Abstract
This paper reviews the prevention of suicide according to programme evaluation, risk and protective factors, type of intervention, level of intervention and the interface between clinical and public health levels. From nearly a century of experience, a few but important lessons have been learned: since suicide is affected by sociocultural factors, there is no safe indication that what has worked somewhere will work elsewhere; in order to acquire any public health importance, suicide prevention programmes must clearly spell out their objectives and targets; isolated actions have a much lesser probability of yielding significant population outcome results than more articulated approaches that integrate public health measures and individual care with appropriate follow-up and social support.
Keywords: Suicide, prevention, risk factors, protective factors, public health, clinical setting
In 1942, the French existentialist philosopher Albert Camus wrote: "There is only one truly serious philosophical problem: suicide" (1). If this is so, why are psychiatrists interested in this philosophical problem still more than 60 years later? Well, suicides are deaths and psychiatry – as part of medicine – has a serious interest in death, as well as in what is behind it and its prevention or postponement. And if it happens that behind suicide there is a lot of mental disorders and suffering – as it seems indeed to be the case (2, 3) – then the prevention and the appropriate management of those mental disorders would ultimately represent a form of prevention of suicide.
From a historical perspective, suicide – or self-killing, as it was referred to in most European languages before the 17th century (4) – has for many centuries caught the attention of theologians, jurists, philosophers, demographers, sociologists and, more recently, of psychologists, anthropologists, epidemiologists, writers, artists, historians, linguists and a long etc. Medicine started to be more systematically interested in suicide in the 18th century and, more frequently than not, through psychiatrists and in connection with melancholia.
From the 18th century on, the connection between suicide and mental disorders (or insanity, to use the epoch's term) was firmly established in the minds of most updated psychiatrists, to the extent that any death to which a natural cause could not be ascertained was ascribed to madness (5). In 1801, Pinel stated that there was a link between internal organs lesions leading towards a "painful feeling of being" and suicide. A few years later, in 1838, Esquirol wrote that "all those who commit suicide are insane", and in 1845 Bourdin categorically affirmed that suicide "is always a disease and always an act of mental insanity".
Since then, the polarity between those who see suicide as a consequence of a mental disorder (be it caused by biological/genetic or by psychological factors) and those who attribute it to other causes (social, economic, existential, etc.) has, to a large extent, taken precedence over other considerations; even the relevant legislation promulgated during the 20th century reflects this polarity.
This had the clear consequence of grounding suicide, in the health domain, somewhere between public health and psychiatry (6). It is from this double perspective that the prevention of suicide will be overviewed heretofore, according to programme evaluation, risk and protective factors, type of intervention, level of intervention and the interface between clinical and public health levels.
SUICIDE, SUICIDE ATTEMPTS, SUICIDAL BEHAVIOURS
In 1964 Stengel (7), reflecting a common clinical perception, proposed that suicide and suicide attempts reflected two distinct populations. At the root of this distinction was the intention to die (present in the former and absent in the latter), but there were also demographic factors (predominantly elderly males committing suicide and young females attempting it) and epidemiological elements (predominance of psychotic disorder among those who died from suicide and of personality and adjustment disorders among those who attempted it); finally the means employed also contributed to differentiate between these two populations: more lethal means were employed by the former group and less lethal ones by the latter.
Probably due to the fact that the outcome of completed suicide is much more obvious (and severe) than that of suicide attempts, the literature on the former is much more abundant. Also, information (which depends on recording systems and indicators) has been more commonly available for suicide than for suicide attempts. For many countries, for instance, there are extensive time series of data about mortality related to suicide, whereas similar information on suicide attempts is badly missing.
Nevertheless, with recent changes in demography, in social structure and mores and – perhaps more importantly – with the greater availability of more lethal means employed in suicide attempts, the previous clear demarcation lines between suicide and suicide attempt "populations" are getting more and more blurred. This brought in the need to find an umbrella term that would encompass both. Under the influence of North-American psychology, the term now commonly used is suicidal behaviours, and this term will be adopted in the present paper.
