Abstract
The endocannabinoid N-arachidonoyl ethanolamine (anandamide), found both in the CNS and in the periphery, plays a role in numerous physiological systems. One might expect that the chemically related N-arachidonoyl-l-serine (ARA-S) could also be formed alongside anandamide. We have now isolated ARA-S from bovine brain and elucidated its structure by comparison with synthetic ARA-S. Contrary to anandamide, ARA-S binds very weakly to cannabinoid CB1 and CB2 or vanilloid TRPV1 (transient receptor potential vanilloid 1) receptors. However, it produces endothelium-dependent vasodilation of rat isolated mesenteric arteries and abdominal aorta and stimulates phosphorylation of p44/42 mitogen-activated protein (MAP) kinase and protein kinase B/Akt in cultured endothelial cells. ARA-S also suppresses LPS-induced formation of TNF-α in a murine macrophage cell line and in wild-type mice, as well as in mice deficient in CB1 or CB2 receptors. Many of these effects parallel those reported for abnormal cannabidiol (Abn-CBD), a synthetic agonist of a putative novel cannabinoid-type receptor. Hence, ARA-S may represent an endogenous agonist for this receptor.
Keywords: abnormal cannabidiol, anandamide, cannabinoids, endothelium, reactive oxygen intermediates
The identification, structural elucidation, and syntheses of the plant cannabinoids in the early 1960s led to thorough investigations of the chemistry, metabolism, and pharmacology of these compounds, in particular of the psychoactive constituent Δ9-tetrahydrocannabinol (1, 2). However, until the late 1980s and early 1990s, when specific receptors were identified and shortly thereafter cloned, the mechanism of the numerous cannabinoid actions remained an enigma (3–5). Two main receptors are now known: the CB1 receptor, found in the CNS, as well as in some peripheral tissues, and the CB2 receptor, found predominantly in the immune system (6–8). Additional, not yet fully identified receptors are present both in the CNS and in the periphery (6, 9, 10).
Because receptors in mammals are not formed to encounter a plant constituent, research was initiated to discover endogenous ligands. In the 1990s two endogenous cannabinoids (endocannabinoids) were identified, N-arachidonoyl ethanolamine (anandamide) (11) and 2-arachidonoyl-glycerol (12, 13). Additional endocannabinoids have been reported, but their biological roles are yet obscure (6, 14). Anandamide and 2-arachidonoyl-glycerol have large spectrum of physiological actions, most of which are associated with the neural and immune systems. However, cardiovascular effects, which are in part CB1-mediated (15), are also well established (9, 14, 16).
Anandamide is a product of phosphatidylethanolamine (17). Because phosphatidylserine is found alongside phosphatidylethanolamine in body tissues, one might expect that arachidonoyl-l-serine (ARA-S) is also an endogenous constituent (see Fig. 1A for the structures of anandamide and ARA-S). We report that we have isolated ARA-S from bovine brain and have evaluated some of its biological properties.
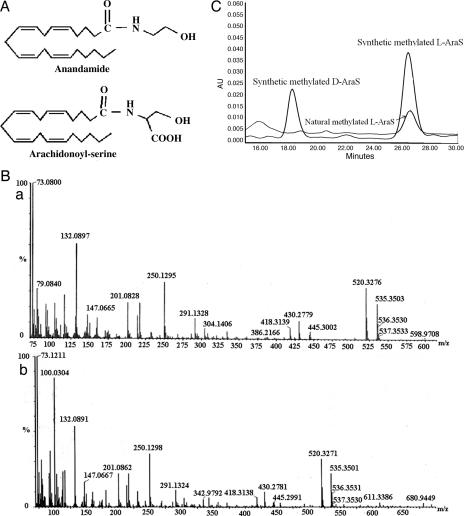
Fig. 1.
Identification of ARA-S in bovine brain. (A) Structures of anandamide and ARA-S. (B) Electron impact high-resolution mass spectra of synthetic ARA-S (a) and endogenous ARA-S (b) from bovine brain. Both spectra are after derivatization with N,O-bis(trimethyl-silyl)trifluoroacetamide. (C) Overlay chromatogram of natural and synthetic d- (≈18 min), l- (≈26 min) ARA-S methyl esters obtained with HPLC chiral chromatography.
Results
ARA-S was extracted from bovine brains by the procedure described below to yield extract A. Two routes were followed to identify ARA-S. In the first, extract A was silylated with N,O-bis(trimethyl-silyl)trifluoroacetamide and analyzed by GC-MS. The peak of synthetic di-trimethyl-silyl (di-TMS)-ARA-S appears at 17.32 min. The mass spectra of the peak from silylated synthetic material and of extract A, eluting at a comparable time period, were identical.
The high-resolution mass spectra of endogenous and synthetic ARA-S (as their di-TMS derivatives) were also identical (Fig. 1B). Both natural di-TMS-ARA-S and synthetic di-TMS-ARA-S eluted after ≈18 min. Natural di-TMS-ARA-S was found to have a molecular weight ion at 535.3501 m/z, which is within 2.3 ppm of the calculated mass (535.3513 m/z) and indicates an elemental composition of C29H53NO4Si2, which is consistent with the di-TMS derivative of the proposed structure (Fig. 1A). ARA-S is therefore a C23H37NO4 compound, with a molecular weight of 391.5.
ARA-S is not stable at room temperature or at −20°C (without a solvent). However, kept at −20°C in ethanol it was stable for at least up to 2 months.
The second route involved methylation of extract A, followed by silylation. We compared the mass spectrum of the TMS derivative of the compound peak, eluting at 15.87 min, with that of the of synthetic TMS-ARA-S methyl ester, which elutes at the same time. The mass spectra were identical, with molecular ion [M]+ 477 m/z. The NMR spectral data of synthetic ARA-S methyl ester are presented in Supporting Text, which is published as supporting information on the PNAS web site.
