Abstract
The ovalbumin323–339 peptide that binds H2I-Ab was engineered into the globular heads of hemagglutinin (H) molecules from serologically non-cross-reactive H1N1 and H3N2 influenza A viruses, the aim being to analyze recall CD4+ T cell responses in a virus-induced respiratory disease. Prime/challenge experiments with these H1ova and H3ova viruses in H2b mice gave the predicted, ovalbumin-specific CD4+ T cell response but showed an unexpectedly enhanced, early expansion of viral epitope-specific CD8+ T cells in spleen and a greatly diminished inflammatory process in the virus-infected respiratory tract. At the same time, the primary antibody response to the H3N2 challenge virus was significantly reduced, an effect that has been associated with preexisting neutralizing antibody in other experimental systems. Analysis of serum from the H1ova-primed mice showed low-level binding to H3ova but not to the wild-type H3N2 virus. Experiments with CD4+ T cell-depleted and Ig−/− mice indicated that this cross-reactive Ig is indeed responsible for the modified pathogenesis after respiratory challenge. Furthermore, the effect does not seem to be virus-dose related, although it does require infection. These findings suggest intriguing possibilities for vaccination and, at the same time, emphasize that engineered modifications in viruses may have unintended immunological consequences.
Keywords: cross-reactivity, vaccines
Many of the vaccination strategies for promoting cell-mediated immunity against lethal pathogens such as HIV use other RNA or DNA viruses that have been engineered to incorporate sequences encoding foreign peptides (1). Such protocols can involve DNA priming followed by boosting with the modified vector, which is generally a high-titer, infectious (but nonreplicating) or severely attenuated virus. Sometimes two different vectors, such as vaccinia and adenovirus, are used for the primary and secondary challenges. Prime/boost studies with selectively mutated viruses have also facilitated the experimental dissection of, in particular, virus-specific CD8+ T cell responses. The laboratory strain A/PR/8/34 (PR8, H1N1) and A/HK/x31 (Hkx31, H3N2) influenza A viruses have been used extensively for this purpose (2, 3).
The preferred site for peptide insertion in the influenza A viruses has generally been the stalk of the viral neuraminidase (N) molecule, which can tolerate an additional 40 or so additional amino acids without obvious functional compromise (4). However, some molecules do not express in the N, so an alternative protocol (5) is to modify the globular head of the viral hemagglutinin (HA or H). This protocol has been used successfully to insert both CD8+ T cell and B cell epitopes. N and HA are the two principal glycoproteins expressed on the surface of the influenza A viruses and, as such, are subject to antibody-mediated selection pressure. The HA binds to sialic acid and plays a key part in virus entry, whereas the N has the opposite role of facilitating the release of new virus progeny.
“Antigenic drift” in, particularly, the HA is responsible for the periodic epidemics associated with, for instance, the Hong Kong (H3N2) influenza A viruses that have been causing severe human disease for more than 30 years (5). Many of these natural variants emerge as a consequence of mutational changes that modify the globular head of the HA molecule and abrogate or diminish the extent of neutralization by antibodies generated as a result of exposure to an earlier iteration of the H3 molecule (6). More distant influenza strains, such as the H1N1 “human” viruses or the H5N1 “avian” strains, induce responses that show no evidence of cross-neutralization, either with each other or with H3N2 isolates. A mutation in the HA of what may have originally been a bird pathogen is thought to have contributed to the extreme pathogenicity of the H1N1 influenza A virus that killed more than 40 million people during the course of the 1918–1919 pandemic (7).
Despite this understanding that glycoprotein structure may be a major determinant of both antigenicity and pathogenicity, little thought is generally given to the possibility that changes other than those that modify fitness (measured by the capacity to replicate) will have any substantial effect on the endogenous response to a viral vector. This was certainly the case when we inserted the coding sequences for an ovalbumin peptide (OVA323–339) into the HA molecules of H1N1 and H3N2 influenza A viruses. The OVA323–339 peptide binds to the H2-IAb MHC class II glycoprotein to form the OT-II epitope; therefore, we anticipated that prime/boost experiments with these two viruses (H1ova and H3ova) in C57BL/6J H2b (B6) mice would promote significant clonal expansion of OT-II-specific CD4+ T cells. The expected result was achieved, but the surprise was the generation of a cross-reactive, although weak, antibody response (between H1ova and H3ova) that modified the characteristics of secondary influenza-specific CD8+ T cell-mediated immunity. This unpredicted finding has obvious implications for vaccines based upon viral vectors that may be subject to preexisting antibody responses within a population.
Results
Virus Clearance and CD4+ T Cell and Antibody Responses.