PREVENTIVE EFFORTS
Documented systematic suicide prevention efforts are almost a century old (8). Suicide prevention programmes were initiated in both New York (National Save-A-Life League) and London (Suicide Prevention Department of the Salvation Army) in 1906, in Vienna (Suicide Prevention Agency) in 1948, and in Berlin (Suicide Prevention Service) in 1956. Whereas these initiatives remained basically local, the one launched in London in 1953 by the Samaritans soon spread out to numerous countries, using the same principle of "befriending". Today, there are countless numbers of suicide prevention services, as well as "crisis centres" aiming at preventing suicide.
With almost a century of preventive efforts, there should be enough data to evaluate their efficacy. Actually, numerous papers have been published on this, with sometimes contradictory, if not puzzling, results, probably owing to the only partial control of variables involved in the suicidal process. Should any one of these several efforts have demonstrated an unquestionable and universal superiority over others, in all probability it would have already been widely adopted. In reality, what we find is proponents of a variety of preventive programmes and theories trying – without great success – to convince others of the superiority of their own.
A careful review of the evidence of effectiveness of suicide prevention interventions published by Gunnel and Frankel in 1994 (9) examined the medical literature in English language from 1975 on. Out of 19 studies identified, only two were randomised controlled studies (10, 11); the majority of the remaining relied on experts' or expert committees' opinion or clinical experience. When they analysed results of studies combined by setting and intervention, and by exposure to intervention, sadly enough, the highest percentage of reduction in suicide rates observed was 4%.
With a few remarkable exceptions, most evaluative research in suicidology clearly reflects the ideological and etiological views of its authors and addresses the factors (i.e. social, economic, genetic, psychopathological, etc.) believed by them to be relevant in the suicidal process and ignores all others. As a result, a positive and conclusive outcome observed somewhere quite frequently fails to be reproduced elsewhere, where non-controlled variables are at variance (even though usually only the "positive" results are known, due to the fact that "negative" results tend not to be welcome by scientific journals).
In many instances, the lack of precision of the programmes in both objectives and indicators makes true assessment a difficult task. Objectives of prevention programmes can range from a modification of the underlying psychopathological process (e.g. suicidal ideation) to a reduction of morbidity (e.g. suicide attempts) up to a reduction of mortality due to suicide. Ideally, efficacy indicators should be, correspondingly, process or outcome indicators. However, many programmes aiming at modifying psychopathology or morbidity (admittedly or not) are evaluated against changes in mortality rates, whereas some programmes aiming at a reduction of suicide mortality present their results as an improvement in psychopathology or morbidity (or in collateral indicators, such as social integration); this is particularly true when the outcome does not correspond to what was expected and stated at the beginning of the programme.
So far, probably the only large scale, national suicide prevention programme that has been fully implemented and evaluated is the Finnish Suicide Prevention Project (1986-1996). Its aim was "to reduce the suicide rate by 20% by 1995, compared to the situation at the beginning of the project". The evaluation conducted in 1996 indicated a reduction of 8.7% between 1987 and 1996 (with a reduction of 17.5% between the peak years of 1990 and 1996) (12).
RISK AND PROTECTIVE FACTORS
A great amount of research in suicidology revolves around risk – and, to a lesser degree, protective – factors. At any rate, empirical evidence on risk factors for suicide is by far more abundant than that on protective factors, probably due to the fact that their measurement is more straightforward; in other words, there are more studies on the association of suicide with risk factors (irrespective of whether these are actually modifiable or amenable to controlled interventions) than with protective factors (which remain mostly at a rather theoretical level).
The literature on risk factors for suicide and suicidal behaviours is quite vast (albeit not always as critical as one might wish); interested readers are suggested the following critical reviews: Goldney (13), Beautrais (14), Wasserman (15) and Hosman et al (16). Forster and Wu (17) have also proposed an interesting typology of potentially modifiable and non-modifiable risk factors (Table 1). Most studies on risk factors are retrospective, commonly using a single, discrete variable identified close in time to the suicidal event, whereas protective factors remain largely at a theoretical level of discussion, probably owing to the interconnectedness of most protective factors with other variables and their long time span, which render well-controlled studies a quite complex task. Durlak and Wells (18) have reviewed some of these difficulties and suggested ways to improve research related to this issue.
