Abstract
This study aimed to develop a casemix classification of characteristics of New Zealand mental health services users. Over a six month period, patient information, staff time and service costs were collected from 8 district health boards. This information was analysed seeking the classification of service user characteristics which best predicted the cost drivers of the services provided. A classification emerged which explained more than two thirds of the variance in service user costs. It can be used to inform service management and funding, but it is premature to have it determine funding.
Keywords: Casemix classification, mental health services users, service management
Over recent decades, recognition that variations in the characteristics of patients would be reflected in variations in service costs has led to the development of casemix classifications in medicine. The purpose of these is to classify episodes of care based on those factors which best predict the need for, and the cost of, care. Each class should contain episodes with similar patterns of resource consumption and which are clinically similar. This has been particularly represented by the diagnosis related groups (DRG) casemix classification, which currently forms the basis for the purchasing and cost weighting of personal health services by several governments worldwide.
The mental health sector has lagged behind the general health sector in casemix development (1). A number of earlier attempts were based solely on diagnosis: they performed poorly in predicting resource use, had an unwieldy number of classes and/or were limited to inpatient settings (2-9). Several studies identified the following patient factors as predictive of resource use: diagnosis, severity of symptoms, risk of harm to self or others, level of functioning and social support, co-morbidity, sociodemographic characteristics and stage of illness (10-27).
A large study in Australia (28) found similar results. A number of patient and provider characteristics contributed to a casemix classification model that allowed explanation of two thirds of the variations in service cost. This was the major impetus to developing a New Zealand version of that study, the Mental Health Classification and Outcomes Study (CAOS) (29).
After two years of preliminary planning for the project, eight district health boards (DHBs) contributed data over a six month period in 2003, between them covering the whole range of DHB provided psychiatric services.
METHODS
Service use was conceptualized as made up of "episodes of care", which for the purposes of this study were defined as a period of contact between a consumer and a "provider" that occurred in one treatment setting. It was thus a managerial, rather than a clinical, concept and could be up to a maximum of 91 days. It did not necessarily coincide with an episode of illness, or with the patient management plans.
The following types of data were to be entered into a regression analysis approach: patient/consumer characteristics as currently provided by the DHBs to the Mental Health Information National Collection system, plus ratings on outcome scales such as the Health of the Nation Outcome Scales (HoNOS) (30); episode of care cost data provided by the DHBs; and staff time.
For this regression exercise, the episodes of care forming the units for analysis were created as shown in Figure 1.
Figure 1.
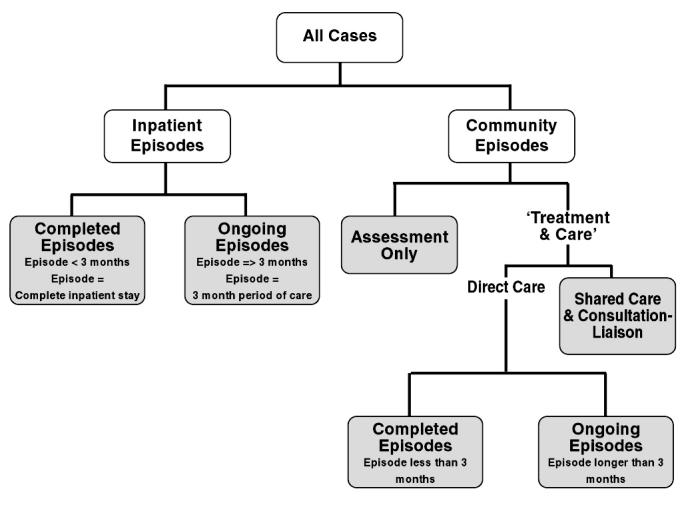
Episode of care model adopted in the study (shaded boxes represent the episode type)
All episode information was collected by the clinical staff members primarily responsible for the patient's care. The additional information collected included ratings on the HoNOS (including the HoNOS 65+ and HoNOSCA for older people and children respectively), the short version of the Life Skills Profile (LSP-16) (31), the Resource Utilisation Groups Activities of Daily Living Scale (RUG-ADL) (32) and the Children's Global Assessment Scale (CGAS) (33). The community based service staff recorded their team code, date of contact, service type, contact duration, staff label category and the service setting. A resource allocation tool (RAT) was developed which recorded the allocation of inpatient nursing hours/patient. A composite measure reflecting the goal of care for the current episode (Focus of Care, FOC) (28) was added.
