in gastrinomas, since 7 of 8 gastrinomas of patients with truncating mutations of exons 2, 9, and 10 were malignant, whereas all 3 gastrinomas of patients with other mutations were benign with yet no recurrence. Functional studies of the MEN1 gene underscore our observation, as it could be demonstrated that mutations in the N- or C-terminal region are very important by disturbing the function of the protein menin, encoded by the MEN1 gene, as a transcriptional repressor through interaction with the transcription factor JunD.48 This potential genotype-phenotype correlation deserves further evaluation in a large-scale study because it might have clinical implications for the management of MEN1-PETs.
CONCLUSION
Early and aggressive surgery of PETs in MEN1 might achieve higher cure rates for ZES patients and prevent the development of distant metastases, which are the unequivocal life-threatening determinant. However, new mainly nonfunctioning PETs arise frequently in the pancreatic remnant during long-term follow-up. PPPD might be the procedure of choice for MEN1-ZES, which has to be proven in large controlled long-term studies.
Discussions
Dr. Izbicki: Chairmen, Dr. Fendrich, dear members and guests, I congratulate the authors with this very nice study on the difficult group of MEN1 patients. We like to thank the authors for the opportunity to review this paper and your prompt submission of the complete manuscript for this review.
You have presented your radical surgical approach to MEN-1-associated pancreaticoduodenal endocrine tumors to prevent potentially lethal metastasis of the liver. My major comment for these difficult to treat patients is that, due to the long period you have covered in your study, various treatment strategies have been employed over time, resulting in rather low number of patients in each group rendering universal conclusions as rather difficult.
I have several questions:
In your study, you are focusing on 26 surgical patients that were isolated from a group of a total of 36 patients with pancreatic endocrine tumors. The remaining 10 patients are under close surveillance. What was your rationale to exclude these patients from your radical approach and what does your surveillance program look like?
In how many cases did you perform diagnostic selective arterial secretin injection in addition to routine endosonography for localization of duodenal gastrinomas? In other words, in how many cases was endosonographic localization not successful?
You say that some tumors (although obviously not significant due to the size below 5 mm) were not enucleated because of their “closeness to the main pancreatic duct.” Would this not be a good indication to perform either a classic duodenum preserving pancreatic head resection or a middle segmental pancreatectomy depending on tumor localization?
You only stated concomitant duodenal gastrinomas with non-functioning parenchymal tumors in 8 patients. How often did you encounter concomitant duodenal and parenchymal functioning endocrine tumors, and what was the exact localization of your gastrinomas in Zollinger-Ellison patients?
Once again, thank you and the society for giving me the opportunity to review this interesting paper.
Dr. Fendrich: Thank you, Dr. Izbicki, for your comments.
Regarding your first question, we have 42 patients who are treated in our department because of their MEN-1-related tumors. Thirty-six patients had PETs, of whom 26 patients underwent surgery and the other 10 patients with PETs are under close surveillance. The 26 patients who underwent surgery fulfilled our criteria to operate. They either had a functional tumor syndrome or nonfunctioning tumor(s) >1 cm in size. The other 10 patients are under close surveillance because they all have nonfunctioning PETs, which are smaller than 1 cm. So some of them will undergo surgery during the next few months or years, after fulfilling the above-mentioned criteria. Therefore, we did not exclude any patients because of advanced local disease or diffuse liver metastases. The annual follow-up includes biochemical testing for different hormones and markers, including functional tests, eg, secretin stimulation test for ZES patients, endoscopic ultrasonography, and somatostatin receptor scintigraphy. Every 3 years, the patients undergo MRI of the brain to evaluate the presence of a pituitary adenoma and thoracic computed tomography for the screening of NETs of the lung and thymus. But, of course, screening should be adapted to individual patient needs.
We do selective arterial secretin injection (SASI) in patients with ZES to regionalize the source of gastrin secretion. If the source is regionalized to the pancreatic head region, the patients will be scheduled for PPPD. Endoscopic ultrasound is not the method of choice to detect duodenal gastrinomas; in fact, the best way to detect them is duodenotomy. EUS failed to detect duodenal gastrinomas in more than half of our ZES patients.
