Abstract
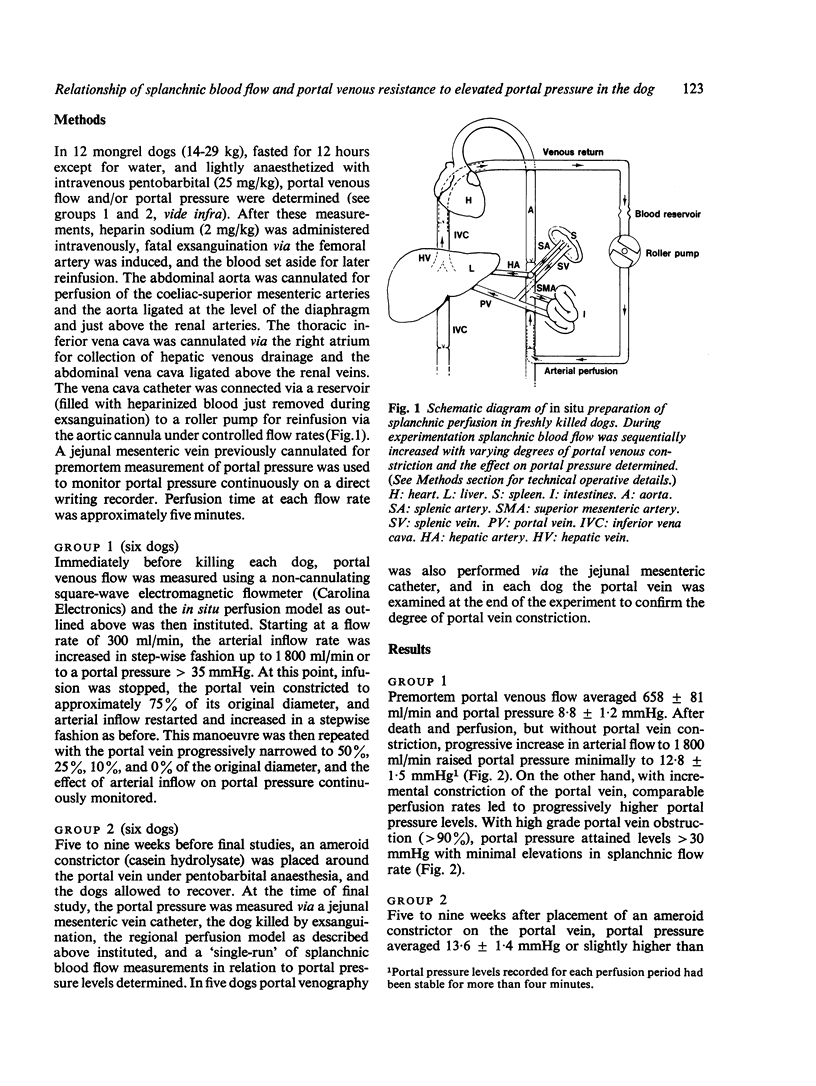
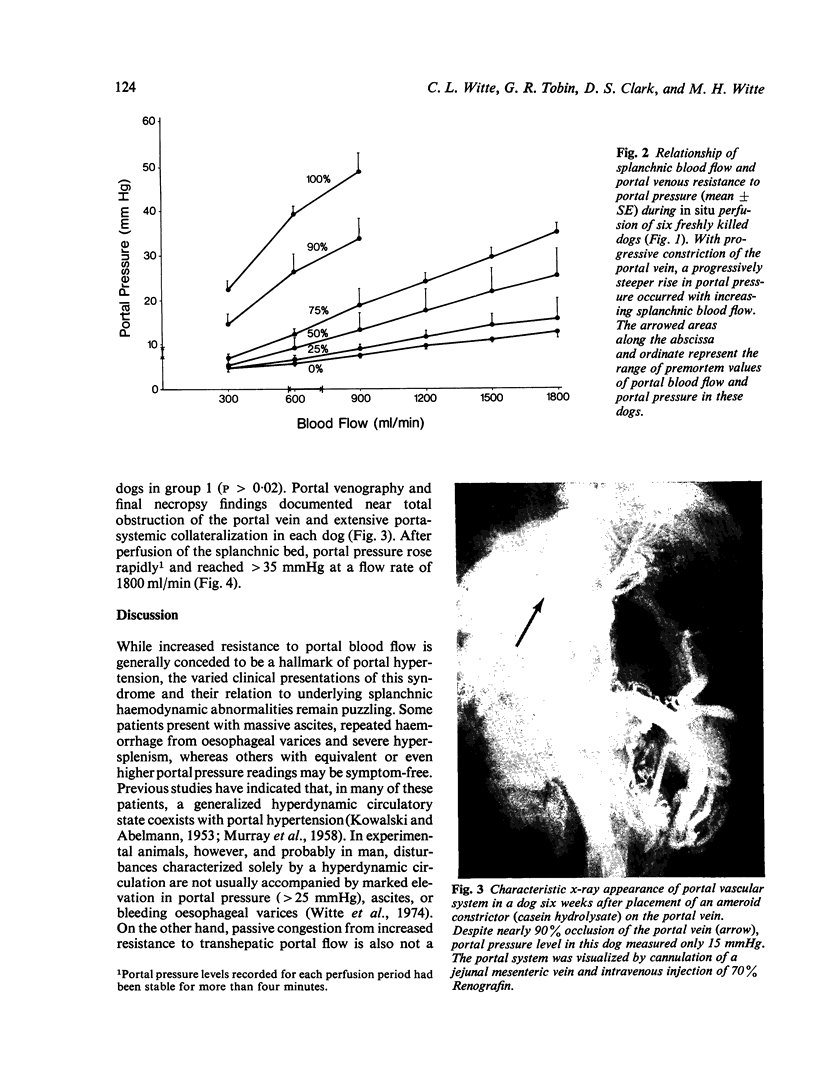
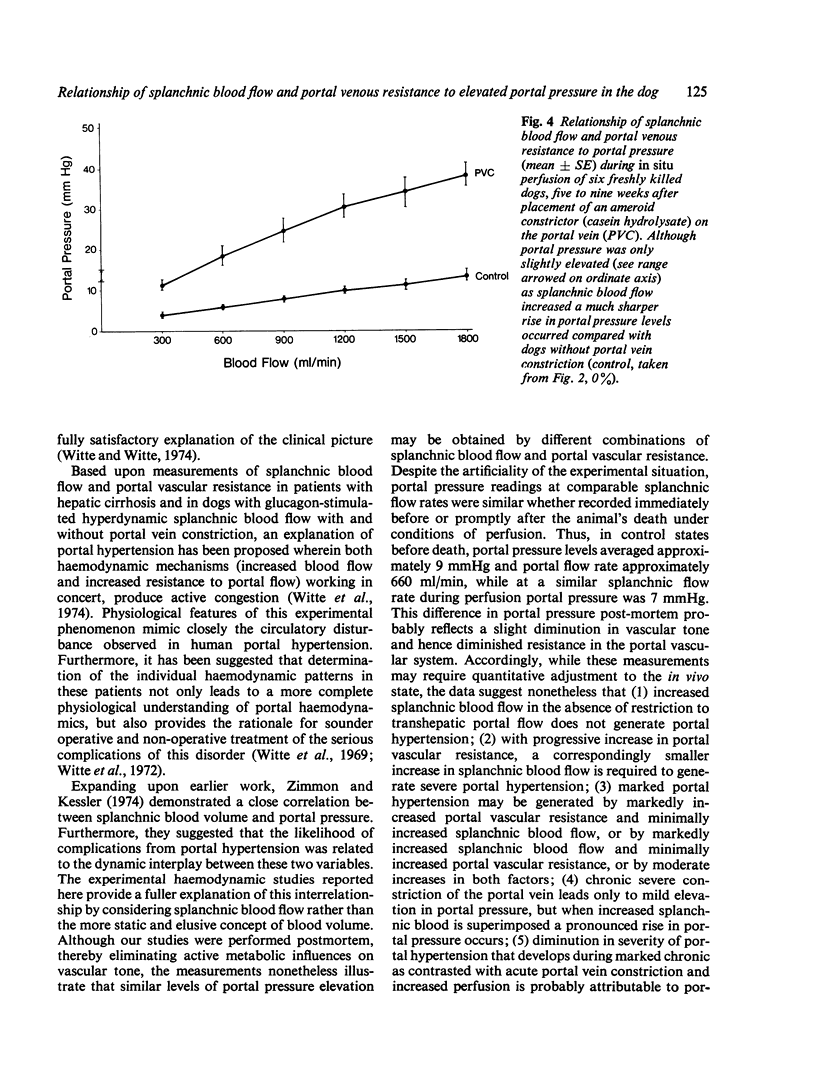
To determine the relationship of splanchnic blood flow and portal venous resistance to elevated portal pressure, in situ perfusion of the splanchnic circuit was carried out in 12 freshly killed dogs at varying perfusion rates and degrees of acute and chronic portal vein constriction. In six normal dogs before being killed, portal pressure averaged 8-8 +/- 1-2 mmHg and portal flow 658 +/- 81 ml/min. In the absence of portal vein constriction, increasing splanchnic perfusion to 1800 ml/min, minimally raised portal pressure (12-8 +/- 1-5 mmHg). With progressive acute constriction of the portal vein, however, comparable perfusion rates lead to progressively higher portal pressure levels and with greater than 90% constriction, portal pressure was greater than 30 mmHg with minimal elevation in splanchnic flow rate. In six other dogs before being killed but live to nine weeks after placement of an ameroid constrictor on the portal vein, portal pressure averaged 13-6 +/- 1-4 mmHg or slightly higher than in normal dogs (P greater than 0-02). Mesenteric venography and necropsy findings uniformly demonstrated 90% occlusion of the portal