The national project team and the New Zealand Health Information Service established a process to match and encrypt all activity data and consolidate it into one file to avoid placing this additional burden on participating sites. Four design rules were adopted for use during the class finding analysis: a) consumer related cost drivers (the cost drivers used in the design of the classification should, wherever possible, be related to consumer characteristics and not to the type, or extent, of services utilised); b) variance reduction (the selection of the cost drivers should result in minimum variation within each class and maximum differences between classes); c) sensible clinical groups (the final classes should be clinically sensible); d) ease of collection (the variables used in the classification should be capable of routine collection, coding and data entry). The dependent or response variable was the cost of an episode of care. The independent variables were those characteristics of consumers that can be measured and that can be demonstrated to be predictive of cost.
PC-Group was used for the class finding. Independent variables were selected from the variety of demographic and clinical measurements recorded for consumers. The 'best' tree was selected as that which accounted for the largest proportion of variation in the cost of care. As this tree was not necessarily clinically the most sensible, PC-Group was also used to improve the clinical logic of the classification. For example, adult inpatient episodes were separated from child and youth episodes because this separation makes clinical sense.
The ultimate aim of the analysis was to form distinct groups within the data, such that consumers within each group were similar to each other, but different from consumers in the other groups. Similarity and dissimilarity between consumers was measured by the cost of care. Independent variables were compared to find the one which could best split the data into two homogeneous groups that were as different from one another as possible. Successive binary splits were performed on the data until there were no significant improvements to be made. At that time, the best classification solution was reached. In parallel with this class-finding analysis, a number of multilevel models were fitted to the data, which confirmed the choice of variables to be included in the class-finding.
RESULTS
Profile of consumers and episodes
In total, 19,239 episodes of care were captured over the six month study period. These were provided to a total of 12,576 individual consumers. 98% of those consumers received their care only at one DHB. Overall, the male to female ratio was 53:47. 62% of the consumers identified themselves as New Zealand European/Pakeha, 20% as Maori and approximately 5% as Pacific Islanders. On the index of deprivation profile, the consumers were weighted towards the seventh to tenth deciles, this being particularly the case for males.
55% of consumers had only one episode of care during this study period, with a further 40% having two episodes. Approximately 10% of all episodes were inpatient based. The population diagnostic distributions are shown in the Tables 1 and 2.
Table 1.
Episodes of care by diagnosis – Adults
| Inpatient | Shared community care | Direct community care | All | |||||
|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | No. | % | |
| Schizophrenia, paranoia and acute psychotic disorders | 1328 | 48.2 | 222 | 24.7 | 3468 | 32.1 | 5018 | 34.7 |
| Mood disorders | 783 | 28.4 | 248 | 27.6 | 3129 | 28.9 | 4160 | 28.8 |
| Personality disorders | 124 | 4.5 | 27 | 3.0 | 344 | 3.2 | 495 | 3.4 |
| Anxiety disorders | 29 | 1.1 | 25 | 2.8 | 430 | 4.0 | 484 | 3.3 |
| Organic disorders | 106 | 3.8 | 33 | 3.7 | 299 | 2.8 | 438 | 3.0 |
| Stress and adjustment disorders | 53 | 1.9 | 25 | 2.8 | 360 | 3.3 | 438 | 3.0 |
| Substance abuse disorders | 75 | 2.7 | 11 | 1.2 | 182 | 1.7 | 268 | 1.9 |
| Eating disorders | 9 | 0.3 | 35 | 3.9 | 82 | 0.8 | 126 | 0.9 |
| Obsessive-compulsive disorders | 11 | 0.4 | 2 | 0.2 | 59 | 0.5 | 72 | 0.5 |
| Mental retardation | 23 | 0.8 | 7 | 0.8 | 20 | 0.2 | 50 | 0.3 |
| Behavioural syndromes associated with physiological disturbances | 3 | 0.1 | 40 | 0.4 | 43 | 0.3 | ||
| Disorders of psychological development | 6 | 0.2 | 1 | 0.1 | 26 | 0.2 | 33 | 0.2 |
| Disorders of childhood and adolescence | 1 | 1 | 0.1 | 25 | 0.2 | 27 | 0.2 | |
| Somatoform disorders | 3 | 0.1 | 3 | 0.3 | 13 | 0.1 | 19 | 0.1 |
| Sexual disorders | 4 | 0.1 | 10 | 0.1 | 14 | 0.1 | ||
| Other/missing | 197 | 7.2 | 257 | 28.7 | 2328 | 21.5 | 2782 | 19.2 |
| Grand total | 2755 | 100.0 | 897 | 100.0 | 10815 | 100.0 | 14467 | 100.0 |
Table 2.