The stereochemistry of ARA-S was established by comparison of the elution time of natural ARA-S methyl ester with the synthetic l and d methyl esters of ARA-S on a HPLC chiral column. Overlaid chromatograms of synthetic arachidonoyl-d-serine or ARA-S methyl esters with methylated ARA-S from brain-derived material showed optical identity of the methyl ester of the natural material with the synthetic l-enantiomer (elution time 26.7 min) and nonidentity with the synthetic d-enantiomer (elution time 18.3 min) (Fig. 1C).
Contrary to anandamide, ARA-S binds very weakly to CB1 receptors in mouse cerebellar membranes (Ki > 10,000 nM). Furthermore, at concentrations up to and including 30 μM, ARA-S failed to displace radioligand binding to rat CB2 receptors or rat TRPV1 (transient receptor potential vanilloid 1) receptors.
ARA-S relaxes rat isolated mesenteric arteries (EC50, 550 nM) and abdominal aorta (EC50, ≈1,200 nM). These effects resemble those of abnormal cannabidiol (Abn-CBD), a synthetic agonist of a novel cannabinoid-type receptor (18). In rat aorta, 1 μM SR-141716A or SR-144528 did not antagonize ARA-S-induced vasorelaxation (data not shown), indicating the lack of involvement of CB1 or CB2 receptors. In the presence of indomethacin (10 μM) the ARA-S effects were unchanged. The cannabidiol (CBD) analog O-1918 is an inhibitor of the mesenteric vasorelaxant effects of Abn-CBD (18, 19) and anandamide (20). O-1918 at 10 μM did not antagonize ARA-S-induced relaxation of aortic rings (Fig. 2A), which was endothelium-dependent: maximum relaxation was 60 ± 4% in intact preparations vs. 29 ± 1% in denuded preparations (Fig. 2A). The aortic relaxant effect of ARA-S was blocked by pertussis toxin (PTX; 0.5 μg/ml, Fig. 2B), which similarly inhibited aortic relaxation by Abn-CBD (data not shown).
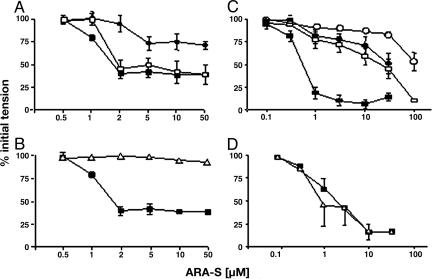
Fig. 2.
ARA-S-induced vasorelaxation in rat aortic rings (A and B) and mesenteric artery segments (C and D). (A) The aortic relaxant effect of ARA-S (filled squares) is not antagonized by 10 μM O-1918 (open squares) and is nearly eliminated by endothelial denudation (filled circles). (B) Relaxation of aortic rings by ARA-S (filled squares) is blocked by PTX (open triangles). (C) Mesenteric vasorelaxation by ARA-S is inhibited by 10 μM O-1918 (open symbols) in endothelium-intact (squares) and endothelium-denuded (circles) preparations. (D) Mesenteric vasorelaxation by ARA-S (filled squares) is unaffected by PTX (open triangles). Points and vertical bars are means ± SE from four to six experiments.
The relaxant effect of ARA-S was less endothelium-dependent in mesenteric artery segments than in aorta: denudation right-shifted the ARA-S concentration–response curve without reducing the maximal response (Fig. 2C). Unlike in aorta, PTX did not influence the ARA-S response (Fig. 2D). Also, 10 μM O-1918 significantly inhibited mesenteric relaxation by ARA-S, and the inhibition remained significant in endothelium-denuded preparations (Fig. 2C). Thus, the different behavior of the two preparations may be related to the presence of an endothelium-independent component in the effect of ARA-S in mesenteric arteries. In these preparations, Abn-CBD also elicited full vasorelaxation (EC50, 2 μM), sensitive to inhibition by O-1918 but not by PTX (data not shown).
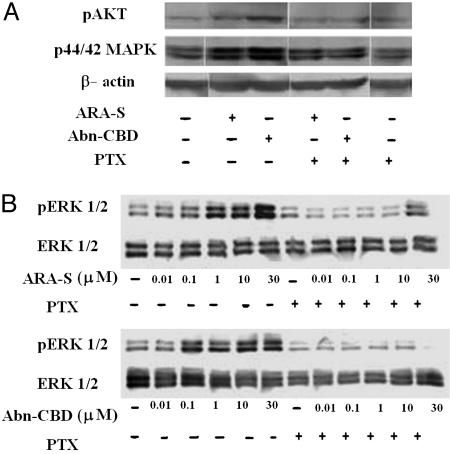
Exposure of cultured human umbilical vein endothelial cells (HUVEC) to 1 μM ARA-S or 30 μM Abn-CBD for 30 min significantly increased the phosphorylation of Akt and p44/42 mitogen-activated protein (MAP) kinase, which was attenuated by preincubation with 400 ng/ml PTX (Fig. 3A). The concentration dependence of these effects is illustrated in Fig. 3B. These findings suggest that a receptor similar to that in rat aorta is present in HUVEC and is involved in mediating the effect of ARA-S on MAP kinase and Akt. The PTX sensitivity of the response suggests the involvement of Gi/Go.
Fig. 3.
Activation of MAP kinase and protein kinase B/Akt. (A) ARA-S (1 μM) and Abn-CBD (30 μM) increase the phosphorylation of protein kinase B/Akt (Top) and p44/42 MAP kinase (Middle), effects inhibited by PTX (400 ng/ml). Western blotting is described in Materials and Methods. β-Actin (Bottom) was used as loading control. This experiment was replicated two more times with similar results. (B) Concentration-dependent phosphorylation of p44/42 MAP kinase by ARA-S and Abn-CBD.
