Abstract
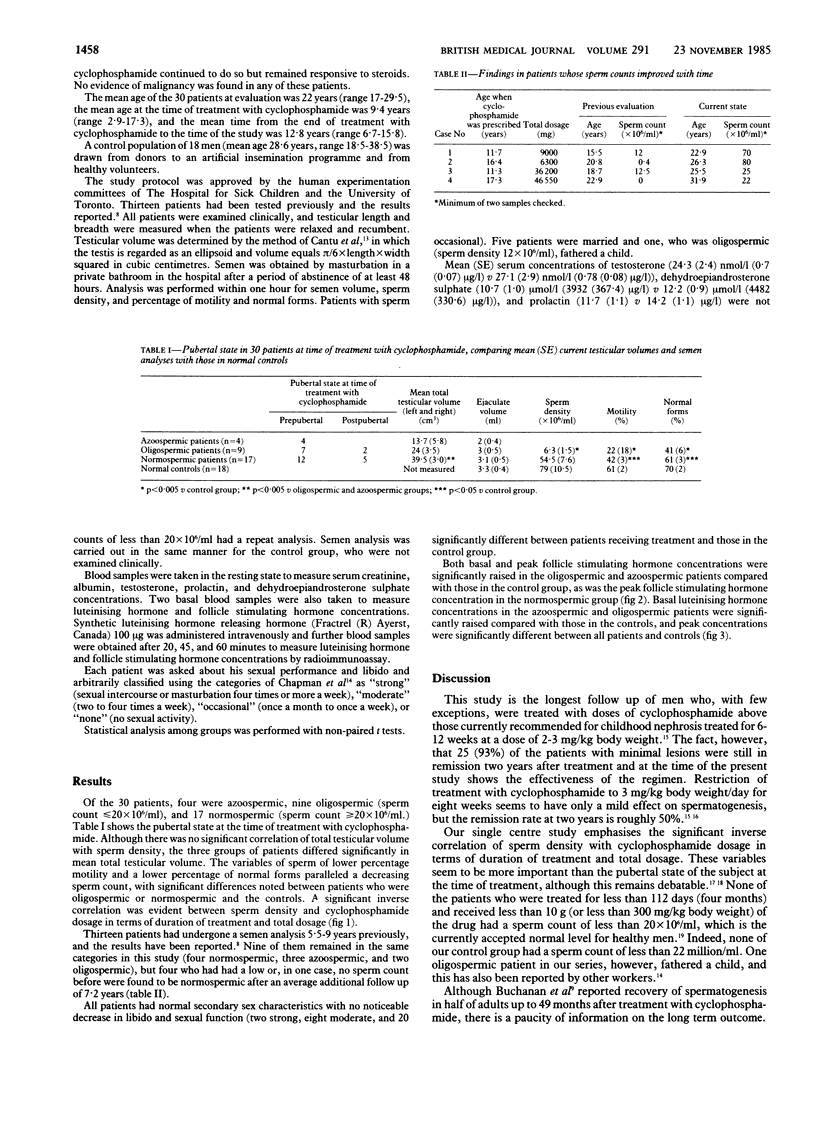
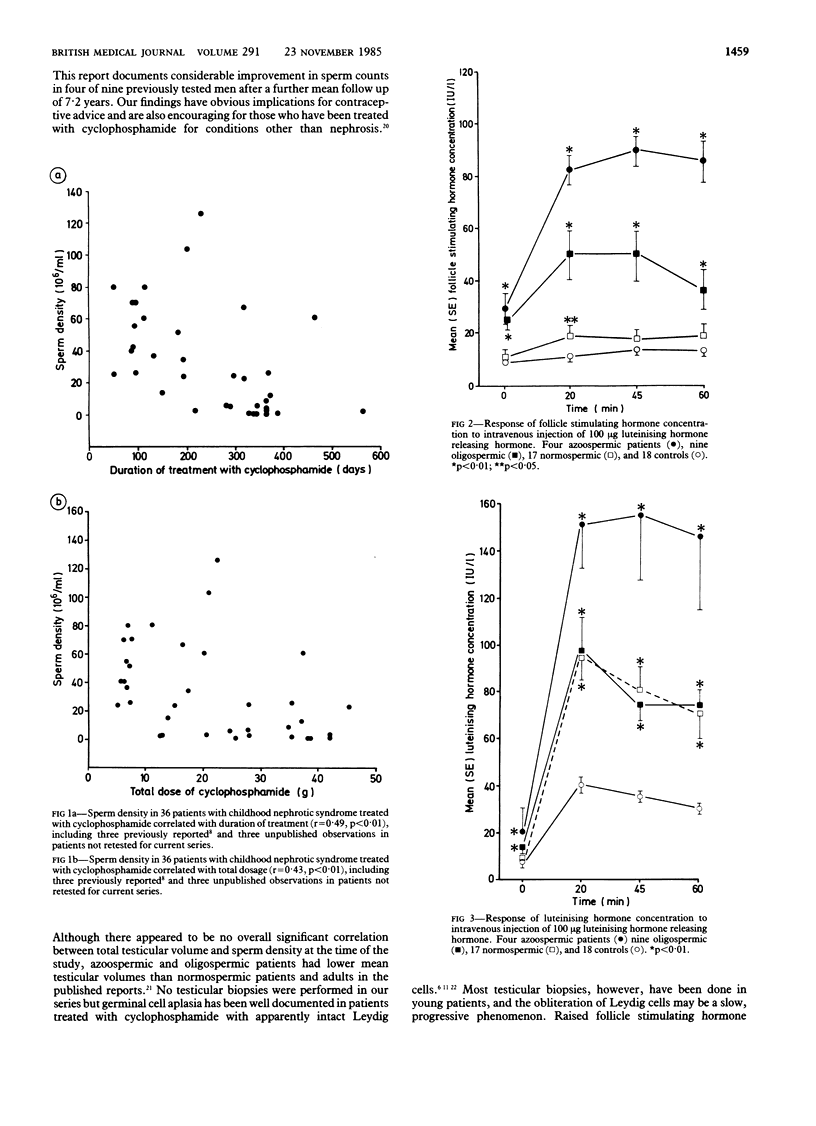
Thirty men treated in childhood with cyclophosphamide for a mean of 280 days were assessed at a mean of 12.8 years after treatment for hormone concentrations and spermatogenesis. Four were azoospermic, nine oligospermic, and 17 normospermic. There was a significant inverse correlation of sperm density with cyclophosphamide dosage and duration of treatment. After a further mean follow up of 7.2 years three patients who were previously oligospermic and one who was azoospermic had normal sperm counts. All patients had normal sexual characteristics and libido. Serum androgen and prolactin concentrations did not differ significantly between patients and controls. Raised basal and stimulated follicle stimulating hormone concentrations were in keeping with impaired spermatogenesis. All patients had significantly raised luteinising hormone responses on stimulation with luteinising hormone releasing hormone. The results suggest compensated Leydig cell failure, and patients with this condition require long term evaluation of testicular function. Potential recovery of spermatogenesis with time requires appropriate counselling and contraceptive advice.
Full text
PDF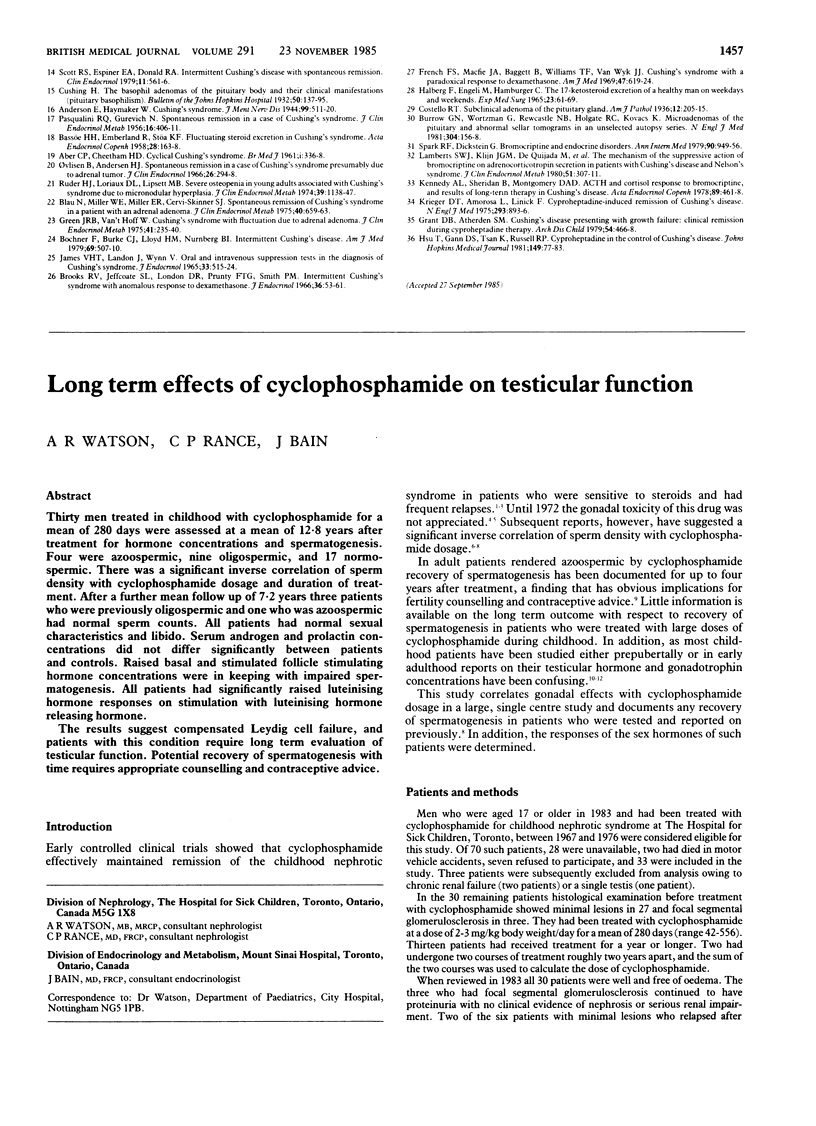

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arneil G. C. Cyclophosphamide and the prepubertal testis. Lancet. 1972 Dec 9;2(7789):1259–1260. doi: 10.1016/s0140-6736(72)92321-5. [DOI] [PubMed] [Google Scholar]
- Bain J. Male hypogonadism. Compr Ther. 1983 Feb;9(2):17–24. [PubMed] [Google Scholar]