Episodes of care by diagnosis – Child/Youth
| Inpatient | Shared community care | Direct community care | All | |||||
|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | No. | % | |
| Disorders of childhood and adolescence | 11 | 11.8 | 22 | 23.9 | 983 | 31.0 | 1016 | 30.3 |
| Mood disorders | 23 | 24.7 | 7 | 7.6 | 420 | 13.3 | 450 | 13.4 |
| Stress and adjustment disorders | 12 | 12.9 | 5 | 5.4 | 317 | 10.0 | 334 | 10.0 |
| Anxiety disorders | 1 | 1.1 | 2 | 2.2 | 199 | 6.3 | 202 | 6.0 |
| Disorders of psychological development | 5 | 5.4 | 5 | 5.4 | 125 | 3.9 | 135 | 4.0 |
| Substance abuse disorders | 1 | 1.1 | 104 | 3.3 | 105 | 3.1 | ||
| Schizophrenia, paranoia and acute psychotic disorders | 27 | 29.0 | 2 | 2.2 | 71 | 2.2 | 100 | 3.0 |
| Mental retardation | 1 | 1.1 | 54 | 1.7 | 55 | 1.6 | ||
| Eating disorders | 4 | 4.3 | 2 | 2.2 | 35 | 1.1 | 41 | 1.2 |
| Obsessive-compulsive disorders | 2 | 2.2 | 34 | 1.1 | 36 | 1.1 | ||
| Personality disorders | 2 | 2.2 | 15 | 0.5 | 17 | 0.5 | ||
| Organic disorders | 2 | 2.2 | 2 | 2.2 | 5 | 0.2 | 9 | 0.3 |
| Somatoform disorders | 1 | 1.1 | 7 | 0.2 | 8 | 0.2 | ||
| Behavioural syndromes associated with physiological disturbances | 1 | 1 | ||||||
| Other | 4 | 4.3 | 42 | 45.7 | 797 | 25.2 | 843 | 25.1 |
| Grand total | 93 | 100.0 | 92 | 100.0 | 3167 | 100.0 | 3352 | 100.0 |
Schizophrenia, paranoia and acute psychotic disorders accounted for 50% of Pacific people's episodes, 38% of Maori and only 24% of European episodes. In contrast, mood disorders accounted for 30% of European episodes, but only 16% of Maori and 14% of Pacific Island episodes. Anxiety disorders were uncommonly recorded for Maori and Pacific people (less than 1%) and accounted for 4.5% of European episodes.
There were 2,715 inpatient episodes with valid HoNOS ratings, representing 98.5% of all inpatient episodes. The HoNOS score pattern across the items was broadly similar for the three ethnicity groupings, with the average scores on item 1 (Overactive, aggressive, disruptive or agitated behaviour), item 6 (Problems associated with hallucinations and delusions) and item 9 (Problems with relationships) being the most elevated. There were some differences between the three ethnicity groupings for particular items. These differences will be explored in a separate outcome analysis. There were similar findings on all of the other clinical measures. The FOC findings showed major ethnic differences, with higher levels of 'acuity' in the Maori and Pacific inpatients.