Table 1.
Major risk factors for suicide (adapted and modified from 17)
| "Fixed" factors | Potentially modifiable factors |
|---|---|
| Gender | Access to means |
| Age | Mental disorders |
| Ethnicity | Medical illnesses |
| Sexual orientation | Social isolation |
| Previous attempts | Marital status |
| Employment status | |
| Anxiety | |
| Hopelessness | |
| Life satisfaction |
Whereas risk/protective factors remain one of the most exciting areas of research in suicidology, their translation into uncontroversial and efficient suicide prevention programmes still is in great need of both demonstration and evidence. One of the main obstacles to this translation is the not always considered distinction between "fixed" and "potentially modifiable" risk factors.
Probably the best way of estimating the contribution of specific risk factors is to calculate what is known as population attributable risk (PAR). Briefly, in this case, PAR gives an indication of the percentage reduction of mortality rates if a given factor, supposed to be causally related to suicide, was eliminated.
PAR can serve two purposes: on the one hand, in relation to "fixed" factors, it indicates groups and individuals that, due to an increased, albeit unmodifiable risk, will benefit from a close follow-up; on the other hand, for modifiable factors, it clearly indicates the type of intervention needed, both at individual and population level. Examples of the estimation of PAR have indicated that a reduction in suicide rates of between 9% and 29% could be expected if individuals with family history of suicide (19) and with substance use disorders were targeted. There is an urgent need of the consideration of PAR when designing and implementing suicide prevention programmes.
TYPES OF INTERVENTION
A thorough discussion of the comparative effectiveness of types of intervention is beyond the scope of this paper. Broadly speaking, major interventions for the prevention of suicide can be grouped under the following headings.
Reduction of access to methods and means of suicide - An overview of the evidence indicates that reduction of access to methods (e.g. medication, pesticides, car exhausts, firearms) is perhaps the intervention with the strongest impact at the population level (20).
Treatment of people with mental disorders - It is remarkable that the introduction, by the middle of the 20th century, of effective medication for the control of major mental disorders associated with suicide (e.g., depression and schizophrenia) has brought no significant reduction in national suicide rates in those countries where the medication was widely used. The recent introduction of new antidepressant medication has led to a controversial evidence concerning its impact on suicide rates (21). However, the evidence is far better when examined for specific diseases (e.g. major depression (22) and schizophrenia (23)) or treatment approaches (e.g. the use of lithium in mood disorders (24)). Probably a close follow-up of people who previously have attempted suicide would also fall under this heading (25).
Improvement of media portrayal of suicide - Although there is a consistent evidence about the improvement of media portrayal of suicide (26), the impact of this intervention at the national level remains to be convincingly demonstrated.
Training of primary health care personnel - The evidence of the efficacy of training primary health care personnel as an approach to suicide prevention, although much touted, remains based on a single remarkable but limited – both geographically and in terms of gender differences – example, developed on the Island of Gotland (27). Larger ongoing studies (e.g. in Hungary and UK (28)) should shed additional light on this issue.
School-based programmes - The same applies to school-based programmes. The ever-quoted example of Dade County (29) (nevertheless more related to suicide attempts than to completed suicides) stands unfortunately in isolation. A full evaluation of other similar ongoing programmes (e.g. in Stockholm) will hopefully contribute a much needed additional evidence. Environmental and epidemiological specificities of school populations should be carefully considered in planning and implementing suicidal behaviour programmes with them (30).
Availability of hot lines and crisis centres - In spite of their popularity and attractiveness, so far there is no conclusive evidence on the effectiveness of suicide prevention hot lines and crise centres (31, 32). Admittedly, it seems that their efficacy to help people in crises (not necessarily suicidal) is far greater than their impact on suicide rates.