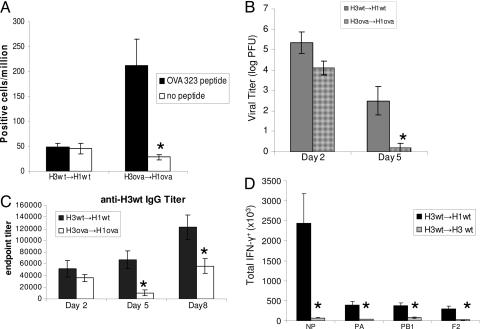
These H1ova (Fig. 1) and H3ova viruses were generated to analyze a possible role for OT-II-specific CD4+ T cells (8) in the H3N2→H1N1 influenza A virus prime/boost model that we routinely use to dissect virus-specific CD8+ T cell-mediated immunity (9). Although infection of naïve B6 mice with either the H1ova or H3ova viruses did not induce a detectable, acute OT-II-specific CD4+ T cell response (data not shown), it was apparent that the memory compartment had been primed because significant numbers of OT-II-specific T cells were found in spleen after a secondary challenge (Fig. 2A). Furthermore, although the engineered H3ova virus grows to much the same extent as the wild-type (wt) H3 virus in the lungs of naïve mice (H3ova, 6.6 ± 0.54; H3wt, 7.3 ± 0.14), those that had been injected i.p. with the H1ova virus 6 weeks earlier cleared a subsequent H3ova infection more rapidly than the H3wt→H1wt controls (Fig. 2B).
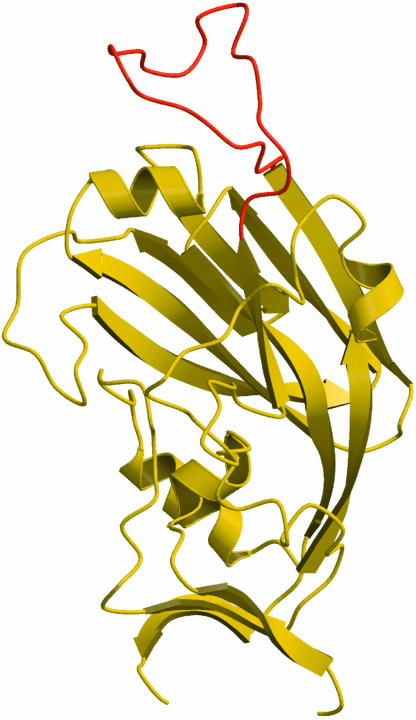
Fig. 1.
Model depicting the insertion of the OVA323–339 peptide (red) into the globular head of H1 (yellow). The engineered H3 is essentially identical. The insertion site is in the loop near antigenic site B. Although the structure of the loop with the OVA peptide is hypothetical, it illustrates why the change is likely to promote antibody binding. This model was generated by S. White (St. Jude Children’s Research Hospital).
Fig. 2.
The response to secondary challenge, measured for five mice per group. (A) Quantification of OT-II-specific CD4+ T cells by ELISPOT analysis of spleen on day 8. (B) Virus titers in lung as determined by Madin–Darby canine kidney (MDCK) cell plaque assay. (C) Serum antibody titers measured by antigen-specific ELISA on days 2, 5, and 8 of secondary challenge. (D) Absence of a CD8+ T cell response on day 8 after homologous challenge of H3wt-infected mice. Results are expressed as mean ± SE (n = 5); ∗, P < 0.05.
Given that cross-reactive helper T cells had been primed (Fig. 2B), an obvious question was whether priming in any way enhanced the antibody response to the engineered H3ova virus. Paradoxically, both the virus-specific (Fig. 2C) and the H1 (data not shown) antibody responses were substantially reduced for the H3ova→H1ova combination. This was exactly opposite of the predicted result but was reminiscent of experiments with other model systems in which a small amount of preexisting virus-specific Ig can be shown to diminish the development of a naïve B cell response (10). The next step, therefore, was to look at serum from mice that had been primed only with the H1ova virus. The results indicated (Table 1) that exposure to the modified H1 of the H1ova virus (Fig. 1) generated a low-level antibody response specific for the comparably engineered H3 of the H3ova virus.
Table 1.
Serological cross-reactivity for the H3 viruses after priming with the H1 viruses
| Serological test | No. of positive mice/no. of mice primed |
|||
|---|---|---|---|---|
| H1wt serum |
H1ova serum |
|||
| Against H3wt virus | Against H3ova virus | Against H3wt virus | Against H3ova virus | |
| Hemagglutination inhibition | 0/5 | 0/5 | 0/4 | 4/4 1:35 average titer |
| MDCK virus neutralization | 0/6 | 0/6 | 0/6 | 3/6 1:100 average titer of positives |
| Embryonated hen egg neutralization | 0/5 | 0/5 | 1/4 >1:40 average titer of positives | 4/4 >1:40 average titer |
The hemagglutination inhibition and neutralization tests utilized serum taken at least 7 weeks after i.p. priming with the H1wt and H1ova viruses.