The cost differences between the various types of episodes are shown in Table 3. The key general cost findings are: a) child and adolescent episodes cost more than adult episodes; b) complete (short-term) episodes cost more on a per diem basis than ongoing (longer-term) episodes, but they cost less on an episode basis; c) shared care episodes cost at least as much as direct care episodes on both a per diem and an episode basis; d) child and adolescent inpatient episodes cost more than adult inpatient episodes on both an episode and a per diem basis; e) assessment only community episodes cost significantly less on an episode basis but, on a per diem basis, they are the most costly community treatment days. These findings lay the groundwork for the design of the casemix classification.
Table 3.
Episode cost profile by episode type
| No. of episodes | Mean | Median | Minimum | Maximum | Percentile 25 | Percentile 75 | CV | |
|---|---|---|---|---|---|---|---|---|
| Child inpatient - Ongoing | 26 | $74,772 | $79,543 | $23,869 | $122,916 | $56,775 | $90,715 | 0.29 |
| Adult inpatient - Ongoing | 1094 | $43,545 | $39,821 | $1,764 | $227,596 | $31,160 | $50,062 | 0.44 |
| Child inpatient - Complete | 67 | $25,762 | $17,633 | $1,612 | $77,175 | $9,374 | $37,366 | 0.82 |
| Adult inpatient - Complete | 1661 | $11,757 | $7,635 | $284 | $108,041 | $3,329 | $15,201 | 1.08 |
| Child shared community care - Complete | 10 | $4,209 | $2,332 | $218 | $17,797 | $885 | $5,349 | 1.27 |
| Adult shared community care - Ongoing | 681 | $1,971 | $1,105 | $64 | $40,837 | $600 | $2,332 | 1.47 |
| Child direct community care - Ongoing | 2613 | $1,867 | $1,207 | $56 | $33,490 | $584 | $2,338 | 1.15 |
| Child direct community care - Complete | 554 | $1,744 | $1,192 | $59 | $17,783 | $476 | $2,272 | 1.07 |
| Adult direct community care - Ongoing | 9034 | $1,694 | $1,085 | $37 | $36,517 | $561 | $2,116 | 1.14 |
| Child shared community care - Ongoing | 82 | $1,682 | $853 | $169 | $8,999 | $407 | $2,213 | 1.10 |
| Adult shared community care - Complete | 216 | $1,673 | $1,100 | $71 | $28,510 | $471 | $1,877 | 1.47 |
| Adult direct community care - Complete | 1781 | $1,560 | $1,010 | $46 | $14,328 | $577 | $1,960 | 1.06 |
| Child assessment only | 102 | $459 | $399 | $131 | $1,109 | $262 | $661 | 0.54 |
| Adult assessment only | 1318 | $423 | $366 | $71 | $1,412 | $233 | $549 | 0.58 |
CV – coefficient of variation
Pacific Island episodes had the highest average cost for adult episodes ($9235), followed by Maori ($7032) and then European ($3776). The situation was different for child and youth inpatient episodes, where the 'all other' group has the highest child and youth episode cost, followed by European episodes. There were no cost differences between Maori and Pacific child and youth episodes.
Casemix classification
After removing partial episodes, a total of 16,665 episodes were used for class finding (Table 4).
Table 4.
Final data set used for class finding
| Episode of care type | Adult | Child and youth | Total | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| Inpatient | 2279 | 16.6 | 77 | 2.6 | 2356 | 14.1 |
| Assessment only (community) | 1318 | 9.6 | 102 | 3.5 | 1420 | 8.5 |
| Shared community care | 774 | 5.6 | 77 | 2.6 | 851 | 5.1 |
| Direct community care | 9349 | 68.1 | 2689 | 91.3 | 12038 | 72.2 |
| Total | 13720 | 100.0 | 2945 | 100.0 | 16665 | 100.0 |
Figure 2 shows the final classification developed. It has a total of 42 classes. For adults, particular HoNOS items, Focus of Care ratings, legal status and ethnicity all contributed significantly as predictive variables for costs. Diagnosis did not. For children and youth, diagnosis (inpatients only), age and HoNOSCA items proved to be useful variables.
Figure 2.