LEVELS OF INTERVENTION
For an overview of the impact of suicide prevention programmes at the public health level, the conceptual model developed by Mrazek and Haggerty (33) seems particularly useful. Briefly, it categorises preventive interventions, according to their coverage, into universal, selective or indicated interventions. Table 2 shows some examples of these interventions, both general and specific to suicide prevention.
Table 2.
Examples of effective preventive interventions for suicidal behaviours, by coverage
| Intervention | Prevention of mental disorders | Prevention of suicide |
|---|---|---|
| Universal | Adequate pre-natal care | Limitation of access to toxic substances |
| Selective | Psychological support to people in crisis situations or with physical diseases | Treatment of people with mental disorders (including substance use disorders) |
| Indicated | Programmes for parents of pre-school children with marked aggression and rebelliousness | Close therapeutic follow-up of people with bipolar disorders or with recurrent psychotic episodes |
| Close (psychosocial) follow-up of previous attempters | ||
A closer look at the numerous actual or proposed suicide prevention approaches and programmes, some of which are mentioned above, would indicate that, according to Mrazek and Haggerty's model, we have more convincing evidence concerning universal and indicated interventions than selective ones. This is not too different from what happens in the overall mental health field (34).
THE INTEGRATION OF PUBLIC HEALTH AND CLINICAL ACTIONS
Overall, in relation to the efficiency of suicide prevention, suicidologists and clinicians are much more optimistic than public health officers. And probably all are right, but not always one finds clinicians, suicidologists and public health officers working hand in hand (35). What is badly needed is an integrated approach bringing closer their specific objectives and outcome measures, allowing for the differences in their respective methods and techniques. Also, this integrated approach should take into account both risk and protective factors, ranging from universal through selective up to indicated interventions. Some of these find an easier and more appropriate implementation at the public health, collective level, while others would be best implemented in clinical settings, at an individual level. Figure 1 graphically depicts this integrated conceptual model.
Figure 1.
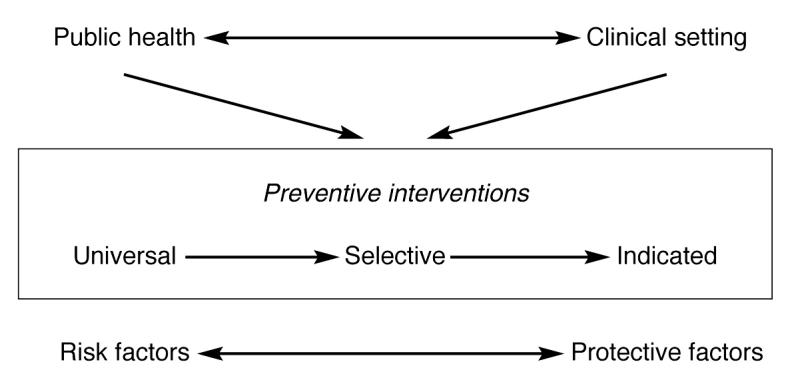
Suicidal behaviours prevention: integration of public health and clinical approaches
CONCLUSIONS
From nearly a century of experiences in suicide prevention, a few but important lessons have already been learned:
Since suicide is intrinsically affected by sociocultural factors, there is no safe indication that what has worked somewhere will work elsewhere. It has been demonstrated that suicide prevention programmes have worked some times, somewhere. However, a "direct transplantation" of policies and programmes, without full consideration of those factors, will probably yield frustrating results.
In order to acquire any public health importance, suicide prevention programmes must clearly spell out their objectives and targets (i.e., specific results in a given timeframe). Without this, they cannot go beyond well intentioned initiatives, with many beneficial collateral outcomes, but perhaps without a real reduction in rates of suicidal behaviours.
Isolated actions have a much lesser probability of yielding significant population outcome results than more sophisticated and articulated approaches that integrate public health measures and individual care with appropriate follow-up and social support.
In terms of the prevention of suicidal behaviours, we have already learned a lot about what to do, and to whom and with whom, where and when. We have today a much clearer idea about the specific role of political/health authorities, health personnel, mental health staff, psychiatrists, journalists, survivors of suicide and the society at large. However, there is still a great deal to improve on what we know about what to do, and to whom and with whom, where and when. Many lessons have been learned but we still have a few terms ahead of us before a full graduation is reached.