Consequences for the CD8+ T Cell Response.
What are the effects of primed CD4+ T help (Fig. 2A) (11) and low-level cross-reactive Ig on secondary CD8+ T cell responses? On one hand, high-titer neutralizing antibody is known to block CD8+ T cell stimulation, presumably because elimination of the input inoculum (12) prevents epitope expression on antigen-presenting cells. This suppressive effect can be seen for the homologous H3wt→H3wt challenge shown here (Fig. 2D). On the other hand, partially cross-reactive influenza HA-specific antibody does allow some reduced clonal expansion after secondary challenge (12). The low-titer HA-OT-II-specific Ig (Table 1) generated in the current experimental system does not significantly inhibit the initial phase of virus growth in the lung (day 2, Fig. 2B), so a secondary virus-specific CD8+ T cell response would be expected.
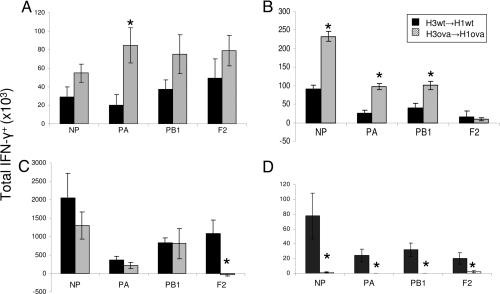
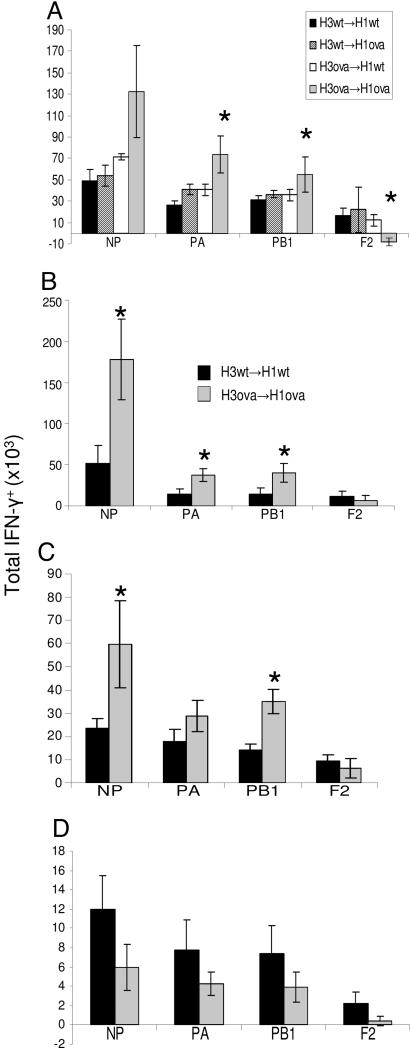
In fact, the development of the various virus-specific CD8+ T cell sets in spleen after the H3ova→H1ova challenge seemed to be significantly enhanced for all except the PB1-F2 epitope (Fig. 3 A–C). Even so, although this increase was apparent at days 2 and 5 (Fig. 3A and B), the NP, PA, and PB1 responses for the H3ova→H1ova and H3wt→H1wt challenges measured on day 8 were equivalent in magnitude (Fig. 3C). Paradoxically, despite the apparently enhanced kinetics in lymphoid tissue, the recruitment of virus-specific CD8+ T cells to the infected lung was greatly diminished for the H1ova→H3ova challenge (Fig. 3D).
Fig. 3.
Measuring epitope-specific CD8+ T cell responses in spleen on day 2 (A), day 5 (B), and day 8 (C) and bronchoalveolar lavage (BAL) on day 5 (D) for the H3wt→H1wt and H3ova→H1ova challenges. Influenza virus epitopes are as follows: NP, nucleoprotein DbNP366-374; PA and PB1, RNA polymerase subunits PA (DbPA224-233) and PB1 (KbPB1703-711); F2, an alternatively spliced PB1 (DbPB1-F262-70). Results were determined by intracellular cytokine (IFN-γ) staining and are expressed as mean ± SE (n = 5); ∗, P < 0.05. Experiments on each day were repeated at least twice.
Possible Virus Dose Effects.