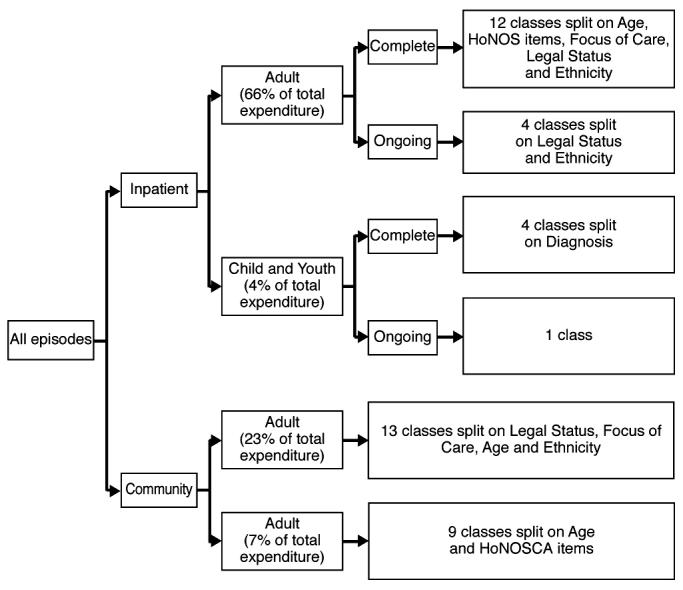
Classification of episodes
The end result is that nine variables were employed in the classification. They fell into three groups: a) a direct service measure, length of stay (used to define complete and ongoing episodes in the inpatient branch); b) five direct consumer measures (age; ethnicity for adults; HoNOS ratings for adult inpatients; diagnosis for child/youth inpatients; HoNOSCA ratings for child/youth); c) measures which are a blend of consumer and service attributes: assessment only (community), legal status (adults) and FOC (adults).
The average case complexity of the three broad ethnicity groupings is shown in Table 5. Pacific people inpatient episodes have an average weight that is 35% above the national average for inpatient episodes, while Maori inpatient episodes have a weight that is 22% above the national average. The European/Other grouping has an inpatient weight that is 14% below the national average. For community episodes, Pacific episodes have an average weight that is 44% above the national average for community episodes, while Maori inpatient episodes have a weight that is 5% above the national average. The European/Other grouping has a community weight that is 4% below the national average.
Table 5.
Average case complexity of the three broad ethnicity groupings
| Ethnicity Grouping | Average case weight - impatient episodes | Average case weight - community episodes | Average case weight - all episodes |
|---|---|---|---|
| Pacific Island | 6.00 | 0.51 | 1.93 |
| Maori | 5.40 | 0.37 | 1.49 |
| European/Other | 3.83 | 0.34 | 0.81 |
| All | 4.44 | 0.36 | 1.00 |
DISCUSSION
The statistical performance of the classification is satisfactory. Although this study is large and the results have statistical strength, two fundamental points need to be borne in mind in discussing it. The first is that this is an essentially descriptive report of current practice reality and cannot be taken to represent best practice. The second is that this is a first ever study of its kind in New Zealand, and can in that sense be thought of as pilot. The amount of data collected, however, makes it very unlikely it will ever be replicated in a similar fashion.
It would have been preferable to use only direct consumer measures instead of including those with significant provider judgement contributions. They are used in the classification when no direct consumer measure could be found that would act as a proxy. In reality, no existing casemix classification consists solely of consumer-related variables. For example, over half the classes in the DRG system are defined on length of stay, the nature of the procedure or the type of intervention. These measures work in the DRG system in the same way that Assessment Only, Legal Status and FOC work in our classification. If the DRG system is the benchmark, the mix of consumer-related and service-related measures in our study is more than acceptable.
Setting an international precedent, this study has resulted in a casemix classification that includes some casemix classes based on ethnicity. The decision to include such classes was carefully considered by all key stakeholders during the design, implementation and analysis phases and makes sense in the New Zealand context. Consistent with clinical expectations, the study found that, after controlling for clinical differences in the mix of cases, there were still statistically significant differences between the three major ethnicity groupings.