- Bain J., Moskowitz J. P., Clapp J. J. LH and FSH response to gonadotropin releasing hormone (GnRH) in normospermic, oligospermic and azoospermic men. Arch Androl. 1978;1(2):147–152. doi: 10.3109/01485017808988331. [DOI] [PubMed] [Google Scholar]
- Barratt T. M., Soothill J. F. Controlled trial of cyclophosphamide in steroid-sensitive relapsing nephrotic syndrome of childhood. Lancet. 1970 Sep 5;2(7671):479–482. doi: 10.1016/s0140-6736(70)90108-x. [DOI] [PubMed] [Google Scholar]
- Buchanan J. D., Fairley K. F., Barrie J. U. Return of spermatogenesis after stopping cyclophosphamide therapy. Lancet. 1975 Jul 26;2(7926):156–157. doi: 10.1016/s0140-6736(75)90059-8. [DOI] [PubMed] [Google Scholar]
- Cantú J. M., Scaglia H. E., Medina M., González-Diddi M., Morato T., Moreno M. E., Pérez-Palacios G. Inherited congenital normofunctional testicular hyperplasia and mental deficiency. Hum Genet. 1976 Jul 7;33(1):23–33. doi: 10.1007/BF00447283. [DOI] [PubMed] [Google Scholar]
- Chiu J., McLaine P. N., Drummond K. N. A controlled prospective study of cyclophosphamide in relapsing, corticosteroid-responsive, minimal-lesion nephrotic syndrome in childhood. J Pediatr. 1973 Apr;82(4):607–613. doi: 10.1016/s0022-3476(73)80585-2. [DOI] [PubMed] [Google Scholar]
- Chong A. P., Walters C. A., Weinrieb S. A. The neglected laboratory test. The semen analysis. J Androl. 1983 Jul-Aug;4(4):280–282. doi: 10.1002/j.1939-4640.1983.tb02368.x. [DOI] [PubMed] [Google Scholar]
- De Groot G. W., Faiman C., Winter J. S. Cyclophosphamide and the prepubertal gonad: a negative report. J Pediatr. 1974 Jan;84(1):123–125. doi: 10.1016/s0022-3476(74)80572-x. [DOI] [PubMed] [Google Scholar]
- Etteldorf J. N., West C. D., Pitcock J. A., Williams D. L. Gonadal function, testicular histology, and meiosis following cyclophosphamide therapy in patients with nephrotic syndrome. J Pediatr. 1976 Feb;88(2):206–212. doi: 10.1016/s0022-3476(76)80983-3. [DOI] [PubMed] [Google Scholar]