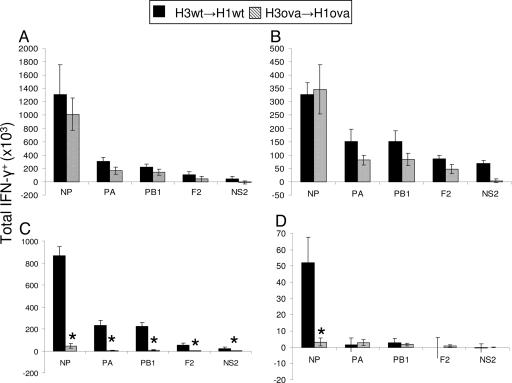
The immediate interpretation of the decreased localization of virus-specific CD8+ T cells to the infected lung (Fig. 3D) was that it might reflect substantial neutralization (Table 1) of the inoculum at the time of respiratory challenge, although such an effect was not apparent from the lung virus titers measured on day 2 (Fig. 2B). However, although both the generation of epitope-specific CD8+ T cells in the lymphoid tissue (spleen, Fig. 4A and B) and subsequent localization to the bronchoalveolar lavage (BAL) (Fig. 4 C and D) were greatly diminished in the mice given a low-titer inoculum (Fig. 4, compare A with B and C with D), dropping the intranasal (i.n.) dose 100-fold (Fig. 4 A–D) reproduced the differential spleen/BAL relationships for the H3ova→H1ova and H3wt→H1wt challenges seen previously on day 8 (Fig. 3A–D). The minimal inflammatory response in the lungs of the H3ova→H1ova mice is not, therefore, due to a reduced virus challenge.
Fig. 4.
Epitope-specific CD8+ T cell responses in spleen (A and B) and BAL (C and D) after high-dose [106 egg 50% infectious dose (EID50)] (A and C) or low-dose (104 EID50) (B and D) secondary intranasal (i.n.) challenge. NS2, nonstructural protein 2. Representative data from two independent experiments are shown. Results were determined by intracellular cytokine staining on day 8 after challenge and are expressed as mean ± SE (n = 5); ∗, P < 0.05.
The next question was whether the apparent enhancement of the response in the spleen on day 5 (Fig. 3B) depended on virus replication. Productive infection with the influenza A viruses requires the presence of an enzyme that cleaves the viral HA but is restricted in distribution to the mouse respiratory tract (13). After i.p. exposure, infected cells will produce new protein but no progeny virus. The i.n. challenge experiment was thus repeated with high-dose [106 egg 50% infective dose (EID50)], heat-inactivated virus, which is known to prime a CD8+ T cell response (14) and for an i.p. boost with live virus. In both cases (data not shown), the enhanced response observed in the spleen on day 5 after i.n. challenge with infectious virus (Fig. 3B) was not reproduced.
Effect of CD4+ T Cell and Antibody Responses.
The increase in spleen CD8+ T cell numbers seen on day 5 (Fig. 3B) for the secondary H3ova challenge is absolutely dependent on prior exposure (H1ova priming, Fig. 5A) to the OVA-modified H1 molecule. Priming with H1wt and challenging with H3ova gives an equivalent response to challenging with H3wt. This response includes the full expansion of the BAL response (data not shown), providing further evidence that the introduced epitope does not significantly affect the fitness of the virus and proving the requirement for memory in the observed modulation of the response. Does this response reflect the concurrent restimulation of primed, OT-II-specific CD4+ helper T cells, or is it in some way related to the fact that low-level, cross-reactive antibody (Table 1) is present from the time of secondary challenge? Eliminating the CD4+ T cells by treatment with the GK1.5 monoclonal antibody to CD4 decreased the overall magnitude of the response but did not obviously change the differential epitope-specific CD8+ T cell response profiles (Fig. 3B and Fig. 5A) found for the H3wt→H1wt and H3ova→H1ova challenges (Fig. 5 B and C). Thus, although CD4+ T cells may well be needed for the development of the cross-reactive antibody found in the H1ova-immune mice, they are not required for the effect on the CD8+ T cell response (Fig. 3B and Fig. 5A) seen after the H3ova challenge. Furthermore, the pattern of early, differential virus clearance on day 5 was not modified for CD4-depleted or CD8-depleted H3ova→H1ova-primed mice (data not shown). There is a substantial body of earlier evidence that the influenza A viruses can be controlled by either CD8+ T cell or CD4+ T help/antibody response (15, 16).
Fig. 5.