I agree that a classic duodenum preserving pancreatic head resection could be a good choice for patients with only nonfunctioning tumors in the pancreatic head, confirmed by IOUS. Both patients where we did not enucleate the tumors, because of their closeness to the main pancreatic duct, had previously undergone a distal pancreatic resection. So a duodenum preserving pancreatic head resection would lead to a functional total pancreatectomy, which is definitely not indicated because of one small nonfunctioning tumor. A pancreatic corpus resection is probably not a good choice for MEN1 patients since the morbidity is higher compared with the left pancreatectomy and the majority of MEN1 patients also have small PETs in the pancreatic tail.
At the time of initial surgery, 1 ZES patient only had duodenal gastrinomas, 2 ZES patients had only pancreatic gastrinomas, whereas 8 of 11 ZES patients had synchronous duodenal gastrinomas and additional nonfunctioning endocrine pancreatic tumors. Norton and colleagues have shown recently how important the routine duodenotomy is in patients with ZES. In nearly every patient with ZES, some duodenal gastrinomas can be found and removed. Additionally, all pancreatic tumors, detected by EUS or IOUS, should be removed because you cannot be sure if there are one or more gastrin sources. As mentioned, we are regionalizing by SASI and then perform a PPPD if the gastrin source is in the pancreatic head/duodenum.
Dr. Brennan: I enjoyed your paper, and I have one comment and 2 questions.
You were careful in your conclusions not to use the word cure, but you use cure a lot during the talk. This disease is incurable; it is a hereditary disease. You had an 8-year follow-up, but most of those patients presented at 30 or 40 years old, it has taken them 40 years to get there. In this disease, 8 years’ follow-up is 8 years’ follow-up; we followed a number of patients with malignant disease more than 10 years with metastasis that do not progress; that presupposes it takes a very long time to develop.
My first question is: the patient you present had multiple tumors in the pancreas and has one functional tumor. How do you identify which tumor is the functional one? The greatest risk is that if you take out only the large tumors, you do a lovely operation and the next day the patient is hypoglycemic.
Second, is the dichotomy in your conclusions for the nonfunctional? Nine of 9 have already occurred, or are known to have persistent disease, and yet you argue at the beginning that anything less than 1 cm should not be resected, but when they recur and they are less than 1 cm, then you follow them. How you decide who gets a reoperation? It is clearly different than the first operation.
Dr. Fendrich: Dr. Brennan brought up a very important fact. Actually, it is very difficult to identify which is the functional tumor among nonfunctioning tumors. Therefore, if you detect multiple pancreatic tumors by EUS or IOUS, never enucleate only one but perform a distal pancreatic resection to the level of the portal vein with enucleation of tumors out of the pancreatic head. With this strategy, we had no recurrence for organic hyperinsulinism. We already discussed our strategy regarding the ZES patients.
The second question was about reoperations. We reoperate patients with nonfunctional tumors for the same criteria as for the initial operation. The patients come to an annual follow-up, and if they have developed a new nonfunctional tumor larger than 1 cm, we schedule the patients for reoperation. But I would like to mention one important fact. In my opinion, it is very important to explain your strategy to the patients. They have to trust you. MEN-1 is a very rare tumor syndrome, and these patients have to deal with it for their whole life. So along with the clinical indications for reoperation, it is necessary to see the patients in relation to their profession, family, and social life. We should not forget that we still know very little about this tumor syndrome, and we are far away from practicing evidence-based medicine.
Dr. Frilling: Mutations in Menin gene, localized on the chromosome 11, have been identified as the underlying genetic cause of the MEN1 syndrome. Do you have any data on the genotype and phenotype correlation in your patients? Are there specific MEN1 mutations known that might be associated with a more aggressive course of the disease? If so, this would imply that a patient with a certain MEN1 genotype should be treated more radically or even prophylactically comparable with the management of patients with MEN 2 syndrome.