- Fairley K. F., Barrie J. U., Johnson W. Sterility and testicular atrophy related to cyclophosphamide therapy. Lancet. 1972 Mar 11;1(7750):568–569. doi: 10.1016/s0140-6736(72)90358-3. [DOI] [PubMed] [Google Scholar]
- Farkas L. G. Basic morphological data of external genitals in 177 healthy Central European men. Am J Phys Anthropol. 1971 May;34(3):325–328. doi: 10.1002/ajpa.1330340303. [DOI] [PubMed] [Google Scholar]
- Hsu A. C., Folami A. O., Bain J., Rance C. P. Gonadal function in males treated with cyclophosphamide for nephrotic syndrome. Fertil Steril. 1979 Feb;31(2):173–177. doi: 10.1016/s0015-0282(16)43818-5. [DOI] [PubMed] [Google Scholar]
- Kirkland R. T., Bongiovanni A. M., Cornfield D., McCormick J. B., Parks J. S., Tenore A. Gonadotropin responses to luteinizing releasing factor in boys treated with cyclophosphamide for nephrotic syndrome. J Pediatr. 1976 Dec;89(6):941–944. doi: 10.1016/s0022-3476(76)80600-2. [DOI] [PubMed] [Google Scholar]
- Kumar R., Biggart J. D., McEvoy J., McGeown M. G. Cyclophosphamide and reproductive function. Lancet. 1972 Jun 3;1(7762):1212–1214. doi: 10.1016/s0140-6736(72)90927-0. [DOI] [PubMed] [Google Scholar]
- Lentz R. D., Bergstein J., Steffes M. W., Brown D. R., Prem K., Michael A. F., Vernier R. L. Postpubertal evaluation of gonadal function following cyclophosphamide therapy before and during puberty. J Pediatr. 1977 Sep;91(3):385–394. doi: 10.1016/s0022-3476(77)81305-x. [DOI] [PubMed] [Google Scholar]
- Need for steroids in kidney transplantation. Lancet. 1979 Feb 3;1(8110):265–266. [PubMed] [Google Scholar]