Treatment of murine RAW264.7 macrophages with ARA-S suppressed the production of zymosan-induced reactive oxygen intermediates (ROI). The inhibitory effect was concentration-dependent and reached 45% at 76.6 μM ARA-S. ARA-S also inhibited the LPS-induced increase of NO production by primary murine macrophages, which reached 50% at the highest concentration tested. In the same cells, 24-h incubation with ARA-S inhibited TNF-α production, reaching 78% inhibition at the highest concentration of ARA-S used (see Fig. 5, which is published as supporting information on the PNAS web site). Contrary to ARA-S, its synthetic d-enantiomer failed to elicit any of these effects (data not shown).
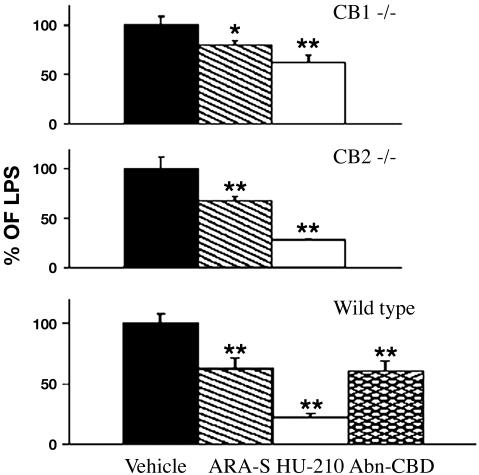
Treatment of wild-type mice with 10 mg/kg ARA-S or 20 mg/kg Abn-CBD i.p. reduced LPS-induced TNF-α production by ≈40%, whereas the potent CB1/CB2 agonist HU-210 (50 μg/kg) reduced plasma TNF-α levels by ≈80%. These effects remained significant in both CB1−/− and CB2−/− mice, although the size of the reduction was lower in CB1−/− mice than in control mice (Fig. 4).
Fig. 4.
The effect of ARA-S (10 mg/kg), Abn-CBD (20 mg/kg), and HU-210 (50 μg/kg) on LPS-induced plasma TNF-α levels in wild-type (n = 32), CB1−/− (n = 5), and CB2−/− (n = 4) mice. Basal levels of TNF-α were 30 ± 10, 39 ± 15, and 35 ± 13 pg/ml, and LPS-stimulated levels were 3,407 ± 197, 3,642 ± 326, and 6,877 ± 857 pg/ml in the three groups, respectively. Significant difference from vehicle-treated values is indicated by ∗ (P < 0.05) and ∗∗ (P < 0.001).
Discussion
We describe the isolation and structural elucidation of a novel endocannabinoid-like component, ARA-S, from bovine brain. For comparison, this compound was synthesized following a known two-step procedure (21). The chromatographic behavior (elution time on GC-MS) and mass spectra (Fig. 1B) of the natural and synthetic materials (after TMS silylation on both the hydroxyl and carboxyl groups) were identical. The methyl ester of synthetic and endogenous ARA-S (both in their mono-TMS forms) also have identical retention time and mass spectra.
A high-resolution MS measurement of endogenous ARA-S (as the di-TMS derivative, Fig. 1B) indicated the elemental composition C23H37NO4 for ARA-S and molecular weight 391.5 (Fig. 1A).
On a HPLC chiral column the elution time of ARA-S methyl ester was identical to that of synthetic l-enantiomer and different from that of synthetic d-enantiomer of methylated ARA-S (Fig. 1C). Thus, the endogenous lipid isolated from brain is ARA-S.
ARA-S binds very weakly to the CB1 receptor with a potency of <1% of that of anandamide and does not bind to either the CB2 or the TRPV1 receptor. Because anandamide can elicit vasodilation by a mechanism that does not involve CB1, CB2, or TRPV1 receptors (9, 22, 23), we tested ARA-S for possible vasodilatory activity. ARA-S is indeed vasorelaxant in an endothelium-dependent manner in both rat abdominal aorta and mesenteric artery segments. The effect is independent of CB1 and CB2 receptors, as indicated by its resistance to blockade by CB1 or CB2 antagonists. However, there are also differences between the effect of ARA-S in aorta and mesenteric arteries, as discussed below.
In intact animals, anandamide elicits hypotension mediated exclusively by CB1 receptors (9, 24). This effect is due primarily to decreased cardiac contractility and output, with little change in vascular resistance (25). Although CB1 receptor activation may lead to localized vasodilation in the coronary (26) or cerebral (27) vasculatures, additional receptors distinct from CB1, CB2, or TRPV1 have been implicated in anandamide-induced vasodilation (9, 20, 23). In the rat mesenteric vascular bed, anandamide causes endothelium-dependent vasodilation inhibited by micromolar concentrations of the CB1 antagonist SR141716A and by PTX (9, 28, 29). However, the effect is not inhibited by another CB1 antagonist, AM251 (20, 29, 30), and potent synthetic CB1/CB2 agonists do not elicit mesenteric vasodilation (31). Furthermore, mesenteric vasodilation by anandamide remains unchanged in CB1 knockout or CB1/CB2 double knockout mice (9), which rules out the involvement of these receptors. Capsazepine fails to antagonize the endothelium-dependent vasodilator effect of anandamide (9, 32), arguing against TRPV1 receptor involvement.