Splenic enhancement phenotype is dependent on a primed B-cell response. (A) The enhanced spleen response is seen only for the H3ova→H1ova combination. H3ova→H1wt and H3wt→H1ova infections produce responses equivalent to H3wt→H1wt. (B and C) Depleting the CD4+ T cells by treatment with the GK1.5 monoclonal antibody (C) every second day from day 3 before secondary challenge (30) causes some decrease in the overall magnitude of the response vs. undepleted mice (B) but does not change the enhancement characteristic of the H3ova→H1ova challenge. These data are representative of three independent experiments. The percentage of CD4+ T cells found by flow cytometric analysis of spleen was always <2% in the depleted mice. (D) The response in Ig−/− μMT (B cell knockout) mice after secondary challenge with the indicated viruses. All results were measured by intracellular cytokine staining on day 5 and are expressed as mean ± SE (n = 5); ∗, P < 0.05.
It seems possible, then, that this effect (Fig. 3B and Fig. 5 C and D) is mediated by low-level, cross-reactive antibody that does not require CD4+ T cell help after secondary exposure (Fig. 5 B and C). The fact that repeating the basic analysis in Ig−/− μMT mutants did not reproduce the differentials found for the H3wt→H1wt and H3ova→H1ova prime/boost in Ig+/+ B6 mice (Fig. 5D) supports this interpretation. The overall magnitude of the response in the Ig−/− μMTs was greatly reduced because of their much smaller spleen size, but the day 5 responses for the H3ova→H1ova and H3wt→H1wt combinations were not significantly different (Fig. 5D). Moreover, equivalent BAL responses were measured in these mice after the H3wt→H1wt and H3ova→H1ova challenges (data not shown).
Discussion
By using a prime/challenge system in which two serodistinct viruses have been engineered to contain a short identical sequence, we have shown that a cross-reactive antibody response that does not fully neutralize infection allows the development of a full CD8+ T cell response and leads to the accumulation of antigen-specific T cells in the spleen rather than at the site of infection. These findings bear upon the important question of how preexisting antibody may affect the efficacy of viral vector-based vaccines. In this case, in the presence of nonsterilizing partial immunity, a robust CD8+ T cell response was generated although not at the site of infection. This is an important consideration for the screening of the effectiveness of viral vectors that may be subject to preexisting immunity within a population. Furthermore, these results suggest a new vaccine design strategy in which a weak cross-reactive antibody response is generated to boost the generation of CD8+ T cell responses to a viral vector while limiting any significant pathology of the vector itself.
Prior experiments with conventional HA-specific monoclonal antibodies suggest that such low-level protection can indeed occur (15). The HAova-specific antibodies do not bind to native OVA (in ELISA, data not shown), and it seems that a new (although minimal) “influenza HA” antibody epitope has been generated. The Ig-mediated effect does not seem to be operating through direct neutralization of the input inoculum, perhaps reflecting that a measure of virus-induced damage (or endothelial activation) must occur in the respiratory tract before the serum HAova-specific Ig is able to access the luminal, type 1 respiratory epithelium that supports influenza virus growth (17).
Despite the possibility that a measure of virus-induced damage to the lung is important in the pathogenesis of this infectious process, it is also the case that the extent of inflammatory pathology is minimal in the H3ova→H1ova-primed mice. The very small numbers of epitope-specific CD8+ T cells recovered from this site are simply a reflection of the fact that the magnitude of mononuclear cell invasion into the infected lung is massively reduced. Although we present the data as epitope-specific CD8+ T cell counts, the immunodominant DbNP366–374-specific set (18) was always the most prevalent influenza-specific component in the BAL population recovered from the H3ova→H1ova mice, indicating that, as is generally the case, there is no selectivity in recruitment to the site of pathology.
The minimal inflammatory process may also explain the diminished response to the PB1-F2 epitope. The lack of clonal expansion for the PB1-F2-specific set suggests that these T cells are not primed in the same “window” as the NP, PA, and PB1 responses, perhaps reflecting that PB1-F2 is not a component of the virus particle but instead is generated from an alternative reading frame that is primarily expressed subsequent to productive infection (19). It is also likely that, because there will be both less damage and decreased cytokine production in the infected lung, the transfer of activated dendritic cells from the respiratory tract to the regional lymphoid tissue via afferent lymph may be substantially diminished for the H3ova→H1ova versus the H3wt→H1wt challenge (20). However, it is not known whether differential dendritic cell activation and/or availability has any particular effect for the PB1-F2 epitope.
The fact that the apparent enhanced response kinetics for influenza-specific CD8+ T cell epitopes (other than PB1-F2) in spleen was seen only after i.n. challenge with infectious virus may simply reflect the delayed exit of immune T cells from the spleen. The implication is therefore that, in a situation in which there is a “normal” level of inflammatory process in the target organ, restimulated memory T cells are moving out of the lymphoid tissue as early as day 2 after infection. This hypothesis implies that between these two compartments there is “cross talk” which must, presumably, be mediated through circulating cytokines generated in the site of pathology.