- Parra A., Santos D., Cervantes C., Sojo I., Carranco A., Cortés-Gallegos V. Plasma gonadotropins and gonadal steroids in children treated with cyclophosphamide. J Pediatr. 1978 Jan;92(1):117–124. doi: 10.1016/s0022-3476(78)80092-4. [DOI] [PubMed] [Google Scholar]
- Pennisi A. J., Grushkin C. M., Lieberman E. Gonadal function in children with nephrosis treated with cyclophosphamide. Am J Dis Child. 1975 Mar;129(3):315–318. doi: 10.1001/archpedi.1975.02120400027006. [DOI] [PubMed] [Google Scholar]
- Penso J., Lippe B., Ehrlich R., Smith F. G., Jr Testicular function in prepubertal and pubertal male patients treated with cyclophosphamide for nephrotic syndrome. J Pediatr. 1974 Jun;84(6):831–836. doi: 10.1016/s0022-3476(74)80758-4. [DOI] [PubMed] [Google Scholar]
- Rance C. P., Arbus G. S., Balfe J. W. Management of the nephrotic syndrome in children. Pediatr Clin North Am. 1976 Nov;23(4):735–750. doi: 10.1016/s0031-3955(16)33357-0. [DOI] [PubMed] [Google Scholar]
- Rapola J., Koskimies O., Huttunen N. P., Floman P., Vilska J., Hallman N. Cyclophosphamide and the pubertal testis. Lancet. 1973 Jan 13;1(7794):98–99. doi: 10.1016/s0140-6736(73)90491-1. [DOI] [PubMed] [Google Scholar]
- Rosen S. W., Weintraub B. D. Monotropic increase of serum FSH correlated with low sperm count in young men with idiopathic oligospermia and aspermia. J Clin Endocrinol Metab. 1971 Mar;32(3):410–416. doi: 10.1210/jcem-32-3-410. [DOI] [PubMed] [Google Scholar]
- Simpson H. C., Simpson R. W., Lousley S., Carter R. D., Geekie M., Hockaday T. D., Mann J. I. A high carbohydrate leguminous fibre diet improves all aspects of diabetic control. Lancet. 1981 Jan 3;1(8210):1–5. doi: 10.1016/s0140-6736(81)90112-4. [DOI] [PubMed] [Google Scholar]