Abn-CBD, a synthetic isomer of the behaviorally inactive phytocannabinoid CBD, elicits endothelium-dependent, capsazepine-insensitive mesenteric vasodilation (9, 18), unaffected by CB1 or CB2 antagonists but inhibited by CBD (9) or O-1918 (18), and is moderately sensitive to resiniferotoxin (≈2-fold increase in EC50; see ref. 18). This finding suggests that Abn-CBD is a selective agonist and CBD and O-1918 are selective antagonists of an atypical endothelial receptor coupled to Gi/Go. Ho and Hiley (19) confirmed the ability of O-1918 to inhibit the mesenteric vasorelaxant effect of Abn-CBD but found it to be PTX-resistant, similar to the present findings with both ARA-S and Abn-CBD in mesenteric artery segments. In these preparations, endothelial denudation caused only a parallel shift of the ARA-S dose–response curve (Fig. 2C), whereas in aorta it nearly abolished it (Fig. 2B). Furthermore, in mesenteric arteries O-1918 inhibited the effect of ARA-S even after removal of the endothelium (Fig. 2C). Therefore, both the inhibition by O-1918 and the resistance to PTX may be properties of the endothelium-independent component of the effect of ARA-S and Abn-CBD, which is present in mesenteric arteries but not in aorta. Qualitative differences in receptor expression are known to exist between large and small vessels even in the same vascular bed (33). The PTX sensitivity of ARA-S responses in HUVEC is compatible with such a scheme, which suggests that there may be more than one vascular receptor for these novel ligands.
The present findings reveal the similar profile of actions of ARA-S and Abn-CBD, implicating parallel mechanisms of action. Other endocannabinoids, including N-arachidonoyl dopamine (34) and virodhamine (35), also interact with the Abn-CBD-sensitive endothelial receptor (30, 36), in addition to their actions at CB1 and TRPV1 receptors. In contrast, ARA-S does not bind to CB1, CB2, or TRPV1 receptors, so it is the first selective endogenous ligand of this putative endothelial receptor. In HUVEC, activation of this receptor by both ARA-S and Abn-CBD results in phosphorylation of p44/42 MAP kinase and protein kinase B/Akt (Fig. 3), pathways involved in endothelial cell migration (37). This finding suggests that ARA-S may be involved in the regulation of angiogenesis. In microglia, Abn-CBD triggers endothelial cell migration, an important component of neuroinflammation (38).
Relaxation of isolated arteries by anandamide is partly mediated by TRPV1 receptors (39–41). Anandamide binds to TRPV1 receptors with low affinity (8), resulting in the release of the vasodilator peptide CGRP (41). This mechanism may account for the endothelium-independent component of vasodilation by anandamide in some vascular beds, but not in others (9, 40). However, this effect of anandamide is not sensitive to TRPV1 receptor blockade (28), and neither is the effect of Abn-CBD (9, 18, 19). The effect of ARA-S is similarly independent of the TRPV1 receptor, because it does not bind to this receptor.
In summary, the brain produces a substance which, although chemically related to anandamide, binds very weakly to the known cannabinoid receptors and parallels the vasodilatory activity of synthetic Abn-CBD. Its activity is endothelium-dependent and PTX-sensitive in some models but not in others. These results reinforce the hypothesis that the effects of ARA-S may be in part mediated by a Gi/Go-coupled receptor distinct from CB1 and CB2 and similar to the Abn-CBD-sensitive receptor.
Anandamide and 2-arachidonoyl-glycerol have been reported to exert their vasodilatory effect by degradation to arachidonic acid (42, 43). Vasodilation by ARA-S is not elicited through a similar mechanism, because it is unaffected by indomethacin, a nonselective cyclooxygenase inhibitor.
ARA-S suppresses formation of reactive oxygen intermediates, NO, and TNF-α in a murine macrophage cell line, as well as TNF-α in vivo, indicating that it may also have antiinflammatory activity. Interestingly, anandamide and certain N-acyl-vanillamines have been reported to inhibit NF-κB activation through a cannabinoid and vanilloid receptor-independent pathway (44). Cannabinoid inhibition of TNF-α production in vivo also has features incompatible with the involvement of CB1 or CB2 receptors (45). ARA-S and Abn-CBD maintain their ability to inhibit TNF-α production in mice deficient in CB1 or CB2 receptors, providing strong evidence for an alternative mechanism. Whether the Abn-CBD-sensitive receptor is the same in macrophages and in vascular endothelium remains to be determined. The effects of ARA-S in cultured RAW264.7 macrophages require high concentrations of this lipid, and it has yet to be shown that such endogenous levels of ARA-S can be reached. Nevertheless, the inability of the d-enantiomer of ARA-S to mimic these effects suggests that they are initiated through a receptor-mediated mechanism.
The above actions of ARA-S suggest that it may be involved in the homeostasis of the vascular system in addition to acting as a vascular protective agent. Cannabinoids have long been known as antiinflammatory agents (45, 46), but some of them are psychotropic. ARA-S is devoid of psychotropic activity and may be involved in the pathology of inflammatory conditions including atherosclerosis, a state in which altered inflammation, cell migration, and altered vascular elasticity are present. Our results point toward the importance of ARA-S as a vascular protective agent.
Materials and Methods
Chemicals.
Abn-CBD [(−)-4-(3–3,4-trans-p-menthadien-[1,8]-yl)-olivetol] was synthesized as described (47). O-1918 was kindly provided by Raj Razdan (Organix, Inc., Woburn, MA) (18). SR-141716A (a CB1 receptor antagonist) and SR-144528 (a CB2 receptor antagonist) were from Triangle Research Laboratories. ARA-S and arachidonoyl-d-serine were synthesized as reported in ref. 21. N,O-bis(trimethyl-silyl)trifluoroacetamide, containing 1% trimethylchlorosilane, phenylephrine HCl, indomethacin, luminol, LPS (Escherichia coli 0127:B8), and zymosan were from Sigma. PTX was obtained from List Biological Laboratories (Campbell, CA) and from Sigma. Antibodies against the phosphorylated and unphosphorylated forms of p44/42 MAP kinase and Akt were from New England Biolabs. Low-protein medium was from Biological Industries (Beit Haemek, Israel), and Ficoll Hypaque–Histopaque (density 1.077) was from Sigma. Transwell trays of 5-μm pore were from Corning, ELISA reagents were purchased from BD Biosciences (San Diego), and RAW 264.7 cells were obtained from American Type Culture Collection. DMEM, FCS, and Hanks’ balanced salt solution (HBSS) were from Biological Industries (Beit Haemek, Israel), and EGM-2 Bullekit was from BioWhittaker. For the in vitro experiments, Abn-CBD, O-1918, and ARA-S were dissolved in ethanol.