It has been shown that Ki-67 is an excellent prognostic predictor in several endocrine tumors. Could you imagine that endoscopically performed fine needle tumor biopsy with consecutive determination of a Ki-67 labeling index could contribute to further characterization of a hormonal inactive endocrine pancreatic tumors in terms of possible malignancy?
Dr. Fendrich: Five years ago, our group suggested a potential genotype-phenotype association in MEN1-related PETs. We found that patients with truncating nonsense or frameshift mutations in the N- or C-terminal region of the MEN1 gene had a significantly higher rate of malignant tumors than patients with other mutations. The evaluation of this potential genotype-phenotype correlation in the extended number of patients in this series revealed not longer statistical significance, but patients with truncating mutations of exons 2, 9, and 10 still tended to have a higher rate of malignant PETs and a higher rate of multiple PETs than patients with other mutations. This was especially noted in gastrinomas, since 7 of 8 gastrinomas of patients with truncating mutations of exons 2, 9, and 10 were malignant, whereas all 3 gastrinomas of patients with other mutations were benign with yet no recurrence. In addition, most other groups who revealed no evidence for a genotype-phenotype correlation in MEN1 did not focus on the individual tumor types as we did. They only compared specific clinical phenotypes regarding tumor presentation in different organs (eg, pancreas and parathyroid glands).
This is a very interesting question because the Ki67-proliferation marker is used in different tumor types as a marker of aggressive growth. But I think our strategy is going in a different way. By removing all nonfunctioning tumors >1 cm in size, we want to prevent malignancy. Because at this time there is no marker for benign and malignant behavior, we think that all tumors have a malignant potential. In addition, it is technically demanding to detect small duodenal gastrinoma endoscopically or to take a EUS-guided biopsy from a small pancreatic PET.
Dr. Akerström: I want to thank you for a very elegant and important presentation. This is a rare disease and that explains why the number of patients is limited, but the conclusions of your presentation are important. You advocate that pancreatic surgery in MEN1 is done mainly with the attempt of malignancy prevention, and you advocate early surgery, which is likely to be crucial for these patients.
It is important to remember that gastrinoma and the Zollinger-Ellison syndrome are a late feature of the MEN1 syndrome and, when present, 30% to 50% of patients already have metastases. Gastrinomas in MEN1 almost always occur in the duodenum, which can be completely filled with minute tumors or microadenomas. Perhaps you cannot cure this part of the disease unless you do pancreaticoduodenectomy. In our experience, however, concomitant nonfunctioning tumors are common and may be multiple as well; and in addition to local excision of gastrinomas, we have often been forced to perform distal 80% pancreatic resection to remove them. Since most of the gastrinomas in MEN1 appear to have a fairly good prognosis, the nonfunctioning tumors may grow larger and perhaps be worse for the patient.
I would like to invite you to discuss what would you do if you had a patient with 1 or 2 minute gastrinomas in the duodenum identified by duodenotomy, if the patients at the same time had 2 or 3 up to 2 cm large distal tumors. What would your choice be? Local removal of the gastrinomas together with 80% distal pancreatic resection or pancreaticoduodenectomy? Which would be the important tumors to take away? Some people advocate that it is possible to treat the Zollinger-Ellison syndrome efficiently by omeprazole and to aim surgery to remove especially the larger, perhaps more threatening pancreatic tumors.
Dr. Fendrich: Thank you, Dr Akerström, for your very realistic example of a typical situation. If there are duodenal gastrinomas and some large nonfunctioning distal tumors, we would excise the duodenal gastrinomas after duodenotomy and perform a distal pancreatic resection to the level of the portal vein with enucleation of any tumors in the pancreatic head, and dissect the peripancreatic lymph nodes. As previously mentioned, after regionalizing the source of gastrin secretion to the pancreatic head by SASI, and in the absence of PETs in the pancreatic corpus and tail, we would recommend a PPPD with lymphadenectomy.