I would like to conclude quoting once again Camus and – as a doctor, a psychiatrist, a public health officer and a being-in-the-world – agree with him that "Through consciousness only, I transform in rule of life what was an invitation to death, and I refuse suicide". Our current limitations should not abate us, rather they should be a strong stimulant for the improvement of the efficiency of our current strategies and methodologies for suicide prevention, both at clinical and public health levels.
Acknowledgements
The author wishes to express his deep gratitude to Dr. B. Saraceno, Dr. A. Fleischmann and Ms. R. Seminario for their comments on earlier drafts of this paper.
References
- 1.Camus A. Le mythe de Sisyphe. Paris: Gallimard; 1942. [Google Scholar]
- 2.Bertolote JM, Fleischmann A. Suicide and psychiatric diagnosis: a worldwide perspective. World Psychiatry. 2002;1:181–185. [PMC free article] [PubMed] [Google Scholar]
- 3.Phillips MR. Suicide rates in China. Lancet. 2002;359:2274. [Google Scholar]
- 4.Minois G. L'histoire du suicide. Paris: Fayard; 1995. [Google Scholar]
- 5.MacDonald M, Murphy T. Sleepless souls: suicide in early modern England. Oxford: Clarendon Press; 1990. [Google Scholar]
- 6.De Leo D, Bertolote J, Lester D. Self-directed violence. In: Krug EG, Dahlberg LL, Mercy JA, et al., editors. World report on health and violence. Geneva: World Health Organization; 2002. pp. 183–212. [Google Scholar]
- 7.Stengel E. Suicide and attempted suicide. Baltimore: Penguin Books; 1964. [Google Scholar]
- 8.Shneidman ES. Suicide prevention. In: Corsini R, editor. Encyclopedia of psychology. Vol. 3. New York: Wiley; 1984. p. 383. [Google Scholar]
- 9.Gunnel D, Frankel S. Prevention of suicide: aspirations and evidence. Br Med J. 1994;308:1227–1233. doi: 10.1136/bmj.308.6938.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Litman RE. Anti-suicide program conducts controlled study. Evaluation. 1976;3:36–37. [PubMed] [Google Scholar]
- 11.Motto JA. Suicide prevention for high risk persons who refuse treatment. Suicide Life Threat Behav. 1976;6:223–230. [PubMed] [Google Scholar]
- 12.Upanne M, Hakanen J, Rautava M. Can suicide be prevented? The Suicide Project in Finland 1992-1996: goals, implementation and evaluation. Helsinki: Stakes; 1999. [Google Scholar]
- 13.Goldney RD. Variation in suicide rates: the "Tipping Point". Crisis. 1998;19:136–138. doi: 10.1027/0227-5910.19.3.136. [DOI] [PubMed] [Google Scholar]
- 14.Beautrais A. Risk factors for suicide and attempted suicide among young people. Aust N Zeal J Psychiatry. 2000;34:420–436. doi: 10.1080/j.1440-1614.2000.00691.x. [DOI] [PubMed] [Google Scholar]
- 15.Wasserman D. Suicide - an unnecessary death. London: Dunitz; 2001. [Google Scholar]
- 16.Hosman C, Wasserman D, Bertolote J. Prevention of suicide. In: Hosman C, Jane Llopi E, Saxena S, editors. Evidence-based prevention of mental disorders. Oxford/Geneva: Oxford University Press/World Health Organization; (in press) [Google Scholar]
- 17.Forster P, Wu L. Assessment and treatment of the suicidal patient in an emergency setting. In: Allen MH, editor. Emergency psychiatry. Washington: American Psychiatric Publishing; 2002. pp. 75–113. [Google Scholar]
- 18.Durlak JA, Wells AM. Primary prevention mental health programs: the future is exciting. Am J Commun Psychol. 1997;25:233–243. doi: 10.1023/a:1024674631189. [DOI] [PubMed] [Google Scholar]