It is often suggested that antibody and CD8+ T cell responses are in direct opposition because both are antigen-dependent and because reduced availability (due to neutralization) would lead to diminished CD8+ T cell numbers (21). This suggestion has caused some concerns about the usefulness of viral vectors where preexisting antibody might be circulating in the population. Instead, we found that the overall size of the CD8+ T cell response is not altered by (at least) low level, cross-reactive antibody. In other model systems, particularly in lymphocytic choriomeningitis and respiratory syncytial viruses, CD8+ T cell responses expand even in the presence of strongly neutralizing Ig, although high virus titers are necessary and T cell proliferation is thought to occur at the site of pathology, producing the pathological changes characteristic of primary challenge (22, 23). The data from the H3ova→H1ova challenge indicate that the clonal expansion of CD8+ T cells in lymphoid tissue is not (except for PB1-F2) directly tuned to the degree of inflammation in an anatomically remote target site such as the lung and, even in the secondary response, follows a predetermined program.
There is also a general lesson to be learned from this analysis. As with genetically manipulated mice (24), it is unwise to come to any substantial conclusions concerning the possible effects of mutating, or otherwise modifying, an infectious virus for immunity without making a detailed, multiparameter analysis. If the current experiment had looked only at the day 5 response in spleen and virus clearance from the lung of infected B6 mice, the conclusion might well have been reached that priming the OT-II-specific CD4+ set leads directly to a more substantial virus-specific CD8+ T cell response that promotes rapid recovery. This is one of the many reasons, including safety (25), that, where possible, any proposed use of replicating, engineered “vaccine” reagents in humans should be preceded by a detailed analysis of mechanism in appropriate laboratory animal models.
The other speculation arising from these studies is that it may be possible to modify the key antigenic sites of influenza A viruses to promote low-level antibody responses that, although they may not prevent infection, could provide a measure of protection, enhance recovery, and allow the full expansion of the CD8+ T cell response. Preliminary experiments (data not shown) in which we mutated the globular head of the H1 glycoprotein to mimic a peptide from the H3 molecule that is known to stimulate CD4+ T cells seemed to give an effect similar to that described here for the OVA-modified viruses. Can viral glycoproteins be engineered to give cross-reactive antibody responses that might not normally be stimulated after natural infection but may nonetheless provide some protection against, say, a previously unencountered, virulent influenza A virus?
Materials and Methods
Viruses, Mice, and Sampling.
Reverse genetics protocols (26, 27) were used to insert the OVA323–339 sequence (ISQAVHAAHAEINEAGR) after the glycines at residue 173 of the H1 (PR8, H1N1) and 174 of the H3 (the A/Aichi HA of HKx31) HA glycoproteins (Fig. 1). No residues were removed. The resultant H1ova and H3ova viruses were rescued in 10-day-old embryonated chicken eggs after the engineered plasmids were transfected into cocultures of 293 T cells and MDCK cells. Female B6 mice were purchased from The Jackson Laboratory and Ig−/− μMT mice were bred at St. Jude Children’s Research Hospital. All mice were held under specific pathogen-free conditions and generally primed by i.p. injection with 108 EID50 of wt H1 or H1ova viruses. They were then left for 6–8 weeks and, after anesthesia by i.p. injection of 2,2,2-tribromoethanol (Avertin), challenged i.n. with 106 EID50 of the H3wt or H3ova viruses. The mice were anesthetized again at the time of sampling and exsanguinated by sectioning the axillary artery. Inflammatory cell populations were recovered from the infected respiratory tract by BAL, followed by removal of the spleen to prepare single-cell suspensions for lymphocyte analysis and to prepare the lungs for later virus plaque assay.
Measuring Virus-Specific CD8+ T Cells.
Epitope-specific CD8+ T cell responses were analyzed by the intracellular cytokine staining flow cytometry assay. Inflammatory cell populations recovered from the pneumonic lung by BAL were depleted of macrophages by incubation on plastic for 1 h at 37°C. Spleen and BAL lymphocytes were then incubated with 1 μM peptide for 5 h in the presence of 10 μg/ml brefeldin A, fixed with formaldehyde, and stained with CD8α allophycocyanin (53-6.7), IFN-γ phycoerythrin (Pharmingen, catalog no. 554412), and TNF-α FITC (catalog no. 554418). Autofluorescence was gated out by using the FL3 channel. Data were acquired on a Becton Dickinson FACSCalibur and analyzed by using cellquest software. The epitope-specific responses measured were to DbNP366–374, DbPA224–233, DbPB1-F262–70, KbPB1703–711, and KbNS2114–121 (2, 28).