Animals.
Heterozygote breeding pairs for mice with deleted cb1 or cb2 gene (CB1−/− and CB2−/− mice) and back-crossed to a C57BL6/J background were originally obtained from A. Zimmer (Bonn University, Bonn, Germany). Wild-type littermates were used as controls. The animal care and the protocols met the guidelines of the Institutional Animal Care and Use Committees.
Isolation of ARA-S.
Fresh bovine brains (≈1.5 kg) were homogenized in chloroform/methanol/water (1:1:0.5), followed by centrifugation for 20 min at 7,500 × g at 4°C. Nonmiscible residues were filtered, and the organic layer was separated from the water layer and evaporated to dryness. This dry organic extract was redissolved in methanol, filtered, and evaporated to dryness (extract A).
GC/MS Analysis.
One milligram of extract A was dissolved in 10 ml of chloroform. Ten microliters of this solution was blown down with nitrogen, and 10 μl of N,O-bis(trimethyl-silyl)trifluoroacetamide, a silylating agent, was added. After 60 min, 1 μl of the silylated mixture was injected into a TRACE GC/MS 2000 system with electron impact ionization detector. The column used was ZB-5 (5% phenyl/95% dimethylpolysiloxane, 30 × 0.25 mm, 0.25 μm). The experimental conditions were as follows: inlet, 250°C; detector, 280°C; splitless injection/purge time, 1 min; initial temperature, 70°C; initial time, 5 min; rate, 20°C/min; final temperature, 280°C.
High-Resolution MS Analysis.
High-resolution electron impact mass spectra were obtained with an AutoSpec Premier mass spectrometer (Waters Micromass). After silylation of synthetic ARA-S and extract A, as described above, 1 μl of the respective solution was injected into the HRGC-MS instrument under identical experimental conditions as described for the low-resolution GC/MS analysis (see above).
HPLC Analysis.
A computer-controlled Waters chromatograph with the following components was used: millennium software (version 3.20), 600E multisolvent delivery pump, 20-, 100-, and 200-μl loops, and a Photodiode Array (996 model) detector. All solvents used were HPLC-grade; acetonitrile, hexane, and ethanol were from J.T. Baker. Doubly distilled water was filtered on a 0.2-μm cellulose mixed ester membrane (Schleicher & Schuell). Before injection into the HPLC, the crude samples were filtered by loading concentrated portion extracts onto a 0.2-μm Gelman nylon syringe filter.
Isolation of ARA-S from extract A was performed on semipreparative Waters RP-Symmetry Prep C18 column (7-μm, 7.8 × 300 mm). A 200-μl aliquot of the crude material dissolved in methanol was injected into the column and analyzed by a reversed-phase HPLC. The mobile phase consisted of water (pH 2.6 by phosphoric acid) and acetonitrile. The gradient conditions were as follows: 75% acetonitrile for 15 min, followed by increasing acetonitrile to 100% acetonitrile within 2 min. After 13 min, the concentration of acetonitrile was returned to the starting conditions (75%) within 2 min. An additional 15 min were needed to reestablish the initial equilibrium state. Flow rate was 3 ml/min, and the monitoring wavelength was 205 nm. The ARA-S sharp peak eluted at almost 13 min. Approximately 25 successive semipreparative injections isolated ≈0.2 mg of ARA-S. Directly after the collection, the ARA-S compound was reinjected to an analytical column of Waters Symmetry C18 (5 μm, 4.6 × 250 mm). A 100-μl aliquot was injected and analyzed by isocratic reversed-phase mode at 30°C. The mobile phase was acetonitrile/water (pH 2.6 by H3PO4), 75:25 (vol/vol). The flow rate was 1 ml/min, and the monitoring wavelength was 205 nm. Synthetic ARA-S eluted at the same retention time (≈11 min) as the natural compound. The UV spectrum of the two compounds showed an excellent match. Waters pda software purity calculations confirmed that the ARA-S eluted peaks were homogeneous; i.e., no coelution was detected.
To determine the optical properties of the isolated natural ARA-S, the methyl esters of arachidonoyl-d-serine and ARA-S were prepared (see below) and resolved by chiral chromatography. A commercially available carbamated amylose ChiralPak-AD chiral stationary phase coated on silica support was used (Daicel Chemical Industries, Tokyo). Column dimensions were 10 μm, 250 × 4.6 mm i.d. The mobile phase was 10% ethanol and 90% hexane, the flow rate was 1 ml/min, and the monitoring wavelength for the compound was 205 nm. When a 20-μl mixture of the two pairs of d- and l-methylated ARA-S isomers was injected, good selectivity (selectivity factor, α > 1.5) and resolution were obtained (Fig. 1C).
Methylation of ARA-S.
Synthetic ARA-S (39.1 mg, 1 mmol) was dissolved in dimethylformamide (2 ml), and potassium carbonate (750 mg, 5.42 mmol) was added, some of which remained undissolved. The mixture was stirred under nitrogen. Then iodomethane (100 μl, 1.62 mmol) was injected, and the reaction was stirred overnight. Water (20 ml) was added, and reaction mixture was extracted with chloroform (3 × 25 ml). The chloroform extract was washed with brine solution (2 × 25 ml), dried over MgSO4, filtered, and evaporated. The residue was purified by column chromatography by using petroleum ether/ether (6:4) as eluent (yield: 77%). NMR and GC/MS analyses indicated that methylation had taken place at the carboxyl position only. Extract A was methylated by the same method.
Tissue Preparation.