- 19.Qin P, Agerbo E, Mortensen PB. Suicide risk in relation to socioeconomic, demographic, psychiatric, and family factors: a national register-based study of all suicides in Denmark, 1981-1997. Am J Psychiatry. 2003;160:765–772. doi: 10.1176/appi.ajp.160.4.765. [DOI] [PubMed] [Google Scholar]
- 20.Lester D. Preventing suicide by restricting access to methods for suicide. Arch Suicide Res. 1998;4:7–24. [Google Scholar]
- 21.World Health Organization. The controversial evidence of the population impact on suicide rates of new antidepressants. Geneva: World Health Organization; (in press) [Google Scholar]
- 22.Angst J, Angst F, Stassen HH. Suicide risk in patients with major depressive disorder. J Clin Psychiatry. 1999;60(Suppl. 2):57–62. [PubMed] [Google Scholar]
- 23.Meltzer HY. Treatment of suicidality in schizophrenia. Ann NY Acad Sci. 2001;932:44–58. doi: 10.1111/j.1749-6632.2001.tb05797.x. [DOI] [PubMed] [Google Scholar]
- 24.Coppen A. Lithium in unipolar depression and the prevention of suicide. J Clin Psychiatry. 2000;61(Suppl. 9):52–56. [PubMed] [Google Scholar]
- 25.Retterstöl N, Mehlun N. Attempted suicide as a risk factor for suicide: treatment and follow-up. In: Wasserman D, editor. Suicide - an unnecessary death. London: Dunitz; 2001. pp. 125–131. [Google Scholar]
- 26.Schmidtke A, Schaller S. The role of mass media in suicide prevention. In: Hawton K, van Heeringen K, editors. The international handbook of suicide and attempted suicide. New York: Wiley; 2000. pp. 675–697. [Google Scholar]
- 27.Rutz W, von Knorring L, Wallinder J. Frequency of suicide on Gotland after systematic postgraduate education of general practitioners. Acta Psychiatr Scand. 1989;80:151–154. doi: 10.1111/j.1600-0447.1989.tb01318.x. [DOI] [PubMed] [Google Scholar]
- 28.Thompson C, Kinmoth AL, Stevens L, et al. Effects of a clinical-practice guideline and practice-based education on detection and outcome of depression in primary care: Hampshire Depression Project randomised controlled trial. Lancet. 2000;355:185–191. doi: 10.1016/s0140-6736(99)03171-2. [DOI] [PubMed] [Google Scholar]
- 29.Zenere FJ, Lazarus PJ. The decline of youth suicidal behaviour in an urban, multicultural public school system following the introduction of a suicide prevention and intervention programme. Suicide Life Threat Behav. 1997;27:387–402. [PubMed] [Google Scholar]
- 30.Silverman MM, Meyer PM, Sloane F, et al. The big ten student suicide study: a 10-year study of suicides on Midwestern university campuses. Suicide Life Threat Behav. 1997;27:285–303. [PubMed] [Google Scholar]
- 31.Diekstra RF, Kerkhof AJ. The prevention of suicidal behaviour: a review of effectiveness. In: Maes S, Leventhal H, Johnston M, editors. International review of health psychology. Vol. 3. Chichester: Wiley; 1994. pp. 145–165. [Google Scholar]
- 32.Lester D. The effectiveness of suicide prevention centers: a review. Suicide Life Threat Behav. 1997;27:304–310. [PubMed] [Google Scholar]
- 33.Mrazek PJ, Haggerty RJ. Reducing risks from mental disorders: frontiers for preventive intervention research. Washington: National Academy Press; 1994. [PubMed] [Google Scholar]
- 34.Hosman C, Jane Llopi E, Saxena S, editors. Evidence-based prevention of mental disorders. Oxford/Geneva: Oxford University Press/World Health Organization; (in press) [Google Scholar]
- 35.Leenaars A. Controlling the environment to prevent suicide. In: Wasserman D, editor. Suicide - an unnecessary death. London: Dunitz; 2001. pp. 259–263. [Google Scholar]