Virus Titration.
Lung titers were determined by using plaque assay on MDCK cells. Near-confluent 25-cm2 monolayers were infected with serial dilutions of lung homogenate (1 ml) for 1 h at 37°C then washed with PBS and 3 ml of MEM containing 1 mg/ml l-1-tosylamido-2-phenylethyl chloromethyl ketone-treated trypsin (Worthington). Agarose (0.8%) was added and the cultures were incubated at 37°C under a 5% CO2 atmosphere for 72 h. Plaques were visualized with crystal violet.
Counting CD4+ T Cells.
An established ELISPOT assay (12) was used to quantify OT-II-specific IFN-γ-producing CD4+ T cells in spleen after stimulation with virus-infected, antigen-presenting cells. Cells were exposed to the OVA323–339 peptide or no peptide, and the number of IFN-γ producers was measured as spots per 106 input cells after 48 h at 37°C.
Antibody Assays.
Standard hemagglutination-inhibition, neutralization, and ELISA protocols were followed (29). The ELISA used virus dried onto plates as an antigen. Mouse sera were treated overnight with Vibrio cholerae receptor-destroying enzyme (Denka-Seiken, Tokyo), heat inactivated for 30 min at 56°C, then assayed by a standard hemagglutination-inhibition protocol (29) by using 4 HA units of virus. Sera were also heat inactivated (as above) for the plaque neutralization assays and only heated (no enzyme treatment) for the egg neutralization assays, diluted serially in PBS, mixed with 100 EID50 of virus, incubated for 30 min at 4°C, then overlaid on MDCK monolayers or injected into 10-day-old embryonated hen’s eggs. After 48 h at 37°C, the eggs were chilled overnight and harvested the next day. Virus that had not been neutralized was detected by hemagglutination (eggs) or as cytopathic effects (MDCK).
Acknowledgments
We thank Dr. Stephen White for generating the model in Fig. 1. This work was supported by U.S. Public Health Service Grants AI29579 and CA21765 (to P.C.D.) and AI065097 (to P.G.T.) and by American Lebanese Syrian Associated Charities at St. Jude Children’s Research Hospital. P.C.D. is a Burnet Fellow of the Australian National Health and Medical Research Council.
Abbreviations
- OVA
ovalbumin
- HA or H
hemagglutinin
- N
viral neuraminidase
- BAL
bronchoalveolar lavage
- MDCK
Madin–Darby canine kidney
- EID50
egg 50%infective dose
- i.n.
intranasal(ly)
- B6
C57BL/6J H2b mice
- wt
wild type.
Footnotes
Conflict of interest statement: No conflicts declared.
References
- 1.Stephenson J. R. Curr. Pharm. Biotechnol. 2001;2:47–76. doi: 10.2174/1389201013378815. [DOI] [PubMed] [Google Scholar]
- 2.Belz G. T., Xie W., Doherty P. C. J. Immunol. 2001;166:4627–4633. doi: 10.4049/jimmunol.166.7.4627. [DOI] [PubMed] [Google Scholar]
- 3.Riberdy J. M., Christensen J. P., Branum K., Doherty P. C. J. Virol. 2000;74:9762–9765. doi: 10.1128/jvi.74.20.9762-9765.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Luo G., Chung J., Palese P. Virus Res. 1993;29:141–153. doi: 10.1016/0168-1702(93)90055-r. [DOI] [PubMed] [Google Scholar]
- 5.Both G. W., Sleigh M. J., Cox N. J., Kendal A. P. J. Virol. 1983;48:52–60. doi: 10.1128/jvi.48.1.52-60.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wiley D. C., Wilson I. A., Skehel J. J. Nature. 1981;289:373–378. doi: 10.1038/289373a0. [DOI] [PubMed] [Google Scholar]
- 7.Gamblin S. J., Haire L. F., Russell R. J., Stevens D. J., Xiao B., Ha Y., Vasisht N., Steinhauer D. A., Daniels R. S., Elliot A., Wiley D. C., Skehel J. J. Science. 2004;303:1838–1842. doi: 10.1126/science.1093155. [DOI] [PubMed] [Google Scholar]
- 8.Robertson J. M., Jensen P. E., Evavold B. D. J. Immunol. 2000;164:4706–4712. doi: 10.4049/jimmunol.164.9.4706. [DOI] [PubMed] [Google Scholar]