Footnotes
Reprints: Detlef K. Bartsch, MD, Department of Surgery, Philipps University Marburg, Baldingerstraße, D-35043 Marburg, Germany. E-mail: bartsch@mailer.uni-marburg.de.
REFERENCES
- 1.Chandrasekharappa SC, Guru SC, Manickamp P, et al. Positional cloning of the gene for multiple endocrine neoplasia type 1 (MEN1). Science. 1997;276:404–407. [DOI] [PubMed] [Google Scholar]
- 2.Gibril F, Schumann M, Pace A, et al. Multiple endocrine neoplasia type 1 and Zollinger-Ellison syndrome: a prospective study of 107 cases and comparison with 1009 cases from the literature. Medicine. 2004;83:43–83. [DOI] [PubMed] [Google Scholar]
- 3.Langer P, Cupisti K, Bartsch DK, et al. Adrenal involvement in multiple endocrine neoplasia type 1. World J Surg. 2002;26:891–896. [DOI] [PubMed] [Google Scholar]
- 4.Wilkinson S, Teh BT, Davey KR, et al. Cause of death in multiple endocrine neoplasia type 1. Arch Surg. 1993;128:683–690. [DOI] [PubMed] [Google Scholar]
- 5.Doherty GM, Olson JA, Frisella MM, et al. Lethality of multiple endocrine neoplasia type I. World J Surg. 1998;22:581–587. [DOI] [PubMed] [Google Scholar]
- 6.Skogseid BS, Rastad J, Oberg K. Multiple endocrine neoplasia type 1: clinical features and screening. Endocrinol Metab Clin North Am. 1994;23:1–8. [PubMed] [Google Scholar]
- 7.Skogseid BS, Eriksson B, Lundqvist G, et al. Multiple endocrine neoplasia type 1: a 10-year prospective screening study in four kindreds. J Clin Endocrinol Metab. 1991;73:281–287. [DOI] [PubMed] [Google Scholar]
- 8.Akerstrom G, Hessman O, Skogseid B. Timing and extent of surgery in symptomatic and asymptomatic neuroendocrine tumors of the pancreas in MEN1. Langenbecks Arch Surg. 2002;386:558–569. [DOI] [PubMed] [Google Scholar]
- 9.Norton JA, Jensen RT. Resolved and unresolved controversies in the surgical management of patients with Zollinger-Ellison syndrome. Ann Surg. 2004;240:757–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Malagelada JR, Edis AJ, Adson MA, et al. Medical and surgical options in the management of patients with gastrinoma. Gastroenterology. 1983;84:1524–1532. [PubMed] [Google Scholar]
- 11.Mignon M, Cadiot G. Diagnostic and therapeutic criteria in patients with Zollinger-Ellison syndrome and multiple endocrine neoplasia type 1. J Intern Med. 1998;243:489–494. [DOI] [PubMed] [Google Scholar]
- 12.MacFarlane MP, Fraker DL, Alexander HR, et al. Prospective study of surgical resection of duodenal and pancreatic gastrinomas in multiple endocrine neoplasia type 1. Surgery. 1995;118:973–979. [DOI] [PubMed] [Google Scholar]
- 13.Norton JA, Wells SA Jr. The surgical management of patients with multiple endocrine neoplasia type 1. J Clin Endocrinol Metab. 1997;82:359–361. [DOI] [PubMed] [Google Scholar]
- 14.Bartsch DK, Langer P, Wild A, et al. Pancreaticoduodenal endocrine tumors in multiple endocrine neoplasia type 1: surgery or surveillance? Surgery. 2000;128:958–966. [DOI] [PubMed] [Google Scholar]
- 15.Lowney JK, Frisella MM, Lairmore TC, et al. Pancreatic islet cell tumor metastasis in multiple endocrine neoplasia type 1: correlation with primary tumor size. Surgery. 1999;125:1043–1049. [DOI] [PubMed] [Google Scholar]
- 16.Gauger PG, Thompson NW. Early surgical intervention and strategy in patients with multiple endocrine neoplasia type 1. Best Pract Res Clin Endocrinol Metab. 2001;15:213–223. [DOI] [PubMed] [Google Scholar]