In conclusion, the performance of this classification is satisfactory as a first version national classification. In total there are 42 classes, 20 for inpatient episodes and 22 for community episodes. Significant differences in episode costs for adult inpatient episodes are noted when ethnicity is taken into consideration. Diagnosis is not an important variable for adult inpatient episodes, but it is for child and youth inpatient episodes. There are significant differences in the case complexity between DHBs. The classification is not suitable to be used as a funding model, but it is sufficient to inform management and funding decisions. The CAOS dataset offers a rich source of data that DHBs could continue to use to further inform costing and clinical assurance initiatives.
Acknowledgement
This study was funded by the Mental Health Research and Development Strategy of the Ministry of Health and the Health Research Council.
References
- 1.Fetter RB, editor. DRGs: their design and development. Ann Arbor: Health Administration Press; 1991. [Google Scholar]
- 2.Ashcraft MLF, Fries BE, Nerenz DR, et al. A psychiatric patient classification system: an alternative to DRGs. Med Care. 1989;27:543–557. doi: 10.1097/00005650-198905000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Ben-Tovim DI, Elzinga R, Burgess P. Psychiatric and substance abuse disorder diagnoses as predictors of length of hospital stay. Aust Health Rev. 1996;19:20–28. doi: 10.1071/ah960020. [DOI] [PubMed] [Google Scholar]
- 4.Fries BE, Nerenz DR, Ashcraft MLF, et al. A classification system for long-staying psychiatric patients. Med Care. 1990;28:311–323. doi: 10.1097/00005650-199004000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Horgan C, Jencks SF. Research on psychiatric classification and payment systems. Med Care. 1987;25:S22–S36. [PubMed] [Google Scholar]
- 6.Horn SD, Chambers AF, Sharkey PD, et al. Psychiatric severity of illness: a casemix study. Med Care. 1989;27:69–83. doi: 10.1097/00005650-198901000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Morath J, Fleischmann R, Boggs R. A missing consideration: the psychiatric patient classification for scheduling staffing schemes. Perspectives in Psychiatric Care. 1989;25:40–47. doi: 10.1111/j.1744-6163.1989.tb01217.x. [DOI] [PubMed] [Google Scholar]
- 8.Phelan M, McCrone P. Effectiveness of diagnosis related groups in predicting psychiatric resource utilisation in the UK. Psychiatr Serv. 1995;46:547–549. doi: 10.1176/ps.46.6.547. [DOI] [PubMed] [Google Scholar]
- 9.Stoskopf C, Horn SD. The Computerised Psychiatric Severity Index as a predictor of inpatient length of stay for psychoses. Med Care. 1991;29:179–195. doi: 10.1097/00005650-199103000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Mezzich JE. Architecture of clinical information and prediction of service utilisation and cost. Schizophr Bull. 1991;17:469–474. doi: 10.1093/schbul/17.3.469. [DOI] [PubMed] [Google Scholar]
- 11.Mezzich JE, Coffman GA. Factors influencing length of hospital stay. Hosp Commun Psychiatry. 1985;36:1262. doi: 10.1176/ps.36.12.1262. [DOI] [PubMed] [Google Scholar]
- 12.McFarland BH, Faulkner LR, Bloom JD. Predicting involuntary patients' length of stay. Administration and Policy in Mental Health. 1990;17:139–149. [Google Scholar]
- 13.Gordon RE, Jardiolin P, Gordon KK. Predicting length of hospital stay of psychiatric patients. Am J Psychiatry. 1985;142:235–237. doi: 10.1176/ajp.142.2.235. [DOI] [PubMed] [Google Scholar]
- 14.Chang G, Brenner L, Bryant K. Factors predicting inpatient length of stay in a CMHC. Hosp Commun Psychiatry. 1991;42:853–855. doi: 10.1176/ps.42.8.853. [DOI] [PubMed] [Google Scholar]