- 9.Turner S. J., Diaz G., Cross R., Doherty P. C. Immunity. 2003;18:549–559. doi: 10.1016/s1074-7613(03)00087-6. [DOI] [PubMed] [Google Scholar]
- 10.Crowe J. E., Jr, Firestone C. Y., Murphy B. R. J. Immunol. 2001;167:3910–3918. doi: 10.4049/jimmunol.167.7.3910. [DOI] [PubMed] [Google Scholar]
- 11.Bevan M. J. Nat. Rev. Immunol. 2004;4:595–602. doi: 10.1038/nri1413. [DOI] [PubMed] [Google Scholar]
- 12.Riberdy J. M., Flynn K. J., Stech J., Webster R. G., Altman J. D., Doherty P. C. J. Virol. 1999;73:1453–1459. doi: 10.1128/jvi.73.2.1453-1459.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walker J. A., Sakaguchi T., Matsuda Y., Yoshida T., Kawaoka Y. Virology. 1992;190:278–287. doi: 10.1016/0042-6822(92)91214-f. [DOI] [PubMed] [Google Scholar]
- 14.Cho Y., Basta S., Chen W., Bennink J. R., Yewdell J. W. J. Virol. 2003;77:4679–4684. doi: 10.1128/JVI.77.8.4679-4684.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mozdzanowska K., Furchner M., Washko G., Mozdzanowski J., Gerhard W. J. Virol. 1997;71:4347–4355. doi: 10.1128/jvi.71.6.4347-4355.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Topham D. J., Doherty P. C. J. Virol. 1998;72:882–885. doi: 10.1128/jvi.72.1.882-885.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hughey P. G., Compans R. W., Zebedee S. L., Lamb R. A. J. Virol. 1992;66:5542–5552. doi: 10.1128/jvi.66.9.5542-5552.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marshall D. R., Turner S. J., Belz G. T., Wingo S., Andreansky S., Sangster M. Y., Riberdy J. M., Liu T., Tan M., Doherty P. C. Proc. Natl. Acad. Sci. USA. 2001;98:6313–6318. doi: 10.1073/pnas.101132698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen W., Calvo P. A., Malide D., Gibbs J., Schubert U., Bacik I., Basta S., O’Neill R., Schickli J., Palese P., et al. Nat. Med. 2001;7:1306–1312. doi: 10.1038/nm1201-1306. [DOI] [PubMed] [Google Scholar]
- 20.Legge K. L., Braciale T. J. Immunity. 2003;18:265–277. doi: 10.1016/s1074-7613(03)00023-2. [DOI] [PubMed] [Google Scholar]
- 21.Arnaout R. A., Nowak M. A. J. Theor. Biol. 2000;204:431–441. doi: 10.1006/jtbi.2000.2027. [DOI] [PubMed] [Google Scholar]
- 22.Seiler P., Brundler M. A., Zimmermann C., Weibel D., Bruns M., Hengartner H., Zinkernagel R. M. J. Exp. Med. 1998;187:649–654. doi: 10.1084/jem.187.4.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Battegay M., Seiler P., Hunziker L., Wolf K., Zinkernagel R. M. J. Infect. Dis. 2001;183:1425–1427. doi: 10.1086/319871. [DOI] [PubMed] [Google Scholar]
- 24.Doherty P. C., Kaufmann S. H. Curr. Opin. Immunol. 1994;6:515–517. doi: 10.1016/0952-7915(94)90134-1. [DOI] [PubMed] [Google Scholar]
- 25.Jackson R. J., Ramsay A. J., Christensen C. D., Beaton S., Hall D. F., Ramshaw I. A. J. Virol. 2001;75:1205–1210. doi: 10.1128/JVI.75.3.1205-1210.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoffmann E., Krauss S., Perez D., Webby R., Webster R. G. Vaccine. 2002;20:3165–3170. doi: 10.1016/s0264-410x(02)00268-2. [DOI] [PubMed] [Google Scholar]
- 27.Webby R. J., Andreansky S., Stambas J., Rehg J. E., Webster R. G., Doherty P. C., Turner S. J. Proc. Natl. Acad. Sci. USA. 2003;100:7235–7240. doi: 10.1073/pnas.1232449100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Andreansky S. S., Stambas J., Thomas P. G., Xie W., Webby R. J., Doherty P. C. J. Virol. 2005;79:4329–4339. doi: 10.1128/JVI.79.7.4329-4339.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hoffmann E., Lipatov A. S., Webby R. J., Govorkova E. A., Webster R. G. Proc. Natl. Acad. Sci. USA. 2005;102:12915–12920. doi: 10.1073/pnas.0506416102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Allan W., Tabi Z., Cleary A., Doherty P. C. J. Immunol. 1990;144:3980–3986. [PubMed] [Google Scholar]