Isolated mesenteric artery segments were prepared from male Sprague–Dawley rats (185–200 g), and the contractile responses of phenylephrine precontracted preparations were monitored by using a wire myograph under conditions described in ref. 18. Vasodilator responses were expressed as percentage relaxation of the phenylephrine-induced tone. The functional integrity of the endothelium was verified in all preparations by >90% relaxation elicited by 10 μM acetylcholine. Endothelial denudation was achieved by rubbing the inside of the vessel with a mounting wire and verified by the loss of the relaxing response to 10 μM acetylcholine (>10% residual relaxation). Concentration–response curves were generated by cumulative addition of an agonist. Antagonists were added 20 min before the agonist and remained in the medium throughout the test period.
Segments of the abdominal aorta were from male Sabra rats (300 g) obtained from the animal facility of Hebrew University. Rats were anesthetized by pentobarbital (50 mg kg−1 i.p.), and the abdominal aorta was excised and transferred to a dish filled with Krebs–Henseleit solution, cleared of periadventitial tissue, and cut into 3-mm-long ring segments. The rings were suspended in a 10-ml organ bath gassed with 5% CO2 in O2 and maintained at 37°C by using two stainless steel hooks, one of which was attached to an isometric force transducer (BIOPAC Systems, Goleta, CA). The rings were stretched to a basal tension of 1.0 g and were equilibrated for 60 min with the medium changed every 15–20 min. The segment was then precontracted by 5 μM phenylephrine. Concentration–response curves were generated by cumulative addition of the agonist. Indomethacin dissolved in 5% wt/vol NaHCO3 solution was added to the organ bath to a final concentration of 10 μM.
Cell Culture.
HUVEC were maintained in primary culture as described in ref. 48. Preconfluent cultures (two to five passages) were incubated with vehicle or agonist in the presence or absence of an antagonist, as described below. As for the RAW 264.7 macrophages, the cells were cultured at 37°C in a humid atmosphere of 5% CO2 for 6 h in DMEM with 10% FCS and all supplements.
Western Blotting.
Phosphorylated and unphosphorylated forms of protein kinase B/Akt and p42/44 MAP kinase were visualized by Western blotting using appropriate antibodies as described earlier (48).
Ligand Binding.
ARA-S binding to CB1 receptors was assessed in displacement assays by using 0.5 nM [3H]CP-55,940 as the labeled ligand and 1 μM SR141716 to determine nonspecific binding, using crude plasma membranes from mouse cerebellum (49). ARA-S binding to CB2 receptors was assayed similarly by using 1.0 nM [3H]CP-55,940 and 0.5 μM SR144528 in HEK293 cells transfected with rat CB2 receptors (50). TRPV1 receptor binding competition assays were done by using CHO cells transfected with the rat TRPV1 receptor, [3H]resiniferotoxin as the labeled ligand, and 1 μM unlabeled resiniferotoxin to determine nonspecific binding (51).
Murine Macrophages.
Peritoneal exudate macrophages from 8- to 9-week-old C57BL/6 female mice were harvested 4 days after injection of 1.5 ml of 3% thioglycolate medium. Peritoneal macrophages were cultured in 96-microwell flat bottomed plates. Two hours later the cells were rinsed to remove unattached cells. After activation with LPS (1 μg/ml), ARA-S diluted to various concentrations with DMEM was added to the cells. After 24-h incubation, supernatants were collected and stored at −20°C until assayed for TNF-α and NO.
Plasma TNF-α Levels in Endotoxemic Mice.
Male C57Bl6/J, CB1−/−, and CB2−/− mice were pretreated with the indicated drug 45 min before an i.p. injection of 1 mg/kg LPS. After an additional 90 min, the mice were decapitated, and trunk blood was collected for determination of TNF-α levels. ARA-S and Abn-CBD were dissolved in one part DMSO, one part Tween 80, and four parts PBS, and controls were treated with the same vehicle.
Reactive Oxygen Intermediate Assay.
RAW 264.7 cells, suspended in HBSS without phenol red, were distributed in plastic luminometer tubes. ARA-S was added to the samples followed by addition of 10 μl of luminol and 30 μl of zymosan (53). The chemiluminescense peak was then recorded by luminometer (Biomate LB 9500 T, Berthold, Wildbad, Germany).
NO Determination.
NO was determined by measuring the accumulated nitrite in the supernatants of ARA-S-treated peritoneal macrophages (52).
TNF-α Determination.
TNF-α (pg/ml) in cell culture supernatants or in mouse blood plasma was determined by “sandwich” ELISA technique. ELISA reagents were used according to the manufacturer’s protocol (R & D Systems).
Supplementary Material
Acknowledgments
We thank the National Institute on Drug Abuse for Grant DA 9789 (to R.M.). Work done in the U.S. laboratory was supported by intramural National Institutes of Health funds.
Glossary
Abbreviations:
- CBD
cannabidiol
- Abn-CBD
abnormal CBD
- ARA-S
N-arachidonoyl-l-serine
- HUVEC
human umbilical vein endothelial cell
- PTX
pertussis toxin
- TMS
trimethyl-silyl
- MAP
mitogen-activated protein.
Footnotes
Conflict of interest statement: No conflicts declared.