- 15.Nieminen P, Isohanni M, Winblad I. Length of hospitalisation in an acute patients' therapeutic community ward. Acta Psychiatr Scand. 1994;90:466–472. doi: 10.1111/j.1600-0447.1994.tb01626.x. [DOI] [PubMed] [Google Scholar]
- 16.Havassy BE, Hopkin JT. Factors predicting utilisation of acute psychiatric inpatient services by frequently hospitalised patients. Hosp Commun Psychiatry. 1989;40:820–823. doi: 10.1176/ps.40.8.820. [DOI] [PubMed] [Google Scholar]
- 17.Borchardt CM, Garfinkel BD. Predictors of length of stay of psychiatric adolescent inpatients. J Am Acad Child Adolesc Psychiatry. 1991;30:994–998. doi: 10.1097/00004583-199111000-00019. [DOI] [PubMed] [Google Scholar]
- 18.Caton CLM, Gralnick A. A review of issues surrounding length of psychiatric hospitalisation. Hosp Commun Psychiatry. 1987;38:858–863. doi: 10.1176/ps.38.8.858. [DOI] [PubMed] [Google Scholar]
- 19.Taube CA, Goldman HH, Burns BJ, et al. High users of outpatient mental health services. (I) Definition and characteristics. Am J Psychiatry. 1988;145:19–23. doi: 10.1176/ajp.145.1.19. [DOI] [PubMed] [Google Scholar]
- 20.Knapp M, Beecham J, Fenho A, et al. Community mental health care for former hospital inpatients: predicting costs from needs and diagnoses. Br J Psychiatry. 1995;166:10–18. [PubMed] [Google Scholar]
- 21.Swett C, Noones J. Factors associated with premature termination from outpatient treatment. Hosp Commun Psychiatry. 1989;40:947–951. doi: 10.1176/ps.40.9.947. [DOI] [PubMed] [Google Scholar]
- 22.Kirshner LA. Length of stay of psychiatric patients: a critical review and discussion. J Nerv Ment Dis. 1982;170:27–33. doi: 10.1097/00005053-198201000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Cuffel B. Disruptive behaviour and the determinants of costs in the public mental health system. Psychiatr Serv. 1997;48:1562–1566. doi: 10.1176/ps.48.12.1562. [DOI] [PubMed] [Google Scholar]
- 24.Sylvester CT, Bean GJ. Predicting community tenure after psychiatric hospitalisation. Commun Ment Health J. 1989;25:109–120. doi: 10.1007/BF00755383. [DOI] [PubMed] [Google Scholar]
- 25.Allen JG, Coyne L, Lyle J, et al. Assessing need for extended psychiatric hospitalisation. Compr Psychiatry. 1992;33:346–386. doi: 10.1016/0010-440x(92)90043-p. [DOI] [PubMed] [Google Scholar]
- 26.Huxley P, Braude W. Acute admission to psychiatric care: factors related to length of stay. J Ment Health. 1994;3:377–386. [Google Scholar]
- 27.Ghuman JS, Jayprakash S, Saidel DH, et al. Variables predictive of the need for placement in a long-term structured setting for adolescents. Psychiatric Hospital. 1990;20:31–34. [PubMed] [Google Scholar]
- 28.Burgess P, Pirkis J, Buckingham W, et al. Developing a casemix classification for specialist mental health services. Casemix. 1999;4 [Google Scholar]
- 29.Gaines P, Bower A, Buckingham W, et al. New Zealand Mental Health Classification and Outcomes Study: final report. Auckland: Health Research Council of New Zealand; 2003. [Google Scholar]
- 30.Research Unit Royal College of Psychiatrists. Health of the Nation Outcome Scales for Children and Adolescents. London: Royal College of Psychiatrists; 1995. [Google Scholar]
- 31.Rosen A, Parker G, Hadzi-Pavlovic D, et al. The Life Skills Profile: a measure assessing functioning and disability in schizophrenia. Schizophr Bull. 1987;15:325–337. doi: 10.1093/schbul/15.2.325. [DOI] [PubMed] [Google Scholar]
- 32.Williams BC. Activities of daily living and costs in nursing homes. Health Care Financing Review. 1994;15:117–135. [PMC free article] [PubMed] [Google Scholar]
- 33.Schaffer D, Gould MS, Brasic J, et al. A Children's Global Assessment Scale (CGAS) Arch Gen Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]