- 17.Thompson NW. Management of pancreatic endocrine tumors in patients with multiple endocrine neoplasia type 1. Surg Clin North Am. 1998;7:881–891. [PubMed] [Google Scholar]
- 18.Imamura M, Takahashi K, Adachi H, et al. Usefulness of selective arterial secretin injection test for localization of gastrinoma in the Zollinger-Ellison syndrome. Ann Surg. 1976;205–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thompson NW, Lloyd RV, Nishiyama RH, et al. MEN I pancreas: a histological and immunohistochemical study. World J Surg. 1984;8:561–574. [DOI] [PubMed] [Google Scholar]
- 20.Majewski JT, Wilson SD. The MEA-I syndrome: an all or none phenomenon? Surgery. 1979;86:475–484. [PubMed] [Google Scholar]
- 21.Bartsch D, Kopp I, Bergenfelz A, et al. MEN1 gene mutations in 12 MEN1 families and their associated tumors. Eur J Endocrinol. 1998;139:416–420. [DOI] [PubMed] [Google Scholar]
- 22.Langer P, Kann PH, Fendrich V, et al. Prospective evaluation of imaging procedures for the detection of pancreaticoduodenal endocrine tumors in patients with multiple endocrine neoplasia type 1. World J Surg. 2004;28:1317–1322. [DOI] [PubMed] [Google Scholar]
- 23.Gauger PG, Scheiman JM, Wamsteker EJ, et al. Role of endoscopic ultrasonography in screening and treatment of pancreatic endocrine tumours in asymptomatic patients with multiple endocrine neoplasia type 1. Br J Surg. 2003;90:748–754. [DOI] [PubMed] [Google Scholar]
- 24.Norton JA, Fraker DL, Alexander HR, et al. Surgery to cure the Zollinger-Ellison syndrome. N Engl J Med. 1999;341:635–644. [DOI] [PubMed] [Google Scholar]
- 25.Cadiot G, Vuagnat A, Doukhan I, et al. Prognostic factors in patients with Zollinger-Ellison syndrome and multiple endocrine neoplasia type 1: Groupe d'Etude des Neoplasies Endocriniennes Multiples (GENEM and groupe de Recherche et d'Etude du Syndrome de Zollinger-Ellison (GRESZE). Gastroenterology. 1999;116:286–293. [DOI] [PubMed] [Google Scholar]
- 26.Weber HC, Venzon DJ, Lin JT, et al. Determinants of metastatic rate and survival in patients with Zollinger-Ellison syndrome: a prospective long-term study. Gastroenterology. 1995;108:1637–1649. [DOI] [PubMed] [Google Scholar]
- 27.Fraker DL, Norton JA, Alexander R, et al. Surgery for Zollinger-Ellison syndrome alters the natural history of gastrinoma. Ann Surg. 1994;220:320–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hausman MS Jr, Thompson NW, Gauger PG, et al. The surgical management of MEN-1 pancreatoduodenal neuroendocrine disease. Surgery. 2004;136:1205–1211. [DOI] [PubMed] [Google Scholar]
- 29.Pipeleers-Marichal M, Somers G, Willems G, et al. Gastrinomas in the duodenums of patients with multiple endocrine neoplasia type 1 and the Zollinger-Ellison syndrome. N Engl J Med. 1990;322:723. [DOI] [PubMed] [Google Scholar]
- 30.Waddell WR, Coppinger WR, Loughry RW. Pancreaticoduodenectomy for Zollinger-Ellison syndrome. Ann Surg. 1968;168:641–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lind T, Olbe L. Long-term follow up of patients with Zollinger-Ellison syndrome (ZES). Acta Chir Scand. 1989;155:383–388. [PubMed] [Google Scholar]
- 32.Delcore R, Friesen SR. Role of pancreatoduodenectomy in the management of primary duodenal wall gastrinomas in patients with Zollinger-Ellison syndrome. Surgery. 1992;112:1016–1022. [PubMed] [Google Scholar]