References
- 1.Gaoni Y., Mechoulam R. J. Am. Chem. Soc. 1964;86:1646–1647. [Google Scholar]
- 2.Iversen L. L. The Science of Marijuana. New York: Oxford Univ. Press; 2000. [Google Scholar]
- 3.Devane W. A., Dysarz F. A., Johnson M. R., Melvin L. S., Howlett A. C. Mol. Pharmacol. 1988;34:605–613. [PubMed] [Google Scholar]
- 4.Munro S., Thomas K. L., Abu-Shaar M. Nature. 1993;365:61–65. doi: 10.1038/365061a0. [DOI] [PubMed] [Google Scholar]
- 5.Matsuda L. A., Lolait S. J., Brownstein M. J., Young A. C., Bonner T. I. Nature. 1990;346:561–564. doi: 10.1038/346561a0. [DOI] [PubMed] [Google Scholar]
- 6.Howlett A. C., Barth F., Bonner T. I., Cabral G., Casellas P., Devane W. A., Felder C. C., Herkenham M., Mackie K., Martin B. R., et al. Pharmacol. Rev. 2002;54:161–202. doi: 10.1124/pr.54.2.161. [DOI] [PubMed] [Google Scholar]
- 7.Pazos M. R., Núñez E., Benito C., Tolón R. M., Romero J. Life Sci. 2004;75:1907–1915. doi: 10.1016/j.lfs.2004.03.026. [DOI] [PubMed] [Google Scholar]
- 8.Golech S. A., McCarron R. M., Chen Y., Bembry J., Lenz F., Mechoulam R., Shohami E., Spatz M. Mol. Brain Res. 2004;132:87–92. doi: 10.1016/j.molbrainres.2004.08.025. [DOI] [PubMed] [Google Scholar]
- 9.Jarai Z., Wagner J. A., Varga K., Lake K. D., Compton D. R., Martin B. R., Zimmer A. M., Bonner T. I., Buckley N. E., Mezey E., et al. Proc. Natl. Acad. Sci. USA. 1999;96:14136–14141. doi: 10.1073/pnas.96.24.14136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Begg M., Pacher P., Batkai S., Osei-Hyiaman D., Offertaler L., Mo F.-M., Liu J., Kunos G. Pharmacol. Ther. 2005;106:133–145. doi: 10.1016/j.pharmthera.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 11.Devane W. A., Hanus L., Breuer A., Pertwee R. G., Stevenson L. A., Griffin G., Gibson D., Mandelbaum A., Etinger A., Mechoulam R. Science. 1992;258:1946–1949. doi: 10.1126/science.1470919. [DOI] [PubMed] [Google Scholar]
- 12.Mechoulam R., Ben-Shabat S., Hanus L., Ligumsky M., Kaminski N. E., Schatz A. R., Gopher A., Almog S., Martin B. R., Compton D. R. Biochem. Pharmacol. 1995;50:83–90. doi: 10.1016/0006-2952(95)00109-d. [DOI] [PubMed] [Google Scholar]
- 13.Sugiura T., Kondo S., Sukagawa A., Nakane S., Shinoda A., Itoh K., Yamashita A., Waku K. Biochem. Biophys. Res. Commun. 1995;215:89–97. doi: 10.1006/bbrc.1995.2437. [DOI] [PubMed] [Google Scholar]
- 14.Bradshaw H. B., Walker J. M. Br. J. Pharmacol. 2005;144:459–465. doi: 10.1038/sj.bjp.0706093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kunos G., Jarai Z., Batkai S., Goparaju S. K., Ishac E. J., Liu J., Wang L., Wagner J. A. Chem. Phys. Lipids. 2000;108:159–168. doi: 10.1016/s0009-3084(00)00194-8. [DOI] [PubMed] [Google Scholar]
- 16.Hiley C. R., Ford W. R. Biol. Rev. Camb. Philos. Soc. 2004;79:187–205. doi: 10.1017/s1464793103006201. [DOI] [PubMed] [Google Scholar]
- 17.Sugiura T., Kobayashi Y., Oka S., Waku K. Prostaglandins Leukotrienes Essent. Fatty Acids. 2002;66:173–192. doi: 10.1054/plef.2001.0356. [DOI] [PubMed] [Google Scholar]
- 18.Offertaler L., Mo F.-M., Batkai S., Liu J., Begg M., Razdan R. K., Martin B. R., Bukoski R. D., Kunos G. Mol. Pharmacol. 2003;63:699–705. doi: 10.1124/mol.63.3.699. [DOI] [PubMed] [Google Scholar]
- 19.Ho W. S., Hiley C. R. Br. J. Pharmacol. 2004;138:1320–1332. doi: 10.1038/sj.bjp.0705160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O’Sullivan S. E., Kendall D. A., Randall M. D. Br. J. Pharmacol. 2004;142:435–442. doi: 10.1038/sj.bjp.0705810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sheskin T., Hanus L., Slager J., Vogel Z., Mechoulam R. J. Med. Chem. 1997;40:659–667. doi: 10.1021/jm960752x. [DOI] [PubMed] [Google Scholar]
- 22.Randall M. D., Harris D., Kendall D. A, Ralevic V. Pharmacol. Ther. 2002;95:191–202. doi: 10.1016/s0163-7258(02)00258-9. [DOI] [PubMed] [Google Scholar]
- 23.Randall M. D., Kendall D. A. Trends Pharmacol. Sci. 1998;19:55–58. doi: 10.1016/s0165-6147(97)01161-9. [DOI] [PubMed] [Google Scholar]
- 24.Ledent C., Valverde O., Cossu G., Petitet F., Aubert J. F., Beslot F., Bohme G. A., Imperato A., Pedrazzini T., Roques B. P., et al. Science. 1999;283:401–404. doi: 10.1126/science.283.5400.401. [DOI] [PubMed] [Google Scholar]
- 25.Pacher P., Batkai S., Kunos G. J. Physiol. (London) 2004;558:647–657. doi: 10.1113/jphysiol.2004.064824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wagner J. A., Abesser M., Karcher J., Laser M., Kunos G. J. Cardiovasc. Pharmacol. 2005;46:348–355. doi: 10.1097/01.fjc.0000175437.87283.f2. [DOI] [PubMed] [Google Scholar]