vein with extensive portasystemic collateralization. With increased perfusion of the splanchnic bed, portal pressure rose rapidly to approximately 35 mmHg with a flow rate of 1 800 ml/min.. These data suggest that, in disorders where resistance to transhepatic portal flow is marked, a small increment in splanchnic blood flow, which normally exerts little or no influence on portal pressure, promotes profound portal hypertension and may account for spontaneous 'rupture' of oesophageal varices. On the other hand, where resistance to transhepatic portal flow is mild but splanchnic blood flow is markedly hyperdynamic, reducing inflow may be sufficient to ameliorate extreme portal hypertension and its sequelae.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- KOWALSKI H. J., ABELMANN W. H. The cardiac output at rest in Laennec's cirrhosis. J Clin Invest. 1953 Oct;32(10):1025–1033. doi: 10.1172/JCI102813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MURRAY J. F., DAWSON A. M., SHERLOCK S. Circulatory changes in chronic liver disease. Am J Med. 1958 Mar;24(3):358–367. doi: 10.1016/0002-9343(58)90322-x. [DOI] [PubMed] [Google Scholar]
- WOMACK N. A., PETERS R. M. The significance of splenomegaly in cirrhosis of the liver. Ann Surg. 1961 Jun;153:1006–1019. doi: 10.1097/00000658-196106000-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witte C. L., Witte M. H., Bair G., Mobley W. P., Morton D. Experimental study of hyperdynamic vs. stagnant mesenteric blood flow in portal hypertension. Ann Surg. 1974 Mar;179(3):304–310. doi: 10.1097/00000658-197403000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witte C. L., Witte M. H., Krone C. L. Contrasting hemodynamic patterns of portal hypertension. Ann Surg. 1972 Jul;176(1):68–79. doi: 10.1097/00000658-197207000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witte C. L., Witte M. H., Renert W., Corrigan J. J., Jr Splenic circulatory dynamics in congestive splenomegaly. Gastroenterology. 1974 Sep;67(3):498–505. [PubMed] [Google Scholar]
- Witte C. L., Witte M. H. The circulation in portal hypertension. Yale J Biol Med. 1975 May;48(2):141–155. [PMC free article] [PubMed] [Google Scholar]
- Witte M. H., Witte C. L., Cole W. R., Koehler P. R. Contrasting patterns of ascites formation in hepatic cirrhosis. JAMA. 1969 Jun 2;208(9):1661–1666. [PubMed] [Google Scholar]
- Zimmon D. S., Kessler R. E. The portal pressure-blood volume relationship in cirrhosis. Gut. 1974 Feb;15(2):99–101. doi: 10.1136/gut.15.2.99. [DOI] [PMC free article] [PubMed] [Google Scholar]