- 33.Stadil F. Treatment of gastrinomas with pancreatoduodenectomy. In: Mignon M, Jensen RT, eds. Endocrine Tumors of the Pancreas: Recent Advances in Research and Management, vol. 23. Frontiers of Gastrointestinal Research. Basel, Switzerland: Karger, 1995:333. [Google Scholar]
- 34.Schroder W, Holscher AH, Beckurts T, et al. Duodenal microgastrinomas associated with Zollinger-Ellison syndrome. Hepatogastroenterology. 1996;43:1465–1469. [PubMed] [Google Scholar]
- 35.Jordan PH Jr. A personal experience with pancreatic and duodenal neuroendocrine tumors. J Am Coll Surg. 1999;189:470–482. [DOI] [PubMed] [Google Scholar]
- 36.Kato M, Imamura M, Hosotani R, et al. Curative resection of microgastrinomas based on the intraoperative secretin test. World J Surg. 2000;24:1425–1430. [DOI] [PubMed] [Google Scholar]
- 37.Lairmore TC, Chen VY, DeBenedetti MK, et al. Duodenopancreatic resections in patients with multiple endocrine neoplasia type 1. Ann Surg. 2000;231:909–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Norton JA, Alexander HR, Fraker DL, et al. Comparison of surgical results in patients with advanced and limited disease with multiple endocrine neoplasia type 1 and Zollinger-Ellison syndrome. Ann Surg. 2001;234:495–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sarmiento JM, Farnell MB, Que FG, et al. Pancreaticoduodenectomy for islet cell tumors of the head of the pancreas: long-term survival analysis. World J Surg. 2002;26:1267–1271. [DOI] [PubMed] [Google Scholar]
- 40.Demeure MJ, Klonoff DC, Karam JH, et al. Insulinomas associated with multiple endocrine neoplasia type I: the need for a different surgical approach. Surgery. 1991;110:998–1004. [PubMed] [Google Scholar]
- 41.O'Riordian DS, O'Brian T, van Heerden JA, et al. Surgical management of insulinoma associated with multiple endocrine neoplasia type I. World J Surg. 1994;18:488–494. [DOI] [PubMed] [Google Scholar]
- 42.Skogseid B, Öberg K, Eriksson B, et al. Surgery for asymptomatic pancreatic lesions in multiple endocrine neoplasia type 1. World J Surg. 1996;20:872–877. [DOI] [PubMed] [Google Scholar]
- 43.Phan GQ, Yeo CJ, Cameron JL, et al. Pancreaticoduodenectomy for selected periampullary neuroendocrine tumors: fifty patients. Surgery. 1997;122:989–996. [DOI] [PubMed] [Google Scholar]
- 44.Park BJ, Alexander HR, Libutti SK, et al. Operative management of islet-cell tumors arising in the head of the pancreas. Surgery. 1998;124:1056–1061. [DOI] [PubMed] [Google Scholar]
- 45.Cullen JJ, Sarr MG, Ilstrup DM. Pancreatic anastomotic leak after pancreaticoduodenectomy: incidence, significance, and management. Am J Surg. 1994;168:295–298. [DOI] [PubMed] [Google Scholar]
- 46.Giraud S, Zhang CX, Serova-Sinilnikova O, et al. Germ-line mutation analysis in patients with multiple endocrine neoplasia type 1 and related disorders. Am J Hum Genet. 1998;63:455–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kouvaraki MA, Lee JE, Shapiro SE, et al. Genotype-phenotype analysis in multiple endocrine neoplasia type 1. Arch Surg. 2002;137:641–647. [DOI] [PubMed] [Google Scholar]
- 48.Gobl AE, Berg M, Lopez-Egido JR, et al. Menin represses JunD-activated transcription by a histone deacetylase-dependent mechanism. Biochim Biophys Acta. 1999;1447:51–56. [DOI] [PubMed] [Google Scholar]