- 27.Gebremedhin D., Lange A. R., Campbell W. B., Hillard C. J., Harder D. R. Am. J. Physiol. 1999;276:H2085–H2093. doi: 10.1152/ajpheart.1999.276.6.H2085. [DOI] [PubMed] [Google Scholar]
- 28.Chaytor A. T., Martin P. E., Evans W. H., Randall M. D., Griffith T. M. J. Physiol. (London) 1999;520:539–550. doi: 10.1111/j.1469-7793.1999.00539.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.White R., Ho W. S., Bottrill F. E., Ford W. R., Hiley C. R. Br. J. Pharmacol. 2001;134:921–929. doi: 10.1038/sj.bjp.0704333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O’Sullivan S. E., Kendall D. A., Randall M. D. Br. J. Pharmacol. 2004;141:803–812. doi: 10.1038/sj.bjp.0705643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wagner J. A., Varga K., Jarai Z., Kunos G. Hypertension. 1999;33:429–434. doi: 10.1161/01.hyp.33.1.429. [DOI] [PubMed] [Google Scholar]
- 32.Mukhopadhyay S., Chapnick B. M., Howlett A. C. Am. J. Physiol. 2002;282:H2046–H2054. doi: 10.1152/ajpheart.00497.2001. [DOI] [PubMed] [Google Scholar]
- 33.O’Sullivan S. E., Kendall D. A., Randall M. D. Br. J. Pharmacol. 2005;145:514–526. doi: 10.1038/sj.bjp.0706218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huang S. M., Bisogno T., Trevisani M., Al-Hayani A., De Petrocellis L., Fezza F., Tognetto M., Petros T. J., Krey J. F., Chu C. J., et al. Proc. Natl. Acad. Sci. USA. 2002;99:8400–8405. doi: 10.1073/pnas.122196999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Porter A. C., Sauer J. M., Knierman M. D., Becker G. W., Berna M. J., Bao J., Nomikos G. G., Carter P., Bymaster F. P., Leese A. B., et al. J. Pharmacol. Exp. Ther. 2002;301:1020–1024. doi: 10.1124/jpet.301.3.1020. [DOI] [PubMed] [Google Scholar]
- 36.Ho W. S., Hiley C. R. J. Pharm. Pharmacol. 2003;56:869–875. doi: 10.1211/0022357023682. [DOI] [PubMed] [Google Scholar]
- 37.Mo F.-M., Offertaler L., Kunos G. Eur. J. Pharmacol. 2004;489:21–27. doi: 10.1016/j.ejphar.2004.02.034. [DOI] [PubMed] [Google Scholar]
- 38.Walter L., Franklin A., Witting A., Wade C., Xie Y., Kunos G., Mackie K., Stella N. J. Neurosci. 2003;23:1398–1405. doi: 10.1523/JNEUROSCI.23-04-01398.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Harris A., McCulloch A. I., Kendall D. A., Randall M. D. J. Physiol. 2002;539:893–902. doi: 10.1113/jphysiol.2001.013489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ralevic V., Kendall D. A., Randall M. D., Smart D. Life Sci. 2002;71:2577–2594. doi: 10.1016/s0024-3205(02)02086-6. [DOI] [PubMed] [Google Scholar]
- 41.Zygmunt P. M., Petersson J., Anderson D. A., Chuang H., Sorgard M., Di Marzo V., Julius D., Hogestatt E. D. Nature. 1999;400:452–457. doi: 10.1038/22761. [DOI] [PubMed] [Google Scholar]
- 42.Pratt P. F., Hillard C. J., Edgemond W. S., Campbell W. B. Am. J. Physiol. 1998;274:H375–H381. doi: 10.1152/ajpheart.1998.274.1.H375. [DOI] [PubMed] [Google Scholar]
- 43.Gauthier K. M., Baewer D. V., Hittner S., Hillard C. J., Nithipatikom K., Reddy D. S., Falck J. R., Campbell W. B. Am. J. Physiol. 2005;288:H1344–H1351. doi: 10.1152/ajpheart.00537.2004. [DOI] [PubMed] [Google Scholar]
- 44.Sancho R., Calzado M. A., Di Marzo V., Appendino G., Munoz E. Mol. Pharmacol. 2003;63:429–438. doi: 10.1124/mol.63.2.429. [DOI] [PubMed] [Google Scholar]
- 45.Mechoulam R., Parker L. A., Gallily R. J. Clin. Pharmacol. 2002;42:11S–19S. doi: 10.1002/j.1552-4604.2002.tb05998.x. [DOI] [PubMed] [Google Scholar]
- 46.Zurier R. B. J. Cell Biochem. 2003;88:462–466. doi: 10.1002/jcb.10291. [DOI] [PubMed] [Google Scholar]
- 47.Razdan R. K., Dalzell H. C., Handrick G. R. J. Am. Chem. Soc. 1974;96:5860–5865. doi: 10.1021/ja00825a026. [DOI] [PubMed] [Google Scholar]
- 48.Liu J., Gao B., Mirshahi F., Sanyal A. J., Khanolkar A. D., Makriyannis A., Kunos G. Biochem. J. 2000;346:835–840. [PMC free article] [PubMed] [Google Scholar]
- 49.Aung M. M., Griffin G., Huffman J. W., Wu M., Keel C., Yang B., Showalter V. M., Abood M. E., Martin B. R. Drug Alcohol Depend. 2000;60:133–140. doi: 10.1016/s0376-8716(99)00152-0. [DOI] [PubMed] [Google Scholar]
- 50.Griffin G., Tao Q., Abood M. E. J. Pharmacol. Exp. Ther. 2000;292:886–894. [PubMed] [Google Scholar]
- 51.Szallasi A., Blumberg P. M., Annicelli L. L., Krause J. E., Cortright D. N. Mol. Pharmacol. 1999;56:581–587. doi: 10.1124/mol.56.3.581. [DOI] [PubMed] [Google Scholar]
- 52.Brenner T. A., Yamin A., Gallily R. Brain Res. 1994;641:51–56. doi: 10.1016/0006-8993(94)91814-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.